The Urinary System
Functions of the Urinary System:
Elimination of waste products:
nitrogenous wastes
toxins
drugs
Regulate aspects of homeostasis
electrolyte balance
water balance
acid-base balance of the blood
blood pressure
red blood cells production
activation of vitamin D
carries out gluconeogenesis during extensive fasting
Organs of the Urinary System:
Kidneys
Ureters
Urinary bladder
Urethra
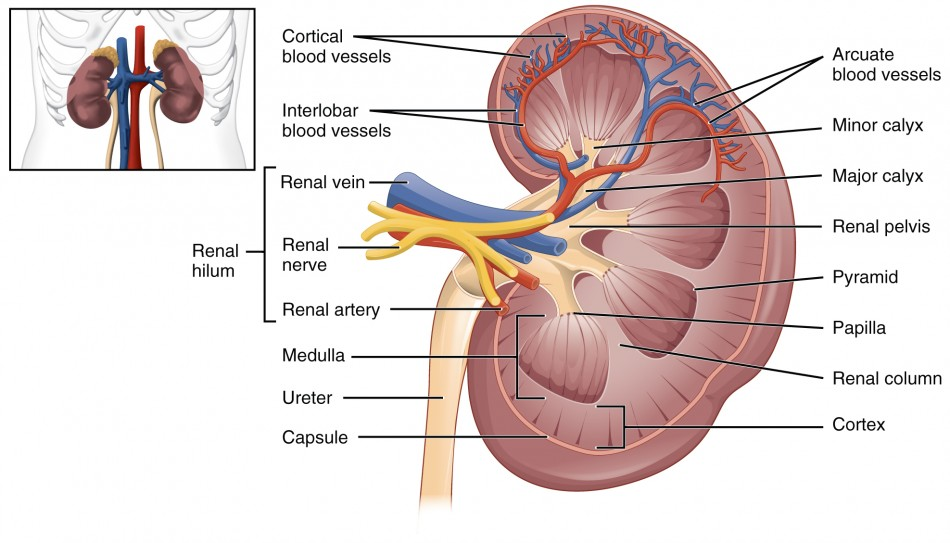
The Kidneys
Location:
between the dorsal body wall and the parietal peritoneum
right kidney is slightly lower than the left
Renal hilum
the medial indentation of the kidney
ureters, renal blood vessels, and nerves enter and exit the kidneys through their renal hilum
Adrenal glands
one on top of each kidney
Coverings of the Kidneys
From inside to outside of the kidneys
Renal capsule
surrounds each kidney
gives the kidney a glistening appearance
prevents infections from spreading to the kidneys
Adipose capsule
surrounds the kidneys together
provides protection to the kidneys
helps the kidneys stay at its correct location by attaching it to the posterior body wall
Renal fascia
outer layer of dense fibrous connective tissue
anchors the kidneys and adrenal glands to surrounding structures
Homeostatic Imbalance- Renal ptosis
A condition when the kidneys drop to a lower position because the amount of fatty tissue that surrounds the kidneys (the adipose capsule) decreases, because of rapid weight loss.
Homeostatic Imbalance- Hydronephrosis
Ptosis causes problems if the ureters which drain from the kidneys become twisted. If this happens, the urine can no longer pass through the ureters and backs up, exerting pressure on the kidney tissue. This condition is called Hydronephrosis and can lead to necrosis of the kidney tissue and renal failure.
Parts of the Kidney:
renal cortex: outer region, contains most nephrons
renal medulla: inside the cortex, contains collecting ducts
medullary pyramids: triangular regions of tissue in the medulla.
the broader base of each pyramid faces towards the cortex
the tip (apex papilla) points towards the inner region
They appear striped because it is made up of parallel bundles of urine collection tubules and capillaries.
renal columns: inward extensions of cortex-like material separating the medullary pyramids
kidney lobes: each kidney lobe is made up of a medullary pyramid and its surrounding cortical tissue
about 8 of them in each kidney
minor calyces: cup shaped structure that encloses the papilla at the tips of the pyramids.
they collect urine from the pyramids and funnel it to the major calyces
major calyces: collects urine from the minor calyces and empties it out in the renal pelvis.
2 to 3 per kidney
renal pelvis: inner funnel-shaped collecting tube that continues into the ureter leaving the kidney via the hilum.
 Homeostatic Imbalance: Pyelitis and Pyelonephritis
Homeostatic Imbalance: Pyelitis and Pyelonephritis
Pyelitis: infection of the renal pelvis and calyx
Pyelonephritis: infection of the entire kidneys
Infections in females are caused by fecal bacteria travelling through the urinary tract
Bloodborne pathogens from other infected sites may sometimes cause these infections
They may lodge in the kidneys and multiply. In severe conditions of pyelonephritis, the kidney swells, abscesses form, and the pelvis is filled with pus.
If left untreated, can severely damage the kidneys, but antibiotics can cure the infection.
Blood Flow in the Kidneys:
The kidneys continuously cleanse the blood and adjust its composition.
The arterial supply of each kidney is called a renal artery.
A network of autonomous nerve fibers supplies nerves to the kidneys and forms the nerve plexus.
Nephrons:
Nephrons are the structural and functional units of kidneys.
Each kidney has millions of tiny nephrons.
They are responsible for forming urine
Main structures:
glomerulus (blood vessels)
renal tubules (urine producing regions)
Every nephron is associated with two capillary beds
a glomerulus capillary bed
a peritubular capillary bed
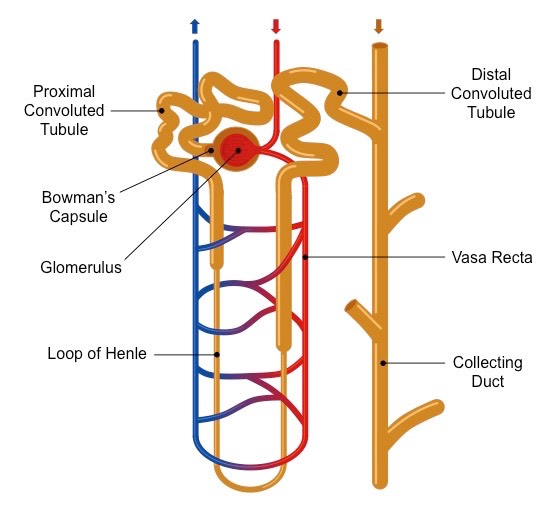
Glomerulus:
Sits within the glomerular capillary.
It is a specialized capillary bed because it is attached on both sides to arterioles. This maintains pressure.
Capillaries are fenestrated allowing large amounts of solute-rich fluid to pass out into a capsule.
The feeder vessel is the large afferent arteriole that brings blood into the glomerulus
The narrow, efferent arteriole receives blood that has already passed through the glomerulus.
Blood pressure within the glomerular capillaries is much higher than other capillaries.
The extremely high blood pressure forces out fluids and solute from the blood and into the glomerular capsule. Most of this filtrate (99%) is eventually reclaimed by the renal tubule cells and returned to the blood in the peritubular capillary beds.
Peritubular Capillaries:
Arises from the efferent arteriole of the glomerulus.
Has a normal, low blood pressure.
Adapted for absorption instead of filtration.
It clings close to the whole renal tube and absorbs substances from it.
Drain into the interlobular veins leaving the cortex
Renal Tubule:
Made up of:
glomerular capsule
proximal convoluted tubule (maximum reabsorption region)
loop of Henle
distal convoluted tubule (maximum secretion region)
Glomerular Capsule:
The closed end of the renal tubule
enlarged and cup-shaped, completely surrounds the glomerulus
The capsule and the glomerulus are together called the renal corpuscle
It has two layers:
The external parietal layer is made up of simple squamous epithelium (does not play a role in filtration)
The inner visceral layer plays a role in filtration and is made up of highly modified cells called podocytes
Proximal Convoluted Tubule:
The glomerular capsule continues into the proximal convoluted tubule.
Its walls are made up of cuboidal epithelium.
The lumen surfaces that are exposed to the filtrate are covered in dense microvilli and increase which increase their surface area for absorption tremendously.
Loop of Henle and Distal Convoluted Tubule:
U-shaped and has ascending and descending limbs
Proximal part of the descending limb is continuous with the proximal convoluted tubule.
The rest of the segment has a thin simple squamous epithelium and is permeable to water.
The ascending limb has cuboidal and columnar epithelium making it the “thick segment”.
Types of Nephrons:
Cortical nephrons:
located entirely in the cortex
includes most nephrons
ascending limbs have a thick segment
Function: production of urine
Juxtamedullary nephrons:
found at the boundary of the cortex and medulla. Their loops of Henle dip deep into the medulla
Ascending limbs have thin and thick segments.
Function: concentration of urine
Juxtaglomerular Apparatus:
Each nephron has a region called the juxtaglomerular apparatus.
It is located where the most distal part of the ascending limb of the loop of Henle meets the afferent arteriole.
Both the ascending limb and afferent arteriole are modified at the point of contact.
Cells in the juxtaglomerular apparatus:
Juxtaglomerular cells: enlarged smooth muscle cells that have prominent renin secreting granules in the arterioles walls.
act as mechanoreceptors and sense blood pressure in the arterioles
Macula densa cells: tall and closely packed cells in the ascending limb
act as chemoreceptors and sense NaCl content in the filtrate.
Extraglomerular mesangia l cells: engulf and degrade macromolecules that get stuck in the filtration membrane
they are a part of the JGA, but their function is unclear
Collecting Ducts:
Collecting ducts have two types of cells:
Intercalated cells: They are cuboidal with plenty of microvilli. It has two varieties: type A and type B. They play a major role in the acid base balance of blood.
Principal cells: They are short and have few microvilli. They help maintain the body’s water and Na+ balance.
The collecting ducts receive urine from the many nephrons. They run down the medullary pyramids giving them a striped appearance.
They deliver the final urine product to the calyces and renal pelvis.
Urine then flows from the renal pelvis to the ureter which brings the urine to the bladder for temporary storage.
Urine Formation Process:
Urine formation is a result of three processes:
Filtration- from capillaries in the glomerulus by the glomerular capsule cells.
Reabsorption- reabsorbed by PCT cells and passed to the peritubular capillaries to be retained in the body.
Secretion: peritubular capillaries take urine to the DCT for elimination
Filtration Membrane:
Lies between the blood and the interior of the glomerular capsule. It consists of three layers:
Fenestrated endothelium
Basement membrane- a glycoprotein layer made up of fused basal laminae of the endothelial cells and podocytes
Podocytes
Filtration
Filtration is a nonselective, passive process of filtration of the blood plasma.
Filtrate includes: molecules smaller than 3nm in diameter, water, glucose, amino acids, and nitrogenous acids.
These are forced through the filtration membrane.
Filtrate does NOT include: proteins (such as albumin) and blood cells.
These cannot pass through the filtration membrane.
Filtrate: blood plasma without the blood cells and most blood proteins.
Filtrate is collected in the glomerular capsule and leaves via the renal tubule.
Glomerular filtration rate (GFR): the volume of filtrate formed every minute by all the two million glomeruli of the kidneys.
As long as the systemic blood pressure is normal, filtrate will continue to be formed. If the arterial blood pressure drops, glomerular pressure becomes inadequate to force substances out of the blood into the tubules and filtrate formation stops.
Tubular Reabsorption:
The peritubular capillaries reabsorb several materials:
some water
glucose
amino acids
ions
Most reabsorption is active, but some is passive.
Water is absorbed passively through aquaporins.
Chloride and bicarbonate ions are absorbed passively using a gradient created by sodium.
Sodium absorption is active using the sodium potassium pump
Glucose, amino acids, lactate, and vitamins are absorbed through secondary active transport
Most absorption occurs in the proximal convoluted tubule.
Routes through which reabsorption can take place:
Transcellular route: tubule cells are transporters → they take up needed substances from the filtrate → they release them into the interstitial fluid → they are absorbed into the peritubular capillary blood
Paracellular route: There is limited space between the tubule cells because of the tight junctions in the PCT. In the regions where these junctions become leaky, water and ions can pass through.
Materials Not Reabsorbed
Urea: formed by the liver as an end product of protein breakdown when amino acids are used to produce energy.
Uric Acid: released when nucleic acids are broken down.
Creatinine: associated with creatine metabolism in muscle tissue
Since tubule cells cannot reabsorb these substances, these substances stay in the filtrate and are found in high concentrations in urine excreted from the body.
Urine Contents:
Various ions are either reabsorbed or exit the body through urine depending on the body’s needs at a particular time to maintain a proper pH balance and electrolyte balance in the blood.
Although most reabsorption occurs through the proximal convoluted tubule, the distal convoluted tubule and collecting ducts are also active.
The descending loop of Henle has many aquaporins and allows for water absorption.
Aquaporins are scarce in the ascending loop of Henle. These permeability differences play an important role in producing dilute or concentrated urine.
Reabsorption in the distal convoluted tubule depends on the hormone levels in the body. (ADH, aldosterone, atrial natriuretic peptide, and PTH).
Tubular Secretion
Some materials move from the peritubular capillaries into the renal tubules to be eliminated as urine. This elimination regulates blood pH and substances that aren’t already in the filtrate.
Most tubular secretion occurs in the distal convoluted tubule. Tubular secretion includes:
excess hydrogen and potassium ions
creatinine
urea
uric acid
This process is important because it helps the body get rid of toxins, poisons, and drugs.
These materials then leave the renal tubules and go to the ureters.
Medullary Osmotic Gradient
Juxtamedullary nephrons create an osmotic gradient within the renal medulla that allows the kidneys to produce urine of varying concentrations.
There are two types of countercurrent mechanisms that determine the urine concentration and volume.
Countercurrent multiplier- the filtrate in the ascending and descending limbs of the juxtamedullary nephrons combine to create a medullary gradient.
Countercurrent exchanger- blood flows through the ascending and descending portions of the vasa recta surrounding the juxtamedullary nephrons maintaining the gradient.
Characteristics of Urine Concentration:
Concentration of urine mainly depends on the amount of ADH present in the blood.
Characteristics of urine concentration:
Amount- In 24 hours, the kidneys filter 150-180 liters of blood plasma and produce 1.0-1.8 liters of urine.
Color- Urine is clear and colored somewhat yellow due to the pigment urochrome (results from the destruction of hemoglobin) and other solutes.
Urine may be another color as a result of eating certain foods (ex. beets) or the presence of bile or blood in the urine.
Slightly aromatic- if it is allowed to stand, urine takes on the smell of ammonia due to the bacteria in urine. Some drugs, vegetables, and various diseases alter the usual odor of urine.
Normal pH- pH is usually around 6, but diet can make it more acidic (by eating lots of protein and whole wheat) or more basic (by eating lots of plant food). Bacterial infection of the urinary tract can also make the pH more alkaline.
Specific gravity- 1.001 to 1.035. Since urine is water plus solutes, urine weighs more and is more dense than regular water.
When a urine is dilute (thinner) it has a lower specific gravity. This is caused by consuming excessive fluids, diuretics, or having chronic renal failure.
Conditions that result in higher specific gravity (thicker urine) are inadequate fluid intake, fever, and a kidney inflammation called pyelonephritis.
Generally, the smaller the volume, the greater the specific gravity, and the darker the color of urine.
Normal and Abnormal Urine
Solutes normally found in urine:
sodium and potassium ions
major nitrogenous wastes:
urea
uric acid
creatinine
ammonia
bicarbonate ions
various other ions
Abnormal substances in urine:
glucose- normally is completely reabsorbed unless there are excessive levels in the blood
blood proteins
red blood cells
hemoglobin
white blood cells (pus)
bile
The presence of abnormal substances in urine helps the doctor diagnose homeostatic imbalances.
Homeostatic Imbalances of Urine Concentration:
Oliguria- abnormally low urine output between 100-400 ml per day
Anuria- abnormally low urine output that is less than 100 ml per day
low urine output usually indicates that glomerular pressure is too low for filtration to occur, but it can also result from, transfusion reactions, acute inflammation, or crush injuries of the kidneys
Chronic renal disease- the GFR or glomerular filtration rate is less than 60ml/min for at least 3 months. Nitrogenous wastes accumulate in the blood, and pH becomes more acidic.
Can cause diabetes mellitus, hypertension, or repeated kidney infections.
Renal Failure- GFR is less than 15 ml/min. Filtration formation decreases or stops leading to uremia or urine in the blood.
Ureters
The ureters are thin, urine transporting tubes attaching from the kidneys to the bladders.
Continuous with the renal pelvis
Exits the kidneys through the renal hilus
Runs behind the peritoneum and obliquely enters the proximal aspect of the bladders.
The ureter wall is tri layered:
Mucosa: lines the lumen, has transitional epithelium
Muscular layer: made up of smooth muscle cells arranged two layers: an internal longitudinal layer and an external circular layer.
An additional longitudinal layer appears at the lower part of the ureter
Adventitia- covers the external surface and is fibrous connective tissue.
Peristalsis aids in urine transport.
Urine is prevented from flowing backward by valve like folds of the bladder mucosa that flaps over the ureter openings. Any increase in bladder pressure compresses and closes the distal ends of the ureters.
Homeostatic Imbalance- Kidney Stones
Kidney stones or urine calculi form when urine becomes extremely concentrated and solutes such as calcium, magnesium, or uric acid salts form crystals in the renal pelvis.
Excruciating pain that radiates to the sides occurs when the ureter walls contract to propel urine by peristalsis or when the calculi become wedged in a ureter.
Kidney stones can be caused by frequent bacterial infections of the urinary tract, urinary retention, high blood levels of calcium, and alkaline urine.
Surgery has been a treatment choice, but there is a newer noninvasive procedure (shock wave lithotripsy) that uses ultrasound waves to shatter the stones. The sand like remnants of the stones are then painlessly excreted through urine.
People with a history of kidney stones should drink cranberry juice and plenty of water to acidify and dilute the urine.
Urinary Bladder
Smooth, collapsible, muscular sac
Temporarily stores urine
The interior of the bladder has three openings:
two from the ureters
one to the urethra
The smooth triangular region of the bladder base outlined by these three openings is called the trigone.
The trigone is clinically important because infections tend to persist in this region
In males, the prostate gland surrounds the neck of the bladder where it empties into the urethra.
Urinary Bladder Wall:
The urinary bladder wall has three layers:
Inner mucosal layer- made up of transitional epithelium (basal layer has cuboidal or columnar cells and apical cells are dome shaped or squamous depending on the amount of urine in the bladder.
Middel smooth muscle layers- collectively called the detrusor muscle consisting of inner and outer longitudinal layers and middle circular layers.
Outer fibrous adventitia layer- made up of fibrous connective tissue
In an empty bladder, walls are thick and folded into rugae. The bladder can expand significantly without increasing internal pressure.
A moderately full bladder is about 12.5 cm long and holds about 500 ml of urine. The bladder is capable of holding more than twice than that! However, if overextended, it can burst.
Urethra
A thin-walled muscular tube that carries urine from the urinary bladder to the outside of the body using peristalsis.
Epithelium of the mucosal lining is pseudostratified columnar epithelium.
Near the bladder it is transitional epithelium and near the external opening it is stratified squamous epithelium.
Release of the urine is controlled by two sphincters:
Internal urethral sphincter- involuntary, a thickening of the detrusor muscle and forms at the junction of the urinary bladder and urethra.
External urethral sphincter- voluntary, formed by skeletal muscle surrounding the urethra as it passes through the urogenital diaphragm.
Urethra in Males vs Females:
Length:
Females: 3-4 cm
Males: 20 cm
Location:
Females: along the wall of the vagina and external opening
Males: through the prostrate and penis
Function:
Females: only carries urine
Males: carries urine and is a passageway for sperm cells
Homeostatic Imbalance- Urinary Tract Infection:
Since the female urinary opening is so close to the anal opening and feces contains lots of bacteria, improper toilet habits can carry bacteria into the urethra
UTIs are common in sexually active women. The use of spermicides as birth control kills the helpful bacteria allowing for infectious fecal bacteria to colonize
Since the mucosa of the urethra is continuous with that of the rest of the urinary tract organs an inflammation of the urethra can lead to bladder or kidney inflammations as well.
Symptoms of urinary tract infection include- dysuria (painful urination), urinary urgency and frequency, fever, and cloudy or blood-tinged urine. When kidneys are involved, back pain and headaches are common.
UTIs can be cured with antibiotics
Micturition or Voiding (peeing)
Both urethral sphincters must be relaxed in order for voiding to occur.
The internal urethral sphincter (involuntary) is relaxed after the bladder is stretched.
Activation is from an impulse sent to the spinal cord and then back via the pelvic splanchnic nerves causing the bladder to go into reflex contractions.
As the contractions become stronger, stored urine opens the internal urethral sphincter into the upper part of the urethra. This is when the person feels the urge to void (pee).
The external urethral sphincter must be voluntarily relaxed. A person can choose to keep it closed and postpone bladder emptying temporarily.
If one chooses not to void, the reflex contractions of the bladder will temporarily stop, and urine will continue to accumulate in the bladder.
Eventually micturition will occur whether the person wills to or not.
Homeostatic Imbalance- Incontinence
Incontinence occurs when a person is unable to voluntarily control the external sphincter.
This is normal in children two or younger who have not yet gained control over the external sphincter.
It also occurs when even older children are sleeping so soundly that they are not awakened by the stimulus.
Stress incontinence can also occur in which, abdominal pressure during laughing or coughing can force urine through the external sphincter. This can also happen during late pregnancy when the baby puts pressure and stretches the pelvic muscles.
Homeostatic Imbalance- Urinary Retention
Urinary retention occurs when the bladder is unable to expel its contained urine.
It can occur after surgery when general anesthesia is given, and smooth muscles need time to regain their activity.
Elderly men with enlarged prostate glands may get urinary retention. As the prostate gland enlarges, the urethra narrows making it hard to void.
When urinary retention is prolonged, a slender and flexible drainage tube called a catheter must be inserted through the urethra to drain the urine and prevent bladder trauma from excessive stretching.
Excretion through the Kidneys Pathway:
Glomerular capsule → proximal convoluted tubule → loop of Henle → distal convoluted tubule → collecting duct → minor calyx → major calyx → renal pelvis → ureter → bladder → urethra → internal urinary sphincter → external urinary sphincter
Fluid, Electrolyte and Acid-Base Balance
Blood composition depends on three major factors:
Diet
Cellular metabolism
Urine output
The kidneys play four major roles in keeping the blood composition constant:
Excretion of nitrogen containing wastes
Maintaining water balance
Maintaining electrolyte balance in the blood
Ensuring proper blood pH
Maintaining Water Balance:
The normal amount of water in the body is:
50% in young adult females
60% in young adult males
This difference is because males have more body mass while females have more body fat (adipose tissue is less hydrated).
Babys have 75% due to less body mass and less body fat.
As people age, water percentage decreases (45%).
Water is important for many body functions, so water levels must be maintained.
Distribution of Body Fluid:
Water is located in three areas within the body. They are referred to as fluid compartments:
Intracellular fluid (inside the cell): 2/3 of water
Extracellular fluid (outside of the cells): 1/3 of water
Interstitial fluid
Blood plasma
Extracellular fluid also accounts for cerebrospinal fluid, serous fluids, humors of the eye, lymph, synovial fluid, and gastrointestinal fluid (basically everything that’s not plasma).
Link Between Water and Salt:
Nonelectrolytes such as carbohydrates, lipids, creatinine, and urea have covalent bonds that prevent them from disassociating in the solution.
Electrolytes such as salts, acids, bases and some proteins, disassociate into ions in H2O and have a greater osmotic power since each molecule dissociates into at least 2 ions.
Changes in electrolyte balance such as sodium, potassium, and calcium) causes water to move from one compartment to another.
This can alter blood volume, blood pressure, and impair the activity of nerve and muscle functions.
Maintaining Water Balance:
Water intake must equal water output
Water intake varies widely and on average (in adults) is 2500 ml per day.
Sources for water intake:
ingested foods and fluids
water produced by metabolic processes
Sources for water output:
vaporization out of the lungs
lost in perspiration (sweating)
leaves the body as feces
urine production
A rise in plasma osmolality triggers thirst and the release of ADH which prevents water lose.
Plasma osmolality is the amount of solutes in the plasma (blood).
Dilute urine is produced if water intake is excessive.
Less concentrated urine is produced if large amounts of water are lost (not less water is taken in).
Thirst is the driving force of water intake. It is controlled by the hypothalamic thirst center which is activated by:
osmoreceptors
sensory receptors that detect changes in osmotic pressure resulting in a gain or loss of water
dry mouth
an increase in blood osmotic pressure results in a decrease saliva production
a decrease in blood volume or pressure
this will cause the release of angiotensin 2 resulting in thirst
Homeostatic Imbalance- Dehydration
Dehydration is the loss of water from the extracellular fluid (ECF). Cells will lose water and shrink.
Causes: hemorrhages, severe burns, prolonged vomiting, diarrhea, excessive sweating, water deprivation, diuretic abuse, diabetes mellitus or insipidus.
Symptoms: sticky oral mucosa, thirst, flushed skin, and decreased urine
Prolonged dehydration leads to mental confusion, weight loss, fever, and inadequate blood volume leading to hypovolemic shock.
Homeostatic Imbalance- Hypotonic Hydration
Hypotonic hydration is caused by quick overhydration. The extracellular fluid is diluted.
Symptoms: nausea, vomiting, cramps, and cerebral edema which causes coma and death
It is treated by hypotonic saline solution administered intravenously.
Regulation of Water and Electrolyte Reabsorption:
This regulation is primarily controlled by hormones.
Antidiuretic hormone (ADH)- prevents excessive water loss through urine.
ADH travels in the blood to its main target, the kidney’s collecting duct cells, where it makes the ducts reabsorb more water.
Aldosterone- regulates ion content in the extracellular fluid.
Aldosterone regulates sodium content in the ECF. Less sodium makes the blood dilute. Water leaves the bloodstream and flows out into the tissue spaces causing edema and possible shutdown of the circulatory system. This is triggered by the renin-angiotensin mechanism.
Cells in the kidneys and hypothalamus are active monitors.
Homeostatic Imbalance: Diabetes Insipidus
When ADH is not released huge amounts of dilute urine are flushed out of the body everyday.
This condition is called diabetes insipidus and can lead to severe dehydration and electrolyte imbalance.
Affected individuals are always thirsty and have to drink fluids continuously to maintain normal fluid balance.
Homeostatic Imbalance: Addison’s disease and Polyuria
People with Addison’s disease have hypoaldosteronism. This leads to polyuria or the excretion of large amounts of urine. They lose tremendous amounts of salt and water to urine.
Individuals have a craving for salty or sour foods.
As long as adequate amounts of salt and fluids are ingested, people with this condition can avoid problems but they are usually on the brink of dehydration.
Homeostatic Imbalance- Pica
Pica is the condition in which a person has mineral deficiencies causing them to have abnormal food cravings.
People with this condition may crave and eat chalk, clay, starch, and even burnt matches.
Regulation of Calcium, Phosphate, and Anions
ECF calcium and phosphate ion levels are regulated by the parathyroid hormone.
The parathyroid hormone stimulates osteoclasts to break down bone and stimulates kidneys to reabsorb calcium ions while decreasing phosphate ion reabsorption.
Chloride ions play a crucial role in maintaining osmotic pressure. PCT is responsible for its regulation.
Acid-Base Balance in the Blood
Blood pH must remain between 7.35 and 7.45 in order to maintain homeostasis.
Alkalosis- pH above 7.45
Acidosis- pH below 7.35
Most ions originate as byproducts of cellular metabolism which continuously adds substances to the blood that tend to disrupt the acid-base balance.
Acids produced include- phosphoric acid, lactic acid, fatty acids, and carbonic acid (from carbon dioxide)
Bases produced include- ammonia
Most acid-base balance is maintained by the kidneys. Other acid-base controlling systems are:
Blood buffers
Respiration
Blood Buffers:
Buffers are molecules that react to prevent dramatic changes in hydrogen ion concentrations when acids or bases are added.
They bind to H+ ions when pH drops
They release H+ ions when pH rises
Three major chemical buffer systems:
Bicarbonate buffer system
Phosphate buffer system
Protein buffer system
The Bicarbonate Buffer System:
The bicarbonate buffer system is a mixture of carbonic acid (a weak acid) and sodium bicarbonate (a weak base).
When a strong acid, such as hydrochloric acid is added to the blood, the bicarbonate ions of the salt, act as bases forming more carbonic acid.
hydrochloric acid + sodium bicarbonate → carbonic acid + salt
strong acid weak base weak acid salt
If a strong base like sodium hydroxide is added to the blood, carbonic acid will dissociate.
sodium hydroxide + carbonic acid →sodium bicarbonate + water
strong base weak acid weak base water
The Phosphate Buffer System:
The phosphate buffer system is a combination of sodium dihydrogen phosphate (a weak acid), sodium salts, dihydrogen phosphate, and monohydrogen phosphate.
When a strong acid like hydrochloric acid is added to the urine, the monohydrogen phosphate ions of disodium phosphate act as bases forming more sodium dihydrogen phosphate (weak acid).
hydrochloric acid + disodium phosphate →dihydrogen phosphate + salt
strong acid weak base weak acid salt
If a strong base like sodium hydroxide is added to the blood, sodium dihydrogen phosphate will release water.
sodium hydroxide + dihydrogen phosphate → disodium phosphate + water
It is not important in blood because there isn’t enough phosphate but it is more important in urine where phosphate concentrations are higher.
The Protein Buffer System:
The protein buffer system is ¾ of all buffering power in the body fluids inside the cells due to intracellular proteins.
When pH rises, the exposed carboxyl groups within the amino acids release H+ ions.
amino acid → basic ion + hydrogen ion
Some amino acids have exposed amino groups that act as bases and accept H+ molecules becoming ammonium ions.
amino acid + hydrogen ion → weak base
A single protein molecule can function reversibly as an acid or as a base depending on the environment. Such molecules are called amphoteric molecules.
The Respiratory Controls of Acid-Base Balance:
Carbon dioxide in the blood is converted into bicarbonate ion and transported in the plasma.
carbon dioxide + water → carbonic acid + hydrogen ion + bicarbonate ion
carbonic anhydrase
Increases in hydrogen ion concentration produces more carbonic acid
Excessive hydrogen ion concentration can be blown off with the release of carbon dioxide from the lungs.
Respiratory rate can rise and fall depending on changing blood pH.
Renal Mechanisms of Acid-Base Balance:
Chemical buffers can tie up excess acids or bases temporarily, but they cannot eliminate them from the body. And while the lungs can dispose of carbonic acid by eliminating carbon dioxide, only the kidneys can rid the body of the other acids generated during metabolism.
Only the kidneys have the power to regulate blood levels of alkaline substances.
However while, the kidneys act slowly and require hours or days to bring about changes in blood pH, they are the most effective mechanisms for regulating blood pH.
The most important ways that the kidneys maintain pH balance are:
Conserving filtered bicarbonate ions- When carbonic acid dissociates, it produces bicarbonate ions and hydrogen ions. When large amounts of H+ ions are secreted, large amounts of bicarbonate ions enter the peritubular capillaries to be conserved. This prevents acidosis
Generating new bicarbonate ions- PCT and collecting ducts generate new bicarbonate ions by secretion and excretion of hydrogen ions or ammonium ions. This prevents acidosis
Excreting bicarbonate ions- collecting ducts excrete bicarbonate ions of the body is in alkalosis.
Urine pH varies from 4.5 to 8 showing the kidneys’ ability to excrete acidic or basic ions to maintain blood pH balance.
Abnormalities of Acid-Base Balance:
Respiratory abnormalities:
Respiratory acidosis- characterized by the falling of blood pH and rising of carbon dioxide levels.
Respiratory alkalosis- Carbon dioxide is eliminated from the body faster than it is produced, increasing blood pH levels. Also called hyperventilation.
Metabolic abnormalities:
Metabolic acidosis- results from excessive alcohol intake, excess loss of bicarbonate ions, accumulation of lactic acid (during exercise), ketosis (caused by dieting), or kidney failure.
Metabolic alkalosis- caused by vomiting acidic contents or excess intake of bases.
When the acid-base balance is disrupted, the respiratory pathways attempt to compensate for the metabolic pathways and vice versa. The respiratory system can regulate the balance by changing the rate and depth of breathing. Kidneys can change the acid base balance by returning or excreting bicarbonate ions.
Developmental Aspects of the Urinary System
Functional kidneys are developed by the third month.
Urinary system of a newborn:
bladder is small
urine cannot be concentrated
Control of the voluntary sphincter does not start until 18 months
There is a progressive decline of the urinary system with age.
Bladder shrinks with aging
Urinary retention is common in elderly men.
?