PDO 315 Pulp Therapy
Primary Pulp
Morphological Differences:
Increased number of accessory canals
Flat ribbon shaped canals
More open apices
Greater curvature of molar roots
Relatively longer more slender roots in molars
Larger pulp relative to crown size
Pulp horns closer to outer surface of tooth
Mesial pulp horns closer to surface than distal
Apical physiologic resorption
Presence of succedaneous tooth
Pulpal Diagnosis
Healthy (normal) pulp
Reversible pulpitis: Inflamed pulp capable of healing
Irreversible pulpitis: Inflamed pulp incapable of healing
Necrotic pulp
Clinical Diagnosis
Comprehensive medical history
Dental history with chief complaint
Subjective evaluation of current symptoms
Objective examination (extraoral and intraoral soft and hard tissue)
Radiographic examination
Clinical tests: palpation, percussion, mobility
Pulp testing: EPT & thermal tests unreliable in primary and immature permanent teeth
Direct pulpal observation as the final diagnostic step
Pain Evaluation Questions
When did symptoms start
Point specifically where in your mouth the pain is coming from
Wong-Baker pain scale
Describe pain: sharp, dull, aching, throbbing, etc.
Is pain constant or does it come and go
Does anything make the pain worse (hot/cold food, sweet/spicy food, biting, etc.)
If there is anything that triggers pain, does the pain linger or go away quickly
Does anything make the pain better (OTC pain medication)
Does it hurt to eat
Does it hurt when you are trying to sleep or watch tv
Healthy Pulp
Clinical and Radiographic exam often reveals caries that are superficial to moderate in depth
No history of pain associated with carious lesions
Soft tissue and supporting periodontal structures normal
Primary teeth with diagnosis of “healthy” pulp requiring pulp therapy should be treated with vital pulp therapy
Reversible Pulpitis
Clinical and Radiographic exam often reveals caries that are moderate to deep and may be approximating the pulp
Non-spontaneous pain
Pain of short duration that does not linger
Pain relieved with OTC analgesics, removal or stimulus, or brushing away plaque and food debris
Absence of signs or symptoms of irreversible pulpitis
Primary teeth with diagnosis of “reversible pulpitis” requiring pulp therapy should be treated with vital pulp therapy
Irreversible Pulpitis
Clinical and Radiographic exam often reveals caries that are moderate to deep and may be approximating the pulp
Spontaneous unprovoked pain
Nocturnal pain (while sleeping or relaxing watching tv)
Pain not relieved with OTC analgesics, removal or stimulus, or brushing away plaque and food debris
Signs of irreversible pulpitis: sinus tract, excessive mobility, furcation/apical radiolucency, radiographic evidence of internal/external non-physiologic root resorption
Primary teeth with diagnosis of “irreversible pulpitis” requiring pulp therapy should be treated with nonvital pulp therapy
Necrotic Pulp
Clinical and Radiographic exam often reveals caries that are moderate to deep and may be approximating or into the pulp
May or may not have current symptoms of pain
Ask about periods of pain in the past
Signs of necrotic pulp: sinus tract, excessive mobility, furcation/apical radiolucency, radiographic evidence of internal/external non-physiologic root resorption
Primary teeth with diagnosis of “necrotic” pulp requiring pulp therapy should be treated with nonvital pulp therapy
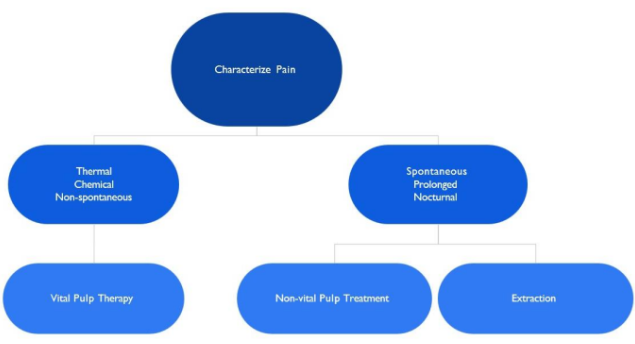
Characterize Pain
Radiographic Interpretation
Furcation or periapical changes
Widening of the PDL
Destruction of supporting bone (lamina dura & alveolar trabeculation)
Pathologic root resorption
Proximity of carious lesion to the pulp not always accurately determined from radiograph
Inflammatory response of the pulp can not be accurately diagnosed on radiograph
Treatment Considerations
Patient’s medical history
Value of each tooth in relation to child’s development
Restorability of the tooth
Consider extraction when:
Infectious process cannot be arrested
Bony support cannot be regained
Inadequate tooth structure remains
Excessive pathologic root resorption exists
Evaluation of treatment prognosis:
Pulp treatment/restoration vs. extraction/space maintenance:
importance of maintaining tooth in arch for continued development
more likely to elect to perform pulp therapy vs extraction on primary second molar to prevent mesial drift/tipping of permanent first molars
Other considerations:
patient and parent cooperation/motivation
Caries activity of patient and prognosis of rehabilitation
Stage of dental development
Degree of difficulty in performing procedure
Space management issues
Isolation:
Necessary to minimize bacterial contamination and to protect soft and hard tissues
Rubber dam isolation is gold standard for pulpal treatment
If unable to use rubber dam, other isolation may be considered
Anesthesia:
Profound anesthesia is a requirement for pulpal therapy
Beware of teeth with acutely inflamed pulp (hot teeth)
Use of sterile burs and instruments required:
Direct pulpal observation: The final diagnostic step
Size of exposure and degree of inflammation are directly related
Watery exudate or pus at site of pulpal exposure indicative of pulpal necrosis
Black or white pulp coloration indicative of pulpal necrosis
No bleeding of pulp tissue indicative of pulpal necrosis
Excessive bleeding of pulp that is not controlled by pressure of damp cotton pellet in 2-5 min indicative of irreversible pulpitis
Pink to red pulp tissue with bleeding controlled by pressure of damp cotton pellet in 2-3 min indicative of healthy or reversibly inflamed pulp
Vital Pulp Therapy in Primary Teeth
Protective liner
Tooth with a normal pulp and complete caries removal
A thinly-applied material placed on dentin in proximity to underlying pulpal surface of deep cavity prep
MTA, trisilicate cements, calcium hydroxide, or other biocompatible material
Protective barrier between the restorative material and pulp
To minimize injury to the pulp, promote pulp tissue healing and tertiary dentin formation, and/or minimize post- operative sensitivity
Indirect pulp treatment (IPT)
Deep caries lesion approximating the pulp
No pulpitis or reversible pulpitis
Leaves the deepest caries adjacent to the pulp undisturbed in an effort to avoid a pulp exposure
Margins must be caries free to establish an adequate seal during restoration
Caries-affected dentin is sealed with biocompatible material
Stimulate healing and repair
Examples: Resin modified glass ionomer (Vitrebond), calcium hydroxide (Dycal), or MTA (or any other biocompatible material)
Tooth restored with a material that seals the tooth from microleakage
Direct pulp cap
A pinpoint exposure (one millimeter or less) of the pulp is during cavity preparation (mechanical exposure) or following traumatic injury
Biocompatible radiopaque base such as MTA or calcium hydroxide placed in contact with the exposed pulp tissue
Tooth is restored with material that seals tooth from microleakage
Pulp healing and reparative dentin formation should result
Not typically performed for carious exposures on primary teeth
Pulpotomy
Caries removal results in a pulp exposure in a tooth with a normal pulp or reversible pulpitis or after a traumatic pulp exposure
Coronal pulp is amputated, pulpal hemorrhage controlled, and remaining vital radicular pulp tissue surface is treated
Pulpotomy Medicaments
Only MTA and formocresol are recommended as the medicament of choice for teeth expected to be retained for 24 months or longer
Ferric sulfate, lasers, sodium hypochlorite, and tricalcium silicate have also been used but have conditional recommendations based on a review of the literature according to the AAPD
Calcium hydroxide is NOT recommended for pulpotomy
Pulpotomy Success
Asymptomatic without sensitivity, pain or swelling
No postoperative radiographic evidence of pathologic external root resorption
Monitor internal root resorption
May be self-limiting and stable
Remove tooth if clinical signs of infection or inflammation
Success
Clinical > radiographic > histological
In vital primary teeth with deep carious lesions treated with pulpotomy due to pulp exposure during caries removal, does the choice of medicament or technique affect success?
Systematic review
Overall success rate at 24 months for MTA, formocresol, FS, NaOCl, calcium hydroxide, and laser → 82.6 percent
MTA and formocresol success rates were the highest and not significantly different ○ MTA → 89.6% ○ Formocresol → 85.0%
Recommends the use of MTA or formocresol ○ Strong recommendation, moderate-quality evidence
Recommends AGAINST the use of calcium hydroxide
Pulpotomy Steps
Pulpal Diagnosis
Appropriate anesthesia, proper isolation, sterile burs & instruments
Caries removal → pulp exposure
Pulp access:
Complete removal of roof of pulp chamber necessary
Removal of all caries and overhanging dentin to allow clear access
Removal of coronal pulp tissue
Pain during pulp removal may indicate hyperemia → non-vital pulp therapy or extraction
Funnel shaped access to canals, with pulp amputated to this level
No tissue tags remain
Achieve hemostasis with damp cotton pellets (use sterile water)
Remove all cotton pellets
Examine pulp →
Bleeding after treatment may indicate hyperemia → non-vital pulp therapy or extraction
May gently disinfect chamber with cotton pellet soaked in sodium hypochlorite
Place MTA on pulp stumps with enough material to completely cover all exposed pulp
Fill chamber with base (GI, ZOE, Tempit)
Restore tooth (full coverage restoration preferred)
Non-vital Pulp Therapies in Primary Teeth
Pulpectomy
Lesion sterilization/tissue repair (LSTR)
Pulpectomy Indications
Tooth with irreversible pulpitis or necrosis (due to caries or trauma)
Tooth treatment planned for pulpotomy in which the radicular pulp exhibits clinical signs of irreversible pulpitis or pulp necrosis (e.g., suppuration, purulence)
Roots should exhibit minimal or no resorption
Pulpectomy Steps
Pulp access:
Complete removal of roof of pulp chamber necessary
Removal of all caries and overhanging dentin to allow clear access
Complete pulpal debridement with hand or rotary files:
Pulp chamber AND root canals are debrided
Use radiographs for working length
Care not to force instruments through apex
Irrigation & Disinfection of canals with sodium hypochlorite (care must be taken not to force irrigation fluid out of apicies)
Canals dried with paper points
Filled with resorbable material
Vitapex or Kri-paste
Fill chamber with GI, ZOE, Tempit, etc.
Restored with a restoration that seals the tooth from microleakage → full coverage restoration
Evaluate non-vital pulp treatments for success and adverse events clinically and radiographically at least every 12 months.
Lesion Sterilization Tissue Repair (LSTR) Indications
Primary tooth with irreversible pulpitis or necrosis
When a tooth is to be maintained for less than twelve months and exhibits root resorption LSTR is preferred to pulpectomy
Steps
Primary tooth with irreversible pulpitis or necrosis
After opening pulpal chamber, canal orifices are enlarged using a large round bur to create medication receptacles
No instrumentation of the root canals
Walls of the chamber are cleaned with phosphoric acid, rinsed and dried
A three antibiotic mixture of clindamycin, metronidazole, and ciprofloxacin is combined with a liquid vector to form a paste
Paste placed directly into the medication receptacles and over the pulpal floor → disinfect the root canals
Covered with glass-ionomer cement and full coverage restoration
When a tooth is to be maintained for less than twelve months and exhibits root resorption, LSTR is preferred to pulpectomy
Vital Pulp Therapy in Immature Permanent Teeth
Protective liner
Indirect pulp treatment
see slides under vital pulp therapy in primary teeth
Direct pulp cap
Partial pulpotomy for carious or traumatic exposure (Cvek pulpotomy)
Complete pulpotomy
Apexogenesis (root formation)
Direct Pulp Cap
Permanent tooth with small carious, mechanical or traumatic exposure in a tooth with a normal pulp
Hemorrhage control is obtained
Exposed pulp is capped with a material such as calcium hydroxide or MTA
Restoration that seals the tooth from microleakage
Partial pulpotomy for carious exposure
Young permanent tooth with carious pulp exposure
Vital tooth with diagnosis of normal pulp or reversible pulpitis
Inflamed pulp tissue beneath an exposure is removed to a depth of 1-3mm or deeper to reach healthy pulp tissue
Pulpal bleeding controlled (within several minutes) by irrigation with a bacteriocidal agent
Sodium hypochlorite or chlorhexidine
Exposure covered with calcium hydroxide or MTA
MTA (at least 1.5 millimeters thick) should cover the exposure and surrounding dentin followed by a layer of light cured resin-modified glass ionomer
Restoration that seals the tooth from microleakage is placed
Partial Pulpotomy for traumatic exposure (Cvek pulpotomy)
Vital, traumatically-exposed, young permanent tooth, especially one with an incompletely formed apex
Inflamed pulp tissue beneath an exposure that is 4mm or less in size removed to a depth of 1-3mm or more to reach the deeper healthy tissue
Pulpal bleeding controlled using irrigants (ex. sodium hypochlorite or chlorhexidine) and site is covered with calcium hydroxide or MTA
Calcium hydroxide has been demonstrated to have long-term success, MTA results in more predictable dentin bridging and pulp health
MTA (at least 1.5 millimeters thick) should cover the exposure and surrounding dentin, followed by a layer of light- cured resin-modified glass ionomer
Complete Pulpotomy
Immature permanent teeth with carious pulp exposure → interim procedure to allow continued root development (apexogenesis)
Emergency procedure for temporary relief of symptoms until a definitive root canal treatment can be accomplished
Complete removal of the coronal vital pulp tissue
Placement of a biologically acceptable material in the pulp chamber
Restoration of the tooth
Compared to traditionally-used calcium hydroxide, MTA and tricalcium silicate exhibit superior long-term seal and reparative dentin formation leading to a higher success rate
Apexogenesis
Histological term → continued physiologic development and formation of the root’s apex
Formation of the apex in vital young permanent teeth can be accomplished by implementing the appropriate vital pulp therapy
Indirect pulp treatment
Direct pulp capping
Partial pulpotomy for carious and traumatic exposures
Non-vital Pulp Therapy in Immature Permanent Teeth
Pulpectomy
Apexification
Regenerative Endodontics
Non-vital Pulp Therapy in Immature Permanent Teeth: Pulpectomy
Restorable permanent tooth with closed apex that exhibits irreversible pulpitis or a necrotic pulp
Entire roof of the pulp chamber removed → gain access to the canals and eliminate all coronal pulp tissue
Following cleaning, disinfection, and shaping of the root canal system, obturation of the entire root canal accomplished with a biologically-acceptable semi-solid or solid filling material
Non-vital Pulp Therapy in Immature Permanent Teeth: Apexification
Non-vital permanent teeth with incompletely formed roots
Inducing root end closure by removing coronal and non-vital radicular tissue just short of the root end
Biocompatible agent (ex. calcium hydroxide) placed in the canals for two weeks to one month to disinfect canal space
Root end closure accomplished with apical barrier (ex. MTA)
Gutta percha to fill remaining canal space
Non-vital Pulp Therapy in Immature Permanent Teeth: Regenerative Endodontics
Definition: biologically based procedures designed to physiologically replace damaged tooth structure (dentin, root structures, pulp-dentin complex)
Indication: nonvital permanent teeth with incompletely formed roots
Goals:
Elimination of clinical symptoms/ signs and resolution of apical periodontitis in teeth with a necrotic pulp and immature apex
Thickening of the canal walls and/or continued root maturation is an additional goal
Disinfected root canal space is filled with the host’s own vital tissue
Summary of Materials
Pulpal liner or Indirect Pulp Treatment
Vitrebond (resin modified glass ionomer)
Ultra-Blend (calcium hydroxide in urethane dimethacrylate base)
Direct Pulp Cap
Calcium Hydroxide (Dycal)
MTA
Pulpotomy
MTA
Formocresol
Pulpectomy
Vitapex
Kri-paste
Base
Zinc Oxide Eugenol (ZOE)
Calcium sulfate and zinc oxide → Tempit
GI
RMGI
Calcium Hydroxide
Mineralizing/bacteriostatic agent
Alkaline pH → 12
Caustic when placed against vital pulp tissue
Causes superficial necrosis
Irritant quality
Stimulates development of calcific bridge → evident 1 month after placement
Pulp beneath material remains vital and free of inflammation
MTA
High biocompatibility
Alkaline pH
Induces dentin bridging
Expensive (relative to cost of formocresol)
Grey MTA → discoloration
White MTA
Formocresol
Fixative and bactericidal action
Does not promote healing
Caustic to gingival tissues
1:5 concentration → Buckley’s formocresol
1:5 dilution → equally good results with fewer post op complications than full strength
Interim use in permanent teeth to be followed by conventional endodontic therapy (RCT)
Concerns with toxicity
Study
Purpose: determine presence of formocresol in plasma of children undergoing oral rehabilitation involving pulp therapy under general anesthesia
Method:
30 children age 2-6 years
Preop, intra-op, & post-op peripheral venous samples collected
Samples analyzed for formaldehyde and cresol levels
Results/Conclusions:
85 pulpotomies performed, 312 blood samples collected
Formaldehyde was undetectable above baseline and cresol was undetectable in all samples
Benzyl alcohol (byproduct of cresol metabolism) present in all samples except pre-op samples
Levels present far below FDA daily allowance
Unlikely that formocresol used in dose typical for vital pulpotomy poses any risk to children
Primary Pulpectomy Medicaments
Vitapex – Iodoform and calcium hydroxide
Radiopaque
Antibacterial
Easy to use
Kri Paste – Iodoform, parachlorophenol, camphormen
Bacteriocidal
Resorable
Less easy to use
Summary and Goals of Pulp Therapy
Summary
Proper diagnosis is KEY
Consider:
Most conservative treatment
Treatment that offers best chance of long term success
Treatment with least risk of subsequent complications
Always weigh potential risk of failure
Monitor pulpal treatment regularly
Abnormal root resorption
Abscess
Early exfoliation or over retention
Goals
Eliminate pain and infection
In vital teeth, maintain integrity and health of teeth and supporting tissue while maintaining vitality of pulp
In non-vital teeth, maintain integrity and health of supporting tissue, while retaining tooth to preserve form and function
Maintaining pulp vitality is a primary goal for treatment of young permanent dentition
In young permanent teeth with immature roots, the pulp is essential for continued apexogenesis
Long term retention of a permanent tooth requires favorable crown/root ratio and thick dentinal walls to withstand normal function
PDO 315 Pulp Therapy
Primary Pulp
Morphological Differences:
Increased number of accessory canals
Flat ribbon shaped canals
More open apices
Greater curvature of molar roots
Relatively longer more slender roots in molars
Larger pulp relative to crown size
Pulp horns closer to outer surface of tooth
Mesial pulp horns closer to surface than distal
Apical physiologic resorption
Presence of succedaneous tooth
Pulpal Diagnosis
Healthy (normal) pulp
Reversible pulpitis: Inflamed pulp capable of healing
Irreversible pulpitis: Inflamed pulp incapable of healing
Necrotic pulp
Clinical Diagnosis
Comprehensive medical history
Dental history with chief complaint
Subjective evaluation of current symptoms
Objective examination (extraoral and intraoral soft and hard tissue)
Radiographic examination
Clinical tests: palpation, percussion, mobility
Pulp testing: EPT & thermal tests unreliable in primary and immature permanent teeth
Direct pulpal observation as the final diagnostic step
Pain Evaluation Questions
When did symptoms start
Point specifically where in your mouth the pain is coming from
Wong-Baker pain scale
Describe pain: sharp, dull, aching, throbbing, etc.
Is pain constant or does it come and go
Does anything make the pain worse (hot/cold food, sweet/spicy food, biting, etc.)
If there is anything that triggers pain, does the pain linger or go away quickly
Does anything make the pain better (OTC pain medication)
Does it hurt to eat
Does it hurt when you are trying to sleep or watch tv
Healthy Pulp
Clinical and Radiographic exam often reveals caries that are superficial to moderate in depth
No history of pain associated with carious lesions
Soft tissue and supporting periodontal structures normal
Primary teeth with diagnosis of “healthy” pulp requiring pulp therapy should be treated with vital pulp therapy
Reversible Pulpitis
Clinical and Radiographic exam often reveals caries that are moderate to deep and may be approximating the pulp
Non-spontaneous pain
Pain of short duration that does not linger
Pain relieved with OTC analgesics, removal or stimulus, or brushing away plaque and food debris
Absence of signs or symptoms of irreversible pulpitis
Primary teeth with diagnosis of “reversible pulpitis” requiring pulp therapy should be treated with vital pulp therapy
Irreversible Pulpitis
Clinical and Radiographic exam often reveals caries that are moderate to deep and may be approximating the pulp
Spontaneous unprovoked pain
Nocturnal pain (while sleeping or relaxing watching tv)
Pain not relieved with OTC analgesics, removal or stimulus, or brushing away plaque and food debris
Signs of irreversible pulpitis: sinus tract, excessive mobility, furcation/apical radiolucency, radiographic evidence of internal/external non-physiologic root resorption
Primary teeth with diagnosis of “irreversible pulpitis” requiring pulp therapy should be treated with nonvital pulp therapy
Necrotic Pulp
Clinical and Radiographic exam often reveals caries that are moderate to deep and may be approximating or into the pulp
May or may not have current symptoms of pain
Ask about periods of pain in the past
Signs of necrotic pulp: sinus tract, excessive mobility, furcation/apical radiolucency, radiographic evidence of internal/external non-physiologic root resorption
Primary teeth with diagnosis of “necrotic” pulp requiring pulp therapy should be treated with nonvital pulp therapy
Characterize Pain
Radiographic Interpretation
Furcation or periapical changes
Widening of the PDL
Destruction of supporting bone (lamina dura & alveolar trabeculation)
Pathologic root resorption
Proximity of carious lesion to the pulp not always accurately determined from radiograph
Inflammatory response of the pulp can not be accurately diagnosed on radiograph
Treatment Considerations
Patient’s medical history
Value of each tooth in relation to child’s development
Restorability of the tooth
Consider extraction when:
Infectious process cannot be arrested
Bony support cannot be regained
Inadequate tooth structure remains
Excessive pathologic root resorption exists
Evaluation of treatment prognosis:
Pulp treatment/restoration vs. extraction/space maintenance:
importance of maintaining tooth in arch for continued development
more likely to elect to perform pulp therapy vs extraction on primary second molar to prevent mesial drift/tipping of permanent first molars
Other considerations:
patient and parent cooperation/motivation
Caries activity of patient and prognosis of rehabilitation
Stage of dental development
Degree of difficulty in performing procedure
Space management issues
Isolation:
Necessary to minimize bacterial contamination and to protect soft and hard tissues
Rubber dam isolation is gold standard for pulpal treatment
If unable to use rubber dam, other isolation may be considered
Anesthesia:
Profound anesthesia is a requirement for pulpal therapy
Beware of teeth with acutely inflamed pulp (hot teeth)
Use of sterile burs and instruments required:
Direct pulpal observation: The final diagnostic step
Size of exposure and degree of inflammation are directly related
Watery exudate or pus at site of pulpal exposure indicative of pulpal necrosis
Black or white pulp coloration indicative of pulpal necrosis
No bleeding of pulp tissue indicative of pulpal necrosis
Excessive bleeding of pulp that is not controlled by pressure of damp cotton pellet in 2-5 min indicative of irreversible pulpitis
Pink to red pulp tissue with bleeding controlled by pressure of damp cotton pellet in 2-3 min indicative of healthy or reversibly inflamed pulp
Vital Pulp Therapy in Primary Teeth
Protective liner
Tooth with a normal pulp and complete caries removal
A thinly-applied material placed on dentin in proximity to underlying pulpal surface of deep cavity prep
MTA, trisilicate cements, calcium hydroxide, or other biocompatible material
Protective barrier between the restorative material and pulp
To minimize injury to the pulp, promote pulp tissue healing and tertiary dentin formation, and/or minimize post- operative sensitivity
Indirect pulp treatment (IPT)
Deep caries lesion approximating the pulp
No pulpitis or reversible pulpitis
Leaves the deepest caries adjacent to the pulp undisturbed in an effort to avoid a pulp exposure
Margins must be caries free to establish an adequate seal during restoration
Caries-affected dentin is sealed with biocompatible material
Stimulate healing and repair
Examples: Resin modified glass ionomer (Vitrebond), calcium hydroxide (Dycal), or MTA (or any other biocompatible material)
Tooth restored with a material that seals the tooth from microleakage
Direct pulp cap
A pinpoint exposure (one millimeter or less) of the pulp is during cavity preparation (mechanical exposure) or following traumatic injury
Biocompatible radiopaque base such as MTA or calcium hydroxide placed in contact with the exposed pulp tissue
Tooth is restored with material that seals tooth from microleakage
Pulp healing and reparative dentin formation should result
Not typically performed for carious exposures on primary teeth
Pulpotomy
Caries removal results in a pulp exposure in a tooth with a normal pulp or reversible pulpitis or after a traumatic pulp exposure
Coronal pulp is amputated, pulpal hemorrhage controlled, and remaining vital radicular pulp tissue surface is treated
Pulpotomy Medicaments
Only MTA and formocresol are recommended as the medicament of choice for teeth expected to be retained for 24 months or longer
Ferric sulfate, lasers, sodium hypochlorite, and tricalcium silicate have also been used but have conditional recommendations based on a review of the literature according to the AAPD
Calcium hydroxide is NOT recommended for pulpotomy
Pulpotomy Success
Asymptomatic without sensitivity, pain or swelling
No postoperative radiographic evidence of pathologic external root resorption
Monitor internal root resorption
May be self-limiting and stable
Remove tooth if clinical signs of infection or inflammation
Success
Clinical > radiographic > histological
In vital primary teeth with deep carious lesions treated with pulpotomy due to pulp exposure during caries removal, does the choice of medicament or technique affect success?
Systematic review
Overall success rate at 24 months for MTA, formocresol, FS, NaOCl, calcium hydroxide, and laser → 82.6 percent
MTA and formocresol success rates were the highest and not significantly different ○ MTA → 89.6% ○ Formocresol → 85.0%
Recommends the use of MTA or formocresol ○ Strong recommendation, moderate-quality evidence
Recommends AGAINST the use of calcium hydroxide
Pulpotomy Steps
Pulpal Diagnosis
Appropriate anesthesia, proper isolation, sterile burs & instruments
Caries removal → pulp exposure
Pulp access:
Complete removal of roof of pulp chamber necessary
Removal of all caries and overhanging dentin to allow clear access
Removal of coronal pulp tissue
Pain during pulp removal may indicate hyperemia → non-vital pulp therapy or extraction
Funnel shaped access to canals, with pulp amputated to this level
No tissue tags remain
Achieve hemostasis with damp cotton pellets (use sterile water)
Remove all cotton pellets
Examine pulp →
Bleeding after treatment may indicate hyperemia → non-vital pulp therapy or extraction
May gently disinfect chamber with cotton pellet soaked in sodium hypochlorite
Place MTA on pulp stumps with enough material to completely cover all exposed pulp
Fill chamber with base (GI, ZOE, Tempit)
Restore tooth (full coverage restoration preferred)
Non-vital Pulp Therapies in Primary Teeth
Pulpectomy
Lesion sterilization/tissue repair (LSTR)
Pulpectomy Indications
Tooth with irreversible pulpitis or necrosis (due to caries or trauma)
Tooth treatment planned for pulpotomy in which the radicular pulp exhibits clinical signs of irreversible pulpitis or pulp necrosis (e.g., suppuration, purulence)
Roots should exhibit minimal or no resorption
Pulpectomy Steps
Pulp access:
Complete removal of roof of pulp chamber necessary
Removal of all caries and overhanging dentin to allow clear access
Complete pulpal debridement with hand or rotary files:
Pulp chamber AND root canals are debrided
Use radiographs for working length
Care not to force instruments through apex
Irrigation & Disinfection of canals with sodium hypochlorite (care must be taken not to force irrigation fluid out of apicies)
Canals dried with paper points
Filled with resorbable material
Vitapex or Kri-paste
Fill chamber with GI, ZOE, Tempit, etc.
Restored with a restoration that seals the tooth from microleakage → full coverage restoration
Evaluate non-vital pulp treatments for success and adverse events clinically and radiographically at least every 12 months.
Lesion Sterilization Tissue Repair (LSTR) Indications
Primary tooth with irreversible pulpitis or necrosis
When a tooth is to be maintained for less than twelve months and exhibits root resorption LSTR is preferred to pulpectomy
Steps
Primary tooth with irreversible pulpitis or necrosis
After opening pulpal chamber, canal orifices are enlarged using a large round bur to create medication receptacles
No instrumentation of the root canals
Walls of the chamber are cleaned with phosphoric acid, rinsed and dried
A three antibiotic mixture of clindamycin, metronidazole, and ciprofloxacin is combined with a liquid vector to form a paste
Paste placed directly into the medication receptacles and over the pulpal floor → disinfect the root canals
Covered with glass-ionomer cement and full coverage restoration
When a tooth is to be maintained for less than twelve months and exhibits root resorption, LSTR is preferred to pulpectomy
Vital Pulp Therapy in Immature Permanent Teeth
Protective liner
Indirect pulp treatment
see slides under vital pulp therapy in primary teeth
Direct pulp cap
Partial pulpotomy for carious or traumatic exposure (Cvek pulpotomy)
Complete pulpotomy
Apexogenesis (root formation)
Direct Pulp Cap
Permanent tooth with small carious, mechanical or traumatic exposure in a tooth with a normal pulp
Hemorrhage control is obtained
Exposed pulp is capped with a material such as calcium hydroxide or MTA
Restoration that seals the tooth from microleakage
Partial pulpotomy for carious exposure
Young permanent tooth with carious pulp exposure
Vital tooth with diagnosis of normal pulp or reversible pulpitis
Inflamed pulp tissue beneath an exposure is removed to a depth of 1-3mm or deeper to reach healthy pulp tissue
Pulpal bleeding controlled (within several minutes) by irrigation with a bacteriocidal agent
Sodium hypochlorite or chlorhexidine
Exposure covered with calcium hydroxide or MTA
MTA (at least 1.5 millimeters thick) should cover the exposure and surrounding dentin followed by a layer of light cured resin-modified glass ionomer
Restoration that seals the tooth from microleakage is placed
Partial Pulpotomy for traumatic exposure (Cvek pulpotomy)
Vital, traumatically-exposed, young permanent tooth, especially one with an incompletely formed apex
Inflamed pulp tissue beneath an exposure that is 4mm or less in size removed to a depth of 1-3mm or more to reach the deeper healthy tissue
Pulpal bleeding controlled using irrigants (ex. sodium hypochlorite or chlorhexidine) and site is covered with calcium hydroxide or MTA
Calcium hydroxide has been demonstrated to have long-term success, MTA results in more predictable dentin bridging and pulp health
MTA (at least 1.5 millimeters thick) should cover the exposure and surrounding dentin, followed by a layer of light- cured resin-modified glass ionomer
Complete Pulpotomy
Immature permanent teeth with carious pulp exposure → interim procedure to allow continued root development (apexogenesis)
Emergency procedure for temporary relief of symptoms until a definitive root canal treatment can be accomplished
Complete removal of the coronal vital pulp tissue
Placement of a biologically acceptable material in the pulp chamber
Restoration of the tooth
Compared to traditionally-used calcium hydroxide, MTA and tricalcium silicate exhibit superior long-term seal and reparative dentin formation leading to a higher success rate
Apexogenesis
Histological term → continued physiologic development and formation of the root’s apex
Formation of the apex in vital young permanent teeth can be accomplished by implementing the appropriate vital pulp therapy
Indirect pulp treatment
Direct pulp capping
Partial pulpotomy for carious and traumatic exposures
Non-vital Pulp Therapy in Immature Permanent Teeth
Pulpectomy
Apexification
Regenerative Endodontics
Non-vital Pulp Therapy in Immature Permanent Teeth: Pulpectomy
Restorable permanent tooth with closed apex that exhibits irreversible pulpitis or a necrotic pulp
Entire roof of the pulp chamber removed → gain access to the canals and eliminate all coronal pulp tissue
Following cleaning, disinfection, and shaping of the root canal system, obturation of the entire root canal accomplished with a biologically-acceptable semi-solid or solid filling material
Non-vital Pulp Therapy in Immature Permanent Teeth: Apexification
Non-vital permanent teeth with incompletely formed roots
Inducing root end closure by removing coronal and non-vital radicular tissue just short of the root end
Biocompatible agent (ex. calcium hydroxide) placed in the canals for two weeks to one month to disinfect canal space
Root end closure accomplished with apical barrier (ex. MTA)
Gutta percha to fill remaining canal space
Non-vital Pulp Therapy in Immature Permanent Teeth: Regenerative Endodontics
Definition: biologically based procedures designed to physiologically replace damaged tooth structure (dentin, root structures, pulp-dentin complex)
Indication: nonvital permanent teeth with incompletely formed roots
Goals:
Elimination of clinical symptoms/ signs and resolution of apical periodontitis in teeth with a necrotic pulp and immature apex
Thickening of the canal walls and/or continued root maturation is an additional goal
Disinfected root canal space is filled with the host’s own vital tissue
Summary of Materials
Pulpal liner or Indirect Pulp Treatment
Vitrebond (resin modified glass ionomer)
Ultra-Blend (calcium hydroxide in urethane dimethacrylate base)
Direct Pulp Cap
Calcium Hydroxide (Dycal)
MTA
Pulpotomy
MTA
Formocresol
Pulpectomy
Vitapex
Kri-paste
Base
Zinc Oxide Eugenol (ZOE)
Calcium sulfate and zinc oxide → Tempit
GI
RMGI
Calcium Hydroxide
Mineralizing/bacteriostatic agent
Alkaline pH → 12
Caustic when placed against vital pulp tissue
Causes superficial necrosis
Irritant quality
Stimulates development of calcific bridge → evident 1 month after placement
Pulp beneath material remains vital and free of inflammation
MTA
High biocompatibility
Alkaline pH
Induces dentin bridging
Expensive (relative to cost of formocresol)
Grey MTA → discoloration
White MTA
Formocresol
Fixative and bactericidal action
Does not promote healing
Caustic to gingival tissues
1:5 concentration → Buckley’s formocresol
1:5 dilution → equally good results with fewer post op complications than full strength
Interim use in permanent teeth to be followed by conventional endodontic therapy (RCT)
Concerns with toxicity
Study
Purpose: determine presence of formocresol in plasma of children undergoing oral rehabilitation involving pulp therapy under general anesthesia
Method:
30 children age 2-6 years
Preop, intra-op, & post-op peripheral venous samples collected
Samples analyzed for formaldehyde and cresol levels
Results/Conclusions:
85 pulpotomies performed, 312 blood samples collected
Formaldehyde was undetectable above baseline and cresol was undetectable in all samples
Benzyl alcohol (byproduct of cresol metabolism) present in all samples except pre-op samples
Levels present far below FDA daily allowance
Unlikely that formocresol used in dose typical for vital pulpotomy poses any risk to children
Primary Pulpectomy Medicaments
Vitapex – Iodoform and calcium hydroxide
Radiopaque
Antibacterial
Easy to use
Kri Paste – Iodoform, parachlorophenol, camphormen
Bacteriocidal
Resorable
Less easy to use
Summary and Goals of Pulp Therapy
Summary
Proper diagnosis is KEY
Consider:
Most conservative treatment
Treatment that offers best chance of long term success
Treatment with least risk of subsequent complications
Always weigh potential risk of failure
Monitor pulpal treatment regularly
Abnormal root resorption
Abscess
Early exfoliation or over retention
Goals
Eliminate pain and infection
In vital teeth, maintain integrity and health of teeth and supporting tissue while maintaining vitality of pulp
In non-vital teeth, maintain integrity and health of supporting tissue, while retaining tooth to preserve form and function
Maintaining pulp vitality is a primary goal for treatment of young permanent dentition
In young permanent teeth with immature roots, the pulp is essential for continued apexogenesis
Long term retention of a permanent tooth requires favorable crown/root ratio and thick dentinal walls to withstand normal function