7. Muscular Tissue NOTES
MUSCULAR SYSTEM
TYPES OF MUSCLE TISSUE
Three Types of Muscle
A. Skeletal Muscle
B. Cardiac Muscle
C. Smooth Muscle
COMPARING THREE TYPES OF MUSCULAR TISSUE
Skeletal Muscle
Location: Attached to bones
Shape: Long cylinder
Nucleus: Multiple, located under sarcolemma
Striations: Striated
Function: Skeletal movement, heat production
Control: Voluntary
Cardiac Muscle
Location: Heart
Shape: Branched
Nucleus: Single, centrally located
Striations: Striated
Function: Pumping action of heart
Control: Involuntary
Smooth Muscle
Location: Lines some Internal organs & walls of blood vessels
Shape: Spindle
Nucleus: Single, centrally located
Striations: No striations
Function: Propels contents of organs, changes diameter of blood vessels
Control: Involuntary
4 FUNCTIONS OF SKELETAL MUSCLE
Movement
Maintaining posture
Stabilizing joints
Generating body heat
ORGANIZATION OF A SKELETAL MUSCLE
Muscle
Muscle Fascicle
Muscle Fiber (Cell) → made up of myofibrils
Myofibril → made up of sarcomeres
Myofilament → thick and thin filaments that make up the sarcomeres
CONNECTIVE TISSUE COVERINGS OF MUSCLE
Epimysium: Covers muscle
Perimysium: Covers fascicle
Endomysium: Covers muscle fiber
4 STRUCTURES OF THE MUSCLE FIBER (CELL)
Sarcolemma - plasma membrane that surrounds it
Sarcoplasm (cytoplasm) - the cytoplasm(fluid) of the muscle fiber/cell, enclosed by the sarcolemma, filled with mitochondria.
Nuclei - Multiple nuclei located under the sarcolemma.
Myofibrils- units that make up the muscle fibers.
3 STRUCTURES OF THE MYOFIBRILS
Sarcoplasmic Reticulum (SR): Network of tubes all around/surrounding each myofibril.
Terminal Cisterns - when the SR enlarges into a pouch. It stores calcium.
Transverse Tubule (T-tubule): Fold/tube coming from the sarcolemma that transmits electrical signals deep into muscle fiber (action potential)
→ Triad: Formed by 2 terminal cisterns on either side of 1 T-tubule.
SARCOMERE
Sarcomeres are what makes up the myofibrils.
Contain two main types of myofilaments Thick and Thin
Functional unit of muscle fiber
→ Z Discs: The Boundaries of a Sarcomere
Z discs are the boundaries of a sarcomere, marking where one sarcomere ends and the next begins.
They only anchor/attached to the thin (actin) filaments and help maintain structure.
When a muscle contracts, sarcomeres shorten as actin and myosin slide past each other, pulling the Z discs closer together.
Where Sarcomeres Fall in the Muscle StructureMuscle → Made of muscle fascicles
Muscle fascicle → Made of muscle fibers (cells)
Muscle fiber → Filled with myofibrils
Myofibrils → Made up of repeating sarcomeres
Sarcomeres → In the Myofibrils and Contain myofilaments (Thick (myosin & Thin (actin) )
ARRANGEMENT OF SARCOMERE
M Line: Middle line of sarcomere
A Band: Contains thick filaments (dark). red thick lines
I Band: Contains thin filaments (light). blue thin lines
BANDS (STRIATIONS) OF SARCOMERE
ONLY Thin filaments are attached to Z discs
A Band (appear in dark striations) contain thick filaments only. RED thick lines
I Band (appear in light striations) contain thin filaments only. BLUE thin lines.
ARRANGEMENT OF MYOFILAMENTS
2 types of myofilaments, THICK & THIN
Six thin filaments surround one thick filament
Thick filaments do not move; thin filaments slide towards the midline when the muscle contracts
MYOFILAMENTS: THICK FILAMENT(myosin)
Composed of myosin proteins
Each myosin molecule head 1 tail and 2 heads.
The actin binding sites are on the 2 heads.
When muscle contraction begins, Actin-Binding sites on myosin heads will attach to actin(on the thin filaments) and form a cross bridge.
Myosin → bind to actin (on thin filaments) Z discs.
MYOFILAMENTS: THIN FILAMENTS(actin)
Composed of three proteins:
Actin : the main protein in thin filaments and serves as the binding site for myosin(on thick filaments) during muscle contraction.
→ Myosin heads attach to actin to form cross-bridges, allowing contraction.
→ Forms the Structure of Thin Filaments : Actin molecules form a twisted chain that makes up the thin filament.
→ Works with Regulatory Proteins : Tropomyosin covers the binding sites when the muscle is relaxed, and troponin moves tropomyosin when calcium is present, allowing contraction.Tropomyosin: long strand of protein that Covers binding sites on actin when muscle is relaxed.
Troponin: Anchors tropomyosin in place, but when ready to contract it binds to calcium and moves/pulls the tropomyosin exposing the binding sites .
CONTROL OF SKELETAL MUSCLE MOVEMENT
Motor Area in the Brain: Sends action potential through neurons
Neurons transmit action potential to skeletal muscle at a synapse.
Motor Unit: a functional unit that connects the nervous system to the muscular system.
→ Consists of 1 somatic motor neuron and all muscle fibers it activates.
Somatic Motor Neuron: This is a nerve cell that sends electrical signals from the brain or spinal cord to the muscle fibers.
ALL Muscle Fibers: These are the cells of the muscle that contract when activated by the motor neurons.
How It Works:
A motor unit consists of one motor neuron and all the muscle fibers it connects to and activates.
When the motor neuron sends a signal, it activates all the muscle fibers in the motor unit, causing them to contract together.
Key Idea:
A motor unit is like a team—the motor neuron is the coach, and the muscle fibers are the players. The coach tells all the players to move at once! 🏆💪
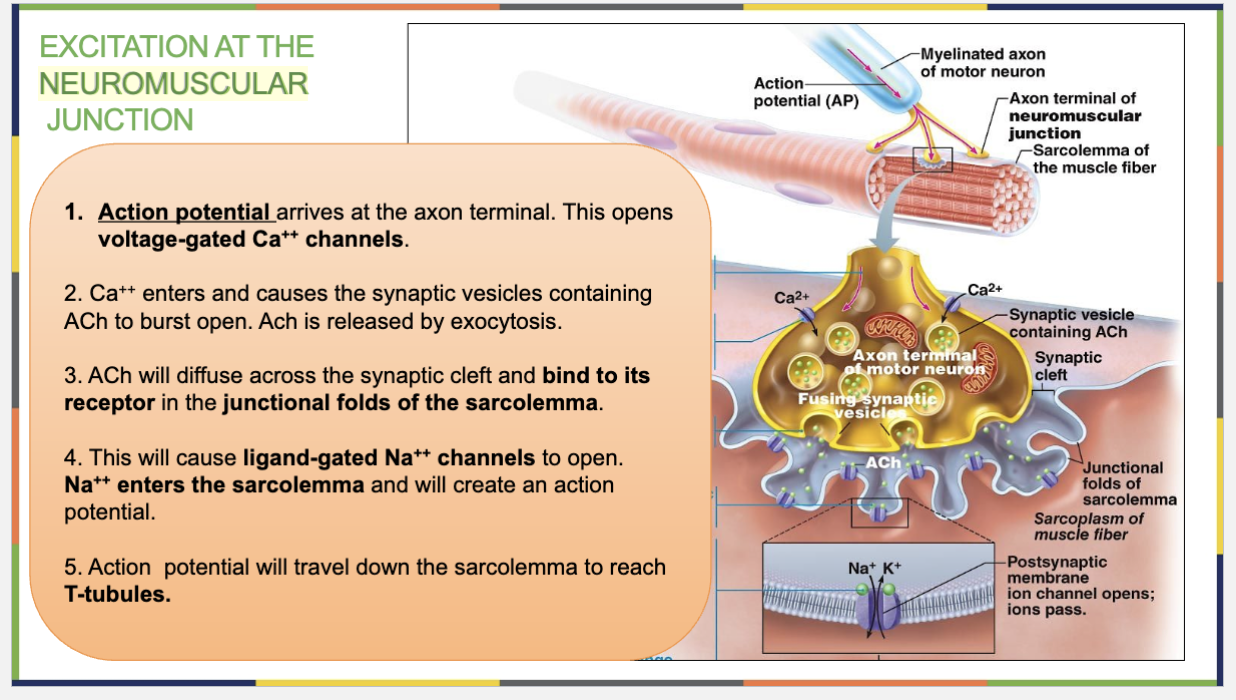
NEUROMUSCULAR JUNCTION
The neuromuscular junction (NMJ) is the connection between a motor neuron and a skeletal muscle fiber, where nerve signals trigger muscle contraction.
Neuromuscular Junction: Contact point between motor neuron and skeletal muscle
STRUCTURES AT NEUROMUSCULAR JUNCTION & Muscle Contraction Steps
→ Structures : Axon terminal , Synaptic knob, Motor end plate(contains the junctional folds) & Synaptic Cleft
Axon Terminal – End of the motor neuron, where it meets a muscle fiber at the neuromuscular junction (NMJ) , releases ACh.
Synaptic Knob: This is the end of the motor neuron where communication with the muscle fiber happens.
→ It contains synaptic vesicles, which are small sacs filled with acetylcholine (ACh)—the neurotransmitter responsible for stimulating muscle contraction.
Functions of synaptic knob
Holds synaptic vesicles filled with acetylcholine (ACh) (a neurotransmitter).
Releases ACh into the synaptic cleft when a nerve signal arrives.
Starts muscle contraction by transmitting the signal to the muscle fiber.
Key differences between Axon terminal & Synaptic knob:
Axon Terminal = The entire end section of the neuron. (Final part of the motor neuron before the NMJ)
Synaptic Knob = The very tip of the axon terminal that stores and releases ACh.
(It Holds synaptic vesicles filled with ACh and releases it into the synaptic cleft)
Motor End-Plate: This is the specialized part of the sarcolemma of the muscle fiber/cell that receives signals from the neuron.
→ It has the junctional folds, which increase surface area and contain ACh receptors to bind acetylcholine.
Synaptic Cleft: This is the space between the synaptic knob and the motor end plate.
→ purpose : acetylcholine (ACh) molecules travel across this gap to reach the muscle cell.
How It Works:
A nerve impulse (action potential) travels down the motor neuron to the synaptic knob.
ACh is released from synaptic vesicles into the synaptic cleft.
ACh binds to receptors on the motor end plate, triggering an electrical signal (action potential) in the muscle fiber.
This signal spreads through the muscle, leading to muscle contraction.
Acetylcholinesterase (ACh) breaks down ACh, stopping the signal and allowing muscle relaxation.
This entire process ensures precise and controlled muscle movement & The NMJ is essential for converting nerve signals into muscle movement, making voluntary movements possible.
Excitation at the Neuromuscular Junction (NMJ) – Easy Breakdown & Memory Trick
→ Sending the signal from the neuron to the muscle, how the nerve tells the muscle to contract
(Excitation → process of activating a muscle fiber, "waking up" the muscle)
Axon terminal → the end of a motor neuron’s axon where it meets a muscle fiber at the neuromuscular junction (NMJ).
Synaptic Knob → is the rounded end of the axon terminal where the motor neuron communicates with the muscle fiber at the neuromuscular junction (NMJ).
Nerve Signal Arrives 🚀
An action potential (electrical signal) reaches the axon terminal of the motor neuron.
This opens voltage-gated Ca²⁺ channels, allowing calcium ions (Ca²⁺) to enter the neuron.
ACh is Released 💥
Calcium ions trigger synaptic vesicles to release acetylcholine (ACh - a neurotransmitter) into the synaptic cleft by exocytosis (vesicle bursting).
ACh Binds to Receptors 🔑
ACh diffuses across the synaptic cleft and binds to ACh receptors that are on the ligand gated Sodium (Na++) Channels. These channels are in the junctional folds of the muscle sarcolemma (motor end plate).
Sodium Channels Open ⚡
The ACh binding opens ligand-gated Sodium (Na⁺) channels.
Sodium (Na⁺) rushes into the muscle fiber, creating a new action potential in the sarcolemma.
Action Potential Spreads 🚦
This new action potential travels down the sarcolemma and into the T-tubules, spreading the signal deep into the muscle fiber.
Memory Trick: "NAASA" 🚀
Nerve Signal Arrives
ACh is Released
ACh Binds to Receptors
Sodium Channels Open
Action Potential Spreads
What is ACH (Acetylcholine) ?
Definition:
Acetylcholine (ACh) is a neurotransmitter (a chemical messenger) that sends signals from nerves to muscles to start contraction.
Where Is It Found?
Stored in synaptic vesicles inside the axon terminal of motor neurons.
Released into the synaptic cleft at the neuromuscular junction (NMJ).
→ Binds to ACh receptors that are on the ligand gated NA++ Channels on the motor end plate in the junctional folds of the muscle.
ACh receptors are protein structures on the sarcolemma (muscle cell membrane) at the motor end plate.
These receptors are linked to ligand-gated Na⁺ channels.
When acetylcholine (ACh) binds to the ACh receptor, it causes the ligand gated Na⁺ channels to open, allowing Na⁺ ions to flow into the muscle fiber, triggering an action potential.
(ACH receptor is on the channels)
Key Idea:
The ACh receptors activate the Na⁺ channels when ACh binds to them, starting the muscle contraction process! 🔑⚡
Function of ACH:
1⃣ Released from the neuron when a nerve signal arrives.
2⃣ Binds to ACh receptors on the muscle, opening Na⁺ channels.
3⃣ Starts an action potential, leading to muscle contraction.
4⃣ Broken down by acetylcholinesterase (AChE) to stop the signal.
Key Idea:
ACh is like a “go” signal that tells muscles to contract! 🚦⚡💪
EXCITATION-CONTRACTION COUPLING
→ how a nerve signal turns into a muscle contraction, turning the signal into movement
( the process that links the electrical signal (excitation) to muscle contraction. It describes how an action potential in the muscle fiber triggers the release of calcium ions (Ca²⁺), leading to muscle contraction )
ACTA
Action potential travels down T-tubule, releasing Ca++ from terminal cisterns
Ca++ binds to troponin
Troponin pulls tropomyosin, exposing myosin-binding sites
A cross-bridge forms between actin and the myosin heads. The heads will do a “power-stroke” causing the thin filaments to slide inwards. (thick filaments don’t move)
Difference Between Excitation at the NMJ & Excitation-Contraction Coupling
Term | Excitation at the Neuromuscular Junction (NMJ) | Excitation-Contraction Coupling |
|---|---|---|
Definition | How a nerve signal reaches the muscle | How the nerve signal triggers muscle contraction |
Focus | Sending the signal from the neuron to the muscle | Turning the signal into movement |
Key Idea | Muscle gets the message 💡 | Muscle actually moves 💪 |
Easy Trick to remember excitation at NMJ & Excitation-Contraction couplin:
Excitation at NMJ = “Hey muscle, wake up!” 🗣⚡
Excitation-Contraction Coupling = “Hey muscle you’re awake, it’s time to move!” 🏃💪
ROLE OF CALCIUM IN SLIDING FILAMENT MECHANISM
(occurs at thin filament)
Calcium binds to troponin : Ca²⁺ is released from the sarcoplasmic reticulum (SR) and binds to troponin on the thin filament.
Exposure of Myosin-Binding Sites : Troponin pulls tropomyosin away so that the myosin binding sites on actin are exposed.
Cross-Bridge Formation & Power Stroke: Myosin heads attach to actin, forming cross-bridges. Myosin pulls actin inward using a power stroke, shortening the sarcomere.
Sarcomere shortens creating muscle contraction: Thin filaments slide inward toward the M line.
Z discs move closer together, I band shrinks, while A band stays the same width.
ROLE OF ATP IN MUSCLE CONTRACTION
1 ATP will help the myosin head to attach and form the cross bridge. it will enable the myosin head to bend and pull on actin.
1 new ATP causes the cross bridge to detach, allowing process to repeat.
(1 ATP to attach + 1 To detach → this process repeats)
RELAXATION OF A MUSCLE FIBER
Cessation(end) of action potential down the motor neuron, stopping ACh release
Acetylcholine-esterase enzyme removes ACh from synaptic cleft.
Ca++ reabsorbed back into terminal cisterns
Troponin moves back to its position
Tropomyosin moves back to blocking myosin-binding sites.
Cross bridges detach, thin filaments slides back outwards and the muscle elnogates back to its original length.
MUSCLE TWITCH
Myogram: Recording of muscle contraction
Phases of Muscle Twitch:
Latent Period: Action potential propagated along the sarcolemma (stimuli is given, everything before cross bridges)
Contraction Phase: Ca++ binds to troponin, tropomyosin moves away exposing myosin-binding sites, cross-bridges form, and sarcomeres
shorten.
Relaxation Phase: Ca++ reabsorbed back into the SR and crossbridges gradually detach, & muscle returns to original length.
WAVE (TEMPORAL) SUMMATION
(3 examples of muscle contraction patterns)
when the second contraction starts before the muscle has fully relaxed.
Some cross bridges are still not yet detached
it will release more calcium and result in more cross bridges and so a stronger muscle contraction.
TETANUS
When the stimulus frequency is so high that the relaxation phase disappears completely, resulting in continuous sustained contractions.
TREPPE
Gradual increase in muscle tension resembling a staircase pattern, basis for warm-up
Difference Between Wave Summation & Treppe
Feature | Wave Summation | Treppe |
|---|---|---|
Definition | When a second stimulus occurs before the muscle fully relaxes, increasing force. | When repeated stimuli at the same strength cause a gradual increase in contraction force. |
Cause | Due to overlapping contractions (muscle is already partially contracted). | Due to increased muscle efficiency (warmer temperature, more available Ca²⁺). |
Effect on Force | Stronger contractions than the first, without full relaxation. | Step-like increase in contraction strength with each stimulus. |
Also Called | Temporal summation | Staircase effect |
Key Idea:
Wave summation = stacking contractions → stronger force 💪📈
Treppe = gradual warm-up effect → better efficiency 🚶♂➡🏃♂
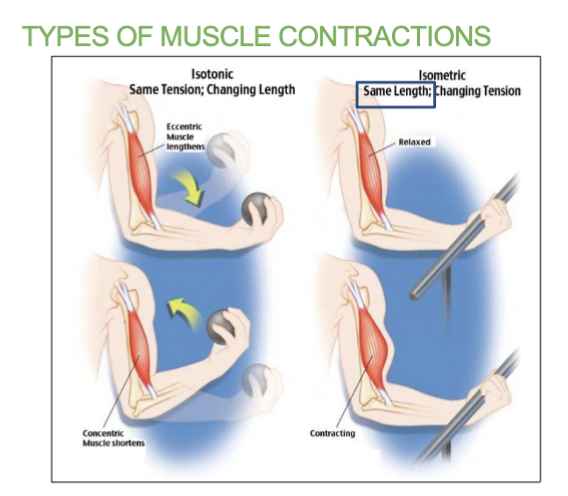
TYPES OF MUSCLE CONTRACTIONS
Isotonic contraction - Muscle length shortens to move load
Isometric contraction - muscle length does not change because the load exceeds the tension the muscle can generate.
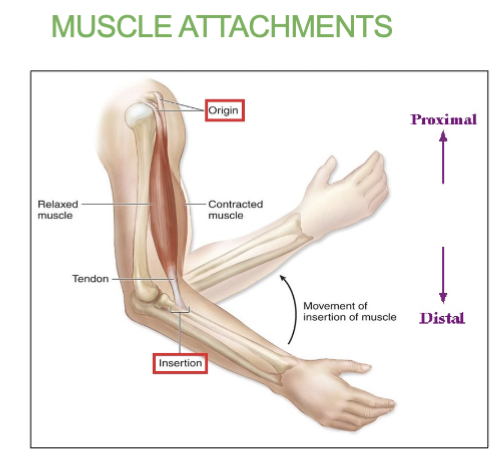
MUSCLE ATTACHMENTS
Origin - less movable attachment and is more proximal in limbs
Insertion - more movable and more distal (away from body). During contraction, the insertion will move closer to origin.
4 PATHWAYS FOR REGENERATING ATP DURING MUSCLE ACTIVITY
Stored ATP
Creating Phosphate - Creating ATP from phosphate, lasts for about 15 secs.
Anaerobic pathways - Using sugar/glucose for ATP , lasts between 30-40 seconds
Aerobic pathway - Oxygen is used to create ATP, can last hours.
—
Short-duration Exercise:
Anaerobic pathway using creatine phosphate (15 seconds)
Prolonged-duration Exercise:
Aerobic pathway using glucose and oxygen (30 minutes)
1. Creatine Phosphate
Provides immediate ATP for 15 seconds:
CP + ADP → Creatine + ATP
2. Anaerobic Pathway
Utilizes glucose through glycolysis
Energy provided for 30-40 seconds:
1 Glucose → 2 Pyruvic acid + 2 ATP
3. Aerobic Pathway
Utilizes glucose and oxygen for 32 ATP (30 minutes)
Glucose + O2 → CO2 + H2O + ATP
After 30 minutes, fatty acids and amino acids provide energy for hours.