Week 1 - ITRODUCTION + ANXIETY DISORDERS
CHAPTER 2 - Theories and Treatment of Abnormality
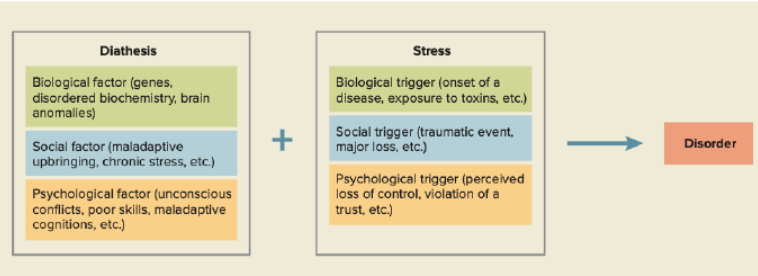
The diathesis-stress model states that people have a certain vulnerability for disorders (diathesis). Diathesis means risk factor.
Biological causes of abnormality: brain dysfunction; chemical imbalances; genetic abnormalities
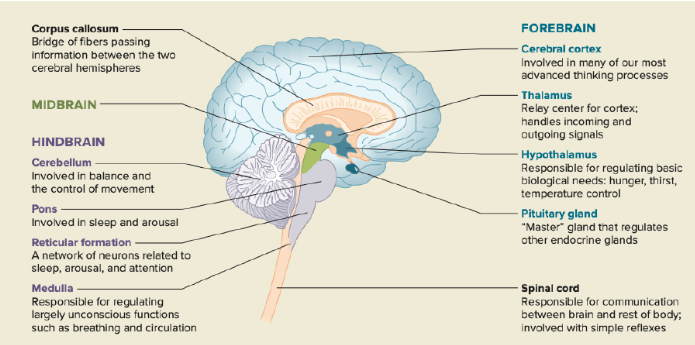
Hindbrain: controlling movement, balance; sleep and arousal patterns; attention; unconscious functions (breathing circulation).
Forebrain: advanced thinking; basic biological needs (hunger, thirst, temperature control)
Limbic system: instinctive behaviors (reactions to stressful events, eating). Amygdala - fear. Hippocampus - memory.
Neurotransmitters and synapse
hormones affect mood, levels of energy and reaction to stress (especially in women)
behavioral genetic - study of the genetics of personality and abnormality. To what extend are behavioral tendencies inherited? what are processes by which genes affect behavior?
Gene abnormality - associated with psychological disorders. Polygenic process - multiple genetic abnormalities cause a specific disorder. Epigenetics - environment affects the expression of genes.
Biological therapies
Drug therapies - help relieve psychological symptoms by improving functioning of neurotransmitter systems (ANTIPSYCHOTIC; ANTIDEPRESSANTS; LITHIUM - mania; ANTIANXIETY)
Electroconvulsive therapy and brain stimulations - deep brain stimulation; vagus nerve stimulation; repetitive transcranial magnetic stimulation (rTMS) (very severe cases of depression)
Psychosurgery - very severe disorders (not common anymore)
Psychological approaches
Behavioral - classical conditioning (stimuli, Pavlov’s dog); operant conditioning (reward and punishment); modeling and observational learning (observe or role models); shaping
Cognitive - based on thoughts and/or beliefs; identifying and challenging negative thoughts and beliefs. Generally short term. Encouraging to face fears.
Psychodynamic and humanistic - behavior, thoughts and emotions (normal or abnormal) are influenced by unconscious processes. Psychoanalysis, designed to be long term. Helps recognize maladaptive coping strategies and sources of unconscious conflicts. Repeatedly going through painful memories and issues
Family systems - problems are rooted in family systems (often a whole family is brought into therapy)
Emotion-focused approaches - the importance of understanding and processing emotions. Recognize and express feelings, learn how to manage emotions effectively.
CHAPTER 3 - Assessing and Diagnosing Abnormality
Validity is the degree to which a test measures what it is supposed to measure.
• Face validity: The items seem to measure what the test intends to measure.
• Content validity: The test measures all important aspects of the phenomenon.
• Convergence validity: The test has the same outcome as other tests that measure the same construct.
• Predictive validity: The test accurately predicts how someone later acts, thinks, or feels.
• Construct validity: The test only measures what it is supposed to measure, and nothing else.
Reliability is a psychometric criterion of how consistently a test measures what it is supposed to measure.
• Test-retest reliability: The consistency of the results of a test over time.
• Alternate form reliability: Different versions of the same test have similar results.
• Internal reliability: People answer similarly among different parts of the same test.
• Interrater (inter-judge) reliability: Different raters come to the same conclusion.
Clinical interview
mental status exam; appearance and behavior; thought processes; mood and affect; intellectual functioning; orientation
Symptom Questionnaires: cover variety of symptoms of different disorders; BDI (Beck Depression Inventory) is criticized a lot.
Personality Inventories: asses ways of thinking, feeling and behaving
Behavioral Observation: disadvantage - when people are being watched they tend to change their behavior.
Brain-Imaging Techniques
Computer tomography (CT) - x-ray procedure; quite harmful - avoided
Positron-emission tomography (PET) - picture of activity in the brain (injecting a harmless radioactive isotope
Single photon emission computed tomography (SPECT) - like PET but different substance
Magnetic resonance imaging (MRI) - very detailed picture, not harmful
Psychophysiological tests are used to detect changes in the brain and the nervous system that reflect psychological changes (alternative method to CT, PET, SPECT, MRI)
Electroencephalogram (EEG) - measures electrical activity along the scalp
CHALLENGES IN ASSESTMENT - resistance to share information; difficulties with children; across cultures
CHAPTER 7 - Mood Disorders and Suicide
DEPRESSION
/
Symptoms of depression:
depressed mood
anhedonia - loss of interest of everything in life
changes in appetite, sleep, decreased energy/activity levels
losing touch with reality (delusions and hallucinations)
Diagnosing depressive disorders:
Major depressive disorder: symptoms last two weeks or more. Subtypes: anxious distress; mixed features; melancholic features; psychotic features; catatonic features; atypical features; seasonal patters; peripartum onset.
Persistent depressive disorder: depressed mood for most of the day for at least two years
Premenstrual dysphoric disorder: Increase in distress during PMS
Prevalence of depressive disorders:
high possibility in adults; low among people 65+ and difficult to diagnose because less willing to report symptoms; symptoms occur in serious medical illness; ppl with history of depression are likely to die before reaching old age
less common among children
women > men
Mania (bipolar):
Bipolar I disorder: elevated, expansive or irritable mood more than one week (depression - don’t need to be diagnosed; mania - need diagnosis)
Bipolar II disorder: severe depression + mania with less symptoms (depression - need diagnosis; mania - don’t need to be diagnosed)
Cyclothymic disorder: less severe, but more chronic
Symptoms of Mania: rapid cycling bipolar I or bipolar II; disruptive mood dysregulation disorder
Prevalence:
less common that depressive disorders
men = women
the same across cultures
develops in adolescence or early adulthood
Benefits: better creativity
Biological theories of depression:
genetic theory - genes predispose people to depression
neurotransmitters theory - dysregulation of neurotransmitters and their receptors cause depression (take meds to help)
structural and functional brain abnormalities
hormones
Psychological theories:
behavioral: life stress leads to depression because of reduced positive reinforcers in life; learned helplessness theory (uncontrollable negative event is likely to lead to depression
cognitive: negative cognitive triad: negative views of themselves and the world around them; ruminative response style
interpersonal: difficulties and losses can trigger depression; rejection sensitivity - easily perceiving rejection
Theories of Bipolar disorder:
Biological: genetic factors - strong linkage between genes and disorder; structural and functional brain abnormalities; neurotransmitters; psychological factors.
Biological treatments:
Drug therapy:
SSRIs- selective serotonin reuptake inhibitors
SNRIs - selective serotonin-norepinephrine reuptake inhibitors
Norepinephrine-dopamine reuptake inhibitor
Tricyclic antidepressants
MAOIs - monoamine oxidase inhibitors
Mood stabilizers:
lithium and anticonvulsant and atypical antipsychotic medications (blood taken regularly - common overdose)
Electroconvulsive therapy (ECT)
Repetitive transcranial magnetic stimulation (rTMS) - severe case and nothing else has worked
Vagus nerve stimulation
Deep brain stimulation
Light therapy
Psychological treatments:
Behavior therapy
Cognitive-behavioral therapy
Interpersonal therapy focuses on the interpersonal relationships and the role of social interactions in the development and maintenance of mood disorders such as depression. The therapy aims to improve interpersonal skills and enhance relationships. It typically involves identifying and addressing issues related to grief, role disputes, role transitions, and interpersonal deficits.
Suicide
- Death from injury with the intent to end life (could be poisoning, suffocation, injury)
Completed suicide - end in death
Suicide attempt - might not end in death
Suicidal ideation - suicidal thoughts
Females make more attempts; men are more successful
reasons include substance abuse; college students feel intense pressure but few seek treatment
CHAPTER 5 - Trauma, Anxiety, OCD and related Disorders
Post-traumatic stress disorder and acute stress disorder
Consequences of experiencing extreme stressors
Diagnostic criteria of DSM-5 requires that individuals:
Directly experience or witness the traumatic event
Learn that the event happened to someone they are close to
Experience repeated or extreme exposure to the details of a traumatic event
Symptoms of PTSD
Repeated experiencing of the traumatic event
Persistent avoidance of situations, thoughts, or memories associated with the trauma
Negative changes in thought and mood associated with the event
Hypervigilance and chronic arousal
PTSD with prominent dissociative symptoms: Result of Dissociation
Dissociation - Different facets of sense of self or consciousness become disconnected from one another
Other Trauma Related Disorders
Acute stress disorder: Occurs in response to traumas similar to those involved in PTSD
Diagnosed when symptoms arise within 1 month of exposure to the stressor and last no longer than 4 weeks
Adjustment disorder: Emotional and behavioral. Symptoms arise within three weeks
Theories of PTSD
Environmental and social factors
Severity and duration, individual's proximity to trauma and amount of social support available
Psychological factors
Pre-existing conditions aggravate susceptibility
Coping strategies influence vulnerability to PSTD
Gender and cross-cultural differences
Women are more prone
African Americans have higher rates of PTSD
Culture influences the manifestation of anxiety
Biological factors:
Neuroimaging findings - Brains of people with
PTSD are more reactive to emotional stimuliBiochemical findings
Physiological responses to stress are exaggerated in
PTSD sufferersExposure to extreme or chronic stress during childhood increases vulnerability
Genetics
Vulnerability to PTSD can be inherited
Treatments of PTSD:
Cognitive-behavioral (exposure therapy, stress-inoculation therapy(teaching skills to overcome problems associated with PTSD))
Biological treatments(drugs) - SSRIs, benzodiazepines
Specific phobias and agoraphobia
Unreasonable or irrational fears of specific objects or situations
Categories according to DSM-5
Animal type
Natural environment typeSituational type
Blood-injection-injury type
Agoraphobia
People fear:
Places where they might have trouble escaping or getting help if they become anxious
That they will embarrass themselves if others notice their symptoms or efforts to escape
In extreme cases individuals do not leave their homes alone
Theories of phobias:
Behavioral:
Negative reinforcement: Reduction of Anxiety reinforced by the avoidance of the feared object;
Prepared classical conditioning: Conditioning of fear to certain objects or situations
Biological:
Related people share phobias
Treatments of phobias:
behavioural treatments
Exposure therapy
Systematic desensitization
Modeling - watch other people interact with the feared object
Flooding
Applied tension technique: increase blood pressure and heart rate to keep people from fainting when feared object is present
biological: benzodiazepines (decreases the anxiety, not that helpful)
Social anxiety disorder
People become anxious in social situations and are afraid of being rejected, judged, or humiliated in public and focused on avoiding such events
More common in women
Develops either in the early preschool or adolescence
Theories of social anxiety
Genetic basis: runs in families
Cognitive perspective: high standards for social performance; focus on negative aspects of social interaction and judge themselves harshly
Treatments for social anxiety disorder
SSRIs; SNRIs; cognitive-behavioural therapy (identifying negative cognitions people have and learning how to dispute those; mindfulness-based interventions
Panic disorder
Occurrences of panic attack become common without being provoked
Panic attack - short but intense periods during which people experience many symptoms of anxiety
People begin to worry about having these attack and change behaviour as a result of worrying
People fear that they have a life threatening illness
Theories of panic disorder
biological: heritability is 43-48%; triggered if sufferers ingest caffeine, inhale a small amount of carbon dioxide; breathe into a paper bag
People with panic disorder tend to pay close attention to their body sensations and interpret them in a negative way; engage in catastrophic thinking; exaggerating sumo
Unproven belief that bodily symptoms are harmful
High awareness that signal a panic attack
Treatments for panic disorder
medication (benzodiazepines) - when discontinued people often experience relapse of symptoms
Cognitive-behavioural therapy: relaxation and breathing exercises; challenging thoughts
Generalized anxiety disorder
GAD - being anxious all the time; worrying about life; women > men
Theories:
emotional and cognitive factors: intense negative emotions; heightened reactivity to emotional stimuli in the amygdala; making maladaptive assumptions; focusing on detection possible threats in the environment in unconscious cognitions
Biological factors: people with generalized anxiety disorder have a deficiency of GABA
Treatment of generalized anxiety disorder
cognitive-behavioural therapy: confronting issues they worry about the most; challenge negative thoughts; developing coping strategies
Biological: benzodiazepine drugs; tricyclic antidepressants and SSRIs (not a long term solution)
Separation anxiety disorder
Separation from caregivers results in anxiousness and being upset
Not diagnosed unless: symptoms last for at least 4 weeks; significantly affects child’s functioning
Theories of separation anxiety:
Biological factors: causes children to be shy, fearful and irritable as toddlers; cautious, quite and introverted as school-age children
Psychological and sociocultural: learn to be anxious from their parents as an understandable response to their environment
Treatments
cognitive-behavioral therapy: teach coping, relaxation exercises to practice when separated; challenge fears about separation
Drugs: antidepressants, anti anxiety drugs, stimulants and antihistamines
Obsessive compulsive disorder
Obsessions- thoughts, images, ideas or impulses that are persistent; uncontrollably intrude upon consciousness; cause significant anxiety or distress
Compulsions - repetitive behaviours or mental acts that an individual feels he or she must perform; different from other stress related diseases and begins at a young age; tends to be chronic if left untreated
Common types of obsessions: thoughts and images associated with aggression, sexuality, and/or religion; symmetry and ordering, matching; contamination and a cleaning compulsion; HOARDING: closely related to OCD but is classified as a separate diagnosis
Hair-pulling disorder - trichotillomania
Skin-picking disorder - often become infected, causing significant distress
Body dysmorphic disorder
Theories
biological: good response to medication; genes help determine who is vulnerable to OCD
People who develop: depressed, usually anxious; tendency of rigid moralistic thinking; believe inability to control their thoughts; compulsions develop largely through operant conditioning
Treatments
biological: antidepressants, serotonin enhancing drugs (significant side effects)
cognitive-behavioural treatments: exposure therapy to focus on the obsession to prevent compulsive responses; challenging moralistic thoughts, excessive sense of responsibility and maladaptive cognitions