Enteral and Parenteral Nutrition
ENTERAL NUTRITION
ENTERAL NUTRITION (Tube Feeding)
a medical intervention that involves delivering nutrients directly into the gastrointestinal tract using a tube. Employed when oral intake is insufficient or unsafe, ensuring individuals receive essential nutrients for sustenance. Its Nutritional Goalis to provide a balanced and adequate nutrition solution to meet the nutritional requirements of individuals who cannot consume food orally
Indications
Malnutrition - condition where the body lacks essential nutrients, leading to impaired function and health.
Dysphagia - difficulty swallowing that may require tube feeding to bypass the oral route and deliver nutrients directly to the stomach or intestines.
Neurological Disorders - conditions that impair the ability to eat, making tube feeding a necessary intervention. Example: Comatose, Paralyzed, and Stroke.
Chronic/critical Illnesses - such as cancer or cystic fibrosis, may experience difficulty maintaining oral intake or oral intake is no longer feasible.
Gastrointestinal Disorders - gut function is compromised due to surgery, inflammation, or other issues, tube feeding can provide a way to support nutritional needs while bypassing affected areas.
End-of-Life Care - given to patients with irreversible conditions, and oral intake is no longer feasible; to maintain the patient's quality of life
Types
Nasoenteric Tube Feeding
Enterostomy Tube Feeding
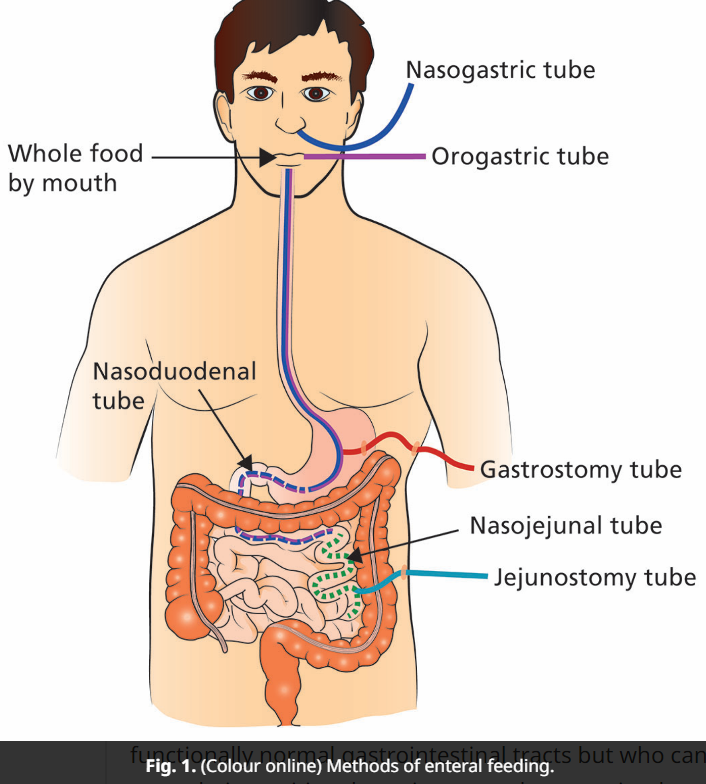
Nasoenteric Tube Feeding - the insertion of a plastic tube through the nose, past the throat, and down into the stomach or duodenum/jejunum. Nasal route makes for easier insertion and tubes are easier to secure.
Orogastric tube - inserted in the mouth when nasal mucosa is obstructed
Nasogastric tube (NGT)/Orogastric tube feeding - Intended for patients requiring nutritional support and need it for less than one month. most used route of access.
Nasoduodenal/Nasojejunal tube feeding - Intended for patients at high risk of pulmonary regurgitation, such as those with gastric atony or gastroparesis, and patients with pancreatitis, where it is considered desirable to feed beyond the ampulla
Enterostomy Tube Feeding - ostomy is creating an opening in the abdomen and gastro intestinal tract. Tube enterostomies can be placed using surgical, endoscopic, or radiological methods into the gastrointestinal tract. Can be either permanent or temporary. Usually placed if feeding of more than four weeks will be required, or if nasoenteral access is compromised in the short term.
Surgical gastrostomy - Indications include esophageal atresia, stricture and cancer, dysphagia due to neuromuscular disorders, or after trauma. Relative contraindications include primary disease of the stomach, abnormal gastric or duodenal emptying, and significant esophageal reflux. Specific complications include local irritation, hemorrhage, skin excoriation from leaking of gastric contents, and wound infection.
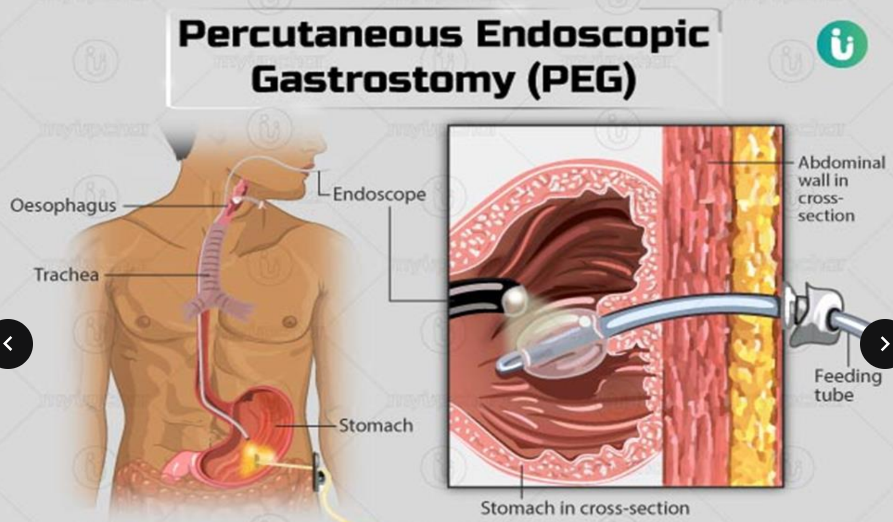
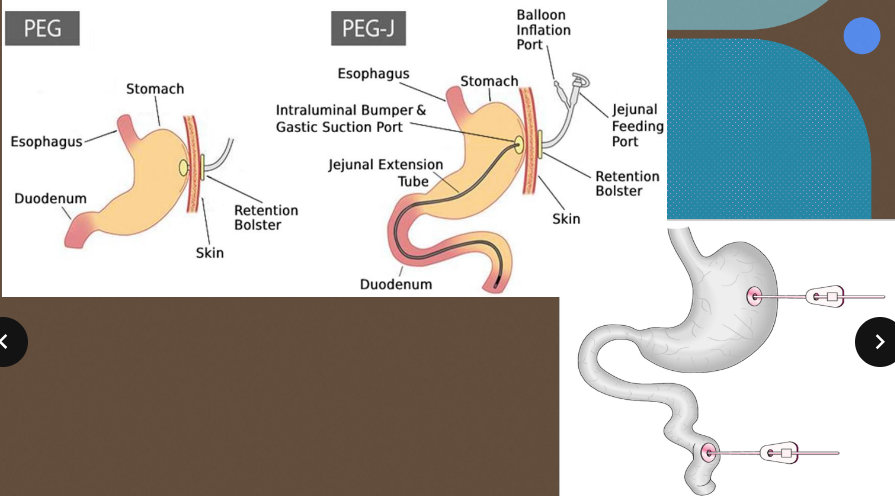
Percutaneous Endoscopic Gastrostomy (PEG) - method of choice for long-term feeding safer and more cost effective than surgically placed gastrostomies. Less risk from tube displacement compared with nasogastric feeding less reflux and feed aspiration, suggesting that overnight feeding. It is relatively safer. Important for mobile patients who do not want to be constrained during the day.
Percutaneous Endoscopic Duodenostomy/ Jejunostomy- used for patients with unsuitable stomach access and patients at risk from aspiration pneumonia; however, insertion is technically more demanding than PEG tubes.
Methods
Bolus Feeding - usually delivered four to eight times per day, with each feeding lasting about 15 to 30 minutes. More similar to a normal feeding pattern, more convenient, less expensive if a pump is not needed. Allows freedom of movement for the patient, so the child is not tethered to a feeding bag.
Asepto Syringe - 50mL
Intermittent Feeding - gravity drip feeding at 240-720 mL every 4-6 hours. commonly used for ambulatory patients and in the home-care setting. Method is more physiologic than continuous feedings. Allows for increased patient mobility and independence, and may enhance quality of life. Slower infusion time (for 60-75 min) may reduce gastrointestinal intolerance. Feeding pump may not be required, less expensive
Continuous Feeding - Delivering enteral nutrition with constant speed for 24 h via nutritional pump. Best suited for post pyloric feedings. Commonly used in patients who are intolerant of intermittent feedings, those who require mechanical intubation, and those who need the slowest possible infusion rate. Commonly believed to be better tolerated than bolus/ intermittent feedings in the critically ill. Ensures constant delivery of nutrients, decrease risk of gastric distention and aspiration; may result in fewer metabolic abnormalities. Limits patient mobility.

Formulas
Tube Feeding Formulas -are specially designed liquid formulations that provide essential nutrients to individuals who are unable to consume food orally. Tailored to meet specific nutritional requirements based on a patient's medical condition, age, and dietary needs.
Standard Polymeric Formulas- contain a balanced combination of macronutrients (carbohydrates, proteins, and fats), micronutrients (vitamins and minerals), and fiber. Suitable for individuals with intact digestive function and normal nutrient absorption. Commonly used for patients with various medical conditions, such as malnutrition, dysphagia, or those recovering from surgery.
Specialized Formulas
High-Calorie Formula - Enriched with higher amounts of calories to meet the increased energy needs of certain patients. Recommended for individuals with increased caloric requirements, such as those with severe malnutrition or hypermetabolic conditions.
Elemental or Semi-Elemental Formula - Predigested or partially broken-down nutrients, suitable for individuals with compromised digestive function. Ideal for patients with malabsorption issues, gastrointestinal disorders, or short bowel syndrome.
Renal Formula - Adjusted levels of electrolytes, proteins, and other nutrients to support individuals with kidney disease. Specifically designed for patients with renal impairment to manage fluid and electrolyte balance.
Pulmonary Formula - Modified to have a lower carbohydrate content, designed for individuals with respiratory conditions. Suitable for patients with (COPD) or those requiring respiratory support.
Disease-Specific Formulas
Diabetes-Specific Formula - Low in simple sugars and designed to manage blood glucose levels. Recommended for individuals with diabetes who require tube feeding.
Hepatic Formula - Adjusted protein levels and increased branched chain amino acids to support liver function. Designed for patients with liver disease or hepatic encephalopathy
Modular Formula - Individual components (carbohydrates, proteins, fats) provided separately, allowing for customization based on specific nutritional needs. Used for patients who require tailored nutritional support, enabling healthcare professionals to adjust macronutrient ratios as needed
Complications
Mechanical
Nasopharyngeal irritation
Luminal obstruction
Mucosal erosions Tube displacement Aspiration
Gastrointestinal Cramping/Distention
Vomiting
Diarrhea
Constipation
Metabolic
Hypertonic dehydration
Glucose intolerance
Cardiac failure Renal failure
Hepatic encephalopathy
Nursing Responsibilities
Assessment
Patient Assessment:
Conduct a thorough assessment of the patient's nutritional status, including weight, BMI, and dietary history.
Assess the patient's tolerance to tube feeding, looking for signs of complications or intolerance.
Tube Site Assessment:
Regularly assess the condition of the tube insertion site for signs of infection, redness, swelling, or discharge.
Ensure the tube is secure and intact (with tape), with no signs of dislodgement or malfunction.
Soiled tape from procedures like bed bath must be replaced
Bowel Sounds and Abdominal Assessment:
Monitor bowel sounds to assess gastrointestinal motility and function.
Perform regular abdominal assessments to identify signs of distention, discomfort, or complications.
Constipation and paralytic ileus might cause absence of bowel sounds so check for stool output.
Administration
Tube Feeding Administration:
Administer tube feedings according to the prescribed schedule and formula unless there is an observed intolerance.
Intolerance can be determined when aspirating with bolus syringe.
Undigested formulas less than 100cc must be taken out (lavage) if intolerance happens and proceed to a different feeding administration.
Aspirated Digested formulas less than 100cc must be returned inside as it contains electrolytes to avoid electrolyte imbalance.
Follow aseptic technique during handling of feeding equipment and formula.
Tube Placement Verification:
Confirm tube placement before each feeding and as per facility policy, using appropriate methods such as pH testing, X-ray, or other validated methods.
X-ray is usually required only in the initial insertion, not every feeding session. Recommended is Auscultation, Immersion, and Aspiration method.
Auscultation - introduce air in the tube, and using stethoscope, listen for whooshing sound over the stomach area.
Immersion - immerse the tip of NGT in a glass of water and observe for presence of bubbles. These bubbles appear due to respiration of the patient and indicates that the NGT is already located in the airway of the patient.
pH strip - used to check pH of aspirated gastric content. Acidic pH changes the strip color into red. Basic pH turns it into bluish or purplish color. Findings must be acidic.
Flushing the Tube:
Flush the feeding tube with water before and after medication administration to prevent blockages.
Use the recommended flush volume and frequency based on facility guidelines.
In normal conditions without limited water intake, you can administer 30-50ml after feeding.
If limited fluid intake, add more fluid as recommended.
Medication Administration
Administer medications as prescribed, considering compatibility with the enteral formula.
Some patients intolerance so it is advised not to mix the medication with the whole formula. Instead, use a medication cup and dissolve with 30ml water and administer after giving half of the initial formula.
Crush or dissolve medications appropriately to ensure smooth administration.
Monitoring for Adverse Reactions:
Monitor for any adverse reactions to medications or the enteral formula, such as nausea, vomiting, or allergic reactions.
Patient Education
Patient and Caregiver Education:
Educate the patient and caregivers about the purpose of tube feeding, the importance of proper care, and signs of complications.
Provide instructions on tube flushing, medication administration, and recognizing potential issues.
Positioning and Mobility:
Ensure proper patient positioning during and after tube feeding to prevent aspiration.
Ideal position is semi-fowlers to fowlers position. Any position with elevated head is fine to prevent gastric reflux.
Promote patient mobility to prevent complications such as pressure ulcers or respiratory issues.
Slow introduction of formula is suggested.
Documentation
Accurate Documentation:
Document all aspects of tube feeding administration, including the type and volume of formula, medications given, patient response, and any complications.
Regularly document tube site assessments and any changes in the patient's condition.
Regular Monitoring and Reporting:
Monitor the patient's overall condition and report any changes or concerns promptly to the healthcare team.
Collaborate with other healthcare professionals, such as dietitians (prepares formula for patients) and physicians (prescribes calories), to adjust the feeding plan as needed.
1kcal = 1ml
Safety
Preventing Infections:
Follow infection prevention protocols during tube feeding administration to minimize the risk of infections.
Practice hand hygiene and ensure a clean environment during tube care.
Use gloves if necessary.
Emergency Preparedness:
Be prepared for potential emergencies, such as dislodged tubes or respiratory distress, and know the appropriate response procedures.
Just remove and do not reinsert dislodged tubes or tubes that are almost out to prevent hitting other organs.
Stop feeding the panicking and nauseous patients and turn their head to the side to stop aspiration
PARENTERAL NUTRITION (PN)
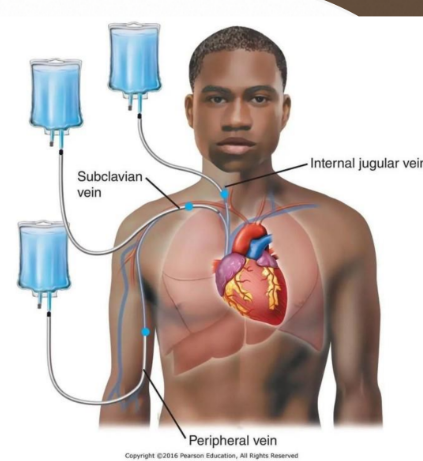
Parenteral Nutrition (PN)
Also known as non-gastrointestinal introduction of nutrition. It is a method of delivering essential nutrients directly into the bloodstream, bypassing the digestive system. Involves intravenous (IV) administration of a nutrient rich solution containing carbohydrates, proteins, lipids, vitamins, and minerals.
Indications of Parenteral Nutrition
Malnutrition - When oral or enteral intake is insufficient to meet nutritional needs, leading to malnutrition.
Gastrointestinal Disorders -In cases where the gastrointestinal tract is compromised, such as severe inflammatory bowel disease or bowel obstruction. Ex: Diverticulitis and Colitis.
Impaired Absorption - For patients with malabsorption syndromes or short bowel syndrome, preventing adequate nutrient absorption.
Inability to Eat -When patients are unable to eat due to conditions like dysphagia, severe nausea, or anorexia nervosa.
Post-Surgery or Trauma - After certain surgeries or traumatic injuries where oral or enteral intake is contraindicated.
Critical Illness - In critically ill patients in the intensive care unit (ICU) who are unable to receive sufficient nutrition orally.
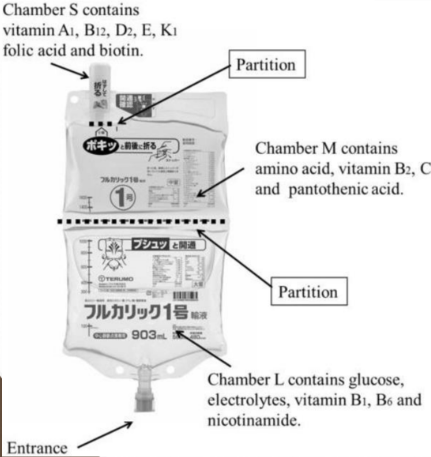
Components of Parenteral Nutrition
A. Macronutrients
Carbohydrates
Proteins
Lipids
B. Micronutrients
Vitamins
Minerals
C. Fluids and Electrolytes
Types Parenteral Nutrition
Total Parenteral Nutrition - is a complete intravenous nutrition solution that provides all essential macronutrients (carbohydrates, proteins, lipids) and micronutrients to meet a patient's total nutritional needs.
Route of Administration: through a central venous catheter, typically placed in large veins such as the superior vena cava.
Rationale: Central venous access ensures rapid dilution and distribution of the nutrient-rich solution, reducing the risk of complications associated with peripheral administration.
Peripheral Parenteral Nutrition (PPN) - is a partial parenteral nutrition solution with a limited nutrient composition compared to TPN. PPN provides a simplified mixture of macronutrients and may lack certain micronutrients, making it suitable for short term nutritional support.
Route of Administration: PPN is administered through a peripheral vein access, commonly in the arm.
Rationale: PPN is used when central venous access is not feasible or when the nutritional requirements are moderate, and the duration of parenteral nutrition is expected to be short-term.
Complications
Bacterial and fungal infections
Liver failure due to excess glucose contained in the solution.
Acute cholecystitis due to complete unuse of gastrointestinal tract
Nursing Responsibilities
Assessment
conduct a comprehensive assessment of the patient's nutritional status, medical history, and current clinical condition to determine the appropriateness of TPN
assess the central venous access site regularly for signs of infection, redness, swelling, or any complications related to catheter insertion.
monitor for complications such as hyperglycemia, electrolyte imbalances, and signs of infections related to TPN administration.
Administration
Participate in the preparation of TPN solutions, ensuring accurate formulation based on the patient's nutritional needs. Double check if the formula is for TPN or PPN because death may occur in misadministration.
Follow strict aseptic technique when accessing and caring for the central venous access used for TPN administration to prevent infections.
Monitor and regulate the TPN infusion rate according to the prescribed schedule, ensuring a gradual initiation and discontinuation to prevent complications
Laboratory Monitoring
Regularly monitor blood glucose levels to ensure glycemic control and promptly address hyperglycemia or hypoglycemia. Adjust if necessary.
Monitor electrolyte levels and adjust TPN components accordingly to maintain a balance of sodium, potassium, calcium, and phosphorus.
Patient Education
Provide thorough education to the patient and family regarding the purpose of TPN, potential complications, and the importance of reporting any adverse effects promptly.
If applicable, provide training and support for patients and caregivers for the administration of TPN at home, ensuring they understand procedures and are capable of managing potential issues.
Safety Measures
Strictly adhere to infection prevention protocols, including proper hand hygiene, use of aseptic technique during central line care, and following facility policies.
Train the patient and caregivers to recognize early signs of complications such as infection, thrombosis, or catheter dislodgement and instruct them to seek immediate medical attention
Documentation
Maintain accurate and timely documentation of TPN administration, including the composition of the solution, infusion rates, and the patient's response.