Lecture 12: Alteration of renal and urinary tract function
alterations of renal and urinary tract function:
renal and urinary tract function can be altered by a variety of disorders
infection of bladder (the most common type)
disorders within kidney
other systemic disease
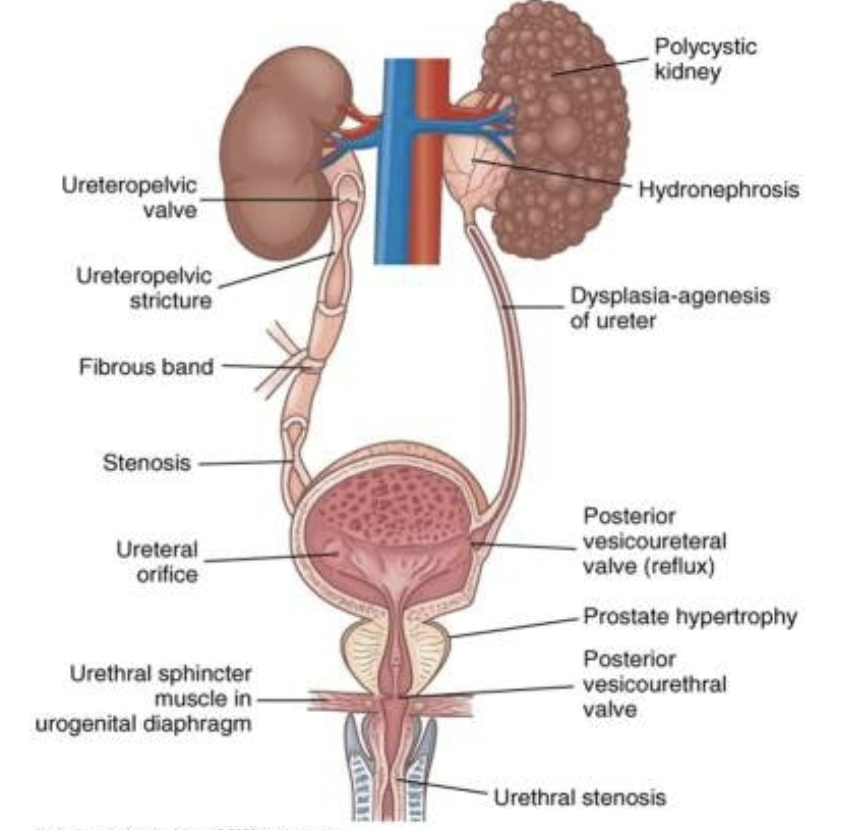
urinary tract obstruction:
a urinary tract obstruction is defined as a blockage of urine flow within the urinary tract
the obstruction can be caused by a anatomic or functional defect (called obstructive uropathy)
regardless of cause the consequence is blockage that leads to
urinary stasis
dilates the urinary system
increases the risk for function
severity of obstructive uropathy is based on
location
completeness
involvement of one or both upper urinary tracts
duration
cause
complete blockage causes
hydroureter (dilation of the ureter)
hydronephrosis (dilation of the renal pelvis and calyces)
dilation leads to
tubulointerstitial fibrosis is the deposition of excessive amount of extracellular matrix
apoptosis
tubulointerstitial fibrosis and apoptosis result detectable damage between 7-14 after obstruction
partial blockage produces less damage
compensatory hypertrophy is essential to recovery of renal function after an obstruction has occurred
obligatory growth- growth of nephrons under influence of human growth hormone
compensatory growth- growth of nephrons under influence of unidentified hormone
postobstructive diuresis- rapid excretion of urine (10 l) in 24 hrs
can cause dehydration, electrolyte imbalance
low bladder wall compliance- create pressure within bladder that reduces or blacks the urine transport
upper urinary tract obstruction:
kidney stones
calculi or urinary stones
masses of crystals, protein, or other substances that form within and may obstruct the urinary tract
risk factors
gender, race, geographic location, seasonal factors, fluid intake, diet, and occupation
kidney stones are classifies according to the minerals comprising the stones
kidney stones:
three factors are required before a stone is formed
supersaturation of one or more salts in urine
presence of a salt in a higher concentration than the volume able to dissolve the salt
precipitation of a salt from liquid to solid state
temperature and ph of urine influence the risk of precipitation (alkaline ph increases formation of calcium phosphate stones and acidic ph increase formation of uric acid stone)
growth into a stone via crystallization or aggregation
acute unilateral renal obstruction predispose people to hypertension because
the reduced perfusion of the affected kidney activates the renin angiotensin aldosterone system, which causes constriction of peripheral arterioles
other factors affecting stone formation
crystal growth inhibiting substances such as
pyrophosphate, potassium citrate, and magnesium
particle retention
matrix- organic material contained in a urinary calculus
stones
calcium oxalate or calcium phosphate is the most common type of renal stone
hypercalciuria is usually atttributable to: hyperthyroidism, intestinal hyperabsorption of dietary calcium, bone demineralization caused by prolonged immobilization
struvite stones
are more common in women than men
they grow large and branch into a staghorn configuration in renal pelvis and calyces
they are closely associated with urinary tract infections caused by urease producing bacteria, such as pseudomonas
cystinuric stones
uric acid stones
manifestation
renal colic
evaluation
clinical symptoms and history
imaging and functional studies
urinalysis (ex. ph)
stone analysis
intravenous pyelogram
spiral abdominal ct
treatment
stone removal
lower urinary tract obstruction:
obstruction of lower urinary tract (lut) affects the entire urinary system
obstruction of lut can be caused by
bladder neck dyssynergia- occurs when the smooth muscle of the urethrovesical junction fails to funnel
prostate enlargements- causes obstruction of urethra
urethral stricture- a scare that narrows urethral lumen
severe pelvic organ prolapse- in women causes bladder outlet obstruction
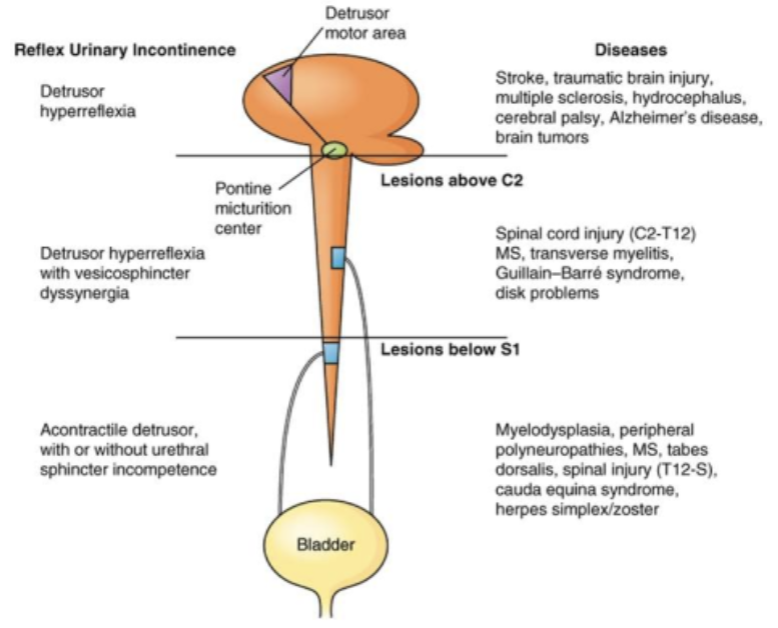
neurogenic bladder- disrupts normal bladder filling and emptying
spinal cord injury is more likely to cause functional obstruction of the bladder outlet in addition to neurogenic detrusor overactivity
caused by lesion of the brain, spinal cord or peripheral nervous system
lesion affecting the brain produces neurogenic detrus overactivity without sphincter dyssynergia
pons regulate and coordinates the detrusor and urethral sphincter muscles during micturition
lesion affecting the spinal cord (c2-s1) produces neurogenic detrus overactivity and sphincter dyssynergia (lack of coordination)
low bladder wall compliance
diagnosis: clinical symptoms (ex. urination more than every two hour during day, awakening urination 3-4 times, perception of incomplete bladder emptying) (bc the obstruction causes the bladder to be unable to empty properly)
treatment: prolapse would need constructive surgery, bladder neck (consist of circular muscles and adrenergic innervation) need alfa adrenergic blocking medications
tumors:
renal tumors
renal adenomas- usually located near the cortex of the kidney
renal cell carcinoma- arises from proximal tubule epithelial cells
bladder tumors
bladder cancer is associated with mutation of the p53 gene
papillary tumors
nonpapillary tumors
urinary tract infection (uti):
uti is inflammation of the urinary epithelium following invasion and colonization by some pathogen within the urinary tract
complicated uti- occurs in an individual with defects of the urinary system
uncomplicated uti- occurs in an individual without defects of the urinary system
persistent uti- ongoing infection despite at least 3 days of treatment
clinical manifestations of a urinary tract infection (of a patient who is 85 yrs old) would be: confusion and poorly localized abdominal discomfort
uti is commonly caused by bacteria, but fungi and protista could also cause uti
most common bacterial pathogens
escherichia coli (the most common causes of uncomplicated urinary tract infections)
staphylococcus saprophyticus
enterobacter spp
virulence of uropathogens- is a potential pathogens ability to evade the host defense mechanisms and cause infection
host defense mechanisms- ex. high urea in the urine is bacteriostatic
cystitis
cystits is an inflammation of the bladder
manifestations
frequency, dysuria, urgency, and lower abdominal and/or suprapubic pain
treatment
antimicrobial therapy, increased fluid intake, avoidance of bladder irritants, and urinary analgesics
pyelonephritis
chilical manifestation: flank pain
pyelonephritis is usually caused by antibody coated bacteria
acute pyelonephritis
acute infection of the ureter, renal pelvis, and/or renal parenchyma
chronic pyelonephritis
persistent or recurring episodes of acute pyelonephritis
risk of chronic pyelonephritis increases in individuals with renal infections and some type of obstructive pathologic condition
glomerular disorgers:
the glomerulopathies are disorders that directly affect the glomerulus
low serum complement is found in glomerular disorders
membranous glomerular lesion is characterized by thickening of the glomerular wall with immune deposition of immunoglobulin g (igg) and c3
glomerular disease demonstrates a sudden or insidious onset of hypertension, edema, and an elevated blood urea nitrogen (bua)
decreased glomerular filtration rate
elevated plasma creatinine, urea, and reduced creatinine clearance
glomerular damage causes a decreased glomerular membrane surface area, glomerular capillary blood flow, and blood hydrostatic pressure
increased glomerular capillary permeability and loss of negative ionic charge barrier result in passage of plasma proteins into the urine
resulting hypoalbuminemia encourages plasma fluid to move into the interstitial spaces
edema
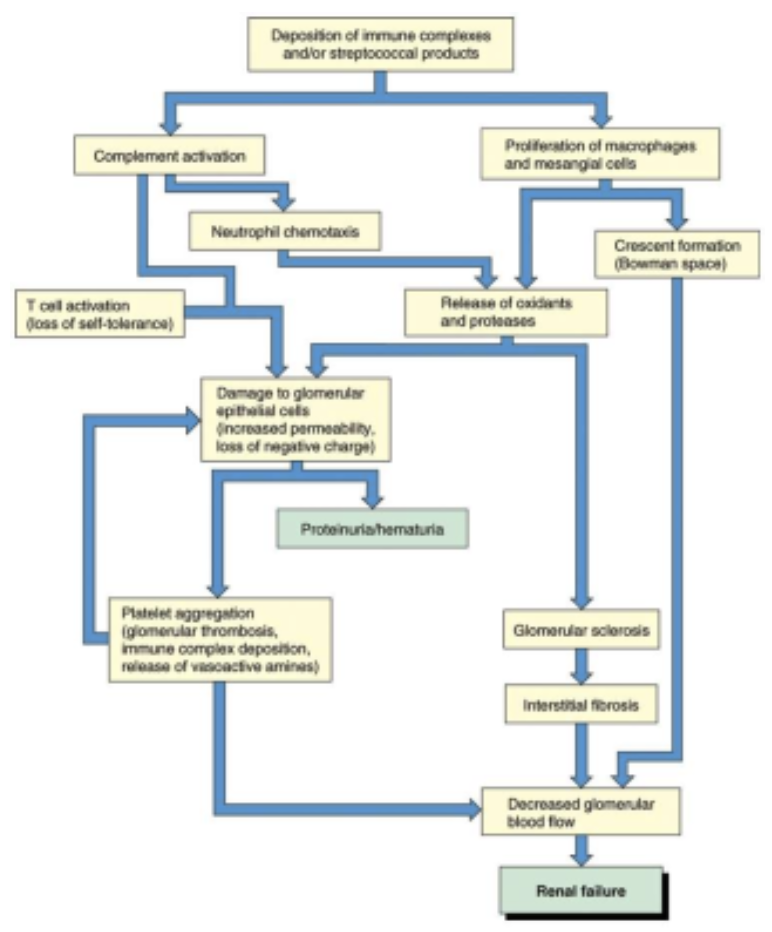
glomerulonephritis
inflammation of the glomerulus
immunologic abnormalities (most common)
drugs or toxins
vascular disorders
systemic diseases
viral causes
glomerulonephritis:
mechanisms of injury
deposition of circulating soluble antigen antibody complexes, often with complement fragments
in glomerulonephritis, the glomerular cell walls damages by lysis from complement
formation of antibodies against the glomerular basement membrane
strepococcal release of neuroamidase
a patient has hematuria with red blood cell casts and proteinuria exceeding 3 to 5 g/day with albumin as the major protein (no clue what this is doing here or what its trying to say)
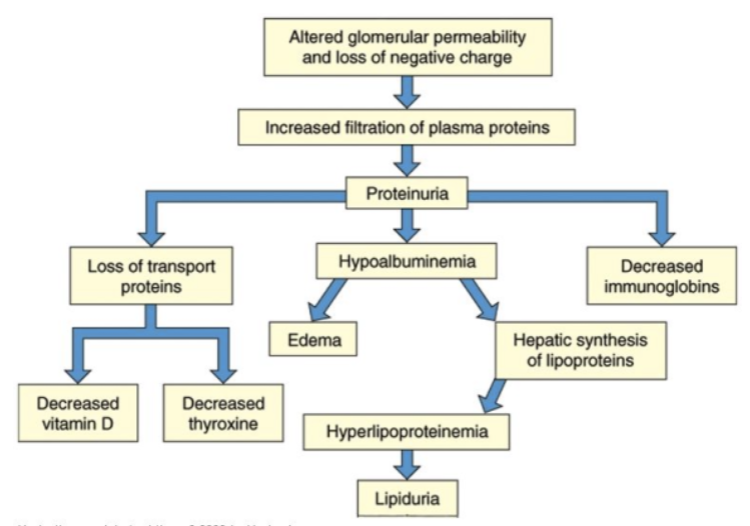
nephrotic syndrome:
excretion of 3.5 g or more of protein in the urine per day
the protein excretion is due to glomerular injury
nephrotic syndrome is characterized by
hypoalbuminemia, edema, hyperlipidemia, and lipiduria
proteinuria causes edema- loss of plasma albumin decreases the plasma oncotic pressure, which normally holds water in the capillaries
renal dysfunction:
decreased renal function is caused by:
renal insufficiency- decline in renal function (loss of about 25%)
renal failure- significant loss of renal function
end stage renal failure- when less than 10% of renal function remains
uremia- renal failure and elevated blood urea and creatinine levels
azotemia- increase serum level caused by renal insufficiency or renal failure
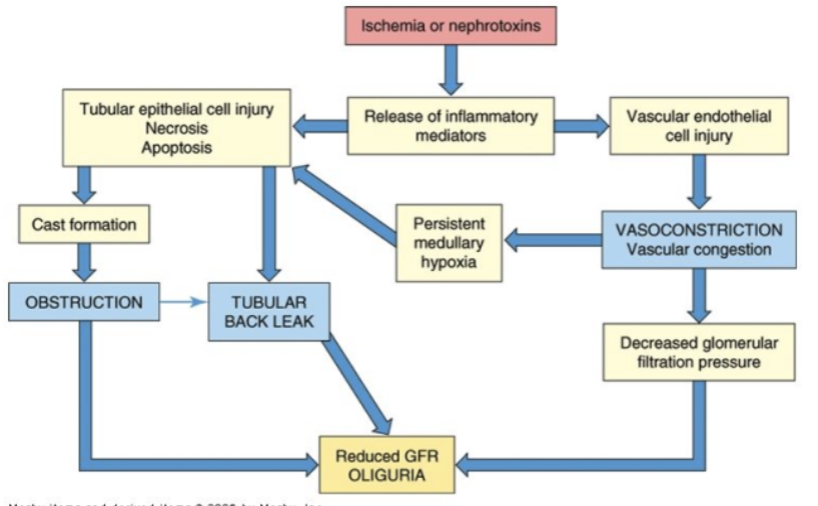
acute renal failure (arf):
prerenal acute renal failure is the most common cause of arf and is caused by impaired renal blood flow
gfr declines due to the decrease in filtration pressure
intrarenal acute renal failure
acute tubular necrosis (atn) is the most common cause of intrarenal renal failure
characteristics of acute tubular necrosis (atn) is urine sodium >30 mEq/L
postrenal acute renal failure
occurs with urinary tract obstructions that affect the kidneys bilaterally
manifestation
initiation phase- the phase of reduced perfusion or toxicity that leads to renal injury
maintenance phase- the period of established renal injury
recovery phase- the renal injury is being repaired
glucose and insulin used to hyperkalemia associated with acute renal failure
when insulin transports glucose into the cell, it also carries potassium with it
anemia of renal failure can be successfully treated with erythropoietin
chronic renal failure:
chronic renal failure is the irreversible loss of renal function that affects nearly all organ systems
progression
reduced renal reserve
renal insufficiency
renal failure
end stage renal disease
chronic renal failure affects
creatinine and urea clearance
creatinine is constantly released from muscle tissue and excreted primarily by glomerular filtration
sodium and water balance
phosphate and calcium balance- metabolism of calcium and phosphate is mediated by parathyroid hormone (pth) and vitamin d
potassium balance- potassium excretion is related to distal tubular secretion mediated by aldosterone
acid base balance
skeletal and bone alteration
when the glomerular filtration (gfr) declines to 25% of normal
parathyroid hormone (pth) is no longer effective in maintaining serum phosphate levels
there is impaired synthesis of 1,25-vitamin d3, which reduces intestinal absorption of calcium, and effectiveness of calcium and phosphate resorption from bone by parathyroid hormone
cardiopulmonary system
neural function
endocrine and reproduction
hematologic alterations