Renal System Physiology
Overview of the Renal System
The renal system plays a crucial role in maintaining homeostasis by regulating body fluid composition and excreting waste products.
Specific Learning Objectives
Organs of the Urinary System:
Kidneys
Ureters
Urinary Bladder
Urethra
Functions of the Kidneys:
Excretion of waste products.
urine production in kidneys via filtration of blood and reabsorption of nutrients
Regulation of blood volume and pressure.
Control of solute concentration and pH.
producing large amounts of dilute urine or small amounts of concentrated urine
Regulation of red blood cell and vitamin D synthesis.
Location and External Anatomy of the Kidneys:
Positioned on either side of the spine, behind the peritoneum.
Protected by a layer of fat and a fibrous capsule.
Structure of the Nephron:
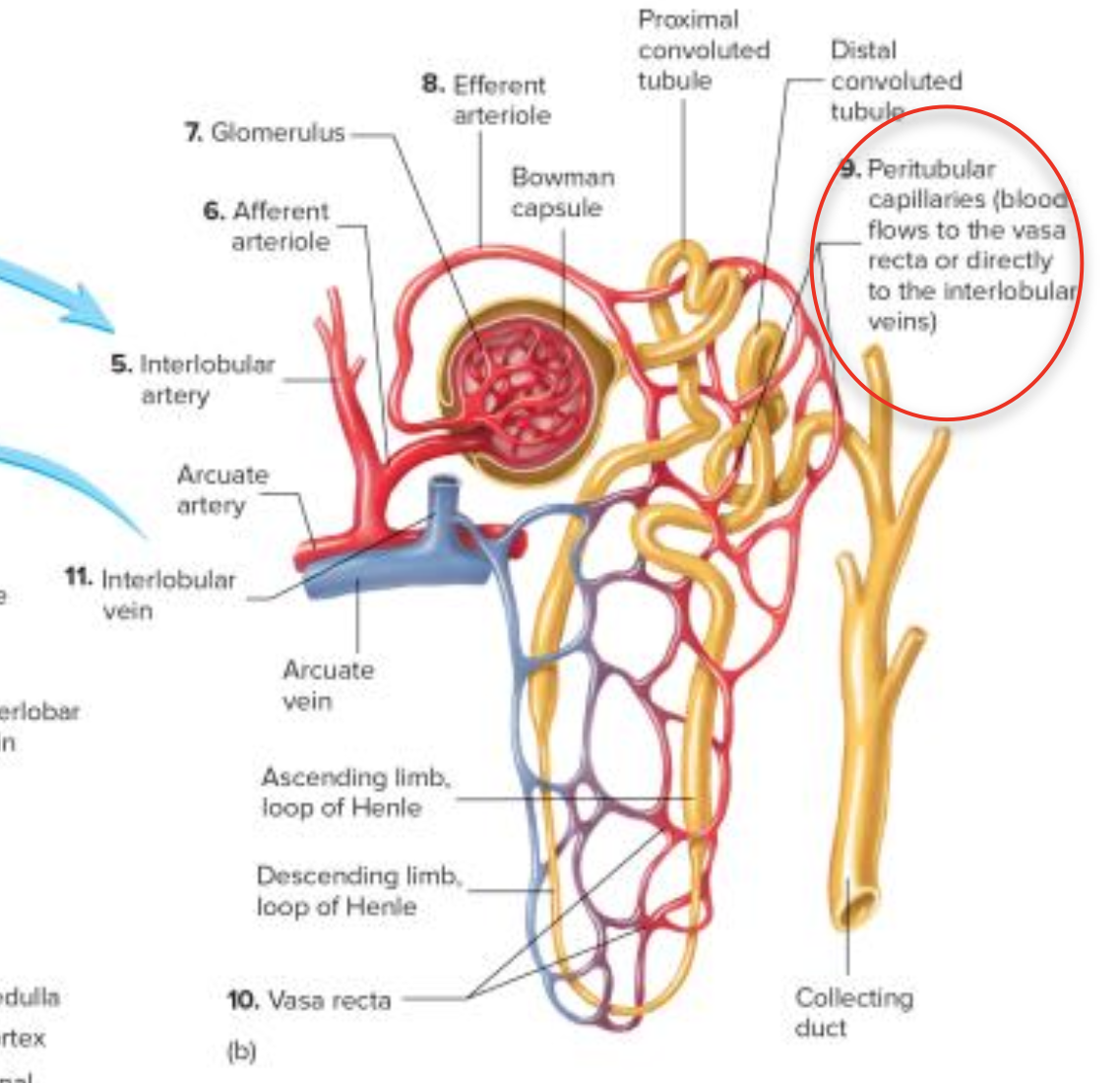
The nephron consists of a renal corpuscle (glomerulus and Bowman’s capsule) and a renal tubule (proximal convoluted tubule, loop of Henle, distal convoluted tubule).
Urine production processes:
Kidneys sort chemicals in blood for removal or return into blood - regulates the body fluid composition
Nephrons are the structural components that sorts the blood
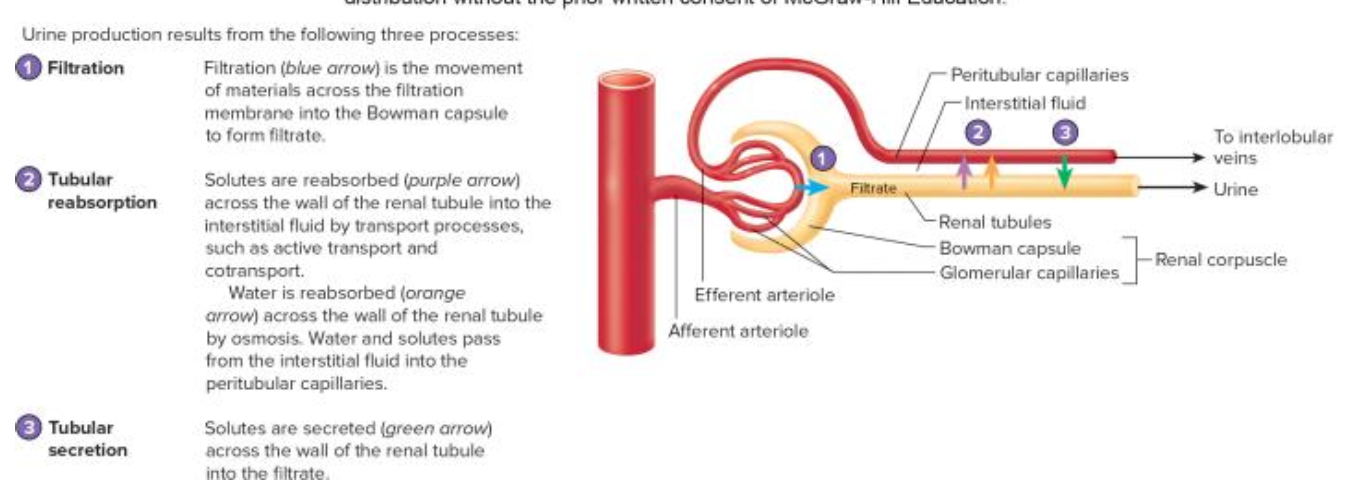
Filtration:
Blood plasma is filtered to form filtrate.
Tubular Reabsorption:
Useful substances are reabsorbed into the blood.
Tubular Secretion:
Additional wastes are secreted into the nephron.
Filtration Membrane Components:
Fenestrae in endothelial cells - highly permeable
Basement membrane.
Filtration slits formed by podocytes.
Nephron Regions and Their Roles:
Proximal Convoluted Tubule: Mainly reabsorbs water, ions, and nutrients.
Loop of Henle: Reabsorption of water and ions; has thin and thick segments.
Distal Convoluted Tubule: Further reabsorption, influenced by hormones.
Collecting Duct: Final adjustments to urine concentration.
Movement Across Cell Membrane of Nephron:
Substances move via active transport for ions and passive transport for water and small molecules.
Sodium is actively transported to create gradients for reabsorption.
Movement of Glucose:
Glucose is reabsorbed via co-transport with sodium in the proximal convoluted tubule.
Waste Products in Urine:
Urea, uric acid, ammonia, creatinine, various ions (H+, K+), and any drugs or toxins.
Urine Production Process
Filtration:
Occurs in the glomerulus.
Driven by blood pressure
Filtration pressure - includes of pressure gradient
99% of filtrate is reabsorbed.
consists of water, glucose, fructose, amino acids, urea, urate ions, creatine, Na+, K+, Ca+2, Cl-
Renal fraction: total blood output by the blood (varies from 12-30%)
Glomerular filtration rate: amount of filtrate produced each minute (~125ml/minute; 180L/day)
Small molecules + ions + H20 (now known as filtrate) are pushed into Bowman’s capsule (doesn’t include RBCs, proteins or large molecules)
FORMATION + REGULATION OF FILTRATE AND BP
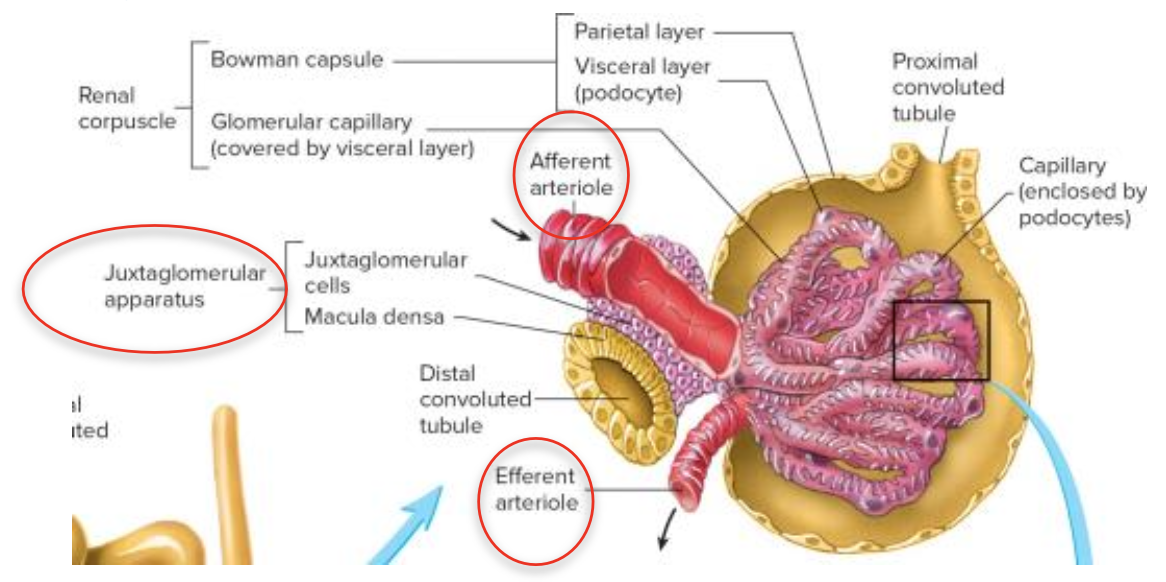
juxtaglomerular apparatus
next to glomerulus - juxtaglomerular cells surrounds afferent arteriole
section of DCT - macula densa (specialised cells)
both of these cells secrete renin - important for formation of filtrate and regulation of BP
Tubular Reabsorption (Process 2):
Return of good, usable substances (filtrate) into blood for cellular function
Reabsorption occurs mainly in the renal tubules, PCT (majority), DCT and in descending limb of loop of Henle.
peritubular capillaries surround tubules - low pressure so substances will diffuse out of renal tubules (~65%) and into capillaries
Active transport of Na+ allows for the reabsorption of glucose and other solutes
HOWEVER both active and passive transport can occur
Under influence of Anti-Diuretic Hormone (ADH), the distal convoluted tubule and collecting duct adjust permeability to water.
Tubular Secretion (Process 3):
Non-filtered substances and toxins are transported into the nephron, typically in the distal convoluted tubule.
Facilitates the excretion of ammonia, H+, K+, and certain drugs.
Urine Movement
Urine moves through ureters to the bladder via peristalsis, with frequency influenced by sympathetic and parasympathetic nervous systems.
Prevention of Backflow:
Achieved by the trigone area of the bladder.
Composition of Urine
Urine is composed of:
1-2L produced daily, varying water content based on body needs.
Waste products include urea, uric acid, creatinine, and ions (H+, K+).
Micturition Reflex
Flow from Bladder to Urethra:
Controlled by stretching of bladder walls, signaling the CNS for voluntary control over the external urethral sphincter (EUS).
Full bladder capacity is around 1L.
Urination occurs when contraction of bladder muscles overcomes sphincter control.