
Chapter 36 - Hypertension
1. Relate the pathophysiology of primary hypertension to the clinical manifestations and complications.
2. Choose appropriate strategies for the prevention of primary hypertension.
3. Describe the interprofessional care for primary hypertension.
4. Explain the interprofessional care of the older adult with primary hypertension.
5. Prioritize the nursing management of the patient with primary hypertension.
6. Describe the nursing and interprofessional care of a patient with a hypertensive crisis.
blood pressure (BP)
elevated blood pressure, Table 36.2
hypertension
hypertensive crisis
orthostatic hypotension
primary hypertension
secondary hypertension
systemic vascular resistance (SVR)
NORMAL REGULATION OF BLOOD PRESSURE
Blood pressure (BP) is the force exerted by the blood against the walls of the blood vessel.
Maintaining tissue perfusion during activity and rest must be adequate.
Regulation of BP involves nervous, cardiovascular, endothelial, renal, and endocrine functions.
HYPERTENSION
Classification of Hypertension
Hypertension, or high BP, is defined as either a persistent systolic BP (SBP) greater than or equal to 130 mm Hg or a diastolic BP (DBP) greater than or equal to 80 mm Hg. If either the SBP or DBP is outside of a normal range, the higher measurement will determine the hypertension classification.
Hypertension is classified as follows:
Elevated blood pressure is defined as an SBP between 120-129 mm Hg and a DBP < 80 mm Hg.
Hypertension (Stage 1) is defined as an SBP between 130-139 mm Hg or a DBP between 80-
89 mm Hg.
Hypertension (Stage 2) is defined as an SBP > 140 mm Hg or a DBP > 90 mm Hg.5 Etiology
Primary hypertension is elevated BP without an identified cause. It accounts for 90% to 95% of all cases of hypertension.
Secondary hypertension is elevated BP with a specific cause. It accounts for 5% to 10% of hypertension in adults.
Pathophysiology of Primary Hypertension.
The hemodynamic hallmark of hypertension is persistently increased systemic vascular resistance (SVR).
This persistent elevation in SVR may occur in several ways. Defects in any of the mechanisms involved in the maintenance of normal BP, including sodium intake, the renin-angiotensin-aldosterone mechanism, and sympathetic nervous system (SNS) stimulation, can result in the development of hypertension.
Defects in glucose, insulin, and lipoprotein metabolism are common in primary hypertension.
Contributing factors to the development of hypertension include cardiovascular risk factors combined with socioeconomic conditions and gender and ethnic differences.
Endothelial dysfunction is a marker for CVD and primary hypertension.
Clinical Manifestations
Called the “silent killer” because it is often asymptomatic until it becomes severe
and target organ disease occurs.
Target organ diseases occur in the heart (hypertensive heart disease), brain
(cerebrovascular disease), peripheral vessels (peripheral vascular disease), kidney
(nephrosclerosis), and eyes (retinopathy).
It is one of the leading causes of end-stage renal disease.
Damage to retinal vessels indicates concurrent vessel damage in the heart, brain, and kidney. Manifestations of severe retinal damage include blurring of vision, retinal hemorrhage, and loss of vision.
There is a direct relationship between hypertension and cardiovascular disease (CVD). Hypertension is a major risk factor for coronary artery disease (CAD), stroke, and cerebral atherosclerosis.
Sustained high BP increases the cardiac workload and produces left ventricular hypertrophy (LVH). Progressive LVH, especially in association with CAD, is associated with the development of heart failure.
Diagnostic Studies
Basic laboratory studies are done to (1) identify or rule out causes of secondary hypertension, (2) evaluate target organ disease, (3) determine overall cardiovascular risk, or (4) establish baseline levels before starting therapy.
Routine urinalysis, BUN, serum creatinine, and creatinine clearance levels are used to screen for renal involvement and to provide baseline information about kidney function.
Lipid profiles provide information about risk factors that predispose to atherosclerosis and cardiovascular disease.
12 lead ECG and echocardiography provide information about the heart status.
Ambulatory BP monitoring (ABPM) measures the BP at preset intervals over a 24-hour period. • Home BP Monitoring (HBPM) measures the BP at home to confirm hypertension diagnosis and for titration of oral agents. HBPM should be done in conjunction with regular follow up visits with the HCP.
Interprofessional Care
Target goals take into consideration both age and comorbidities when recommending treatment options.
Lifestyle modifications are directed toward reducing the patient's BP and overall cardiovascular risk. The AHA’s “Life’s Simple 7” steps support ways to modify and improve health. These are: (1) manage blood pressure, (2) control cholesterol, (3) reduce blood sugar, (4) get active, (5) eat better, (6) lose weight, and (7) stop smoking. Other modifications by the taskforce on hypertension address sodium restrictions and alcohol intake.
Common dietary modifications are the Mediterranean or DASH diet, with reduced sodium and fat intake.
Drug Therapy
Drugs currently available for treating hypertension work by (1) decreasing the volume of circulating blood and/or (2) reducing SVR.
Diuretics promote sodium and water excretion, reduce plasma volume, and reduce the vascular response to catecholamines.
Adrenergic-inhibiting agents act by decreasing the SNS effects that increase BP. Adrenergic inhibitors include drugs that work centrally on the vasomotor center and peripherally to inhibit norepinephrine release or to block the adrenergic receptors on blood vessels.
Direct vasodilators decrease the BP by relaxing the vascular smooth muscle and reducing SVR.
Calcium channel blockers increase sodium excretion and cause arteriolar vasodilation by preventing the movement of extracellular calcium into cells.
Angiotensin-converting enzyme (ACE) inhibitors prevent the conversion of angiotensin I to angiotensin II and reduce angiotensin II (A-II)–mediated vasoconstriction and sodium and water retention.
A-II receptor blockers (ARBs) prevent angiotensin II from binding to its receptors in the walls of the blood vessels.
Most patients who are hypertensive will need 2 or more antihypertensive drugs to achieve their BP goals.
Side effects and adverse effects of antihypertensive therapy may be so severe or undesirable that the patient does not adhere to therapy. Patient and caregiver teaching related to drug therapy is needed to identify and minimize side effects and to cope with therapeutic effects.
Resistant hypertension is the failure to reach goal BP in patients who are adhering to full doses of an appropriate 3-drug therapy regimen that includes a diuretic.
NURSING MANAGEMENT: PRIMARY HYPERTENSION
The primary nursing responsibility for long-term management of hypertension is to help the patient in reducing BP and adhering to the treatment plan.
Nursing actions include evaluating therapeutic effectiveness, detecting and reporting any adverse treatment effects, assessing and enhancing adherence, and patient and caregiver teaching.
Patient and caregiver teaching includes: (1) nutritional therapy, (2) drug therapy, (3) lifestyle modification, and (4) home monitoring of BP.
Blood Pressure Measurement
Accurate BP measurements are critical. A key role of the nurse is to provide patient and caregiver teaching about measuring BP at home.
Orthostatic hypotension is defined as a decrease of 20 mm Hg or more in SBP, a decrease of 10 mm Hg or more in DBP, and/or an increase of 20 beats per min or more in pulse from supine to standing.
Orthostatic changes in BP and pulse should be measured in older adults, in patients taking antihypertensive drugs, and in patients who report symptoms consistent with reduced BP upon standing (e.g., light-headedness, dizziness, syncope).
GERONTOLOGIC CONSIDERATIONS: HYPERTENSION
The prevalence of hypertension increases with age. The lifetime risk of developing hypertension is around 90% for normotensive men and women over age 55.
In some older people, there is a wide gap between the first Korotkoff sound and subsequent beats (auscultatory gap). Failure to inflate the cuff high enough may result in an inaccurate SBP.
BP goals in people older than 65 years of age who live independently are no different for other independent living adults under 65 years old. Adults over 65 who are not independent with comorbidities should have drugs added and titrated using clinical judgement and patient preference as the guide.
Orthostatic hypotension often occurs in older adults because of impaired baroreceptor reflex mechanisms, volume depletion, and chronic disease states, such as decreased renal and hepatic function or electrolyte imbalance.
HYPERTENSIVE CRISIS
Hypertensive crisis is a term used to indicate either a hypertensive urgency or emergency. Diagnosis is determined by the presence of target organ disease and the type of treatment the patient will receive.
Hypertensive urgency has no clinical evidence of target organ disease.
Hypertensive urgencies usually do not need IV drugs but can be managed with oral therapy.
A patient with hypertensive urgency who is not hospitalized should have outpatient follow-up care within 24 hours.
Hypertensive emergencies have evidence of target organ disease. It needs hospitalization with intensive care monitoring and the IV administration of antihypertensive drugs, including vasodilators, adrenergic inhibitors, ACE inhibitors, and/or calcium channel blockers. Drugs are titrated based on the MAP.
Regular, ongoing assessment (e.g., ECG monitoring, vital signs, urinary output, level of consciousness, visual changes) is essential to evaluate the patient with severe hypertension.
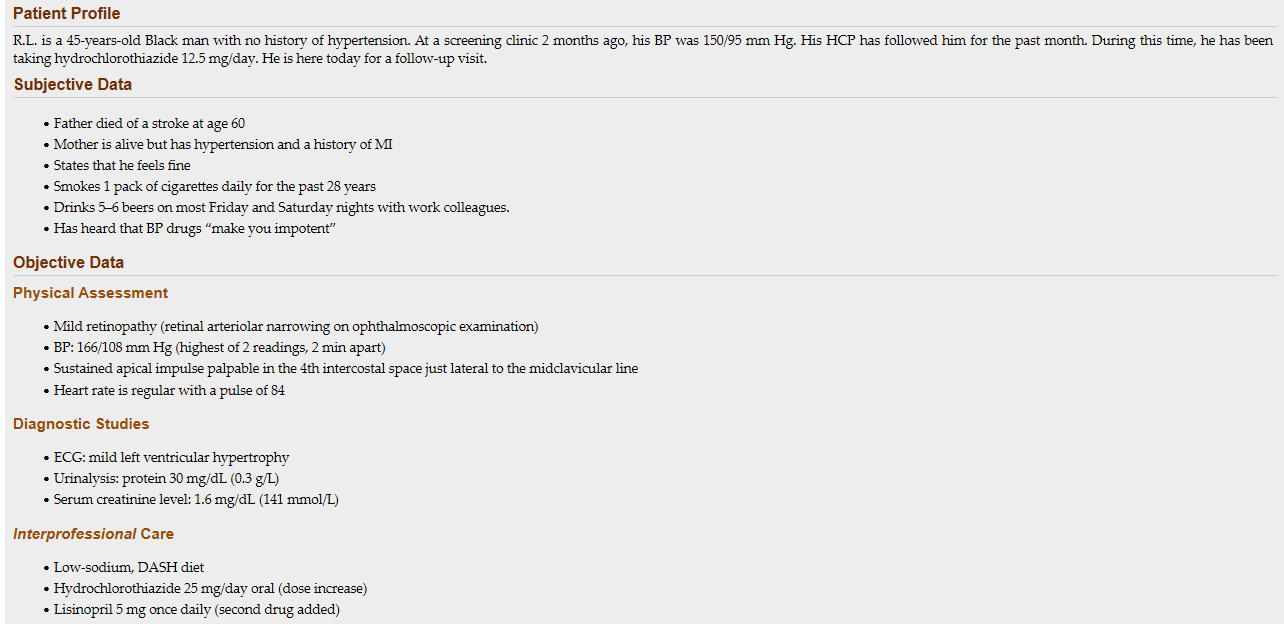 1. Recognize: What risk factors does R.L. have for hypertension?
1. Recognize: What risk factors does R.L. have for hypertension?
R.L’s risk factors include both modifiable and non-modifiable risks. His non-modifiable risk factors include family history and his race/ethnicity. Modifiable risk factors include: tobacco use, alcohol use, and his knowledge deficit related to hypertension,
2. Recognize: What stage of hypertension does R.L. have?
His current blood pressure is 166/108. This places him in Stage 2 hypertension.
3. Analyze: What are the abnormal findings in the objective data?
Physical exam: R.L. has retinopathy on his eye exam. A normal finding is no retinopathy. His blood pressure is abnormal. The apical impulse should be at or medial to the midclavicular line. Diagnostic studies: His ECG has an abnormal finding of left ventricular hypertrophy meaning his heart is enlarged. His urinalysis is abnormal. A normal value for his urine would be no protein. His serum creatinine is higher than the normal range.
4. Analyze: Based on the assessment, what target organ disease may be present?
R.L. has evidence of kidney damage including protein in the urine and elevated creatinine level. He has evidence of heart damage on his ECG and his apical impulse location is likely due to an enlarged heart. The retinopathy indicates potential ocular (eye) damage.
5. Analyze: What additional assessment would be done for this patient?
(1) Height and weight are needed to know if R.L. is obese. (2) The data does not provide as assessment of social determinants of health that are important for understanding risk factors and completing a plan of care. (3) It would be helpful to know more about what types of food he typically eats to understand how to make recommendations for dietary changes. (4) Information is needed about current level of activity before making exercise recommendations. (5) You should ask R.L. about any additional over the counter and supplemental medications that may increase his blood pressure like NSAIDS, cold/sinus medication, high-sodium antacids and appetite suppressants.
6. Plan: What medications would you expect to see ordered for this patient?
R.L.’s blood pressure is not currently controlled with one medication and with lifestyle changes. A second antihypertensive should be added. This will likely include a medication from one of the following categories: Beta-Blockers, Calcium Channel Blockers, ACE inhibitors or Angiotensin Receptor Blockers. In this case lisinopril was selected for this patient because he is already showing signs of kidney damage and lisinopril can protect kidney function.
7. Plan: What referrals may be indicated for R.L.?
R.L. would benefit from a referral to a dietician to discuss dietary changes including the DASH or Mediterranean diet. He may also benefit from referral to a substance abuse specialist due to his alcohol and tobacco use. If he has physical limitations, a physical therapist may be helpful to create an exercise plan.
8. Prioritize: Based on your assessment, which teaching points about hypertension are the most important?
R.L. has some significant modifiable risk factors for his hypertension and ASCVD. You should prioritize medications and medication adherence because his blood pressure has continued to rise. This increases his risk for hypertensive urgency. In addition, teaching about his modifiable risk factors including diet, alcohol, and tobacco use have been shown to be the most effective at decreasing hypertension.
9. Prioritize: What is the most important problem to manage for R.L. right now?
Blood pressure management is the highest priority for this patient. Elevated blood pressure puts him at significant risk for ASCVD and target organ damage.
10. Act: What would you teach this patient about the medications he is prescribed?
You should tell R.L. that the current medication he is taking is not managing his blood pressure. This is not uncommon. Many people need more than one medication to adequately control blood pressure. It is important for him to be consistent taking his medication. He should know that some people do experience sexual side effects with medication, and to tell his HCP about any concerns. You should also educate about possible side effects from his Lisinopril especially angioedema and cough. Tell R.L. if he is experiencing these symptoms he needs to contact his healthcare provider and that if he is having difficulty breathing he should be evaluated immediately.
11. Act: What other teaching is needed for this patient?
Teaching for this patient should be focused on his current misconceptions regarding hypertension and being “hyper” as well as his belief that his medications may prevent sexual function. It is important for him to know that elevated blood pressure can cause damage to many of his body systems and that his testing shows that this is already happening. R.L. has a number of different lifestyle modifications he can make. It is important for him to help set the priority for behaviors he is willing and able to change as this requires life-long changes. R.L. will also need to monitor for signs of orthostasis that can occur when a person is taking blood pressure medications.
12. Evaluate: What follow-up is needed for this patient to assess his response to your plan?
This patient should have a blood pressure recheck in 1 month to assess his response to his medication changes. At this visit medication adherence, lifestyle changes and any side effects should be discussed. R.L. will also benefit from a home blood pressure cuff to monitor his blood pressure at home to see if readings are similar to those in the office. He can bring his home cuff to his next visit so that his machine can be checked for accuracy. He should know that if he experiences chest pain, severe headache, or sudden vision changes that he needs to be evaluated immediately.
1. A defect in which BP-regulating mechanisms can result in the development of hypertension? (select all that apply)
a. Release of norepinephrine
b. Secretion of prostaglandins
c. Stimulation of the sympathetic nervous system
d. Stimulation of the parasympathetic nervous system
e. Activation of the renin-angiotensin-aldosterone system
Norepinephrine (NE) is released from the sympathetic nervous system nerve endings and activates receptors found in the vascular smooth muscle. When the α-adrenergic receptors in smooth muscle of the blood vessels are stimulated by NE, vasoconstriction results. Increased sympathetic nervous system stimulation produces increased vasoconstriction and increased renin release. Increased renin levels activate the renin-angiotensin-aldosterone system, leading to an elevation in BP
2. Which item in a patient history would the nurse recognize as a modifiable risk factor for the development of hypertension?
a. Low-calcium diet
b. Excess alcohol use
c. Family history of hypertension
d. Consumption of a high-protein diet
Alcohol intake is a modifiable risk factor for hypertension. Excessive alcohol intake is strongly associated with hypertension. Males with hypertension should limit their daily intake of alcohol to 2 drinks per day, and one drink per day for females with hypertension.
3. Which information would the nurse apply to a teaching plan for a patient with hypertension?
a. All patients with elevated BP need drug therapy
b. Obese persons must achieve a normal weight to lower BP.
c. It is not necessary to limit salt in the diet if taking a diuretic.
d. Lifestyle modifications are needed for persons with elevated BP.
Lifestyle modifications are needed for all patients with prehypertension and hypertension.
4. Which consideration would the nurse include in the management of the older adult with hypertension?
a. Preventing primary hypertension from converting to secondary hypertension
b. Recognizing that the older adult is less likely to adhere to the drug therapy regimen than a younger adult
c. Ensuring that the patient receives larger initial doses of antihypertensive drugs because of impaired absorption
d. Using a precise technique in assessing the BP of the patient because of the possible presence of orthostatic hypertension
Careful technique is important in assessing BP in older adults. In some older people, there is a wide gap between the first Korotkoff sound and subsequent beats. This wide interval is called an auscultatory gap. Failure to inflate the cuff high enough may result in an inaccurate systolic BP, one that is too low for the patient.
5. A patient with newly discovered high BP has an average reading of 158/98 mm Hg after 3 months of exercise and diet modifications. Which management strategy would the nurse expect?
a. Drug therapy will be needed because the BP has not reached the goal.
b. BP monitoring should continue for 3 months to confirm a diagnosis of hypertension.
c. Lifestyle changes are less important since they were not effective, and drugs will be started.
d. More changes in the patient’s lifestyle are needed for a longer time before starting drug therapy.
The patient has hypertension, stage 1. Lifestyle modifications will continue, but starting drug therapy is a priority. Reducing BP can help to prevent serious complications related to hypertension.
6. A patient is admitted to the hospital in a hypertensive emergency (BP 244/142 mm Hg). Sodium nitroprusside is started to treat the elevated BP. Which management strategies would the nurse anticipate? (select all that apply)
a. Measuring hourly urine output
b. Continuous BP monitoring with an arterial line
c. Decreasing the MAP by 50% within the first hour
d. Maintaining bed rest and giving tranquilizers to lower the BP
e. Assessing the patient for signs of heart failure and changes in mental status
Measure urine output hourly to assess renal perfusion. Patients treated with IV sodium nitroprusside should have continuous intraarterial BP monitoring. Hypertensive crisis can cause encephalopathy, intracranial or subarachnoid hemorrhage, acute left ventricular failure, MI, renal failure, dissecting aortic aneurysm, and retinopathy. The initial treatment goal is to decrease the mean arterial pressure (MAP) by no more than 25% within minutes to 1 hour. Patients receiving IV antihypertensive drugs may be restricted to bed rest. Getting up (e.g., to use the toilet/commode) may cause severe cerebral ischemia and fainting.
The nurse is caring for a patient who has taken hydrochlorothiazide for 10 years to treat hypertension. Which parameter indicates effectiveness of this drug therapy?
BP 128/78 mm Hg
Weight loss of 2 lb
Absence of ankle edema
Output of 600 mL per 8 hours
Hydrochlorothiazide may be used alone as monotherapy to manage hypertension or in combination with other medications if not effective alone. After the first few weeks of therapy, the diuretic effect diminishes, but the antihypertensive effect remains. Because the patient has been taking this medication for 10 years, the most direct measurement of its intended effect would be the blood pressure.
The nurse supervises assistant personnel (AP) taking the blood pressure of a patient admitted with heart failure who is obese. Which action by the AP will require the nurse to intervene?
Deflating the blood pressure cuff at a rate of 8 to 10 mm Hg/sec
Waiting 2 minutes after position changes to take orthostatic pressures
Taking the blood pressure with the patient’s arm at the level of the heart
Taking a forearm blood pressure if the largest cuff will not fit the patient’s upper arm
The cuff should be deflated at a rate of 2 to 3 mm Hg/sec. The arm should be supported at the level of the heart for accurate blood pressure measurements. Using a cuff that is too small causes a falsely high reading and too large causes a falsely low reading. If the maximum size blood pressure cuff does not fit the upper arm, the forearm may be used. Orthostatic blood pressures should be taken within 1 to 2 minutes of repositioning the patient.
A middle aged patient is diagnosed with hypertension and receives a prescription for benazepril. After providing teaching, which statement by the patient indicates correct understanding?
“If I take this medication, I will not need to follow a special diet.”
“It is normal to have some swelling in my face while taking this medication.”
“I will need to eat foods such as bananas and potatoes that are high in potassium.”
“If I develop a dry cough while taking this medication, I should notify my doctor.”
Benazepril is an angiotensin-converting enzyme inhibitor. The medication inhibits breakdown of bradykinin, which may cause a dry, hacking cough. Other adverse effects include hyperkalemia. Swelling in the face could indicate angioedema and should be reported immediately to the prescriber. Patients taking drug therapy for hypertension should also attempt lifestyle modifications to lower blood pressure such as a reduced sodium diet.
When teaching how lisinopril helps lower the patient’s blood pressure, which mechanism of action would the nurse explain?
Blocks β-adrenergic effects.
Relaxes arterial and venous smooth muscle.
Inhibits conversion of angiotensin I to angiotensin II.
Reduces sympathetic outflow from central nervous system.
Lisinopril is an angiotensin-converting enzyme inhibitor that inhibits the conversion of angiotensin I to angiotensin II, which reduces angiotensin II–mediated vasoconstriction and sodium and water retention. β-Blockers result in vasodilation and decreased heart rate. Direct vasodilators relax arterial and venous smooth muscle. Central-acting α-adrenergic antagonists reduce sympathetic outflow from the central nervous system to produce vasodilation and decreased systemic vascular resistance and blood pressure
The nurse teaches a young adult patient newly diagnosed with hypertension about lifestyle modifications to reduce blood pressure. Which patient statement demonstrates further teaching is required?
“I will avoid adding salt to my food during or after cooking.”
“If I lose weight, I might not need to continue taking medications.”
“I can lower my blood pressure by switching to smokeless tobacco.”
“Diet changes can be as effective as taking blood pressure medications.”
Nicotine contained in tobacco products (smoking and chew) cause vasoconstriction and increase blood pressure. Persons with hypertension should restrict sodium to 1500 mg/day by avoiding foods high in sodium and not adding salt in preparation of food or at meals. Weight loss can decrease blood pressure between 5 to 20 mm Hg. Following dietary recommendations (e.g., the DASH diet) lowers blood pressure, and these decreases compare with those achieved with blood pressure–lowering medication.
Which instruction would the nurse give when teaching a patient about stage 1 hypertension?
Increase water intake.
Restrict sodium intake.
Increase protein intake.
Use calcium supplements.
The patient should decrease intake of sodium. This will help to control hypertension, which can be aggravated by excessive salt intake, which in turn leads to fluid retention. Protein intake does not affect hypertension. Calcium supplements are not recommended to lower blood pressure.
The assistive personnel (AP) is taking orthostatic vital signs. In the supine position, the patient’s blood pressure (BP) is 130/80 mm Hg, and the heart rate (HR) is 80 beats/min. In the sitting position, the BP is 140/80, and the HR is 90 beats/min. Which action would the nurse instruct the AP to take next?
Repeat BP and HR in this position.
Record the BP and HR measurements.
Take BP and HR with patient standing.
Return the patient to the supine position.
The vital signs taken do not reflect orthostatic changes, so the AP will continue with the measurements while the patient is standing. There is no need to repeat or delay the readings. The patient does not need to return to the supine position. When assessing for orthostatic changes, the AP will take the BP and pulse in the supine position, then place the patient in a sitting position for 1 to 2 minutes and repeat the readings, and then reposition to the standing position for 1 to 2 minutes and repeat the readings. Results consistent with orthostatic changes would have a decrease of 20 mm Hg or more in systolic BP, a decrease of 10 mm Hg or more in diastolic BP, and/or an increase in HR of greater than or equal to 20 beats/min with position changes
The nurse reviews the medication record of a patient with hypertension. Which medication would the nurse recognize as increasing the patient’s risk for hypokalemia?
Clonidine (Catapres)
Bumetanide (Bumex)
Amiloride (Midamor)
Spironolactone (Aldactone)
Bumetanide is a loop diuretic. Hypokalemia is a common adverse effect of this medication. Amiloride is a potassium-sparing diuretic. Spironolactone is an aldosterone-receptor blocker. Hyperkalemia is an adverse effect of both amiloride and spironolactone. Clonidine is a central-acting α-adrenergic antagonist and does not cause electrolyte abnormalities.
An older adult with hypertension admitted to the emergency department with a blood pressure of 234/148 mm Hg is started on nitroprusside. After 1 hour of treatment, the mean arterial blood pressure (MAP) is 55 mm Hg. Which nursing action is a priority?
Start an infusion of 0.9% normal saline at 100 mL/hr.
Maintain the current administration rate of the nitroprusside.
Request insertion of an arterial line for accurate blood pressure monitoring.
Stop the nitroprusside infusion and assess the patient for potential complications.
Nitroprusside is a potent vasodilator medication. A blood pressure of 234/118 mm Hg would have a calculated MAP of 177 mm Hg. Subtracting 25% (or 44 mm Hg) = 133 mm Hg. The initial treatment goal is to decrease MAP by no more than 20%-25% within minutes to 1 hour. For this patient, the goal MAP would be around 133 mm Hg. Minimal MAP required to perfuse organs is around 60 to 65 mm Hg. Lowering the blood pressure too rapidly may decrease cerebral, coronary, or renal perfusion and could precipitate a stroke, myocardial infarction, or renal failure. The priority is to stop the nitroprusside infusion and then use fluids only if necessary to support restoration of MAP
In caring for a patient with poorly controlled hypertension, which laboratory test result would the nurse recognize as indicating target organ damage?
Serum uric acid of 3.8 mg/dL
Serum creatinine of 2.6 mg/dL
Serum potassium of 3.5 mEq/L
Blood urea nitrogen of 15 mg/dL
The normal serum creatinine level is 0.6 to 1.3 mg/dL. This elevated level indicates target organ damage to the kidneys. The other laboratory results are within normal limits.
The nurse is teaching a women’s group about ways to prevent hypertension. Which information would the nurse include? (Select all that apply.)
Lose weight.
Limit beef consumption.
Limit sodium and fat intake.
Increase fruits and vegetables.
Exercise 30 minutes most days.
Primary prevention of hypertension is to make lifestyle modifications that prevent or delay the increase in BP. Along with exercise for 30 minutes on most days, the DASH eating plan is a healthy way to lower BP by limiting sodium and fat intake, increasing fruits and vegetables, and increasing nutrients that are associated with lowering BP. Beef includes saturated fats, which should be limited. Weight loss may or may not be needed, depending on the person
Which information would the nurse consider when planning care for older adult patients with hypertension? (Select all that apply.)
Systolic blood pressure increases with aging.
White coat syndrome is prevalent in older patients.
Volume depletion contributes to orthostatic hypotension.
Blood pressures should be maintained near 120/80 mm Hg.
Blood pressure drops 1 hour after eating in many older patients.
Older patients require higher doses of antihypertensive medications.
Systolic blood pressure increases with age and patients older than age 60 years should be maintained below 150/90 mm Hg. Older adults are more likely to have elevated blood pressure when taken by health care providers (white coat syndrome). Older patients have orthostatic hypotension related to dehydration, reduced compensatory mechanisms, and medications. One hour after eating, many older patients have a drop in blood pressure. Lower doses of medications may be needed to control blood pressures in older adults related to decreased absorption rates and excretion ability.
The nurse is caring for a patient with chronic obstructive pulmonary disease (COPD), angina, and hypertension. The health care provider adds a new prescription for Atenolol 100 mg PO. For which adverse effect is the patient at risk?
Hypocapnia
Tachycardia
Bronchospasm
Nausea and vomiting
Atenolol is a cardioselective β1-adrenergic blocker that reduces blood pressure and could affect the β2-receptors in the lungs with larger doses or with drug accumulation. Although the risk of bronchospasm is less with cardioselective β-blockers than nonselective β-blockers, atenolol should be used cautiously in patients with COPD
A patient with a history of chronic hypertension is being evaluated in the emergency department for a blood pressure of 200/140 mm Hg. Which patient assessment question is the priority?
Is the patient pregnant?
Does the patient need to urinate?
Does the patient have a headache or confusion?
Is the patient taking antiseizure medications as prescribed?
The nurse’s priority assessments include neurologic deficits, retinal damage, heart failure, pulmonary edema, and renal failure. The headache or confusion could be seen with hypertensive encephalopathy from increased cerebral capillary permeability leading to cerebral edema. In addition, headache or confusion could represent signs and symptoms of a hemorrhagic stroke. Pregnancy can lead to secondary hypertension. Needing to urinate and taking antiseizure medication do not support a hypertensive emergency.
Which information would the nurse teach to a patient about the primary mechanism by which uncontrolled hypertension causes organ damage?
Hypertension promotes atherosclerosis and damage to the walls of the arteries.
Hypertension causes direct pressure on organs, resulting in necrosis and scar tissue.
Hypertension causes thickening of the capillary membranes, leading to hypoxia of organ systems.
Hypertension increases blood viscosity, intravascular coagulation and tissue necrosis distal to occlusions.
Hypertension is a major risk factor for the development of atherosclerosis by mechanisms not yet fully known. Atherosclerosis damages the walls of arteries and reduces circulation to target organs and tissues.
A patient who is taking nifedipine (Procardia XL) for antihypertensive therapy continues to have blood pressures over 140/90 mm Hg. Which action would the nurse take next?
Ask the patient to make an exercise plan.
Assess the patient’s adherence to therapy.
Teach the patient to follow the DASH diet.
Request a prescription for a thiazide diuretic.
A long-acting calcium-channel blocker such as nifedipine causes vascular smooth muscle relaxation, resulting in decreased systemic vascular resistance and arterial blood pressure and related side effects. The patient data the nurse has about this patient is very limited, so the nurse needs to begin by assessing adherence to therapy
The nurse is caring for a patient with hypertension who is scheduled to receive a dose of metoprolol tartrate. Which data collected just before administration indicates that the nurse should consult the prescribing provider before administering the dose?
O2 saturation 93%
Pulse 48 beats/min
Respirations 24 breaths/min
Blood pressure 118/74 mm Hg
Because metoprolol is a β1-adrenergic blocking agent, it can cause hypotension and bradycardia as adverse effects. The nurse should withhold the dose and consult with the health care provider for parameters regarding pulse rate limits.
When teaching to a patient with hypertension, which protein source would the nurse recommend restricting?
Broiled fish
Roasted duck
Roasted turkey
Baked chicken breast
Roasted duck is high in fat, which should be avoided by the patient with hypertension. Weight loss may slow the progress of atherosclerosis and overall cardiovascular disease risk. The other meats are lower in fat and are therefore acceptable in the diet.
1. Relate the pathophysiology of primary hypertension to the clinical manifestations and complications.
2. Choose appropriate strategies for the prevention of primary hypertension.
3. Describe the interprofessional care for primary hypertension.
4. Explain the interprofessional care of the older adult with primary hypertension.
5. Prioritize the nursing management of the patient with primary hypertension.
6. Describe the nursing and interprofessional care of a patient with a hypertensive crisis.
blood pressure (BP)
elevated blood pressure, Table 36.2
hypertension
hypertensive crisis
orthostatic hypotension
primary hypertension
secondary hypertension
systemic vascular resistance (SVR)
NORMAL REGULATION OF BLOOD PRESSURE
Blood pressure (BP) is the force exerted by the blood against the walls of the blood vessel.
Maintaining tissue perfusion during activity and rest must be adequate.
Regulation of BP involves nervous, cardiovascular, endothelial, renal, and endocrine functions.
HYPERTENSION
Classification of Hypertension
Hypertension, or high BP, is defined as either a persistent systolic BP (SBP) greater than or equal to 130 mm Hg or a diastolic BP (DBP) greater than or equal to 80 mm Hg. If either the SBP or DBP is outside of a normal range, the higher measurement will determine the hypertension classification.
Hypertension is classified as follows:
Elevated blood pressure is defined as an SBP between 120-129 mm Hg and a DBP < 80 mm Hg.
Hypertension (Stage 1) is defined as an SBP between 130-139 mm Hg or a DBP between 80-
89 mm Hg.
Hypertension (Stage 2) is defined as an SBP > 140 mm Hg or a DBP > 90 mm Hg.5 Etiology
Primary hypertension is elevated BP without an identified cause. It accounts for 90% to 95% of all cases of hypertension.
Secondary hypertension is elevated BP with a specific cause. It accounts for 5% to 10% of hypertension in adults.
Pathophysiology of Primary Hypertension.
The hemodynamic hallmark of hypertension is persistently increased systemic vascular resistance (SVR).
This persistent elevation in SVR may occur in several ways. Defects in any of the mechanisms involved in the maintenance of normal BP, including sodium intake, the renin-angiotensin-aldosterone mechanism, and sympathetic nervous system (SNS) stimulation, can result in the development of hypertension.
Defects in glucose, insulin, and lipoprotein metabolism are common in primary hypertension.
Contributing factors to the development of hypertension include cardiovascular risk factors combined with socioeconomic conditions and gender and ethnic differences.
Endothelial dysfunction is a marker for CVD and primary hypertension.
Clinical Manifestations
Called the “silent killer” because it is often asymptomatic until it becomes severe
and target organ disease occurs.
Target organ diseases occur in the heart (hypertensive heart disease), brain
(cerebrovascular disease), peripheral vessels (peripheral vascular disease), kidney
(nephrosclerosis), and eyes (retinopathy).
It is one of the leading causes of end-stage renal disease.
Damage to retinal vessels indicates concurrent vessel damage in the heart, brain, and kidney. Manifestations of severe retinal damage include blurring of vision, retinal hemorrhage, and loss of vision.
There is a direct relationship between hypertension and cardiovascular disease (CVD). Hypertension is a major risk factor for coronary artery disease (CAD), stroke, and cerebral atherosclerosis.
Sustained high BP increases the cardiac workload and produces left ventricular hypertrophy (LVH). Progressive LVH, especially in association with CAD, is associated with the development of heart failure.
Diagnostic Studies
Basic laboratory studies are done to (1) identify or rule out causes of secondary hypertension, (2) evaluate target organ disease, (3) determine overall cardiovascular risk, or (4) establish baseline levels before starting therapy.
Routine urinalysis, BUN, serum creatinine, and creatinine clearance levels are used to screen for renal involvement and to provide baseline information about kidney function.
Lipid profiles provide information about risk factors that predispose to atherosclerosis and cardiovascular disease.
12 lead ECG and echocardiography provide information about the heart status.
Ambulatory BP monitoring (ABPM) measures the BP at preset intervals over a 24-hour period. • Home BP Monitoring (HBPM) measures the BP at home to confirm hypertension diagnosis and for titration of oral agents. HBPM should be done in conjunction with regular follow up visits with the HCP.
Interprofessional Care
Target goals take into consideration both age and comorbidities when recommending treatment options.
Lifestyle modifications are directed toward reducing the patient's BP and overall cardiovascular risk. The AHA’s “Life’s Simple 7” steps support ways to modify and improve health. These are: (1) manage blood pressure, (2) control cholesterol, (3) reduce blood sugar, (4) get active, (5) eat better, (6) lose weight, and (7) stop smoking. Other modifications by the taskforce on hypertension address sodium restrictions and alcohol intake.
Common dietary modifications are the Mediterranean or DASH diet, with reduced sodium and fat intake.
Drug Therapy
Drugs currently available for treating hypertension work by (1) decreasing the volume of circulating blood and/or (2) reducing SVR.
Diuretics promote sodium and water excretion, reduce plasma volume, and reduce the vascular response to catecholamines.
Adrenergic-inhibiting agents act by decreasing the SNS effects that increase BP. Adrenergic inhibitors include drugs that work centrally on the vasomotor center and peripherally to inhibit norepinephrine release or to block the adrenergic receptors on blood vessels.
Direct vasodilators decrease the BP by relaxing the vascular smooth muscle and reducing SVR.
Calcium channel blockers increase sodium excretion and cause arteriolar vasodilation by preventing the movement of extracellular calcium into cells.
Angiotensin-converting enzyme (ACE) inhibitors prevent the conversion of angiotensin I to angiotensin II and reduce angiotensin II (A-II)–mediated vasoconstriction and sodium and water retention.
A-II receptor blockers (ARBs) prevent angiotensin II from binding to its receptors in the walls of the blood vessels.
Most patients who are hypertensive will need 2 or more antihypertensive drugs to achieve their BP goals.
Side effects and adverse effects of antihypertensive therapy may be so severe or undesirable that the patient does not adhere to therapy. Patient and caregiver teaching related to drug therapy is needed to identify and minimize side effects and to cope with therapeutic effects.
Resistant hypertension is the failure to reach goal BP in patients who are adhering to full doses of an appropriate 3-drug therapy regimen that includes a diuretic.
NURSING MANAGEMENT: PRIMARY HYPERTENSION
The primary nursing responsibility for long-term management of hypertension is to help the patient in reducing BP and adhering to the treatment plan.
Nursing actions include evaluating therapeutic effectiveness, detecting and reporting any adverse treatment effects, assessing and enhancing adherence, and patient and caregiver teaching.
Patient and caregiver teaching includes: (1) nutritional therapy, (2) drug therapy, (3) lifestyle modification, and (4) home monitoring of BP.
Blood Pressure Measurement
Accurate BP measurements are critical. A key role of the nurse is to provide patient and caregiver teaching about measuring BP at home.
Orthostatic hypotension is defined as a decrease of 20 mm Hg or more in SBP, a decrease of 10 mm Hg or more in DBP, and/or an increase of 20 beats per min or more in pulse from supine to standing.
Orthostatic changes in BP and pulse should be measured in older adults, in patients taking antihypertensive drugs, and in patients who report symptoms consistent with reduced BP upon standing (e.g., light-headedness, dizziness, syncope).
GERONTOLOGIC CONSIDERATIONS: HYPERTENSION
The prevalence of hypertension increases with age. The lifetime risk of developing hypertension is around 90% for normotensive men and women over age 55.
In some older people, there is a wide gap between the first Korotkoff sound and subsequent beats (auscultatory gap). Failure to inflate the cuff high enough may result in an inaccurate SBP.
BP goals in people older than 65 years of age who live independently are no different for other independent living adults under 65 years old. Adults over 65 who are not independent with comorbidities should have drugs added and titrated using clinical judgement and patient preference as the guide.
Orthostatic hypotension often occurs in older adults because of impaired baroreceptor reflex mechanisms, volume depletion, and chronic disease states, such as decreased renal and hepatic function or electrolyte imbalance.
HYPERTENSIVE CRISIS
Hypertensive crisis is a term used to indicate either a hypertensive urgency or emergency. Diagnosis is determined by the presence of target organ disease and the type of treatment the patient will receive.
Hypertensive urgency has no clinical evidence of target organ disease.
Hypertensive urgencies usually do not need IV drugs but can be managed with oral therapy.
A patient with hypertensive urgency who is not hospitalized should have outpatient follow-up care within 24 hours.
Hypertensive emergencies have evidence of target organ disease. It needs hospitalization with intensive care monitoring and the IV administration of antihypertensive drugs, including vasodilators, adrenergic inhibitors, ACE inhibitors, and/or calcium channel blockers. Drugs are titrated based on the MAP.
Regular, ongoing assessment (e.g., ECG monitoring, vital signs, urinary output, level of consciousness, visual changes) is essential to evaluate the patient with severe hypertension.
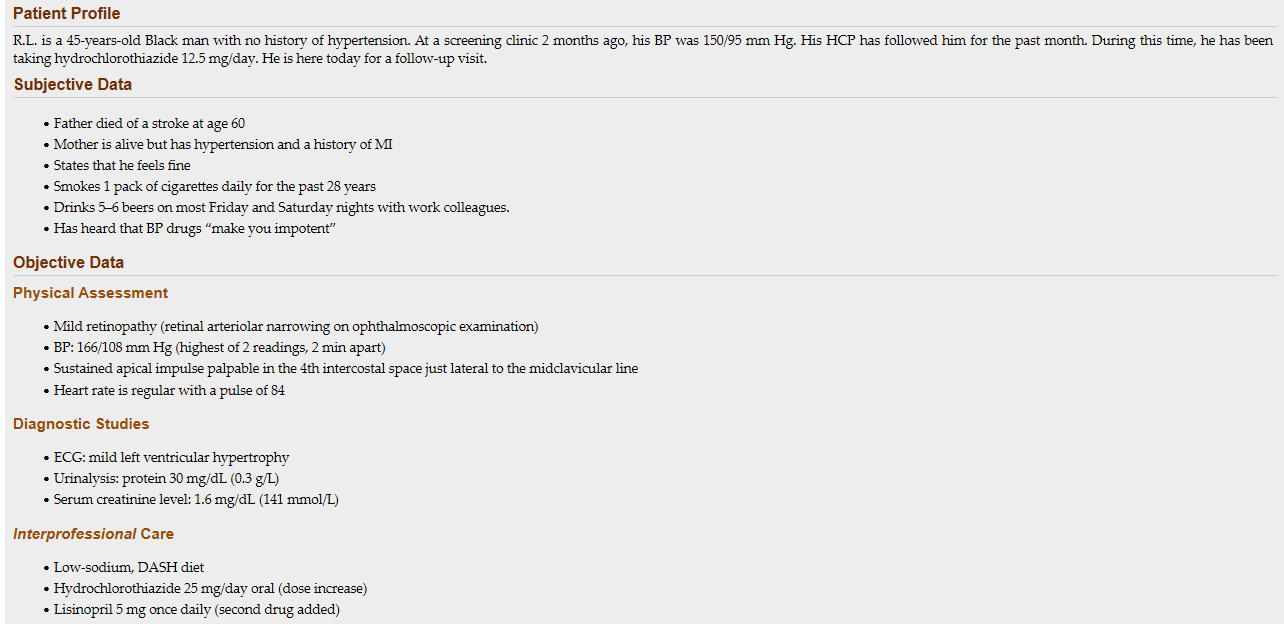 1. Recognize: What risk factors does R.L. have for hypertension?
1. Recognize: What risk factors does R.L. have for hypertension?
R.L’s risk factors include both modifiable and non-modifiable risks. His non-modifiable risk factors include family history and his race/ethnicity. Modifiable risk factors include: tobacco use, alcohol use, and his knowledge deficit related to hypertension,
2. Recognize: What stage of hypertension does R.L. have?
His current blood pressure is 166/108. This places him in Stage 2 hypertension.
3. Analyze: What are the abnormal findings in the objective data?
Physical exam: R.L. has retinopathy on his eye exam. A normal finding is no retinopathy. His blood pressure is abnormal. The apical impulse should be at or medial to the midclavicular line. Diagnostic studies: His ECG has an abnormal finding of left ventricular hypertrophy meaning his heart is enlarged. His urinalysis is abnormal. A normal value for his urine would be no protein. His serum creatinine is higher than the normal range.
4. Analyze: Based on the assessment, what target organ disease may be present?
R.L. has evidence of kidney damage including protein in the urine and elevated creatinine level. He has evidence of heart damage on his ECG and his apical impulse location is likely due to an enlarged heart. The retinopathy indicates potential ocular (eye) damage.
5. Analyze: What additional assessment would be done for this patient?
(1) Height and weight are needed to know if R.L. is obese. (2) The data does not provide as assessment of social determinants of health that are important for understanding risk factors and completing a plan of care. (3) It would be helpful to know more about what types of food he typically eats to understand how to make recommendations for dietary changes. (4) Information is needed about current level of activity before making exercise recommendations. (5) You should ask R.L. about any additional over the counter and supplemental medications that may increase his blood pressure like NSAIDS, cold/sinus medication, high-sodium antacids and appetite suppressants.
6. Plan: What medications would you expect to see ordered for this patient?
R.L.’s blood pressure is not currently controlled with one medication and with lifestyle changes. A second antihypertensive should be added. This will likely include a medication from one of the following categories: Beta-Blockers, Calcium Channel Blockers, ACE inhibitors or Angiotensin Receptor Blockers. In this case lisinopril was selected for this patient because he is already showing signs of kidney damage and lisinopril can protect kidney function.
7. Plan: What referrals may be indicated for R.L.?
R.L. would benefit from a referral to a dietician to discuss dietary changes including the DASH or Mediterranean diet. He may also benefit from referral to a substance abuse specialist due to his alcohol and tobacco use. If he has physical limitations, a physical therapist may be helpful to create an exercise plan.
8. Prioritize: Based on your assessment, which teaching points about hypertension are the most important?
R.L. has some significant modifiable risk factors for his hypertension and ASCVD. You should prioritize medications and medication adherence because his blood pressure has continued to rise. This increases his risk for hypertensive urgency. In addition, teaching about his modifiable risk factors including diet, alcohol, and tobacco use have been shown to be the most effective at decreasing hypertension.
9. Prioritize: What is the most important problem to manage for R.L. right now?
Blood pressure management is the highest priority for this patient. Elevated blood pressure puts him at significant risk for ASCVD and target organ damage.
10. Act: What would you teach this patient about the medications he is prescribed?
You should tell R.L. that the current medication he is taking is not managing his blood pressure. This is not uncommon. Many people need more than one medication to adequately control blood pressure. It is important for him to be consistent taking his medication. He should know that some people do experience sexual side effects with medication, and to tell his HCP about any concerns. You should also educate about possible side effects from his Lisinopril especially angioedema and cough. Tell R.L. if he is experiencing these symptoms he needs to contact his healthcare provider and that if he is having difficulty breathing he should be evaluated immediately.
11. Act: What other teaching is needed for this patient?
Teaching for this patient should be focused on his current misconceptions regarding hypertension and being “hyper” as well as his belief that his medications may prevent sexual function. It is important for him to know that elevated blood pressure can cause damage to many of his body systems and that his testing shows that this is already happening. R.L. has a number of different lifestyle modifications he can make. It is important for him to help set the priority for behaviors he is willing and able to change as this requires life-long changes. R.L. will also need to monitor for signs of orthostasis that can occur when a person is taking blood pressure medications.
12. Evaluate: What follow-up is needed for this patient to assess his response to your plan?
This patient should have a blood pressure recheck in 1 month to assess his response to his medication changes. At this visit medication adherence, lifestyle changes and any side effects should be discussed. R.L. will also benefit from a home blood pressure cuff to monitor his blood pressure at home to see if readings are similar to those in the office. He can bring his home cuff to his next visit so that his machine can be checked for accuracy. He should know that if he experiences chest pain, severe headache, or sudden vision changes that he needs to be evaluated immediately.
1. A defect in which BP-regulating mechanisms can result in the development of hypertension? (select all that apply)
a. Release of norepinephrine
b. Secretion of prostaglandins
c. Stimulation of the sympathetic nervous system
d. Stimulation of the parasympathetic nervous system
e. Activation of the renin-angiotensin-aldosterone system
Norepinephrine (NE) is released from the sympathetic nervous system nerve endings and activates receptors found in the vascular smooth muscle. When the α-adrenergic receptors in smooth muscle of the blood vessels are stimulated by NE, vasoconstriction results. Increased sympathetic nervous system stimulation produces increased vasoconstriction and increased renin release. Increased renin levels activate the renin-angiotensin-aldosterone system, leading to an elevation in BP
2. Which item in a patient history would the nurse recognize as a modifiable risk factor for the development of hypertension?
a. Low-calcium diet
b. Excess alcohol use
c. Family history of hypertension
d. Consumption of a high-protein diet
Alcohol intake is a modifiable risk factor for hypertension. Excessive alcohol intake is strongly associated with hypertension. Males with hypertension should limit their daily intake of alcohol to 2 drinks per day, and one drink per day for females with hypertension.
3. Which information would the nurse apply to a teaching plan for a patient with hypertension?
a. All patients with elevated BP need drug therapy
b. Obese persons must achieve a normal weight to lower BP.
c. It is not necessary to limit salt in the diet if taking a diuretic.
d. Lifestyle modifications are needed for persons with elevated BP.
Lifestyle modifications are needed for all patients with prehypertension and hypertension.
4. Which consideration would the nurse include in the management of the older adult with hypertension?
a. Preventing primary hypertension from converting to secondary hypertension
b. Recognizing that the older adult is less likely to adhere to the drug therapy regimen than a younger adult
c. Ensuring that the patient receives larger initial doses of antihypertensive drugs because of impaired absorption
d. Using a precise technique in assessing the BP of the patient because of the possible presence of orthostatic hypertension
Careful technique is important in assessing BP in older adults. In some older people, there is a wide gap between the first Korotkoff sound and subsequent beats. This wide interval is called an auscultatory gap. Failure to inflate the cuff high enough may result in an inaccurate systolic BP, one that is too low for the patient.
5. A patient with newly discovered high BP has an average reading of 158/98 mm Hg after 3 months of exercise and diet modifications. Which management strategy would the nurse expect?
a. Drug therapy will be needed because the BP has not reached the goal.
b. BP monitoring should continue for 3 months to confirm a diagnosis of hypertension.
c. Lifestyle changes are less important since they were not effective, and drugs will be started.
d. More changes in the patient’s lifestyle are needed for a longer time before starting drug therapy.
The patient has hypertension, stage 1. Lifestyle modifications will continue, but starting drug therapy is a priority. Reducing BP can help to prevent serious complications related to hypertension.
6. A patient is admitted to the hospital in a hypertensive emergency (BP 244/142 mm Hg). Sodium nitroprusside is started to treat the elevated BP. Which management strategies would the nurse anticipate? (select all that apply)
a. Measuring hourly urine output
b. Continuous BP monitoring with an arterial line
c. Decreasing the MAP by 50% within the first hour
d. Maintaining bed rest and giving tranquilizers to lower the BP
e. Assessing the patient for signs of heart failure and changes in mental status
Measure urine output hourly to assess renal perfusion. Patients treated with IV sodium nitroprusside should have continuous intraarterial BP monitoring. Hypertensive crisis can cause encephalopathy, intracranial or subarachnoid hemorrhage, acute left ventricular failure, MI, renal failure, dissecting aortic aneurysm, and retinopathy. The initial treatment goal is to decrease the mean arterial pressure (MAP) by no more than 25% within minutes to 1 hour. Patients receiving IV antihypertensive drugs may be restricted to bed rest. Getting up (e.g., to use the toilet/commode) may cause severe cerebral ischemia and fainting.
The nurse is caring for a patient who has taken hydrochlorothiazide for 10 years to treat hypertension. Which parameter indicates effectiveness of this drug therapy?
BP 128/78 mm Hg
Weight loss of 2 lb
Absence of ankle edema
Output of 600 mL per 8 hours
Hydrochlorothiazide may be used alone as monotherapy to manage hypertension or in combination with other medications if not effective alone. After the first few weeks of therapy, the diuretic effect diminishes, but the antihypertensive effect remains. Because the patient has been taking this medication for 10 years, the most direct measurement of its intended effect would be the blood pressure.
The nurse supervises assistant personnel (AP) taking the blood pressure of a patient admitted with heart failure who is obese. Which action by the AP will require the nurse to intervene?
Deflating the blood pressure cuff at a rate of 8 to 10 mm Hg/sec
Waiting 2 minutes after position changes to take orthostatic pressures
Taking the blood pressure with the patient’s arm at the level of the heart
Taking a forearm blood pressure if the largest cuff will not fit the patient’s upper arm
The cuff should be deflated at a rate of 2 to 3 mm Hg/sec. The arm should be supported at the level of the heart for accurate blood pressure measurements. Using a cuff that is too small causes a falsely high reading and too large causes a falsely low reading. If the maximum size blood pressure cuff does not fit the upper arm, the forearm may be used. Orthostatic blood pressures should be taken within 1 to 2 minutes of repositioning the patient.
A middle aged patient is diagnosed with hypertension and receives a prescription for benazepril. After providing teaching, which statement by the patient indicates correct understanding?
“If I take this medication, I will not need to follow a special diet.”
“It is normal to have some swelling in my face while taking this medication.”
“I will need to eat foods such as bananas and potatoes that are high in potassium.”
“If I develop a dry cough while taking this medication, I should notify my doctor.”
Benazepril is an angiotensin-converting enzyme inhibitor. The medication inhibits breakdown of bradykinin, which may cause a dry, hacking cough. Other adverse effects include hyperkalemia. Swelling in the face could indicate angioedema and should be reported immediately to the prescriber. Patients taking drug therapy for hypertension should also attempt lifestyle modifications to lower blood pressure such as a reduced sodium diet.
When teaching how lisinopril helps lower the patient’s blood pressure, which mechanism of action would the nurse explain?
Blocks β-adrenergic effects.
Relaxes arterial and venous smooth muscle.
Inhibits conversion of angiotensin I to angiotensin II.
Reduces sympathetic outflow from central nervous system.
Lisinopril is an angiotensin-converting enzyme inhibitor that inhibits the conversion of angiotensin I to angiotensin II, which reduces angiotensin II–mediated vasoconstriction and sodium and water retention. β-Blockers result in vasodilation and decreased heart rate. Direct vasodilators relax arterial and venous smooth muscle. Central-acting α-adrenergic antagonists reduce sympathetic outflow from the central nervous system to produce vasodilation and decreased systemic vascular resistance and blood pressure
The nurse teaches a young adult patient newly diagnosed with hypertension about lifestyle modifications to reduce blood pressure. Which patient statement demonstrates further teaching is required?
“I will avoid adding salt to my food during or after cooking.”
“If I lose weight, I might not need to continue taking medications.”
“I can lower my blood pressure by switching to smokeless tobacco.”
“Diet changes can be as effective as taking blood pressure medications.”
Nicotine contained in tobacco products (smoking and chew) cause vasoconstriction and increase blood pressure. Persons with hypertension should restrict sodium to 1500 mg/day by avoiding foods high in sodium and not adding salt in preparation of food or at meals. Weight loss can decrease blood pressure between 5 to 20 mm Hg. Following dietary recommendations (e.g., the DASH diet) lowers blood pressure, and these decreases compare with those achieved with blood pressure–lowering medication.
Which instruction would the nurse give when teaching a patient about stage 1 hypertension?
Increase water intake.
Restrict sodium intake.
Increase protein intake.
Use calcium supplements.
The patient should decrease intake of sodium. This will help to control hypertension, which can be aggravated by excessive salt intake, which in turn leads to fluid retention. Protein intake does not affect hypertension. Calcium supplements are not recommended to lower blood pressure.
The assistive personnel (AP) is taking orthostatic vital signs. In the supine position, the patient’s blood pressure (BP) is 130/80 mm Hg, and the heart rate (HR) is 80 beats/min. In the sitting position, the BP is 140/80, and the HR is 90 beats/min. Which action would the nurse instruct the AP to take next?
Repeat BP and HR in this position.
Record the BP and HR measurements.
Take BP and HR with patient standing.
Return the patient to the supine position.
The vital signs taken do not reflect orthostatic changes, so the AP will continue with the measurements while the patient is standing. There is no need to repeat or delay the readings. The patient does not need to return to the supine position. When assessing for orthostatic changes, the AP will take the BP and pulse in the supine position, then place the patient in a sitting position for 1 to 2 minutes and repeat the readings, and then reposition to the standing position for 1 to 2 minutes and repeat the readings. Results consistent with orthostatic changes would have a decrease of 20 mm Hg or more in systolic BP, a decrease of 10 mm Hg or more in diastolic BP, and/or an increase in HR of greater than or equal to 20 beats/min with position changes
The nurse reviews the medication record of a patient with hypertension. Which medication would the nurse recognize as increasing the patient’s risk for hypokalemia?
Clonidine (Catapres)
Bumetanide (Bumex)
Amiloride (Midamor)
Spironolactone (Aldactone)
Bumetanide is a loop diuretic. Hypokalemia is a common adverse effect of this medication. Amiloride is a potassium-sparing diuretic. Spironolactone is an aldosterone-receptor blocker. Hyperkalemia is an adverse effect of both amiloride and spironolactone. Clonidine is a central-acting α-adrenergic antagonist and does not cause electrolyte abnormalities.
An older adult with hypertension admitted to the emergency department with a blood pressure of 234/148 mm Hg is started on nitroprusside. After 1 hour of treatment, the mean arterial blood pressure (MAP) is 55 mm Hg. Which nursing action is a priority?
Start an infusion of 0.9% normal saline at 100 mL/hr.
Maintain the current administration rate of the nitroprusside.
Request insertion of an arterial line for accurate blood pressure monitoring.
Stop the nitroprusside infusion and assess the patient for potential complications.
Nitroprusside is a potent vasodilator medication. A blood pressure of 234/118 mm Hg would have a calculated MAP of 177 mm Hg. Subtracting 25% (or 44 mm Hg) = 133 mm Hg. The initial treatment goal is to decrease MAP by no more than 20%-25% within minutes to 1 hour. For this patient, the goal MAP would be around 133 mm Hg. Minimal MAP required to perfuse organs is around 60 to 65 mm Hg. Lowering the blood pressure too rapidly may decrease cerebral, coronary, or renal perfusion and could precipitate a stroke, myocardial infarction, or renal failure. The priority is to stop the nitroprusside infusion and then use fluids only if necessary to support restoration of MAP
In caring for a patient with poorly controlled hypertension, which laboratory test result would the nurse recognize as indicating target organ damage?
Serum uric acid of 3.8 mg/dL
Serum creatinine of 2.6 mg/dL
Serum potassium of 3.5 mEq/L
Blood urea nitrogen of 15 mg/dL
The normal serum creatinine level is 0.6 to 1.3 mg/dL. This elevated level indicates target organ damage to the kidneys. The other laboratory results are within normal limits.
The nurse is teaching a women’s group about ways to prevent hypertension. Which information would the nurse include? (Select all that apply.)
Lose weight.
Limit beef consumption.
Limit sodium and fat intake.
Increase fruits and vegetables.
Exercise 30 minutes most days.
Primary prevention of hypertension is to make lifestyle modifications that prevent or delay the increase in BP. Along with exercise for 30 minutes on most days, the DASH eating plan is a healthy way to lower BP by limiting sodium and fat intake, increasing fruits and vegetables, and increasing nutrients that are associated with lowering BP. Beef includes saturated fats, which should be limited. Weight loss may or may not be needed, depending on the person
Which information would the nurse consider when planning care for older adult patients with hypertension? (Select all that apply.)
Systolic blood pressure increases with aging.
White coat syndrome is prevalent in older patients.
Volume depletion contributes to orthostatic hypotension.
Blood pressures should be maintained near 120/80 mm Hg.
Blood pressure drops 1 hour after eating in many older patients.
Older patients require higher doses of antihypertensive medications.
Systolic blood pressure increases with age and patients older than age 60 years should be maintained below 150/90 mm Hg. Older adults are more likely to have elevated blood pressure when taken by health care providers (white coat syndrome). Older patients have orthostatic hypotension related to dehydration, reduced compensatory mechanisms, and medications. One hour after eating, many older patients have a drop in blood pressure. Lower doses of medications may be needed to control blood pressures in older adults related to decreased absorption rates and excretion ability.
The nurse is caring for a patient with chronic obstructive pulmonary disease (COPD), angina, and hypertension. The health care provider adds a new prescription for Atenolol 100 mg PO. For which adverse effect is the patient at risk?
Hypocapnia
Tachycardia
Bronchospasm
Nausea and vomiting
Atenolol is a cardioselective β1-adrenergic blocker that reduces blood pressure and could affect the β2-receptors in the lungs with larger doses or with drug accumulation. Although the risk of bronchospasm is less with cardioselective β-blockers than nonselective β-blockers, atenolol should be used cautiously in patients with COPD
A patient with a history of chronic hypertension is being evaluated in the emergency department for a blood pressure of 200/140 mm Hg. Which patient assessment question is the priority?
Is the patient pregnant?
Does the patient need to urinate?
Does the patient have a headache or confusion?
Is the patient taking antiseizure medications as prescribed?
The nurse’s priority assessments include neurologic deficits, retinal damage, heart failure, pulmonary edema, and renal failure. The headache or confusion could be seen with hypertensive encephalopathy from increased cerebral capillary permeability leading to cerebral edema. In addition, headache or confusion could represent signs and symptoms of a hemorrhagic stroke. Pregnancy can lead to secondary hypertension. Needing to urinate and taking antiseizure medication do not support a hypertensive emergency.
Which information would the nurse teach to a patient about the primary mechanism by which uncontrolled hypertension causes organ damage?
Hypertension promotes atherosclerosis and damage to the walls of the arteries.
Hypertension causes direct pressure on organs, resulting in necrosis and scar tissue.
Hypertension causes thickening of the capillary membranes, leading to hypoxia of organ systems.
Hypertension increases blood viscosity, intravascular coagulation and tissue necrosis distal to occlusions.
Hypertension is a major risk factor for the development of atherosclerosis by mechanisms not yet fully known. Atherosclerosis damages the walls of arteries and reduces circulation to target organs and tissues.
A patient who is taking nifedipine (Procardia XL) for antihypertensive therapy continues to have blood pressures over 140/90 mm Hg. Which action would the nurse take next?
Ask the patient to make an exercise plan.
Assess the patient’s adherence to therapy.
Teach the patient to follow the DASH diet.
Request a prescription for a thiazide diuretic.
A long-acting calcium-channel blocker such as nifedipine causes vascular smooth muscle relaxation, resulting in decreased systemic vascular resistance and arterial blood pressure and related side effects. The patient data the nurse has about this patient is very limited, so the nurse needs to begin by assessing adherence to therapy
The nurse is caring for a patient with hypertension who is scheduled to receive a dose of metoprolol tartrate. Which data collected just before administration indicates that the nurse should consult the prescribing provider before administering the dose?
O2 saturation 93%
Pulse 48 beats/min
Respirations 24 breaths/min
Blood pressure 118/74 mm Hg
Because metoprolol is a β1-adrenergic blocking agent, it can cause hypotension and bradycardia as adverse effects. The nurse should withhold the dose and consult with the health care provider for parameters regarding pulse rate limits.
When teaching to a patient with hypertension, which protein source would the nurse recommend restricting?
Broiled fish
Roasted duck
Roasted turkey
Baked chicken breast
Roasted duck is high in fat, which should be avoided by the patient with hypertension. Weight loss may slow the progress of atherosclerosis and overall cardiovascular disease risk. The other meats are lower in fat and are therefore acceptable in the diet.