GI Disorders
GI Disorders Overview
Focus on peritonitis, bowel obstructions, ostomy, pancreatitis, and biliary tract diseases.
Learning Objectives
Describe the interprofessional and nursing management of peritonitis.
Distinguish among small and large bowel obstructions, including causes, clinical manifestations, and interprofessional and nursing management
Select nursing interventions to manage the care of the patient after bowel resection and ostomy surgery.
Key Terms
Acute Pancreatitis, Bowel Obstruction, Cholecystitis, Cholelithiasis, Chronic Pancreatitis, ERCP, Fistula, Jaundice, Ostomy, Paralytic Ileus, Peritonitis.
Peritonitis
Etiology and Pathophysiology
Inflammation of the peritoneum due to contamination of bacteria/infection or irritating chemicals (peritoneum lines abdominal cavity). Can kill someone within 6 hours if untreated.
Irritating Chemical: Blood, hydrochloric acid (should stay within GI tract/stomach acid), etc.
Causes:
Primary: Blood-borne organisms (virus, bacteria, infection).
Ex. Ascites from cirrhosis/liver failure → accumulation of fluid in the abdominal cavity allows bacteria to grow → infection.
Kidney failure → accumulation of toxins and fluid imbalances → infection.
Secondary: Organ perforation (leakage into the peritoneum from organs/anything that ruptures).
Ex. Ruptured appendix, stab wound, peritoneal dialysis (bad catheter care), ulcer perforation, diverticulitis.
Pathophysiology: Initial chemical irritation (peritonitis) can progress to bacterial peritonitis → fluid shifts and adhesions.
Contents (chemicals) irritate the peritoneum and activate the compliment system. WBCs and fluid move toward site of irritation from intravascular fluid → adhesions develop → peritonitis.
Clinical Manifestations Peritonitis
Severe, continuous RUQ abdominal pain—most common symptom.
Rebound tenderness, rigidity/board-like abdomen, guarding, and spasm - common.
Other symptoms: Shallow breathing (fluid shift), tenderness over area, fever, tachycardia, shallow breathing, nausea, vomiting, altered bowel habits.
Potential complications: Hypovolemic shock (fluid shift into peritoneum & decreased perfusion), sepsis (lactic acid buildup/system response), intra-abdominal abscess (pus) (adhesions), paralytic ileus (volume sitting on top → temporary blockage of food and gas in the digestive tract), ARDS (fluid in air sacs from fluid shift of ascites and immune response).
Diagnostic Studies
Involves history & physical examination (H & P), CBC, CMP, imaging tests (US, x-ray, CT), BUN & creatinine, GFR, and peritoneoscopy.
H&P: Peritoneal dialysis? Normal process? At home or clinic? (H&P)
Hematocrit (fluid shift) may be falsely elevated → look at RBCs and hemoglobin to see if pt is bleeding.
Interprofessional Care
Perforation requires immediate surgical intervention.
Preoperative (mild cases or poor surgical risk): NPO, NG suction (intermittent), IV fluids, antibiotics, analgesics, antiemetics (Zofran).
Often used as early intervention methods.
Postoperative: Similar to preoperative care with additional monitoring and parenteral nutrition.
Nursing Management
Vital sign monitoring (I&Os, O2 needs)
IV access (18 G or sometimes a 20 G for blood if needed)
Pain management
NPO; NG tube to low & intermittent suction
Monitor fluid and electrolyte balance.
Assess for worsening symptoms (sepsis, peritonitis spread).
Emotional support.
Drain care (if one is placed)
Intestinal Obstruction
Simple: Intact blood supply
Strangulated: No bloody supply
GI System Review:
Stomach: Digestion in two ways: mechanical (movement) and chemical (hydrochloric acid/stomach acid and pepsin digestive enzyme). Produces intrinsic factor (needed for absorption of B12).
Small Intestine:
Duodenum: Absorbs minerals (iron, calcium, magnesium) and is where stomach contents meet pancreatic and liver enzymes to neutralize acid.
Jejunum: Absorbs nutrients (water soluble vitamins like B complex and C), sugar, and fats.
Ileum: Absorbs amino acids, fat-soluble vitamins (ADEK), vitamin B12, and has patches apart of immune system to protect against pathogens.
Large Intestine: Water absorption and mucus secretion.
Pts with a colostomy will still pass mucus and it will feel like a bowel movement (option to have anus sewn shut if too much).
Types and Causes (mechanical vs nonmechanical)
Small Bowel Obstruction (SBO):
Mechanical (physical obstruction blocking movement): Surgical adhesions aka scar tissue (most common), hernias, Crohn’s disease (strictures), cancer, intussusception (blockage from intestine telescoping into another).
Ask about prior abdominal surgeries.
Nonmechanical (reduced or absent peristalsis): Paralytic ileus (most common), vascular emboli.
Large Bowel Obstruction (LBO):
Mechanical (physical obstruction blocking movement): Colorectal cancer/CRC and diverticular disease (most common), volvulus (intestine folds onto itself), adhesions (scar tissue), ischemia, Crohn’s disease.
Diverticular disease includes diverticulosis (diverticula/small pouches protruding in the colon) and diverticulitis (diverticula become inflamed or infected).
Nonmechanical (reduced or absent peristalsis): Pseudo-obstruction (impaired peristalsis w/out obstruction), paralytic ileus, vascular emboli.
Most mechanical obstructions occur in the small intestine.
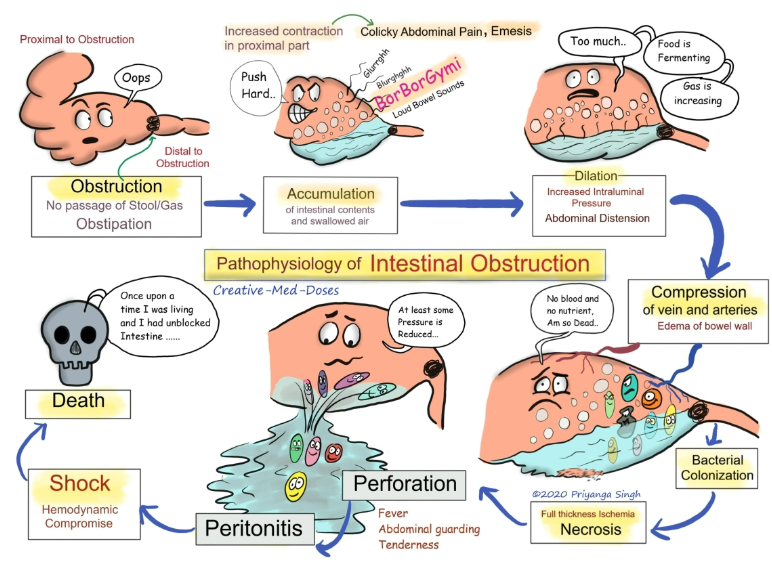
Pathophysiology for SBO and LBO: Fluid, gas, and intestinal contents back up proximally (right before site) of the obstruction and reduces fluid absorption and stimulates intestinal secretions (hydrochloric acid, pancreatic enzymes, etc).
Results in proximal bowel distension → reduces fluid absorption and stimulates intestinal secretion → Distal bowel empties and collapses (determines partial/full)→ Pressure in bowel lumen → increased capillary permeability (fluid moving out) → fluid leaks into the peritoneal cavity (peritonitis risk) → decreased circulating BV → hypotension and hypovolemic shock→ Bowel becomes edematous and ischemic (lactic acid increased from tissue breakdown) → Gangrene and necrosis → Perforation of the bowel wall → peritonitis and severe systemic infection.
Perforation requires immediate surgical intervention.
Nonmechanical Obstruction Subtypes
Paralytic ileus (most common): Lack of intestinal peristalsis and bowel sounds.
Causes: Abdominal surgery (bowel and bladder last two things to wake up after surgery); peritonitis; inflammatory disorders; electrolyte imbalances (potassium/hypokalemia; potassium moves smooth muscle → Lasix is a risk factor); thoracic or lumbar spinal fractures (those nerves go into GI system).
Antispasmodics/ Anticholinergics contraindicated.
Usually affects both intestines.
Pseudo-obstruction (rare): Impaired peristalsis with no actual obstruction and mainly affects large intestine only.
Causes: Neurologic conditions, drugs, endocrine and metabolic problems, lung disease, trauma, or burns.
Vascular obstruction: Emboli or thrombi alter blood supply to a part of the intestines.
Clinical Manifestations of Bowel Obstruction
Hallmark Symptoms (Order depends on cause and obstruction):
1. Abdominal pain
2. N/V (may be projectile)
3. Distention
4. Constipation (may be nothing there)
** Bowel sounds may be high pitched (above obstruction), absent (paralytic ileus), or hypoactive (LBO).
Feature | Small Bowel | Large Bowel |
|---|---|---|
Onset | Rapid (Smaller lumen/tube) | Gradual (larger lumen/tube) |
Vomiting | Frequent, (copious) bile-stained or fecal (if proximal; ileum smells of stool) | Rare |
Pain | Colicky, intermittent (mid to upper abdomen → xiphoid) | Persistent, crampy (lower abdominal pain) |
Distention | Minimal if proximal, severe if distal (at ileum) → possible projectile vomiting. | Noticeable (because more vascular as more water absorption occurs) |
Constipation | May pass stool early | No stool/Obstipation (complete obstruction vs partial) |
Interprofessional and Nursing Management (least invasive → most invasive, unless emergency)
Conservative Management (Preferred if paralytic ileus or early bowel obstruction):
NG Tube for Decompression (hallmark treatment)
Monitor I&Os (30mL/hr normal) / electrolytes / acid-base
Reduces bowel distention and risk of edema, necrosis, and perforation.
Measurement: Nares → earlobe → xiphoid process
IV Fluids (D10W or D5W & Electrolyte Replenishment.
Dehydration Sign: Dry mucous membranes, decreased skin turgor, BP, tachycardia, and low urine output.
NPO Status.
Paralytic ileus and adhesion-related obstructions often resolve without surgical intervention.
Acid-Base Imbalances:
◦ Metabolic alkalosis – high obstruction (from vomiting a lot).
◦ Metabolic acidosis – low obstruction.Surgical Management:
Strangulation/Perforation → Emergency Surgery.
Colonoscopy for tumor removal or stricture dilation.
Partial or total colostomy or ileostomy for obstruction, necrosis, or perforation.
Resection of obstructed segment with anastomosis (put pieces of bowel back together).
Anastomosis works = bowel rest
Anastomosis doesn’t work = ostomy
Diagnostics:
Imaging
LBO: Sigmoidoscopy or colonoscopy (finds location of obstruction and fixes)
Blood tests (CBC, CMP)
Increased WBC = strangulation (necrotic tissue) or perforation
Increased Hct = Hemoconcentration (increased concentration of blood cells, falsely elevated from fluid shift)
Decreased Hct and Hgb = Bleeding
Serum electrolytes, BUN, creatinine, GFR = hydration
Bowel Resection and Ostomy Surgery
Indications
Removes cancer, repair obstruction/fistula (connection that shouldn’t be there)/perforation/traumatic injury, and treat an abscess, hemorrhage, or inflammatory diseases.
Common Etiologies: Colorectal cancer (CRC), IBD (Crohn’s and ulcerative colitis), necrotic bowel, perforated ulcer, diverticulitis, trauma.
Fistulas might exist between small bowel and large, between rectum and bladder.
Pts with Crohn’s disease or ulcerative colitis may have bowel resections done.
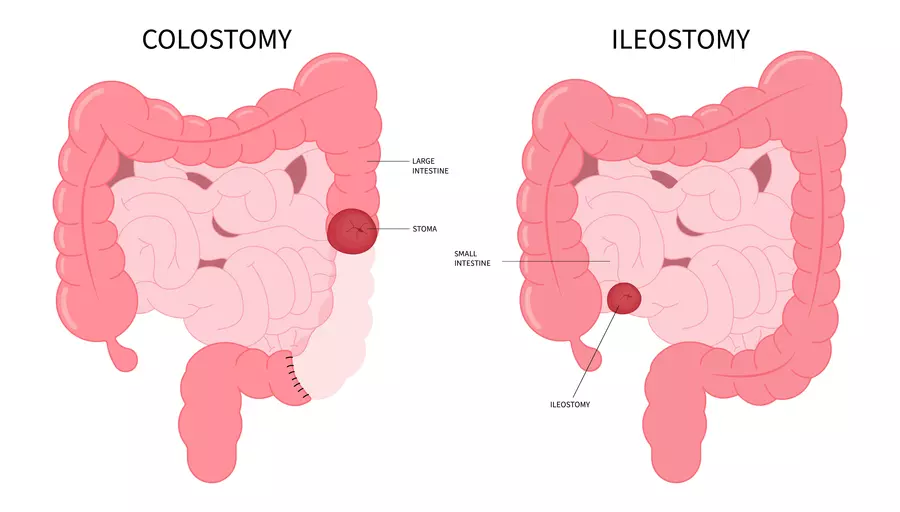
Ostomy Types
Traditional Ostomy
End Stoma: Distal bowel removed and permanent stoma.
Loop Stoma: (Usually temporary) anterior wall opened for fecal
diversion and distal opening to drain mucus; plastic rod in place 7 to 10 daysDouble-barrel Stoma (usually temporary, trying to put back together): Bowel divided and two stomas created; proximal for fecal diversion and distal for mucus drainage.
Continent Ileostomy (pt manually drains stool by insertion of catheter and holds more)
Kock Pouch
Barnett Continent Ileal Reservoir
Temporary or permanent “takedown” procedure to reverse.
Stoma should appear red, moist, and painless.
The more distal the ostomy, the more likely contents will
resemble normal feces (because the stool has more time to pass through).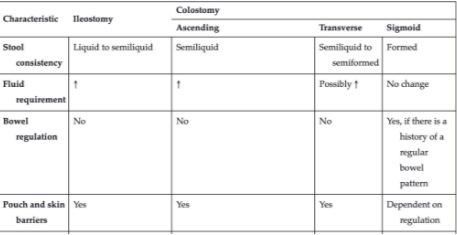
Sigmoid colostomy may not require a stoma bag if the patient has regular bowel movements.
Preoperative Care
Stoma site selection and considerations
Within rectus muscle (decreased risk of hernia)
Flat surface (no creases, seal less likely to leak)
Patient is able to see it but it’s under clothing
Nursing Interventions Post-Surgery
Monitor for Postoperative Complications:
Delayed wound healing, infection, hemorrhage, fistulas.
Record bleeding (minimal bleeding normal → intestines are vascular)
Unusual/foul odor → infection.
Edema, redness, high WBCs, drainage → infection.
WBCs should decreased after surgery otherwise notify HCP.
Electrolyte imbalances and dehydration.
Abnormal output → notify HCP
Ostomy Assessment:
Normal: Pink-red, moist, mild swelling.
Abnormal: Pale, dark, excessive bleeding, “dusky” (blueish).
Assess every 4 hours (especially if new)
Ostomy Care:
Empty pouch when 1/3 full.
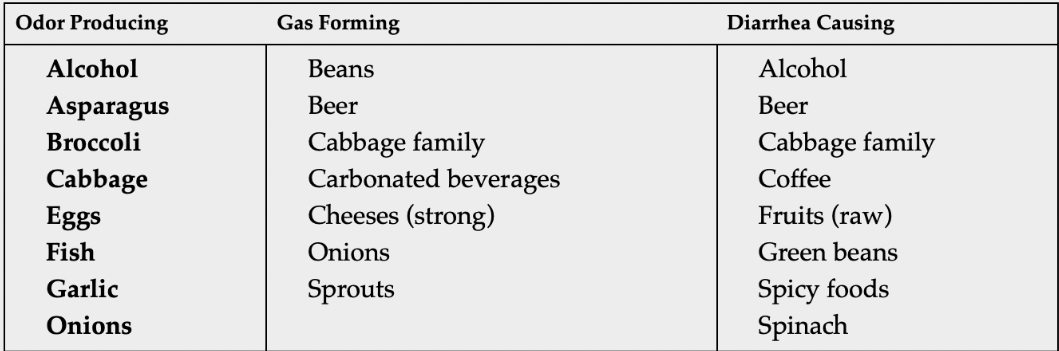
Prevent gas buildup with diet modifications.
Ostomy Education:
Demonstrate and observe patient/caregiver practice the following:
Remove old skin barrier, clean skin, correctly apply new skin barrier
Irrigation for regulation (distal colon ostomy)
Apply, empty, clean, remove pouch.
Empty pouch when 1/3 full.
Males: 3-12 months erectile dysfunction
Females: Vaginal dryness and decreased sensations
“Burp bag” due to gassiness.
May experience rectal bowel movement up to 3 days after surgery if emergency surgery was performed
Dietary Management:
Small, frequent meals, adequate fluid intake.
Psychosocial Support:
Address body image concerns, depression, coping strategies.
Normal ADLs within 6-8 weeks and avoid heavy lifting.
Colostomy Function:
Output after peristalsis returns or up to 2 days after resuming diet
Some mucus production likely.
Excess gas common for 2 weeks
Ileostomy Function:
First 24-48 hours minimal drainage (liquid-semiliquid)
Peristalsis returns → 1500-1800 mL/day and will decrease about 500 mL/day
Water absorption increases and feces thickens while volume decreases → watch for dehydration.
Chew thoroughly any nuts, raisins, popcorn, coconut, mushroom, olive, stringy veggies, foods with skins, dried fruits, and meats with casings (otherwise lead to an obstruction).
Hypocalcemia: Confusion
Anal Canal:
Kegel exercise recommended after 4 weeks
Incontinence of mucus
Phantom rectal pain (do not strain)
Acute Pancreatitis
Pathophysiology and Etiology
Pancreatic enzyme activation that causes autodigestion of pancreas and severe pain by digesting normal organ tissue.
Autodigestion of pancreas → injury to pancreatic cells, activation of pancreatic enzymes → activation of trypsinogen to trypsin within pancreas (bleeding occurs).
Mild Pancreatitis:
Edematous or interstitial
Severe Pancreatitis:
Necrosis, organ failure, sepsis
50% have long-lasting endocrine and exocrine dysfunction
Overall fatality rate 9%
Anatomy: Pancreas sits behind stomach.
Pain in pancreas → Happens in the upper abdomen and can radiate to the back.
Secretes 1000 mL of pancreatic juice per day.
Two functions:
Endocrine function: Related to diabetes and blood sugar function → produces hormones such as insulin and glucagon.
Exocrine Function: Cells secrete buffers (watery solution) and digestive enzymes (pancreatic amylase for breaking starches, lipase for breaking lipids, proteolytic for breaking proteins, and proenzymes).
15 digestive enzymes → packaged into zymogens (proenzymes).
When meal is ingested → vagal nerves, polypeptides, and hormones stimulate release of proenzymes into pancreatic duct.
Digestion in Three Phases:
Cephalic: Think about, smell, and prepare food. Body starts producing liver enzymes, pancreatic enzymes, and hydrochloric acid (stomach acid) at that time.
Gastric: Food enters stomach.
Intestinal: Food enters into duodenum.
Causes:
Gallstones / gallbladder disease (most common in women)
May cause blockage of pancreatic juices from getting into small intestine and backs up into pancreas (autodigestion → pancreatitis).
Chronic alcohol use (most common in men)
10-11 drinks per day for 10 years.
Hypertriglyceridemia (>1000 mg/dL): High triglycerides
Increases chylomicrons (low-dense large particles that can obstruct capillaries).
Less common: Drug reactions or pancreatic cancer.
Clinical Manifestations of autodigestion
Elevation of blood sugar (diabetes may develop)
Sudden onset
Abdominal pain: Severe, LUQ or mid-epigastric pain, radiating to the back.
Eating worsens pain
Starts when lying down (recumbent)
Nausea/Vomiting (remains unrelieved) & Abdominal Guarding.
Jaundice, Abdominal Distension.
Cullen’s Sign (periumbilical ecchymosis/bruising around the navel) & Grey Turner’s Sign (flank ecchymosis/bruising on the flanks) = sign of bleeding/hemorrhage.
Vital Signs:
Resp: Cyanosis, dyspnea, crackles (fluid builds up and decreases movement of diaphragm) → compliment system activation (pleural effusion)
GI: N/V, decreased/absent bowel sounds, distension (if ileus)
Low-grade fever and leukocytes
Cardiovascular: Tachycardia, hypotension, shock
Skin: Jaundice, abdominal skin discoloration
Complications
Pancreatic Pseudocyst: Fluid, pancreatic enzymes, debris, and exudates surrounded by wall.
S/S: Abdominal pain, palpable mass, N/V, anorexia.
May perforate (secondary peritonitis)
Surgical intervention
Pancreatic Abscess (more urgent because already infected with necrosis): Infected pseudocyst; results from extensive necrosis.
S/S: Upper abdominal pain, leukocytosis, mass, high fever (necrosis).
May rupture or perforate (secondary peritonitis) and needs prompt surgical intervention.
Potential Systemic Complications:
Pleural effusion, atelectasis (partial or full collapsed lung), pneumonia, ARDS, hypotension or shock, thrombi, PE, DIC (multiple clots), tetany (hypocalcemia → Chvostek’s and Trousseu’’s), abdominal compartment syndrome (wet-dry and change dressing frequently, soaked saline gauze packed into abdomen).
Diagnostic Studies/Labs
Amylase and lipase, abdominal x-ray or US (best option), contrast CT imaging (look at vasculature to see if hemorrhage).
MRCP: Moves stones magnetically.
Amylase and lipase → first line labs.
Amylase (sensitive but not specific):
Normal 60-120
Produced by salivary glands, skeletal muscles, ovaries, etc.
Elevates within 12 hours and normalizes in 48-72
Pseudo cyst or abscess = elevated (useful in early diagnostics)
May be elevated in a perforated bowel, penetrated peptic ulcer, duodenal obstruction.
Lipase (primary diagnostic marker):
Normal 0-60.
Elevates within 24-48 hours and normalizes after 5-7 days.
This lab is trended to monitor progress.
In pancreatitis elevations are 5-10x normal.
Elevated bilirubin and liver enzymes (AST and ALT) → common if obstructive
Triglyceride level
Elevated glucose and decreased calcium
Interprofessional Care
Aggressive hydration (LR to convert lactate into bicarb or NS), usually start 250 mL/hr.
Metabolic: Give oxygen if less than 95% (curve is moving to the right) and monitor blood glucose levels.
Pain management (morphine unless pancreatitis caused by gallstone because it causes spasms)
Flex trunk
Elevate 45 degrees bed
Frequent oral and nasal care (NPO)
NPO, NG suction, meds to decrease acid secretion (H2 blockers, antacids, “prazoles”)
Enteral nutrition to avoid necrotizing pancreatitis.
Check lipase labs to see if the care is working.
Vital Signs:
Monitor for hypotension and tachycardia
Long-standing tachycardia can decrease perfusion overtime.
Magnesium should be given first for potassium to stick.
Hypocalcemia:
Tetany (jerking, irritability, twitching), Chvostek’s and Trousseau’s sign → treat with calcium gluconate
Acute Pancreatitis Recovery
Nutrition Therapy:
Small, frequent feedings.
High carbs, low fat (fats require more pancreatic enzymes)
Supplemental fat-soluble vitamins (ADEK)
Lookout for hyperglycemia signs (the 3 Ps → polydipsia, polyphagia, polyuria)
Monitor for infection, diabetes, sta
Biliary Tract Disease
Overview
Cholecystitis and cholelithiasis are the primary disorders.
Cholelithiasis (most common):
Stones in gallbladder (leads to pancreatitis because pancreatic duct cant empty)
Bile salts can become hyper concentrated leading to stone formation.
Cholecystitis:
Inflammation of the gallbladder.
Acute or chronic or “acute on chronic”
Associated often with gallstones or biliary sludge.
Causes decrease in digestion and abdominal pain.
Risk Factors
Female, multiparity, estrogen therapy.
Older than 40.
Sedentary lifestyle or obesity
Genetics
Native Americans
Interprofessional Care
Emphasis on infection management, fluid balance, and post-surgical recovery.
Gallbladder Disorders (Cholelithiasis & Cholecystitis)
Pathophysiology
Cholelithiasis: Gallstones obstruct bile flow.
Formed from bile salts, cholesterol, protein, bilirubin, and calcium.
Contributing Factors:
Lithogenic bile (bile supersaturated with cholesterol)
Biliary sludge (stasis of bile)
Caused by immobility, pregnancy, inflammation.
Stones may stay or migrate → cause pain or obstruction → cholecystitis, pancreatitis, obstructive jaundice (yellow seen in eyes first), and increased LFTs (AST/ALT).
Choledocholithiasis = gallstone obstruction of the common bile duct
Cholecystitis: Inflammation of the gallbladder due to obstruction or infection.
Either confined to mucus lining or involves entire wall.
Gallbladder is edematous and hyperemic
May be distended with bile or pus (may be infected)
Scarring and fibrosis after attack → chronic decreased function (more likely leading to stricture and decreased immobility of gallbladder → more likely to develop stones).
Cystic duct may become occluded
Acalculous cholecystitis occurs in:
Older adults and critically ill
Prolonged immobility, fasting, prolonged parenteral nutrition, diabetes
Adhesions, cancer, anesthesia, opioids
If inflammation or infection (acute cholecystitis):
◦ Leukocytosis
◦ Fever, chills
If chronic cholecystitis develops:
fat intolerance,
dyspepsia,
heartburn,
flatulence
Clinical Manifestations
Biliary Colic (stones moving or obstructing): Severe pain post-high-fat meal (within 3-6 hours) or when lying down because that’s when it hits the intestine and gallbladder needs to dump bile into the intestine.
tachycardia, diaphoresis, prostration.
Pain in RUQ and toward scapula as gas tries to move out.
Indigestion, N/V, abdominal pain/guarding, restlessness
Jaundice, Dark Urine, Clay-colored Stools, pruitis, bleeding tendencies, pruritis, intolerance for fatty foods → total obstruction, backed up bile, hyperbilirubinemia → liver congested.
Complications
Cholelithiasis leads to cholecystitis
Gangrenous cholecystitis → gallbladder rupture leads to peritonitis
Abscess and fistulas develop
Cholangitis and choledocholithiasis. If obstructive:
Pancreatitis: Inflammation of the pancreas that can result from gallstones or chronic alcohol use.
Transaminitis: Elevation of liver enzymes, typically indicating liver inflammation or damage.
Biliary cirrhosis: A chronic disease that results in inflammation and destruction of the bile ducts in the liver, ultimately leading to liver failure.
Diagnostics:
Abdominal US → checks for gallstones
Lab changes:
Elevated WBCs
Elevated bilirubin (hyperbilirubinemia, jaundice)
Elevated urinary bilirubin level
Elevated liver enzymes (transaminitis)
Elevated amylase or lipase (pancreatitis)
Interprofessional Care
Conservative Therapy:
Extracorporeal shock-wave lithotripsy (ESWL): Uses shock waves to break down gallstones (used if ECRP fails).
Pain Management: Opioids, Anticholinergics (decrease GI secretions and counteract smooth muscle spasms).
NPO, NG Suction if Severe Vomiting.
Surgical Treatment:
Laparoscopic Cholecystectomy (LapChole) → Gold Standard.
Treatment for symptomatic gallstones
Removal of gallbladder through1-4 puncture holes.
Resume normal activities within 1 week.
Drain: Originates in gallbladder and allows pus, purulent fluid, and bile to drain.
Open Cholecystectomy (less common) → Requires T-Tube for Bile Drainage.
Removal of gallbladder through right subcostal incision.
Indicated if unable to perform LapChole
Drain: Originates in common bile duct and allows excess bile to drain after surgery
ERCP with sphincterotomy for Common Bile Duct Stones.
Direct visualization
Dilation of bile duct for placement of stents
Stones removed with basket or out with stool
Remain NPO until return of gag reflex
Drain (if ERCP fails): Transhepatic Biliary Catheter → a procedure that allows for drainage of bile directly from the liver due to obstruction → used in cases of transaminitis and jaundice.
Postoperative Nursing Management
Monitor VS, Pain, & Infection Signs.
Early Ambulation (day 0) & Deep Breathing.
Dietary Modifications:
Low-fat, small frequent meals and intake of fiber and calcium.
Avoid high-fat, gas-producing foods.