Chapter 17 - Endocrine Notes
Chapter 17 Overview: Endocrine System
Introduction to the Endocrine System
Composed of ductless glands
Synthesize and secrete hormones
Hormones released into the bloodstream affect target cells with specific receptors
Transport process:
Hormones enter interstitial fluid, then blood
Bind to target cell receptors to exert effects
Comparison: Endocrine and Nervous Systems
Both systems release ligands (chemical messengers)
Differences:
Endocrine:
Transmits hormones through the blood
Targets any cell with correct receptors
Widespread effects
Longer reaction times
Longer-lasting effects (minutes to weeks)
Nervous:
Uses neurotransmitters for communication
Targets specific cells
Faster response
Short-lived effects
General Functions of the Endocrine System
Development and Metabolism Regulation
Hormones influence embryonic cell division and differentiation
Regulate metabolic processes (anabolism and catabolism)
Homeostasis Maintenance
Regulate blood composition, volume, and solute concentrations (e.g., glucose, ions)
Digestive Control
Influence secretory processes and movement within the digestive tract
Reproductive Control
Affect reproductive system development and functions, sexual behavior
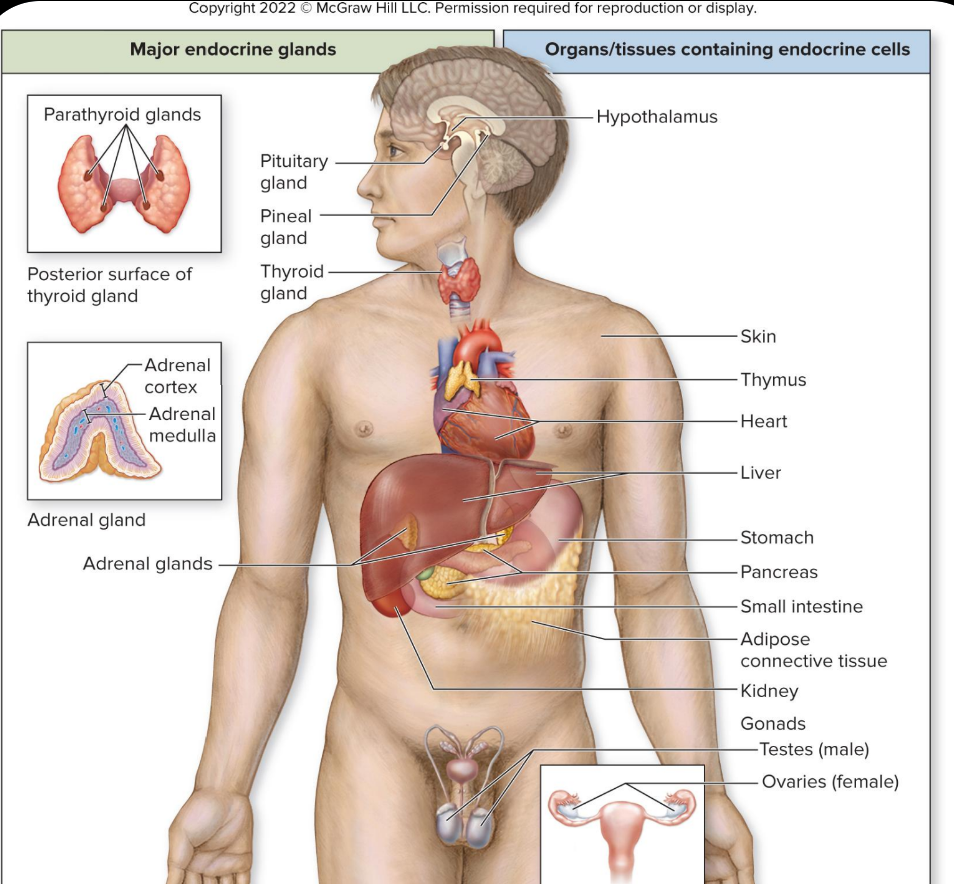
Major Endocrine Glands and Their Functions
Endocrine glands primarily responsible for hormone production:
Pituitary Gland
Pineal Gland
Thyroid and Parathyroid Glands
Adrenal Glands
Glands with endocrine functions within other organs:
Hypothalamus, skin, thymus, heart, liver, stomach, pancreas, kidneys, gonads
Types of Hormone Release Stimuli
Hormonal Stimulation: Hormones triggering other hormone release (e.g., ACTH stimulating cortisol release) Metabolism increases
Humoral Stimulation: Changes in blood nutrient/ion levels triggering hormone release (e.g., increased blood glucose level stimulates insulin)
Nervous System Stimulation: Neuronal stimulation of hormone release (e.g., adrenal medulla releasing epinephrine)
Chemistry of Hormones
Amino Acid-Based Hormones
Includes amines, peptides, and proteins (Lipids cannot enter cells unless bound to a transport protein). These hormones typically exert their effects through second messenger systems, activating specific receptors on the cell surface.
Primarily water-soluble except for thyroxine (thyroid hormone)
Must utilize second messenger systems to exert effects
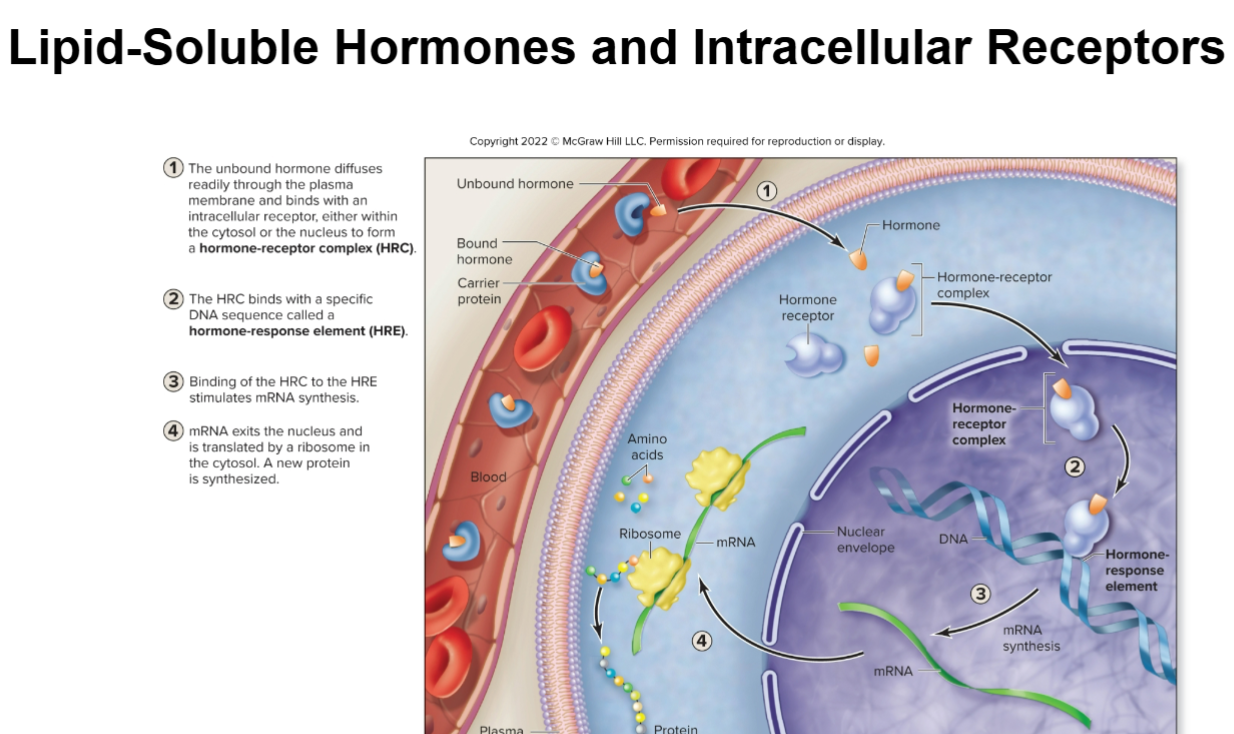
Steroid Hormones
Synthesized from cholesterol (lipid-soluble)
Includes sex hormones and corticosteroids
Can directly activate gene transcription by entering cell and binding to receptors in the cytoplasm or nucleus ( they can cruise into wherever they want to) no need for 2nd messenger system.
Circulating Hormones
Steroids: Lipid-soluble, require carrier proteins for transport
Biogenic Amines: Primarily water-soluble, derived from modifying amino acids
Proteins: Water-soluble chains of amino acids, include most hormones. Polar in nature, these hormones can easily dissolve in the bloodstream and interact with target cells through specific receptors.
Local Hormones vs. Circulating Hormones
Local: Act on the same or nearby cells (e.g., prostaglandins, interleukins)
Circulating: Released into the bloodstream and affect distant target organs
Autocrine vs. Paracrine Stimulation
Autocrine Stimulation: Hormone acts on the same cell that produced it. Example: Immune cells releasing cytokines affecting themselves.
Paracrine Stimulation: Hormone acts on nearby cells. Example: Prostaglandins influencing adjacent cells during inflammation.
Eicosanoids - are a group of local hormones derived from fatty acids, which play critical roles in inflammation, immune response, and cellular signaling.
Prostaglandins: Promote vasodilation and inflammation.
Thromboxanes: Induce vasoconstriction and stimulate blood clotting.
Leukotrienes: Constrict smooth muscle in airways, Promote secretion of mucus, Activate inflammation.
Target Cell Reaction to Hormones
The effect varies by the number of receptors and interaction with other hormones
Up-regulation: Increased receptor number in response to low hormone levels. Example is : Insulin, which leads to an increase in insulin receptors on target cells when glucose levels are consistently low.
Down-regulation: Decreased receptor number in response to high hormone levels Example is : Cortisol, which causes a reduction in the number of glucocorticoid receptors on target cells when cortisol levels are persistently elevated.
Summary of G Protein Activation
Hormone Binding: A hormone (ligand) binds to a G protein-coupled receptor (GPCR) on the cell surface.
Receptor Conformational Change: The binding of the hormone causes a conformational change in the GPCR.
G Protein Activation: This change activates an associated G protein by facilitating the exchange of GDP for GTP on its alpha subunit.
Dissociation: The activated G protein (with GTP) dissociates from the receptor and splits into two parts: the GTP-bound alpha subunit and the beta-gamma dimer.
Signal Transduction: The active alpha subunit (or beta-gamma dimer) then interacts with downstream effector proteins (like enzymes or ion channels), leading to a cellular response.
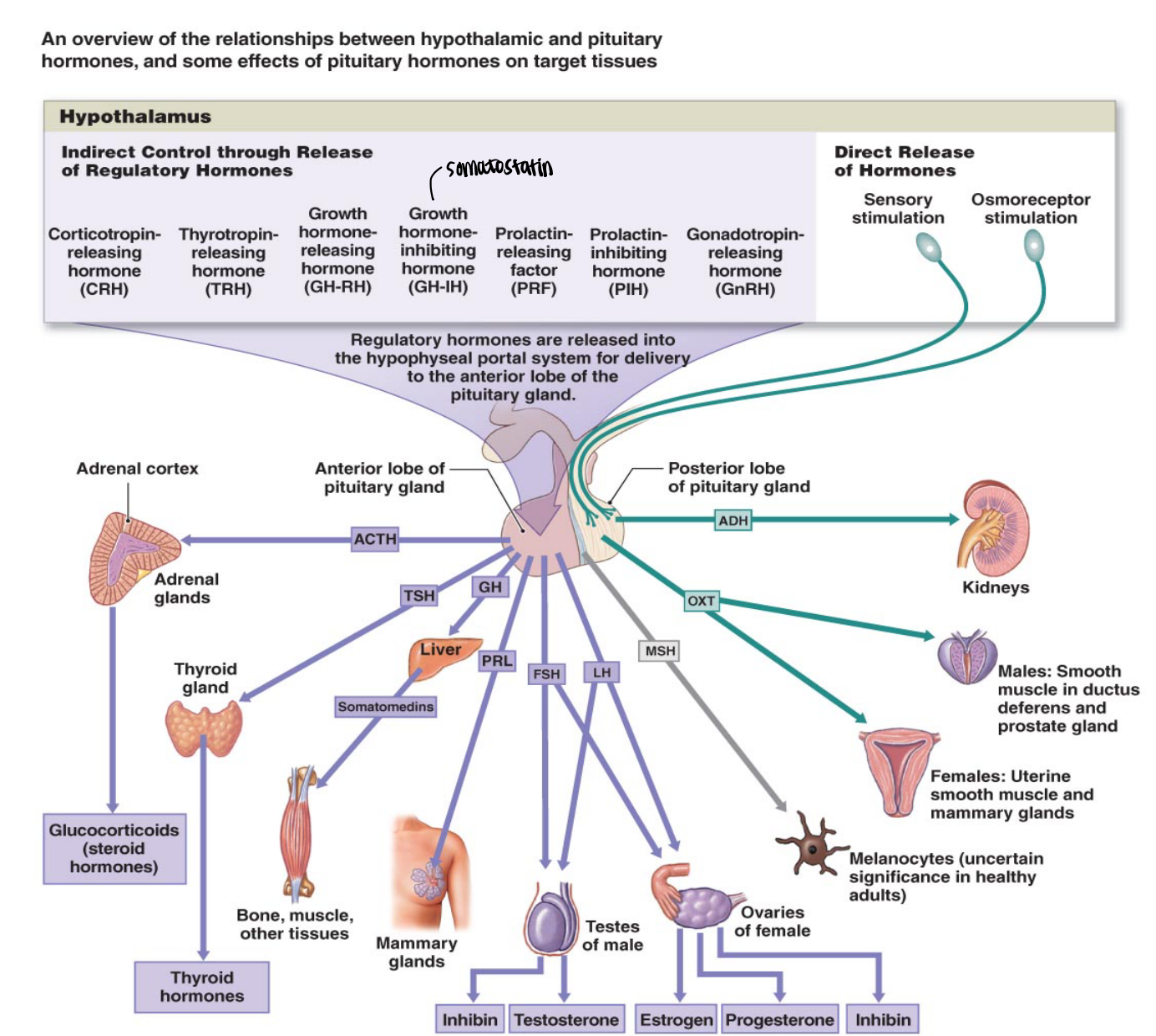
Hypothalamus and Pituitary Gland Interaction
The hypothalamus controls the anterior pituitary through regulatory hormones via the hypothalamo-hypophyseal portal system
Hormones include:
Releasing hormones: e.g., TRH, GnRH
Inhibiting hormones: e.g., PIH, GHIH
The posterior pituitary stores and releases hormones produced by the hypothalamus (ADH and oxytocin)
Types of Hormone Interactions
Synergistic Interaction: Hormones work together for a greater effect.
Example: Cortisol and epinephrine increase blood glucose levels.
Permissive Interaction: One hormone needs another to exert its full effect.
Example: Estrogen is necessary for progesterone to act on the uterus.
Antagonistic Interaction: One hormone opposes the action of another.
Example: Insulin lowers blood glucose; glucagon raises it.
Pituitary Gland (Hypophysis)
Lies inferior to the hypothalamus in the sella turcica of the sphenoid bone.
Pea sized, the pituitary gland is often referred to as the "master gland" because it regulates many bodily functions through hormone secretion.
Posterior Pituitary (Neurohypophysis)
Smaller, neural part of the pituitary gland.
Hypothalamic neurons project through the infundibulum and release hormones in the posterior pituitary.
Somas located in the supraoptic nucleus and paraventricular nucleus.
Axons found in the hypothalmo-hypophyseal tract of the infundibulum.
Synaptic knobs located within the posterior pituitary.
Hypothalamo-Hypophyseal Portal System (Blood Stream)
The hypothalamo-hypophyseal portal system connects the hypothalamus to the anterior pituitary gland.
This system allows regulatory hormones from the hypothalamus to be delivered directly to the anterior pituitary, bypassing general circulation.
Hormones include releasing hormones (e.g., TRH, GnRH) and inhibiting hormones (e.g., PIH, GHIH), which control the secretion of anterior pituitary hormones.
Interactions Between the Hypothalamus and the Posterior Pituitary Gland (Neurohypophysis)
The posterior pituitary serves as a storage and release site for antidiuretic hormone (ADH) and oxytocin (OT).
Hormones are released from synaptic knobs into the bloodstream upon neuron firing.
Antidiuretic Hormone (ADH)
Location of Production: Made in the supraoptic nucleus.
Decreases urine production.
Stimulates thirst.
Constricts blood vessels.
Oxytocin (OT)
Location of Production: Made in the paraventricular nucleus.
Stimulates uterine contractions.
Facilitates milk ejection.
Promotes emotional bonding.
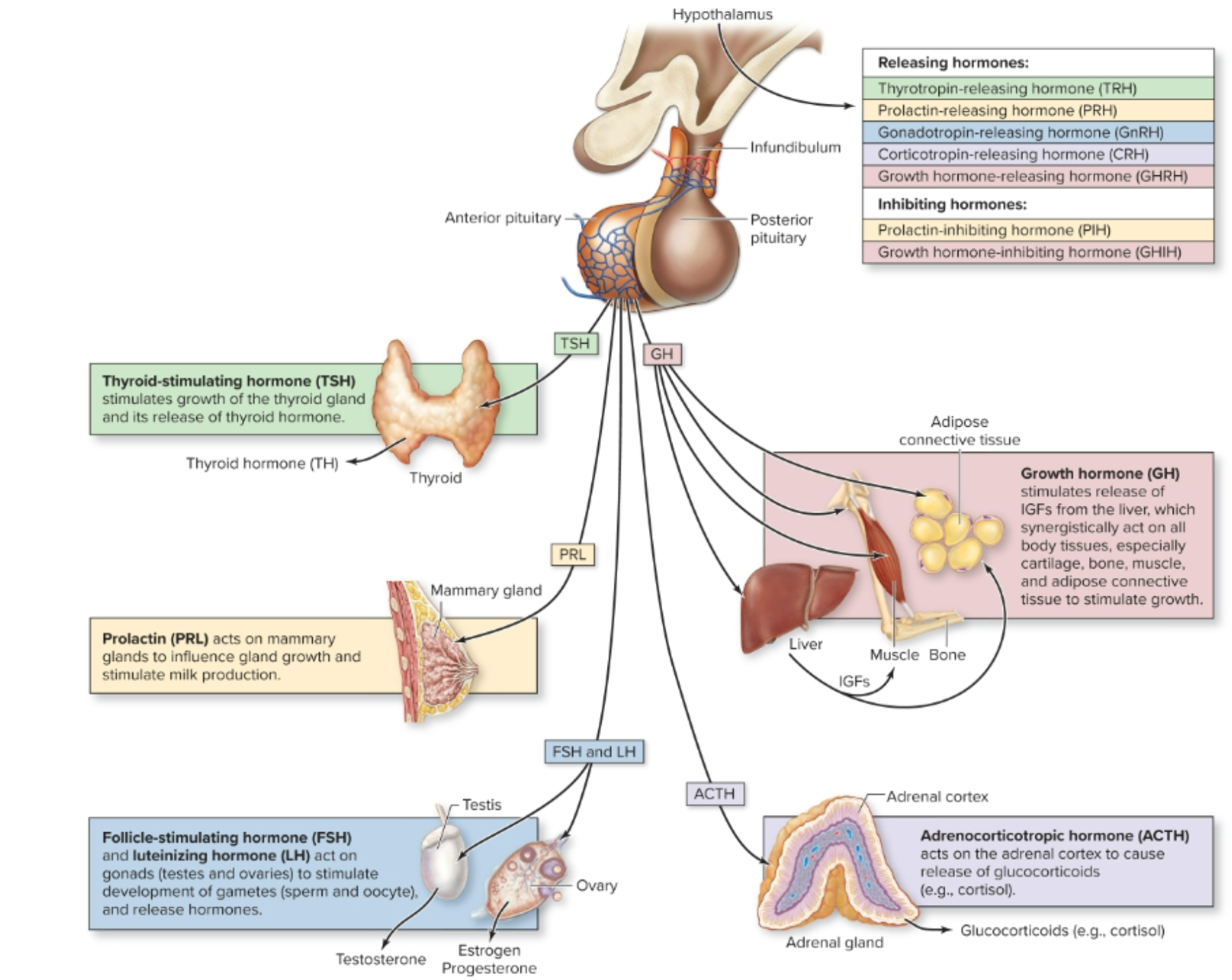
Hormones of the Hypothalamus
Releasing Hormones:
Increase secretion of anterior pituitary hormones.
Include:
Thyrotropin-releasing hormone (TRH)
Prolactin-releasing hormone (PRH)
Gonadotropin-releasing hormone (GnRH)
Corticotropin-releasing hormone (CRH)
Growth hormone-releasing hormone (GHRH)
Inhibiting Hormones:
Decrease secretion of anterior pituitary hormones.
Include:
Prolactin-inhibiting hormone (PIH)
Growth-inhibiting hormone (GHIH)
These hormones play a critical role in regulating the functions of the anterior pituitary gland.
Interactions Between the Hypothalamus and the Anterior Pituitary Gland
Hormones of the Anterior Pituitary
Thyroid-stimulating hormone (TSH; thyrotropin)
Release triggered by thyrotropin-releasing hormone (TRH) from the hypothalamus.
Causes the release of thyroid hormone (TH) from the thyroid gland.
Prolactin (PRL)
Release triggered by prolactin-releasing hormone (PRH) and inhibited by prolactin-inhibiting hormone (PIH) from the hypothalamus.
Causes milk production and mammary gland growth in females.
Adrenocorticotropic hormone (ACTH; corticotropin)
Release triggered by corticotropin-releasing hormone (CRH) from the hypothalamus.
Causes the release of corticosteroids by the adrenal cortex.
Gonadotropins
Follicle-stimulating hormone (FSH) and luteinizing hormone (LH)
Release triggered by gonadotropin-releasing hormone (GnRH) from the hypothalamus.
In females: Regulate ovarian development and secretion of estrogen and progesterone.
In males: Stimulate sperm development and secretion of testosterone.
Growth Hormone (GH; somatotropin)
Causes the liver to secrete insulin-like growth factors 1 and 2.
GH and IGFs function synergistically to stimulate cell growth and division.
Clinical Study: Hypophysectomy
Surgical removal of the pituitary gland due to tumors
Preferred surgical approach through nasal cavity
Hormones need to be replaced and their levels need to be monitored
Clinical View: Disorders of Growth Hormone Secretion
Growth Hormone Deficiency (Pituitary Dwarfism)
Inadequate growth hormone production.
Due to hypothalamic or pituitary problem.
Results in short stature and low blood sugar (hypoglycemia).
Pituitary Gigantism
Caused by too much growth hormone.
Results in excessive growth and increased blood sugar.
Leads to enormous internal organs.
Clinical View: Disorders of Growth Hormone Secretion
Acromegaly
Excessive growth hormone production in adults.
Enlargement of bones in the face, hands, and feet.
Increased release of glucose.
Internal organs also increase in size.
Results from loss of feedback control of growth hormone.
Growth Hormone: Its Regulation and Effects
Regulation of Growth Hormone Release
Release controlled through hormonal stimulation from the hypothalamus by:
GHRH: Growth hormone-releasing hormone
GHIH: Growth hormone-inhibiting hormone
The amount of GHRH released from the hypothalamus is impacted by various factors including:
A person’s age
Time of day
Nutrient levels
Stress and exercise
Effects of Growth Hormone
Stimulates the release of insulin-like growth factors (IGFs) from the liver.
IGFs have similar functions as growth hormone but a longer half-life.
All cells have receptors for either GH, IGFs, or both.
Also promotes the release of nutrients from storage, including:
Glycogenolysis: Breakdown of glycogen into glucose (stimulated).
Gluconeogenesis: Conversion of nutrients to glucose (stimulated).
Glycogenesis: Synthesis of glycogen (inhibited).
Lipolysis: Breakdown of triglycerides (stimulated).
Lipogenesis: Formation of triglycerides (inhibited).
Regulation of Thyroid Hormone Release
Hypothalamic-pituitary-thyroid axis
Cold temperature, pregnancy, high altitude, hypoglycemia
TRH stimulates the anterior pituitary to release TSH (thyroid-stimulating hormone).
TSH binds to receptors on follicular cells and triggers the release of thyroid hormones (TH).
Follicular cells release two forms of TH into the blood: T3 (triiodothyronine) and T4 (tetraiodothyronine).
Clinical View: Disorders of Thyroid Hormone Secretion
Hyperthyroidism
Results from excessive production of thyroid hormones (TH).
Symptoms include increased metabolic rate, weight loss, hyperactivity, and heat intolerance.
Graves' disease is an autoimmune condition where antibodies mimic TSH, leading to hypersecretion of TH; high metabolism may result in edema and exophthalmos (bulging eyes).
Treatment typically involves removal of the thyroid gland followed by hormone supplementation to maintain normal levels
Hypothyroidism
Results from decreased production of thyroid hormones (TH).
Symptoms include low metabolic rate, lethargy, cold intolerance, and weight gain.
Can be caused by various factors such as decreased iodine intake, loss of pituitary stimulation of the thyroid, postsurgical changes, or immune system destruction of the thyroid (e.g., Hashimoto thyroiditis).
Hyposecretion in adults leads to myxedema, characterized by low metabolism. An endemic goiter may develop if caused by a lack of iodine.
Hyposecretion in infants is known as cretinism, which can result in intellectual disability (mental retardation), a thick tongue or neck, and a short body stature.
Treatment involves thyroid hormone replacement.
Calcitonin: Its Regulation and Effects
Calcitonin
Synthesized and released from parafollicular cells of the thyroid gland.
Release is stimulated by elevated blood calcium levels or stress from exercise.
Functions to lower blood calcium levels by:
Inhibiting osteoclast activity (cells that break down bone).
Stimulating the kidneys to increase calcium excretion in urine.
Adrenal Glands
Two regions:
Adrenal Medulla:
Forms inner core of each adrenal gland
Releases epinephrine/norepinephrine
Adrenal Cortex:
Produces more than 25 corticoteroids
Zona glomerulosa, zona fasciculata, and zonna reticularis
Hormones of the Adrenal Cortex
Mineralocorticoids: Regulate electrolyte levels
Location: Produced in the zona glomerulosa
Example: Aldosterone promotes sodium
Glucocorticoids: Regulate blood sugar levels
Location: Produced in the zona fasciculata
Example: Cortisol increases blood sugar levels.
Gonadocorticoids: Function as sex hormones
Location: Produced in the zona reticularis
Androgens: Male sex hormones produced by the adrenals, which can be converted to estrogen in females.
The amount produced by the adrenals is lesser than that produced by the testes.
Cortisol: Its Regulation and Effects
Effects of Cortisol
Cortisol prompts target cells to boost blood nutrient levels.
Liver cells enhance glycogenolysis and gluconeogenesis while reducing glycogenesis.
Adipose cells elevate lipolysis and decrease lipogenesis.
Liver cells utilize the amino acids for gluconeogenesis.
Most cells lower their glucose uptake, conserving it for the brain.
Therapeutic Doses of Corticosterone
Corticosterone is employed as a treatment for inflammation.
It inhibits inflammatory agents and suppresses the immune system.
At elevated doses, side effects include:
Increased risk of infections and cancer.
Enhanced retention of sodium and water.
Inhibition of connective tissue repair.
Clinical View: Disorders in Adrenal Cortex Hormone Secretion
Cushing Syndrome
Can also occur when the adrenal gland overproduces hormones.
Symptoms may include obesity, hypertension, hirsutism (excessive male-pattern hair growth), kidney stones, and menstrual irregularities.
Addison Disease
A form of adrenal insufficiency that arises when the adrenal glands fail.
Symptoms include weight loss, fatigue and weakness, low blood pressure, and skin darkening.
Treatment typically involves oral corticosteroids.
Adrenogenital Syndrome (Congenital Adrenal Hyperplasia)
Begins during the embryonic or fetal stage.
Elevated ACTH levels result in an enlarged adrenal gland and the production of hormones with testosterone-like effects - can lead to masculinization of newborns.
Clinical View: Stress Response
Stressors activate a neuroendocrine response initiated by the hypothalamus, which unfolds in three stages:
Alarm Reaction
Initial activation of the sympathetic nervous system with the release of epinephrine and norepinephrine.
Stage of Resistance
After glycogen is used up, cortisol is released by the adrenal glands to sustain blood sugar levels for energy.
Stage of Exhaustion
Prolonged stress depletes fat stores, leading to protein breakdown for energy and resulting in body weakness and illness.
Anatomy of the Pancreas
Located posterior to the stomach, between the duodenum and spleen.
Contains both endocrine and exocrine functions:
Acinar Cells: Generate exocrine secretions for digestion, making up the vast majority of the pancreas as saclike acini.
Pancreatic Islets (of Langerhans): Contain clusters of endocrine cells:
Alpha Cells: Secrete glucagon.
Beta Cells: Secrete insulin.
Delta Cells: Secrete somatostatin.
F Cells: Secrete pancreatic polypeptide.
Pancreatic Hormones
Purpose: Pancreatic hormones help maintain blood glucose levels.
Normal Range: 70 to 110 mg of glucose/deciliter.
High Levels: Can damage blood vessels and kidneys.
Low Levels: Cause lethargy, mental and physical impairment, and potential death.
Lowering High Blood Glucose Levels with Insulin
After food intake, beta cells detect a rise in blood glucose and respond by secreting insulin.
Insulin travels through the blood and randomly leaves the bloodstream to encounter target cells.
It binds to receptors and initiates second messenger systems.
Once blood glucose falls, beta cells stop secreting insulin.
Actions of Insulin:
In Hepatocytes:
Removes glucose from blood and stores it as glycogen.
In Adipose Cells:
Decreases fatty acid levels in blood and stores fat.
In Most Body Cells:
Increases nutrient uptake in response to insulin.
Enhances amino acid uptake and protein synthesis, especially in muscle.
Increases glucose uptake by incorporating more glucose transport proteins into the plasma membrane.
Glucose Usage:
With less alternate fuels (e.g., fatty acids) available, more body cells use glucose.
Insulin-Independent Cells:
Some cells, including neurons, kidney cells, hepatocytes, and red blood cells, do not require insulin to take in glucose
Clinical View: Conditions Resulting in Abnormal Glucose Levels
Diabetes Mellitus
Inadequate uptake of glucose from blood.
Chronically elevated glucose, leading to blood vessel damage.
Leading cause of retinal blindness, kidney failure, and non-traumatic amputations in the United States.
Associated with increased risk of heart disease and stroke.
Type 1 Diabetes
Characterized by absent or diminished release of insulin by the pancreas.
Tends to occur in children and younger individuals.
May have an autoimmune component.
Requires daily injections of insulin.
Type 2 Diabetes
Results from decreased insulin release or insulin effectiveness.
Obesity is a major cause of development.
Tends to occur in older individuals, but can also affect young adults.
Treatment includes diet, exercise, and medications.
Gestational Diabetes
Occurs in some pregnant women.
If untreated, poses risks to the fetus and increases delivery complications.
Increases the likelihood of developing type 2 diabetes later in life.
Pineal Gland and Hormonal Influence
Melatonin: Influences sleep patterns and reproductive processes
Small unpaired body in the epithalamus of the diencephalon
Melatonin influences GnRH secretion
Parathyroid Gland Functions
PTH: Raises blood calcium levels, acting on bones and kidneys
There are 2-6 parathyroid glands.
PTH goes to your bones to breakdown bone tissue and release calcium into the bloodstream, which helps to increase overall calcium levels in the body.
Age-Related Changes in Endocrine Function
Hormonal production decreases with age, affecting metabolic and physiological processes
Decreased GH and sex hormones lead to various age-related changes
Structures with an Endocrine Function
Thymus: Epithelial cells secrete thymic hormones for T-cell maturation.
Heart Atria: Endocrine tissue secretes atrial natriuretic peptide (ANP) to lower blood pressure (affects kidneys).
Kidney: Endocrine cells release erythropoietin (EPO) to stimulate red blood cell production.
Small Intestine: Secretes secretin and cholecystokinin (CCK) into the blood.
Secretin: Stimulates secretion of bile and pancreatic juice.
CCK: Stimulates release of bile from the gallbladder.
Liver: Secretes insulin-like growth factors and the inactive hormone angiotensinogen.
Angiotensinogen: Converted to active angiotensin II by enzymes from the kidneys and lung blood vessels. Angiotensin II helps raise blood pressure, causes vessel constriction, decreases urine output, and stimulates thirst.
Stomach: Secretes gastrin to increase secretion and motility.
Skin Cells:
Light converts modified cholesterol to Vitamin D3, which is then converted to calcitriol.
Calcitriol raises blood calcium levels.
Adipose Connective Tissue:
Secretes leptin to control appetite. Lower body fat results in less leptin, which stimulates appetite.
Adipose tissue has other significant endocrine effects:
Excess adipose raises cancer risk.
Excess adipose may delay male puberty.
Abnormally low adipose can interfere with the female menstrual cycle.