3.5 Cardiac Electrophysiology cycle
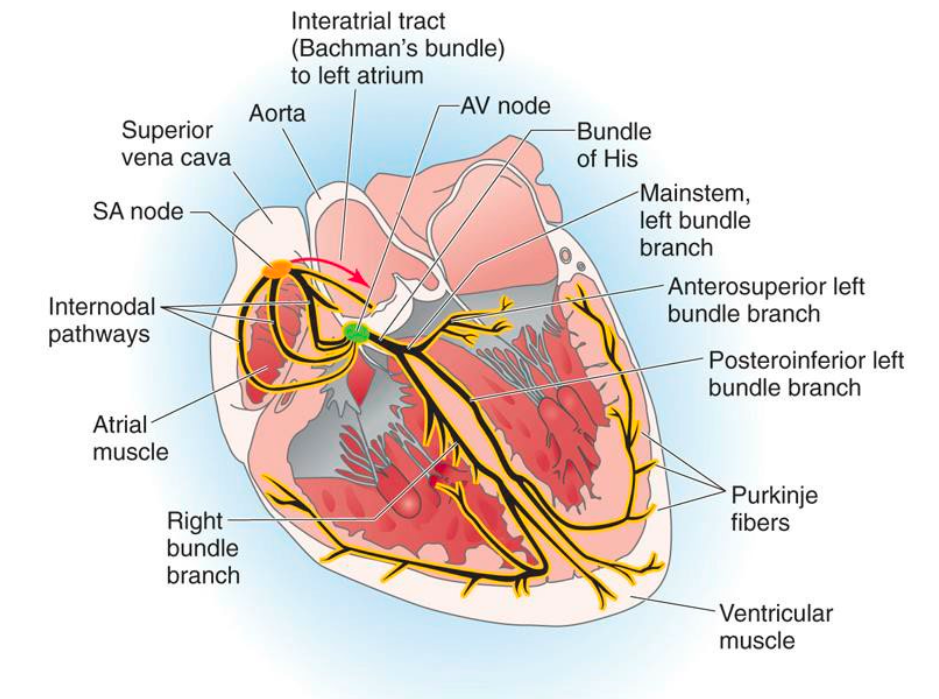
The conduction system of the heart
Major Structures
Sinu-atrial node
Localised in the right atrium near the entry of the superior vena cava
Atrioventricular bundle (bundle of his)
Normally found distal to the AV node next ti the tricuspid valve in the atria
Atrioventricular node
Localised in the right atrium just above the fibrous tissue ring (cardiac skeleton) that separates and isolates atria from ventricles
Right & Left bundle branch
The bundle branches run under the endocardium (subendocardial) of the interventricular septum towards the apex of the heart
Purkinje fibres
They run subendocardial and “deliver” the excitation to the cardiomyocytes
How does it work
All parts of the conduction system are able to generate action potentials without being stimulated.
The SA node has the ability to generate 60-100 action potentials per minute.
Therefore, before the others (AV node, His-bundle, etc.) can generate action potentials by themselves, they are activated by the action potentials from the SA node.
The ion channels on cells determine what happens during an action potential.
Generation of action potentials
The special set of ion channels determines the spontaneous generation of action potentials.
The pacemaker current is essential for this process.
It slowly increases the membrane potential from the usual -70 to -60 mV to more positive values until the potential reaches the threshold, at which point the action potential starts
Ions Channels
Slow entry of Na+ leads to a more positive membrane potential, causing depolarization.
Transient Ca2+ channels (T-type) open, further increasing the membrane potential and contributing to depolarization.
Long-lasting Ca2+ channels (L-type) then open, causing additional depolarization by making the membrane potential even more positive.
This series of events culminates in the action potential.
Following depolarization, K+ channels open which allows K+ to exit the cell, leading to a more negative membrane potential and resulting in hyperpolarization.
Depolarisation of the cells
Depolarization of the cells of the SA node initiates cardiac contraction.
Atrial cardiomyocytes, connected to the SA node via gap junctions, depolarize and contract following the SA node stimulation.
The depolarization generated in the SA node then reaches the AV node.
This depolarization is quickly transported via the His-Purkinje system to the ventricular cardiomyocytes.
The depolarization spreads from the apex of the heart to the base.
It propagates from the endocardium to the epicardium.
Difference between action potentials of the SA node cells and cardiomyocytes of the atria and ventricles
The cardiomyocytes that have the job to contract need more calcium influx and release to conduct the excitation-contraction coupling using microfilaments
Automatic control of the heart
Pacemaker Activity:
The SA node functions as the primary pacemaker of the heart, setting the rate and rhythm of the heart's contractions. Its automaticity ensures that it can initiate action potentials independently, thus controlling the heart rate based on the body's needs.
Influences on Heart Rate:
The autonomic nervous system (ANS) plays a crucial role in modulating heart rate. It consists of two branches:
Sympathetic Nervous System: Increases heart rate and contractility through the release of norepinephrine, enhancing conduction through the AV node and around the heart.
Parasympathetic Nervous System: Decreases heart rate via the vagus nerve, primarily affecting the SA node to slow down the firing rate.
Hormonal Control:
Hormones such as adrenaline (epinephrine) released from the adrenal glands during stress can enhance heart rate and force of contraction, reinforcing the effects of the sympathetic nervous system.
Physiological Mechanisms:
The conduction system, including the SA node, AV node, and Purkinje fibers, ensures impulses are generated and transmitted in a coordinated manner. This organization facilitates timely contractions of the atria followed by those of the ventricles.
The interaction of calcium ions during action potential generation and cardiac muscle contraction is critical for the automatic control of the heart. Calcium influx triggers contraction, while its removal leads to relaxation, influencing heartbeat consistency.
Feedback Mechanisms:
The baroreceptors and chemoreceptors in the cardiovascular system monitor blood pressure and blood chemistry changes. This information is relayed to the central nervous system, which adjusts heart rate and contractility accordingly to maintain homeostasis.
Autonomic nervous systems
Sympathetic Nervous System:
Often referred to as the "fight or flight" system, the sympathetic nervous system prepares the body for stressful or emergency situations. When activated, it increases heart rate, dilates airways, and inhibits digestive activities, preparing the body for immediate action. It achieves these effects primarily through the release of norepinephrine and other stress hormones.
Consist of Spinal cord, preganglionic fibres, sympathetic chains, postganglionic fibres, noradrenaline (norepinephrine)
It activates β1 and β2 receptors
Increases the CA2+currents and the If currents causing faster depolarisation
Parasympathetic Nervous System:
Known as the "rest and digest" system, the parasympathetic nervous system promotes relaxation and conservation of energy. It slows down heart rate, enhances digestion, and facilitates recovery processes in the body. The effects are primarily mediated through the vagus nerve, which releases acetylcholine to calm the body after stressful situations.
Consist of the Brainstem, vagal nuclei, preganglionic fibres, cardiac ganglion, postganglionic fibres acetylcholine
Activates muscarinic M2 receptors
a type of acetylcholine receptor that are part of the parasympathetic nervous system
Increases the K+ currents and causes hyperpolarisation and slows the depolarisation
Cardiac function
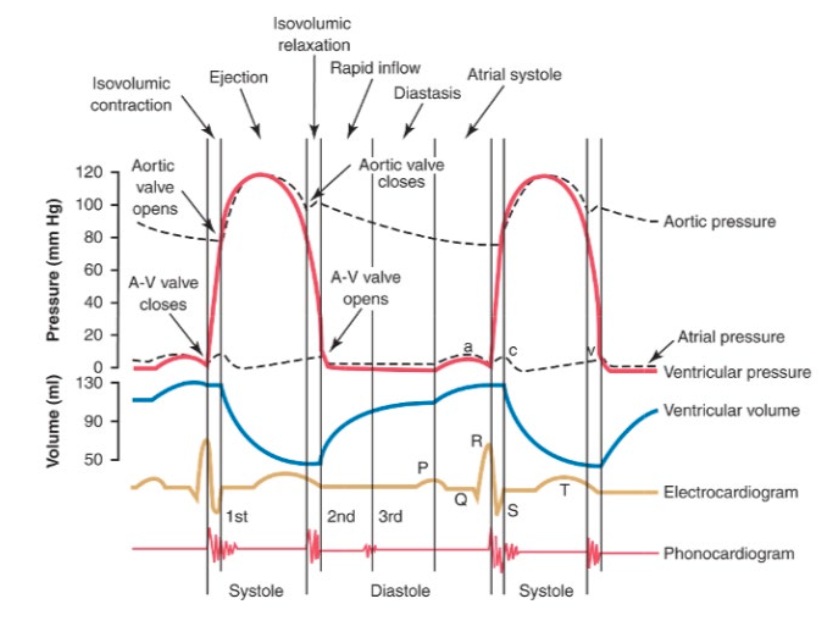
Blood flow through cardiac cycle
Diastole (Relaxation Phase):
The heart is at rest; blood fills the chambers.
Atria fill with blood returning from the systemic circulation via the superior and inferior vena cavae into the right atrium, and from the pulmonary veins into the left atrium.
The AV valves (tricuspid and mitral valves) open, allowing blood to flow passively from the atria into the ventricles.
Systole (Contraction Phase):
The ventricles begin to contract, pushing blood out of the heart.
The tricuspid valve closes to prevent backflow into the atria.
Blood is pumped from the right ventricle into the pulmonary artery (to the lungs for oxygenation) and from the left ventricle into the aorta (to deliver oxygenated blood to the body).
The semilunar valves (pulmonary and aortic valves) open during ventricular contraction and close when the ventricles relax, ensuring proper blood flow direction.
Phases of the cardiac cycle
During diastole
Isovolumetric relaxation
Rapid inflow into ventricles
Diastsis
Atrial contration
During systole
Isovolumetric contraction
Rapid ventricular ejection
Reduced ventricular ejection
These seven specific phases make up the cardiac cycle
Cardiac output Vs Stroke volume
Cardiac output
Blood ejected from the left ventricle each minute
Stroke volume
Blood ejected from the left ventricle with each cardiac cycle
Preload and Afterload
Preload
Refers to the initial stretching of the cardiomyocytes before contraction; effectively the volume of blood in the ventricles at the end of diastole.
It determines the amount of blood that fills the heart and influences stroke volume through the Frank-Starling mechanism.
Influenced by venous return; higher venous return increases preload, which can enhance cardiac output.
Afterload
Refers to the resistance the heart must overcome to eject blood during systole.
It is determined by the pressure in the blood vessels that the ventricles must pump against (i.e., systemic vascular resistance).
An increased afterload (e.g., due to high blood pressure) can decrease stroke volume as the heart has to work harder to eject the stroke volume.
Control of cardiac output
Most healthy individuals have capacity to increase theri cardiac output 4-6 folds such as during exercise
Ways to Achieve Increased Cardiac Output:
Intrinsic Cardiac Regulation of Output:
Primarily achieved via the Frank-Starling Mechanism, which posits that the greater the return of venous blood to the heart, the greater the subsequent output that can be achieved.
Changes in Heart Rate:
Controlled by the autonomic nervous system, which modulates heart rate to match the body's needs.
Bainbridge Reflex:
A reflex that stimulates an increase in heart rate in response to increased atrial stretch due to higher venous return.