FAL CASES TO NOTE
Apical Pneumothorax: Air collection in lung apex, causing respiratory distress.
Collapse of apical lung segment due to cervical pleura puncture.
Caused by puncture during central line placement/shifting.
Presentation: Shortness of breath, elevated heart rate, respiratory rate, agitation, pulse-ox > 92\%.
Radiograph confirms receding line of visceral pleura.
Treatment: Needle thoracocentesis, chest tube.
Case: A 64-year-old female with severe depression had become dehydrated after a prolonged period of self-starvation and refusal to drink. In order to rehydrate the woman, a central line was place in the subclavian vein for administration of a rehydration solution. The patient showed improvement over a period of 2 days, then suddenly developed tachypnea, cyanosis, tachycardia, and hypotension. Blood work and a chest film was ordered. What caused the sudden onset of the above symptoms?
Hemothorax: Accumulation of blood in the pleural space (between parietal/visceral pleura).
Due to tearing of blood vessels in/around pleural cavity (e.g., intercostal arteries/veins).
Presentation: Similar to pneumothorax; may also have referred pain from diaphragm irritation.
Treatment: Thoracocentesis, chest tube, ligation of source of bleed.
Case: While standing on the sidelines, Drew Bledsoe demonstrated untypical restlessness and agitation, and was assessed further in the locker room. As he was packing his belongings, he kept complaining about a painful shoulder. The doctors felt something was not quit right, and so sent him for a consultation with an internist at Mass General.
Pulmonary Embolism: Obstruction of pulmonary artery by blood clot.
Partial/complete blockage of one or more bronchiopulmonary segments by a blood clot.
Commonly results from venous stasis (e.g., bed rest).
Responsible for 10\% - 15\% of deaths in hospital.
Also seen in some traumas, clotting disorders.
Significant blood backup may result in cor pulmonale (right-sided heart failure) and circulatory collapse.
Saddle embolus: Partial/complete obstruction of pulmonary trunk (right/left pulmonary arteries).
Case #3: A 59-year-old man with a history of hypertension presents for an elective subtotal colectomy for colon cancer. The procedure is successful, without any signs of complication. His immediate postoperative state is stable, but on postoperative day 4 he develops sudden-onset shortness of breath. He denies having any chest pain, palpitations, nausea, or diaphoresis (excessive sweating). On physical examination, his blood pressure is 138/68 mm Hg; his pulse is regular, with a rate of 110 beats/min, and his respiratory rate is 30 breaths/min. His temperature is 97.7°F and his oxygen saturation is 92% on room air, which improves to 98% on 2 L of oxygen via nasal cannula. He is in mild respiratory distress but is able to speak in full sentences. He is not recruiting the accessory muscles of respiration. The examination of his head and neck is normal. He has mildly decreased breath sounds at his right lung base. His heart sounds are normal. His abdomen is soft, nontender, and mildly distended with good bowel sounds; a midline incision scar is clean and nontender. He has palpable peripheral arterial pulses in his upper and lower extremities. The patient did not have edema or tenderness in the lower extremities. Laboratory blood tests are normal. An arterial blood gas on room air demonstrates a pH of 7.45, a pCO2 of 32 mm Hg, and a pO2 of 62 mm Hg, with an oxygen saturation of 93%. A chest x-ray reveals bibasilar subsegmental atelectasis. He receives a treatment session with a respiratory therapist, but his condition continues to deteriorate. On postoperative day 5 his oxygen saturation declines despite supplemental oxygen and he is intubated for hypoxemic respiratory distress. He is transferred to the ICU.
Chronic Obstructive Pulmonary Disease (COPD): Irreversible airflow obstruction.
May involve one or more of the following:
Chronic bronchitis: Productive cough \ge 3 months for \ge 2 consecutive years.
Emphysema: Damage/fibrosis of alveolar sacs, breakdown of endothelial wall; visible sac-like spaces.
Asthma: Airway restriction from smooth muscle constriction.
Symptoms: Characterized by chronic cough (worse in mornings), sputum production, dyspnea, and weight loss.
May also notice clubbed fingers and barrel-chested appearance.
Strong direct relationship with smoking history.
Chronic condition worsened by exacerbations/comorbidities (e.g., infections, inflammation).
Treatment: Supplemental oxygen, respiratory therapy, home modifications.
Case #4: After receiving health insurance through the affordable care act, a 55-year-old man is encouraged by his wife to see a family physician for a check-up for the first time in over a decade. The physician assistant noted that the man spent several minutes taking deep breaths and expiring through pursed lips while sitting in a tripod position when he came in the room, but that this subsided over time. During the physical, the physician notices a barrel chested appearance and that his fingernails have a distinct rounded appearance to them. The physician also notices a bluish tinge to the patient’s lips. Body temperature is 98.0\degree C. Blood pressure is 138/85 mmHg, Heart rate is 90 BPM and respiratory rate is 25 breaths per minute. Auscultation is relatively normal, except for Rhonchi in the vicinity of the secondary bronchi. The physician inquires into the patients medical history. He describes a 60-pack-year history of smoking and a “smoker’s cough” that is typically worse when he first wakes up in the morning. Aside from the normal problems that happen with aging, the patients describes himself as being in “pretty good health, all things considered”.
Endocarditis: Inflammation of the inner layer of the heart, commonly caused by bacterial infection, presenting with symptoms such as fever, chills, and heart murmur.
Mitral valve Prolaspse/ Regurgitation: A condition where the mitral valve does not close properly, leading to blood flowing backward into the left atrium, which may cause symptoms like palpitations, shortness of breath, and fatigue.
Most common/ valve prolapse produce clicking sound on auscultation as the valve snap upward
Valve stenosis: Narrowing of the valve opening, which restricts blood flow and can lead to symptoms such as chest pain, fatigue, and heart failure.
diminished stroke volume
Coronary artery Disease: A condition characterized by the narrowing or blockage of the coronary arteries, often due to atherosclerosis, that can result in chest pain, shortness of breath, and may lead to heart attacks.
blockage of the coronary vessels
angia pectoris: A type of chest pain caused by reduced blood flow to the heart muscle, often resulting from coronary artery disease.
Angioplasty: A minimally invasive procedure used to open up narrowed or blocked coronary arteries, typically involving the insertion of a balloon catheter and often accompanied by stent placement to help keep the artery open.
Myocardial Infarction: A condition resulting from the interruption of blood supply to the heart muscle, commonly known as a heart attack, which can occur due to prolonged angina or serious blockages in the coronary arteries.
plaque breaks off result in deficiency in oxygen supplies and heart tissue become narcotic or die
Heart failure: A condition where the heart is unable to pump sufficient blood to meet the body's needs, often resulting from damage caused by a myocardial infarction or chronic high blood pressure.
heart do not pump enough blood, to keep up with returning from venous circulation , this lead to pulmonary edima and fluid accumulation in lung.
Fluid accumulation in the pericardial sac: prevent diastolic filling, or low stroke volume
Cardiac tamponade: Compression of heart by accumulating pericardial contents. can have gradaul or rapid onset
SA node- pace maker of heart = p wave in conduction system
p wave : Electrocardiographic deflection representing atrial depolarization; essential for initiating cardiac contractions.
QRX complex: Electrocardiographic representation of ventricular depolarization; it follows the P wave and is critical for the contraction of the ventricles.
T wave: The T wave represents ventricular repolarization, indicating the recovery phase of the ventricles after contraction.
Purkinjie fiber: ventricular depolariziation
Etiopic Pacemakers (PVCs): purknjie fiber jump first and make heart skip a bit
Vagus n. gives off left and right reccurent laryngeal n.. if left is injured you can have hoarseness or vocal cord paralysis.
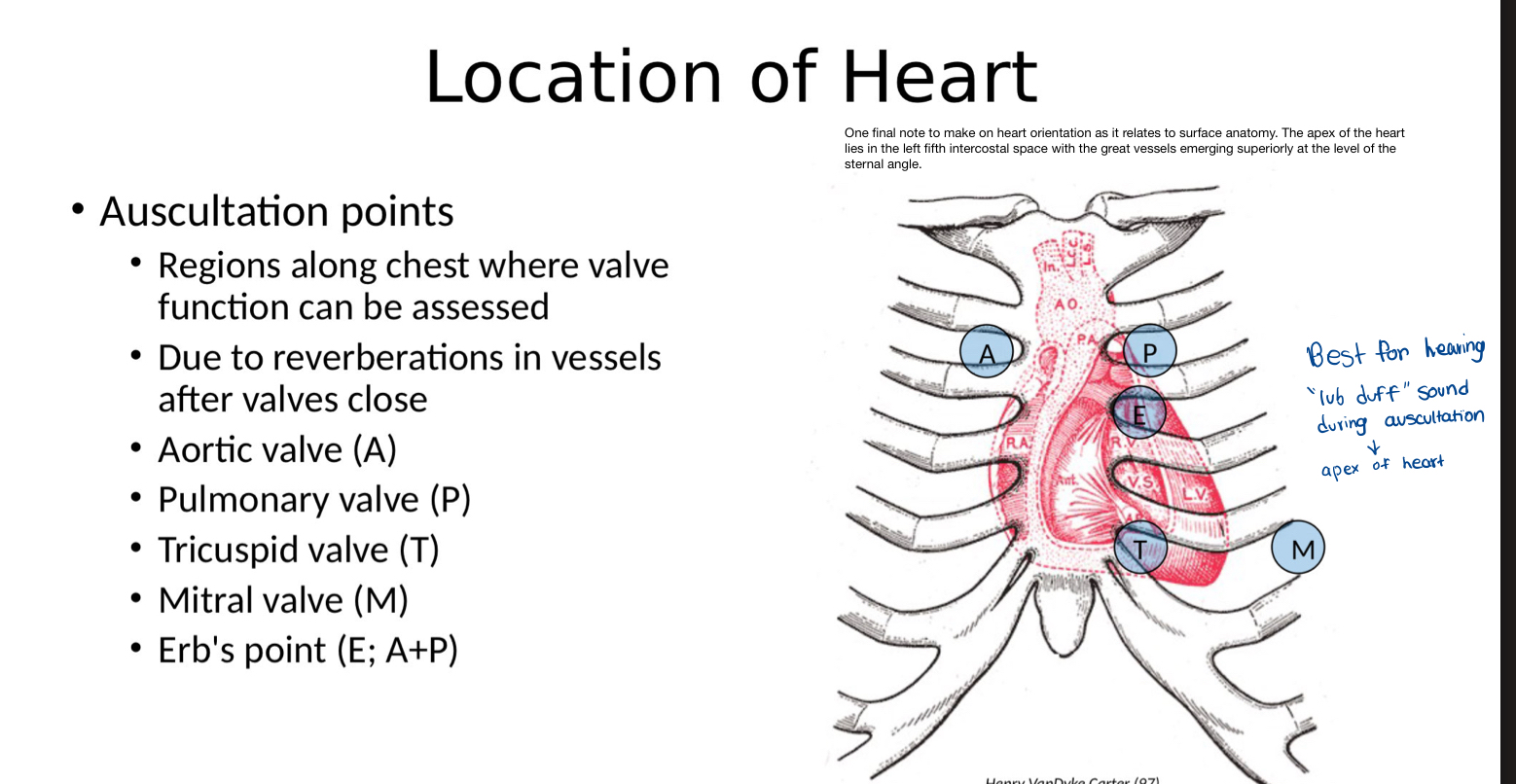
Q1: A patient comes in for his yearly physical, which involves
listening to the heart sounds with a stethescope. At
which location are you most likely to hear a "lub-duff"
sound?Right 2nd intercostal space
Q2: A 7-month pregnant female comes goes to her
OBGYN for a routine check up, the doctor notices
that there appears to be more blood in the lungs
than normal. Which structure is there a potential
problem with?ductus arteriosus
Fetal circulation reason
Q3: What part of the conduction system is abnormal?

SA node
Q4: What part of the conduction system is abnormal
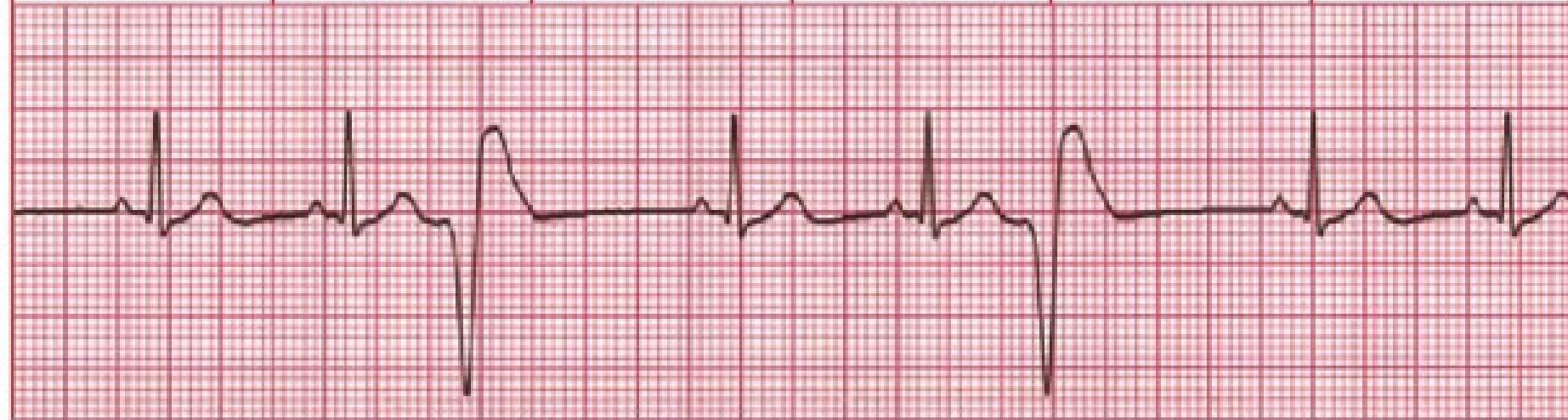
Purkinje fiber
V-Fib:This condition arises when the ventricles experience chaotic electrical activity, leading to ineffective contractions and no useful blood flow, requiring immediate medical intervention.
Q5: A 45 year old woman presents to her family physician. An avid runner,
she has been noticing a progressive decrease in exercise performance
over the past year. She originally attributed this to the effects of aging.
During a group run earlier in the week, however, she was forced to pull
back, and one of her running mates who chose to stay with her became
alarmed to notice a blue tinge develop around the patient’s lips. A
thorough history reveals that the patient has also become susceptible
to dizzy spells, and recalls several moments of almost passing out,
particularly after coughing spells. Among other things, the physician
orders cardiac ultrasonography...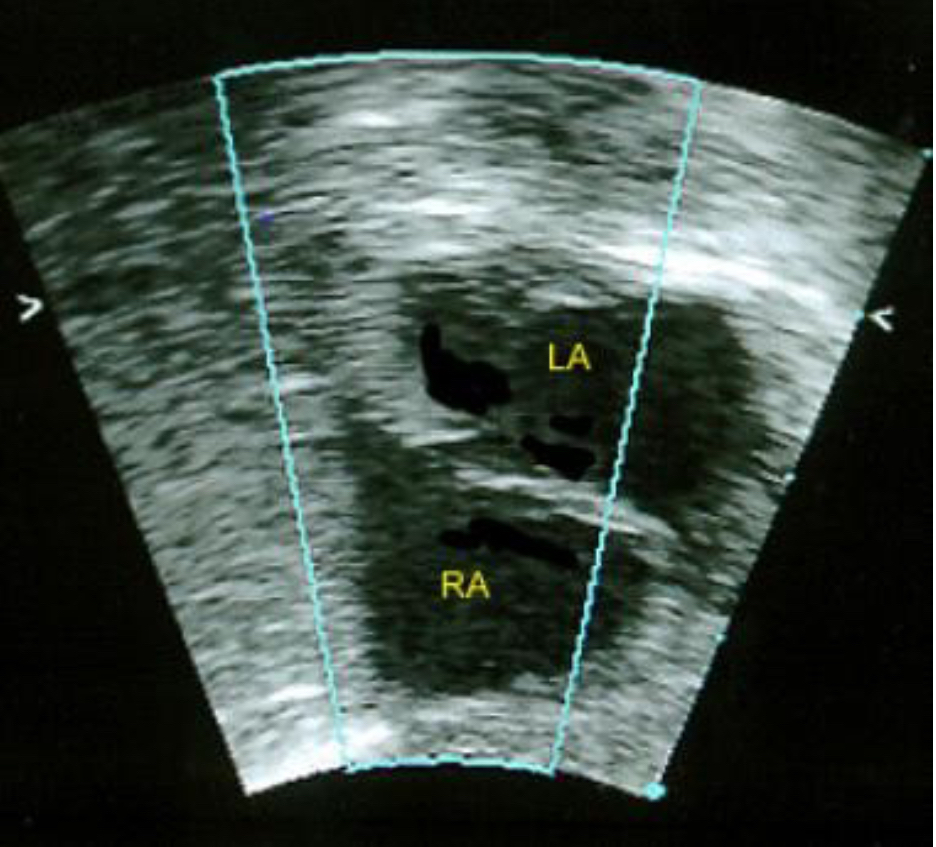
Hole in Atrial Septum / Patent Foramen Ovale (Q5): A patient with progressive decrease in exercise performance, dizzy spells, syncope (fainting) often exacerbated by coughing, and a bluish tinge to the lips. This points to a heart defect where there's an incomplete sealing of the foramen ovale, allowing blood shunting.
Q6: • Four days following a two-vessel coronary artery bypass graft (CABG) procedure and replacement of a mitral valve, a 69-year-old woman
presented with a chief complaint of shortness of breath, inability to
lie supine, oliguria, and overt weakness. Her pulse is 120 beats/min,
respirations are 30 breaths/min, and blood pressure is 70/40 mm Hg.
Jugular venous distention is noted. Breath sounds are normal. Heart
sounds are not audible. The ER physicians order an ultrasound of the
mediastinum...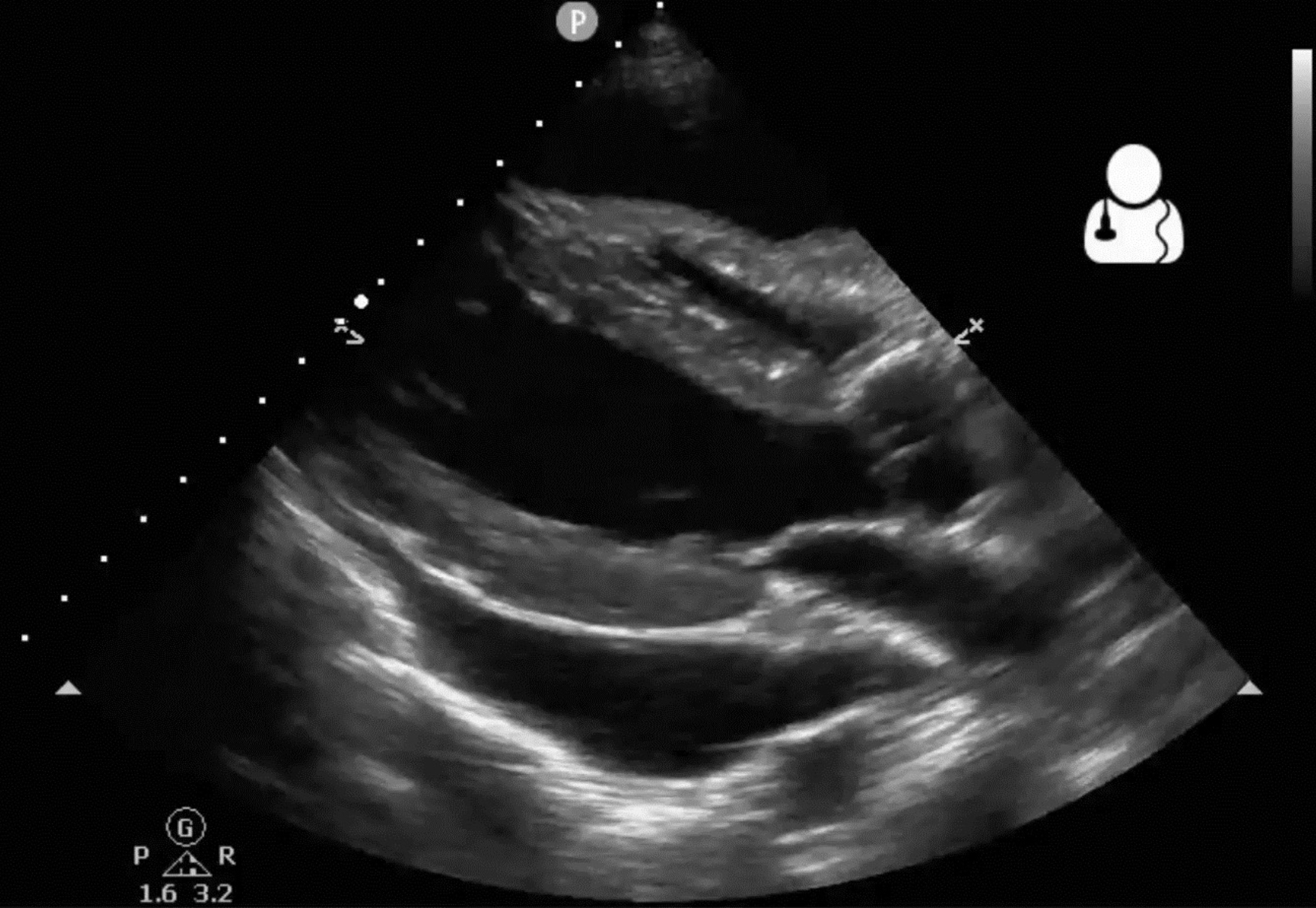
Fibrosis of aortic semilunar valve
Cardiac Tamponade (Q6): A patient post-cardiac surgery presenting with sudden shortness of breath, inability to lie flat, low blood pressure, high heart rate, jugular venous distention, and muffled heart sounds. These are classic signs of fluid accumulation in the pericardial sac compressing the heart.
Q1: Frank, a 59-year-old man is brought to the ER by his wife, Erma. The
couple had been sitting out on the front porch of their home enjoying
the sunset when the man started to experience the gradual onset of
chest pain. Fearing a heart attack, the wife insisted they visit the local
emergency room. The patient describes a burning sensation in the
midthoracic region. The doctor also notes that couple has been arguing
about the husband sitting in the chair; Erma wants the husband to lie
down, but Frank insists that this makes the pain worse.Regurgitation of stomach contents into esophagus
Gastroesophageal Reflux Disease(GERD): Iritation of the lower esophageal lining due to reflux of stomach contents into esophagus
• Causes
• Weak/inactive cardiac sphincter
• Hiatal herniation
• Due to differences in endothelial lining
of esophagus vs. stomach
Q2: An 83-year-old male is brought to the emergency room by his
distraught daughter. The patient is a widow, having lost his wife of 55 years to an acute MI 3 years earlier. He speaks with his daughter, who lives several hours away, over the phone every few days. In recent months, the patient has complained to his daughter about feeling constantly nauseated, especially after eating. While the daughter expressed concern, the patient said it was likely nothing serious, as he was not running a temperature. Two weeks ago the symptoms progress to a complete loss of appetite and vomiting when he did attempt to eat. The daughter became increasing concerned at the lack of improvement and decided to come out to see him. Upon her arrival, she is alarmed by her father’s appearance and immediately rushes him to the ER for assessment. An MRI and CBC are ordered.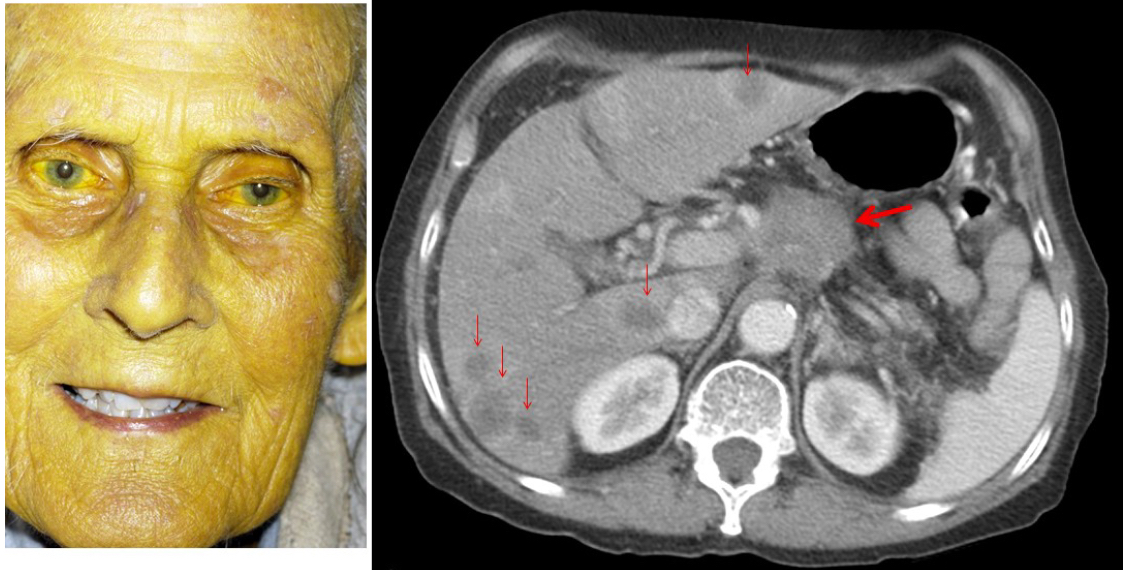
metastatic pancreatic cancer:
Pancreatic adenocarcinoma
• Affecting the exocrine cells
(producing digestive enzymes)
• >80% of cases
• >60% found in pancreatic head
• Tumor can impact other tissues
• Duodenum – loss of appetite,
vomiting
• Common bile duct – jaundice
• Pancreatic duct – acute
pancreatitis
Q3: A 53-year-old man appeared in the ER complaining of pain and
distension in his abdomen that had progressed over the past several
days. He had originally attributed the pain to indigestion and bloating,
but has become concerned that the bloating has continued to increase,
despite not eating. During the patient history, the man admits to eating
fast foot takeout almost every day, and to smoking a pack of cigarettes
and drinking a liter of burbon on an almost daily basis going on 20
years. Inspection of the abdomen reveals distension and the
prominence of the superficial veins.
Destruction and Scaring of the liver
Liver Cirrosis: Scarring of liver tissue due to chronic cycles of inflammation, tissue regeneration
• Causes
• Hepatitis B/C – 60%
• Alcohol – 20%
• Many other causesTypically leads to portal hypertension
• Acitis – accumulation of fluid in
peritoneal cavity
• Caput medusae – varicosities in
campers fascia, due to redirection
of blood through paraumbilical,
superior rectal veins
Q1: A 52 year old male presented to the emergency department with severe left flank pain radiating to the right lower quadrant. His blood pressure was 154/96, pulse rate was 79 bpm, respiratory rate was 24 breadths per minute and temperature was 36.7° C. The pain was insidious in onset and had an intensity of 10/10 on verbal analog scale which decreased to 8/10 after administration of Toradol and Morphine medications provided in the emergency department. The pain was constant, lasting 3 hours in duration, and he had two episodes of vomiting since its onset. He did not report experiencing any chest pain, dyspnea, fever or bowel and bladder dysfunction. His heart rate and respiration were within normal limits. He did not display any signs of edema or nausea, abdominal discomfort or indigestion. His abdomen was soft with diffuse tenderness, which increased over the right lower quadrant. Urinalysis revealed a moderate increase in specific gravity (1.030), significant hematuria (3+) and a trace of protein.
Kidney stone on left renal pelvis (Urethrolothiasis):
• a.k.a kidney stones
• Presentation
• Sudden onset of sever pain originating in flank
• Pain related to dilation, stretching, spasm of
ureter
• “loin to groin” progression as kidney passes
• Diagnosis
• Can be made on clinical presentation along,
although imaging commonly done
• Treatment
• Control pain while stone passes (>80%)
• More serious cases (unrelenting pain, UTIs)
may require drainage with a stent or
percutaneous nephrostomy
Q2: Following the treatment for his kidney stone, the same patient returns to the clinic 3 weeks later with a similar pain presentation. The patient explains that the pain had had a more gradual onset than before, and had suddenly worsened this morning, accompanied with feelings of lightheadedness and weakness. The patient’s vital signs at presentation were: heart rate, 96 beats/minute; blood pressure, 133/76 mm Hg; respiratory rate, 20 breaths/minute; and temperature, 98.9 ̊F. Oxygen saturation was 98% on room air. On physical examination, the patient had left lower quadrant pain and left costovertebral angle tenderness. Plain film radiographs showed nothing of significance. Laboratory studies were remarkable for a hemoglobin level of 6.8 g/dL, and a hematocrit of 21.1%. Based on the patient’s history and symptoms, axial and coronal computed tomography (CT) scans were ordered...
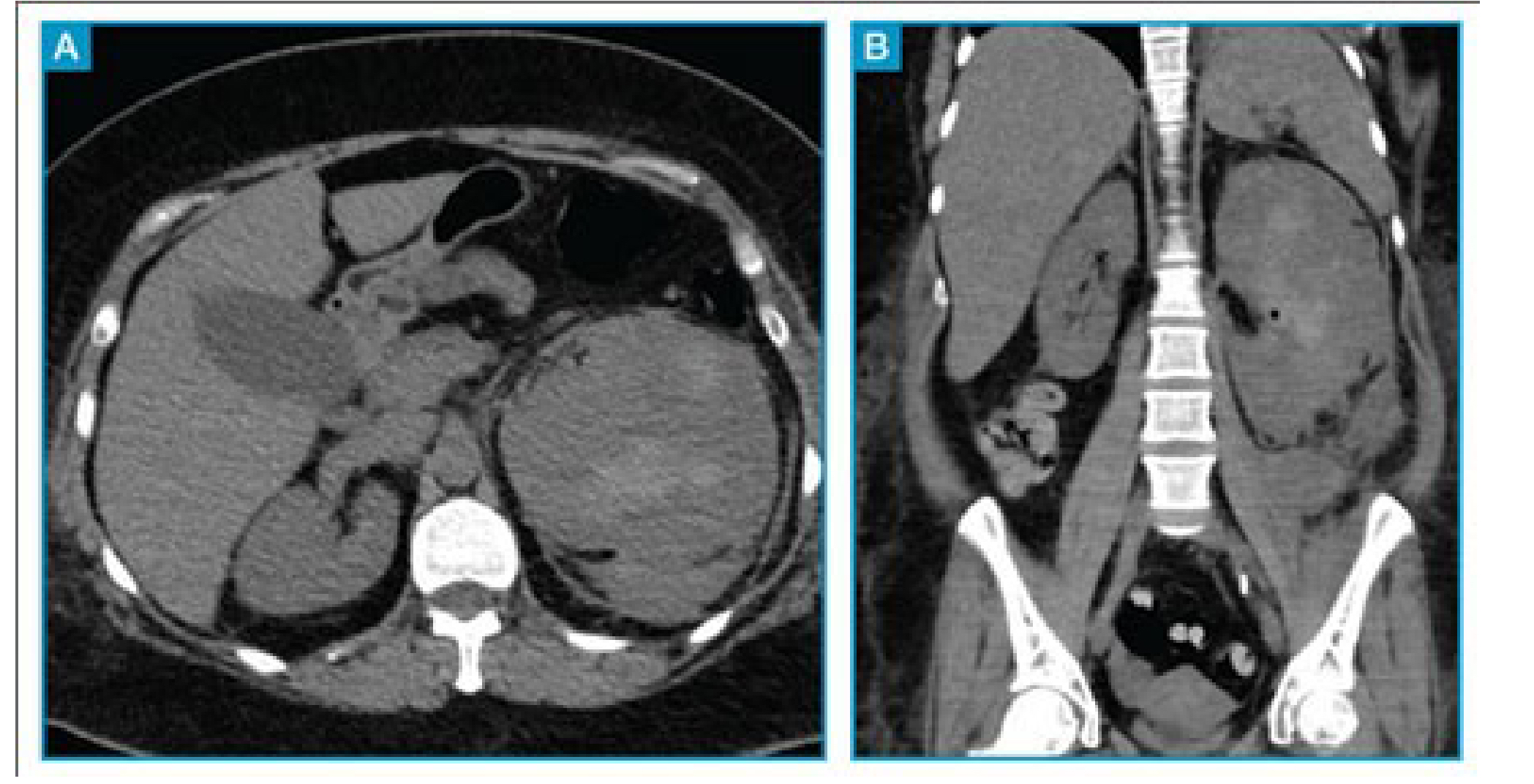
Ruptured renal Calyx: Back-up of fluid, pressure within the renal pelvis, which may ultimately progress to tissue rupture
• Causes
• Unresolved ureterolithiasis (>4wks)
• Typically smaller stones
• Narrowing, scarring of ureter due to previous ureterolithiasis
• Compression from AAA, abdominal tumors
• Results in extravasation of blood urine into peritoneal cavity
• Typically confined to perirenal space
• Treatment
• Identification, treatment of cause
• Ureteric stent
• Conservative treatment as tissue heals
• Monitor for infection
Q3: An 85-year-old man is presented to the emergency department (ED) by
ambulance with severe abdominal pain that began suddenly 2 hours before
presentation. The pain is mainly in his back and radiates toward his left inguinal region. The patient felt light-headed at the onset of the pain to the extent that he had to grip the sink to steady himself. He also reports significant nausea, although he has not vomited. He has no urinary symptoms. His medical history includes type 2 diabetes, hypertension, hyperlipidemia, ischemic heart disease, and intermittent claudication (cramping pain) of his lower extremities. He smoked 10-20 cigarettes a day for over 60 years but stopped 5 years ago.The physical examination reveals tenderness in the left iliac fossa and lef tcostovertebral angle. His vital signs are remarkable for a heart rate of 105 beats/min and a blood pressure of 110/90 mm Hg. An abdominal CT is taken.
ruptured abdominal aortic aneurism: Relatively common
• Men > 65 at greatest risk
• Presentation
• Syncope (fainting)
• Sudden, severe, constant back/flank/abdominal/groin pain
• Pulsatile sensation in lower abdominal area
• Diagnosis
• Palpation sufficient, but angiography better characterizes
• Treatment
• Small sized aneurysms monitored for progression
• Low rupture risk
• Sufficiently large AAA require aortic stents to reinforce wall
• AAA rupture represents medical emergency
• ~65% of ruptures result in cardiovascular collapse, death before
patient arrives at hospital
Q1: A 48 year old woman reports to the ER complaining of severe pain in
her shoulder that is beginning to radiate down her arm. During the
physical examination the physician notices a firm mass in her right
anterior neck and dilation of the external jugular vein (see video).
Palpation of the mass creates a pins and needles sensation down her
arm. The physician also notices that the patient’s right eyelid is
drooping. Shining a penlight in the patient’s eyes, she notices that the
right pupil is fixed and constricted. A plain film radiograph is ordered.Apical lung Cancer: Pancoast Tumor: Pulmonary neoplasms at pleuropulmonary
groove
• Leads to compression of structures within
neck, thoracic inlet
• Presentation
• Shoulder/axillary pain, ultimately radiating into
the upper limb
• Atrophy of upper limb musculature
• Impingement of brachial plexus
• Horner’s syndrome (drooping eyelid, constricted
pupil, hemianhidrosis)
• Impingement of sympathetic chain
Q2: A patient makes an appointment with
his family physician searching for a treatment for laryngitis. The physician
uses a laryngoscope to view the vocal folds, and is surprised to note that there is no discernable inflammation. The physician asks the patient to alternate between saying “aaah” and taking deep breaths and notes that the left vocal fold does not move properly with the right (see video). Among other tests, the doctor refers the patient for angiography. What artery is the doctor interested in viewing?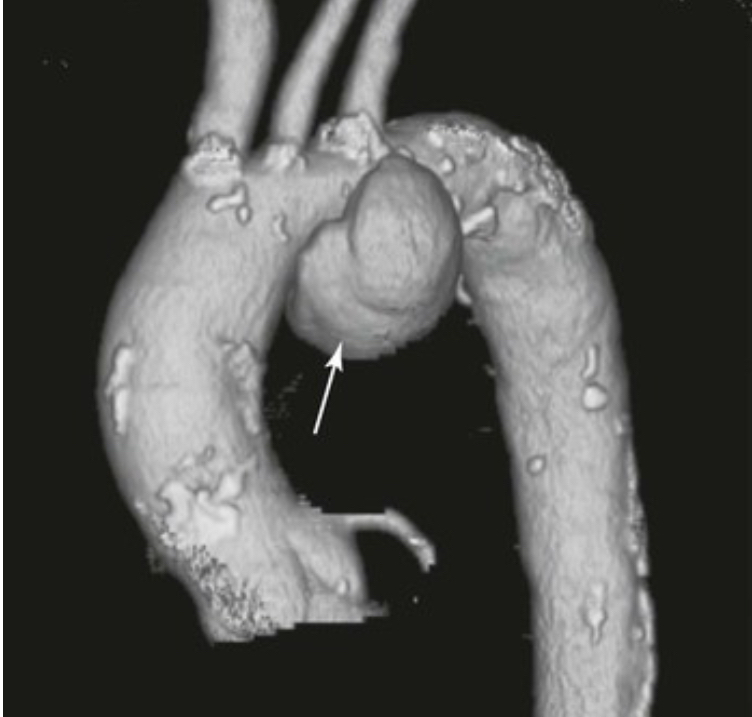
Aortic arch
Aortic arch aneurysm: Aneurysmal dilatation of the arch of the aorta(>50% normal diameter)
• Likely to impinge on left
recurrent laryngeal nerve
• Hemiparalysis of left vocal fold
• Red flag for aneurysm, left lung
tumor
Q3: A woman experiences difficulty during a vaginal childbirth in the
maternity ward of a local hospital. During delivery, the child’s left
shoulder becomes caught at the level of the symphysis pubis. After
much manipulation, the obstetrician is able to clear the shoulder through
the birth canal, and the delivery progresses normally. APGAR scores are within normal levels, and the baby appears healthy, with the exception of a slight cyanotic appearance. A ultrasound is ordered, and no abnormalities are found in heart wall structures. The cyanotic appearance persists in the weeks following delivery, and during a follow up visit, the physician notes diminished breath sounds over the entire left lung. A fluoroscopic analysis is performed...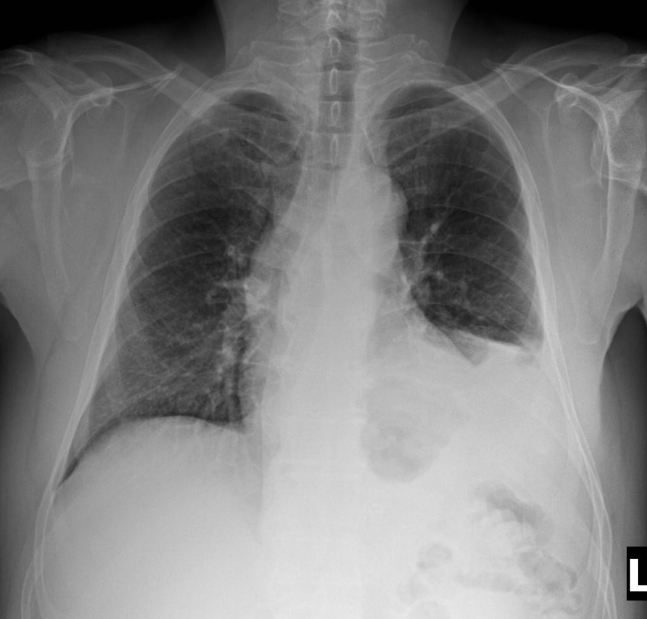
paralysis on the left side of diaphragm
Phrenic Nerve Lesion: Relatively uncommon condition
• May be unilateral or bilateral
• Causes
• Surgical injury
• Pressure from tumors, aneurysms, etct.
• inflammatory
• Unilateral lesion results in diaphragm
hemiparalysis
• Paradoxical breathing pattern
• Paralyzed side moves up during inspiration,
due to pressure from abdominal organs
Q1: A 32-year-old man was referred to a rehabilitation clinic with left shoulder
dysfunction. The physical therapist identifies weakness with shoulder elevation
and develops a rehabilitation program for the patient. Two weeks into treatment,
the patient calls to reschedule a session due to a conflicting doctor’s appointment.
The patient explains in the following session that he was also referred to an ENT
specialist, due to sore throat, left earache, hoarseness, and swallowing difficulty,
which developed three weeks prior to the left shoulder issues. The PT consults
with the ENT physician about his own assessment and learns that the patient’s left
vocal cord was hypomobile, that he showed an impaired gag reflex on the left side
and deviation of the uvula to the right side. There was no impairment of facial
sensation and motion, no tongue deviation or nystagmus. The PT begins to believeCN VIII, CN IX, CN X
Jugular Foramen syndrome: a.k.a Vernet syndrome
• Impingement of the jugular foramen
• Paraganglioma tumors
• Other forms of malignant/benign tumors
• Trauma
• Infection
• Bone diseases
• Presentation
• Dysphonia (CNX)
• Uvula deviation (CNX)
• Loss of sense/taste over posterior 1/3rd of
tongue (CNIX)
• Loss of gag reflex (CNIX/CNX reflex loop)
• Shoulder droop/weakness (CNXI)that the patient’s diverse medical complaints can all be attributed to a single
medical condition affecting 3 different cranial nerves.
Q2: A 46-year-old man was referred to a neurology clinic with a 2-year history of recurrent
vertigo. During the first attack, an initial period of acute severe vertigo lasting several
minutes was immediately followed by sensorineural hearing loss and imbalance. The patient
was treated with intravenous infusions and symptoms resolved completely. The second
episode of severe vertigo occurred 18 months later, accompanied by right-sided aural
fullness and high-frequency nonpulsatile tinnitus, this time without hearing impairment. Six
months after the second episode, the patient started to suffer from recurrent episodes of
severe vertigo lasting from several minutes to hours, which were incapacitating and
significantly impaired the patient's ability to work or carry on with his regular activities.
Symptoms were lessened with bed rest. Both frequency and intensity of the vertigo attacks
increased over the following months. Two months ago the attacks occurred at least several
times a week, sometimes daily. The patient is also contending with persistent fluctuating
high-frequency tinnitus and increasing aural fullness on the right side. All other aspects of
his neurological examination was normal. Audiometric testing showed no significant hearing
impairment and vestibular testing was normal.CNVIII
Vestibulocochlear Nerve Compression/Lesion: Causes
• Tumor
• Ménière's disease (MD)
• Microvascular compression
• Temporal bone fracture
• Symptoms
• Hearing loss, tinnitus
• Vertigo
• Loss of equilibrium
Q3: