OCTH 6130 Psychosocial Occupational Therapy: Framing and Evaluation (copy)
Development of PEO Model
PEO = person, environment, & occupation
Person: mind, body, emotion, spirit
Environment: Broad
“Context in which occupational performance takes place.”
What are elements of the environment?
Physical location, local social situations (family & neighborhoods, community, provincial/state, national and institutional (health insurance, transportation systems, employment opportunities)
Occupation: activities & tasks people engage in carrying
Interactive Frameworks
Environmental press
Forces in the environment, together with individual needs, evoke a response
Adaptation
Skill and challenge are right = good behavior
Cause/effect 🡪 behavior, doesn’t account for occupations
Flow (Csikszentmihalyi)
Losing self in an activity
Nested in social systems (Bronfenbrenner)
Individual influenced
Microsystem (immediate, family, school, peers)
Mesosystem (interconnections, relationship child’s home and school)
Exosystem (external, partners workplace)
Macrosystem (institutions, government, values, customs)
Mutually accounts for occupations
P x E x O fit and interactions
Person x Occupation
Occupation x Environment
Person x Environment
Occupational performance
dynamic relationship between PEO over a lifespan
Choose and participate in occupation for enjoyment
Things shift over time – not static – continually changing
Dimensions of time and space
Time: experience present, remember past, hold ideas and dreams for the future = embody all three at once
Space: emotional element and meaning
Location = physical space people can engage in occupation
Takeaways: client-centered approach & reflective (evidence-based)
Introduction to the Person
Recovery model
Promotes optimism and hope that individuals with psychiatric conditions can achieve wants and needs
Person first language
Performance skills
MNEUMONIC: Colorful Butterflies Soar, Captivating Radiant Mesmerizing Eyes, Creating Serene Peacefulness, Radiating True Happiness
Cognition (how people think about themselves)
Attention
Memory
Executive function
Impacted with schizophrenia, autism disorder, and depression
Cognitive beliefs (How you review self and world)
How people think about themselves and the world
CBT=altering cognitive distortions
Impacted with schizophrenia and eating disorders
Sensory processing
Environment
Reduce restraints and seclusion
Reduce noise level
Calmer environment
Coping and resilience
Strategies:
Emotion or problem focused
Approach or avoidance oriented
Motivation
Practitioner address motivation as a performance skill
It doesn’t have to be a stigmatizing factor of mental illness
MoHO as volition
Emotion
Regulate emotion
Essential to health and occupational engagement
Dialectical behavioral therapy
Communication and socialization
Collaboration = occupational performance
Communication
Impacted by autism, anxiety disorder, and schizophrenia
Pain regulation
Reciprocal relationships
Pain sensitivity increases in individuals with Alzheimer’s disease.
Pain sensitivity decreases in individuals with schizophrenia.
Chronic pain often co-occurs with depression.
Time use and habits
Activity initiation
Occupational balance
Narrative (assessment and intervention)
Assessment:
OPHI-II
Occupational Performance History Interview
Role checklist
Self-assessment
COSA Children’s Occupational Self-assessment
Intervention:
Person’s story
Collaboration and understanding
Promote conversations
Purpose of Evaluation:
Data gathering and measuring occupational performance
Occupational profile: summarize persons occupational history
Analysis of occupational performance: practitioner uses therapeutic reasoning to determine areas of occupational performance that need to be assessed.
Evaluation Process Steps
1: screen data to guide therapeutic reasoning
Who is the person? What do I know? What are their concerns?
2: choose assessments
Consider:
Utility (quality of life)
Validity (measure what intends to be measured)
Reliability (consistency of measure)
3: administer assessment
Obtain consent
Gather material
Establish rapport
4: occupational profile
AOTA template structure
Identify occupational importance
5: analyze occupational performance
6: synthesize data and set goals
Specific
Measurable
Attainable
Relevant
Time
7: reevaluate
Ongoing process
Measures outcomes
Is the intervention effective
Builds body of evidence that supports occupational therapy
Assessment Methods
Interviews
Canadian Occupational Performance Measure
OPHI-II
Occupational Circumstances Assessment Interview and Rating Scale
Kawa River Model
Self-Report Assessment
Role checklist
Occupational self-assessment
Child-occupational self-assessment
Adolescent/adult sensory profile
Performance Assessment
Allen Cognitive Level Screen
A M P S
Executive Function Performance Test
Performance Assessment of Self-Care
Volitional Questionnaire
Cognition
Schizophrenia and cognition (miss input)
Begins in late teens or early 20s
Visual processing impairments
Perceiving motion and speed of motion
Eye tracking
Social difficulty
Interpret emotional expression
Auditory processing
Meaning of intonation and rhythm of speech
Interpreting facial expression
Components of cognition
Cognition: Processes associated with perceiving, making
sense of, and using informationAttention
Automatic and controlled processing 🡪 simplify tasks, repeated practice
Selective attention 🡪 reduce irrelevant stimuli, use cues
Divided attention 🡪 separate tasks to focus attention
Vigilance 🡪 incorporate breaks
Components of memory
Memory
Semantic: memory for facts
Episodic: memory for events that happen to you
Procedural: memory about how to do something
Strategies:
Short term 🡪 memory aids
Long term 🡪 mnemonics
Working 🡪 simplify tasks, assistive devices
Executive function
Requires a level of awareness and conscious effort
Strategies:
Concept formation & Categorization
Cue sheets, exemplars
Schemas
Mental representation that includes relationships of a concept (mental image)
Simple maps
Scripts:
What happens when you get to a place (steps) predicts what happens next
Simple maps
Models and techniques for cognitive impairment
Requires a level of awareness and conscious effort
Strategies:
Concept formation & Categorization
Cue sheets, exemplars
Schemas
Mental representation that includes relationships of a concept (mental image)
Simple maps
Scripts:
What happens when you get to a place (steps) predicts what happens next
Simple maps
Problem-solving
Involves overcoming obstacles that interfere with goal attainment
Decision-making
Metacognition
Strategies:
Problem solving 🡪 eliminate common problem
Decision making 🡪 limit options
Metacognition 🡪 promote reflection
Models and techniques for cognitive impairment
Cognitive remediation: improve/restore specific cognitive skills
Letter cancellation task
Dynamic interactional approach
Functional information processing
Strategy across different activities that gradually change
Cognitive adaptation
Adapting tasks and environments
Cognitive adaptation training
Apathetic behaviors
Strategies: checklist, labels, prompts, cues, etc.
Disinhibited behaviors
Strategies: removal of distractions and organization of materials
Cognitive Orientation to Daily Occupational Performance (CO-OP)
1. Goal–what do you want to do?
2. Plan–how will you go about doing it?
3. Do–carry out the plan
4. Check–did the plan work? Does it need to be modified?
Cognitive Disabilities Model
Best for for individual to promote participation
What a person can do, will do, and may do.
Assessments to test cognitive skills
Test of Everyday Attention–eight everyday tasks
Adults and children with ADHD or Neuro/Psych
Attention whit engaging
Multiple Errands Test–administer in a shopping mall
Adults with brain injury, stroke, or psych
Executive functioning in natural environment
Dynamic Loewenstein Occupational Therapy Cognitive
Assessment (DLOTCA)–assess orientation, visuomotor
organization, and thinking
Dynamic Loewenstein Occupational Therapy Cognitive
Assessment (DLOTCA)–assess orientation, visuomotor
organization, and thinkingAdults with brain injury or pysch, geriatric version for 70 years+
Person’s ability to learn
Executive Functioning Performance Test (EFPT)—assesses
cognition and executive functioningAdults with neuro/psych
Executive impairment for independency
Assessments associated with Toglia’s dynamic
interactional approach—assesses categorization and
conceptualization using everyday objectsContextual Memory Test
Adults with brain injury or pysch
Awareness and memory (awareness & recall)
Toglia Category Assessment
Adults with brain injury or psych
Establish categories and switch conceptual sets and ability to apply strategies
Allen Cognitive Level Screen (ACLS)–measure global
cognition as it affects occupational performanceAdults with psych disorders, dementia, and disruption of cognitive processing skills
Do-Eat–measure task performance, sensory motor skills,
and executive functionChildren 5 to 8
Continuous Performance Test (CPT)–measure cognition as
it affects occupational performanceAdults with dementia
Intervention:
6 hierarchical levels of functioning
conscious but unresponsive -🡪 comforting interventions
confusion (loss of time) & passive participation 🡪 simple repetitive activities (rocking, music)
minimal attention & devoid of goal direction 🡪 fall prevention programs, simple verbal and tactile cues
significant impairments in memory and attention – disoriented 🡪 caregiver training essential (structured, routine, no distractions)
deficits in executive functioning and processing information, difficulties with IADLs 🡪 modify IADLs or replacement of activities (direct, concrete, and verbal cues)
absence of cognitive disability (can plan, problem solve, and learn) 🡪 help learn new occupations or activities as needed
Sensory processing
Four steps of sensory processing IMPORTANT
Step 1 Nervous system detects sensory stimuli.
Some individuals may be hyperresponsive or hyporesponsive.
Step 2 Brain recognizes or classifies a stimulus.
Step 3 Meaning attributed to the information received.
Step 4 Behavioral response can occur at the level of conscious or unconscious awareness and usually includes cognitive and motor processing.
Sensory modalities (systems)
Visual system
Auditory system
Tactile system
Taste (gustatory) & smell (olfactory) systems
Proprioceptive system
Vestibular system
Sensory processing disorders
Over-responsivity
Exaggerated response of nervous system (motion sickness-vestibular)
Under-responsivity
Lack of response (daydreaming or unfocused)
Sensory seeking
Needs intense input
Sensory processing and children with psychiatric conditions
MNEMONIC: Ants Always Try to Steal My Oreos
“to” refers to trauma and schizo type (2).
ADHD
Autism spectrum disorder
Developmental trauma disorder
Schizophrenia and schizoaffective disorders
Mood disorders
Posttraumatic stress disorder
Obsessive-compulsive disorder
PTSD high in: low registration, sensory seeking, and sensation avoiding.
Depression low in all four DUNN quadrants.
Bipolar disorder highest in sensation seeking
Assessments
Informal observation
While participating in occupations to look for responses to the sensory stimuli
Sensory profiles
Use with Dunn’s Model of Sensory Processing
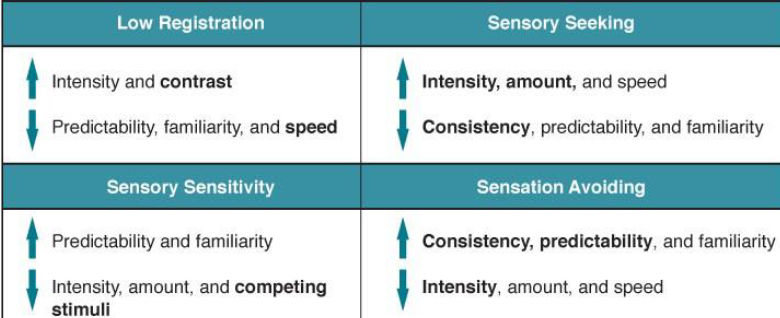
Four quadrants of processing preferences
MNEUMONIC: Rabbits Hop Playfully. Squirrels Hide Acorns. Stinky Little Pigs. Ants Love Picnics.
Low registration [high stimulus, passive response]
Sensory seeking [high stimulus, active response]
Sensory sensitivity low threshold, passive response]
Sensation avoiding [low threshold, active response]
Modify environments to help the person be successful
Matching the sensory processing preferences of the
individual by understanding the environmental features
Sensory processing measure
Assesses the different sensory modalities
Highly sensitive person scale
Rates how respondents relate to environmental features
Interventions
Sensory integration
Selection of activities guided by needs and responses
Focuses on 3 areas of sensory processing
Tactile
Vestibular
Proprioceptive
Sensory based intervention
Identify level of arousal
Alert program 🡪 manage levels of alertness or arousal
Deep pressure touch strategies = tactile sensory input
Motivation
Theories of motivation
Maslow’s hierarchy of needs
Biological (food, water, sleep) (PRIORITY)
Safety (health, financial security)
Affiliation (friends, family, belonging)
Esteem (self-efficacy, confidence)
Self-actualization (meaning, purpose, self-acceptance)
Intervention: address lowest level of unmet need. Establish rapport and demonstrate safety for client.
Self-Determination Theory
Intrinsic (self) & extrinsic (obtain an outcome)
Competence – your knowledge and mastery
Autonomy – source of motivation
Relatedness – connection
Self-Regulation – 3 levels
External – rewards and punishments
Introjected – avoidance of guilt and anxiety; enhance self esteem
Regulation through identification – activity consciously and personally valued
Integrated regulation – activity is for self
Procrastination – waiting last minute
Intervention: group activities, mentorship, and role modeling
Flow
Intense and concentrated on activity
Action and awareness
Loss of self-consciousness
Distortion of time
Intervention: JUST RIGHT FIT
Transtheoretical Model (mostly for substance abuse but can be used for life changes)
MNEUMONIC: Playful Cats Pounce and Meow Regularly
Precontemplation
Contemplation
Planning
Action
Maintenance
Relapse
Intervention: identify stage of change and use strategies to help them move to next level
Self-Efficacy
Belief in your own capability, which motivates you to act.
Mastery
Modeling
Social persuasion
Somatic/emotional states
Intervention: avoid criticism, provide positive, specific and sincere feedback. Break down activities for multiple opportunities for success
Approach & Avoidance
Approach: Behavioral Activation System
What can I do
What can go well
Active in individuals who are impulsive
Slow them down
Avoidance: Behavioral Inhibition System
What can go wrong
Person who is overly cautious
Positive feedback
Intervention: address negative emotions and impulsiveness. Support positive emotions and help change emotional associations, incorporate rewards and remove punishments associated with the activity.
MOHO – Model of Human Occupation
How occupations are motivated and organized into daily life patterns and performed within a person's environment.
Dynamic systems theory
Performance
Habituation
Volitional
Interests
Values
Personal causation
Intervention: target intervention at the factor that interferes with performance
Motivational interviewing
Open-ended questions
Conversation to understanding perspectives of client
Reflective listening
Paraphrased statements
Client provides feedback for accuracy
Affirmation
Acknowledge clients strengths and efforts towards chanfe
Eliciting change talk
Questions focus on desire, ability, reasons, and needs
Motivation and psychiatric disabilities
MNEUMONIC: Squirrels And Mice Scurry Incessantly.
Schizophrenia
ADHD
Mood disorders
Substance Abuse
Intellectual Disabilities
Assessment, including BAS/BIS
BIS/BAS Scales
Adolescent & adult
Motivated by rewards or punishment
Dimensions of Mastery Questionnaire
6 months to 19 years old
Persistence while engaging in challenging activity
Goal Attainment Scaling (GAS)
Adults with mental health but universal
Is goal set achieved?
Leisure Motivation Scale
Adolescents & adult
What motivates you to participate in activity
Volitional Questionnaire and Pediatric Volitional Questionnaire
Older children, adolescents, and adults
Pediatrics: 2 to 7 years
Persons motive and how environment affects choices
Mood disorders (features and impact on occupational performance.
Major depression
Episodically
Onset mid 20s but can occur anytime
High rate of recurrence
Bipolar I and II disorder
More than 50% show symptoms before age of 19
Type 1:
Manic episode with or without major depressive disorder
Type 2:
hypomanic disorder with a major depressive disorder
cyclothymic disorder
2-year period – chronic fluctuating hypomanic symptoms and depressive symptoms
Hypomania
periods of elevated, expansive, or irritable mood, but symptoms are at a lower intensity and without marked impairment in social or occupational functioning.
Prevalence
Depression is high
Diagnosis of bipolar disorder is rising sharply among children and adolescents
Men 7% women 12% 2 to 1 ratio
Lifetime prevalence for bipolar disorder is 1% 1 to 1 ratio
Caucasian less likely to seek help
Stigma
Suicide risk factors
Most frequently in males
Peaks in adolescents
15-29 years old
Improve
Easier access to healthcare
Depression is the highest risk factor
Emotion
Modal Model of Emotion
Interactive process between person and situation
situation —> attention —> appraisal —> response
Emotional regulation and dysregulation
Performance skill (emotional regulation)
dysregulation
Negative or unpleasant experience that interferes with goal-oriented activity
Impairment in modulation
Neurophysiology of emotion regulation
Mind-body phenomenon – nervous and endocrine system
Polyvagal theory
how our nervous system responds to stress, danger, and safety
Emotional regulation in adolescence
Starts in early childhood
Difficulties with self-regulation 🡪
Poor stress response
hyperreactivity
Emotional dysregulation and psychiatric disorders
Borderline personality disorder
Responds quickly and intensely
Depression
Avoid and suppress negative emotions and experiences
Anxiety
Worry about future experiences
Mindfulness training and skill development
Substance abuse
Impulse control
Bipolar disorder & disruptive behavior disorders
Assessment
DBT Diary Cards (dialectical behavior therapy)
Adolescents and adults
Measures quality of engagement, pleasure, & capacity to regulate emotional responses
Difficulties in emotion regulation scale
Emotion regulation skills questionnaire
Self-compassion scale
Cognitive emotion regulation questionnaire
Emotion Regulation Questionnaire
Adults
Differences in habitual use of 2 emotion regulation strategies
Cognitive appraisal
Suppression of emotional expression
Mindful attention awareness scale
Five facet mindfulness questionnaires
Dialectical behavior therapy
Has to want to change or won’t be effective
Behavior that’s targeted is understandable
Group setting and training manual should be followed
Mindfulness taught first 🡪 CORE skill of emotional regulation
Interpersonal effective skills
Distress tolerance skills
Contemplating pro/con
Distracting
Self-soothing
Improving movement
Modification
Acceptance and change
Mindfulness-based occupational therapy
Pay attention to present moment and nonjudgmental
 Knowt
Knowt