t2
TERMS TO KNOW
Bradykinesias=low movement
Cerebrovascular accident=stroke; interruption in blood supply to the brain
Dysarthria=difficulty forming words associated with poor muscular control due to damage to the central or peripheral nervous system
Dysphasia=difficulty expressing or comprehending verbal or written language due to brain lesion or injury
Hemiparesis=weakness on one side of the body
Hemiplegia=paralysis on one side of the body
Hemianopsia=decreased vision or blindness in half of one eye or the same half of both eyes
Parkinson’s disease=progressive degeneration of neurons in the basal ganglia resulting in the reduced production of dopamine
Transient ischemic attack (TIA)=temporary or intermittent neurological event that can result from any situation that reduces cerebral circulation
Emotional homeostasis=balance of emotions
Pseudodementia=false appearance of dementia that occurs when persons demonstrate cognitive deficits secondary to being depressed
Substance abuse=inappropriate or excessive use of alcohol, caffeine, cannabis, hallucinogens, inhalants, opioids, sedatives, hypnotics, anxiolytics, stimulants, tobacco, and other or unknown substances that result in disorders
Delirium=acute confusion, usually reversible
Dementia=irreversible, progressive impairment in cognitive function
Mild cognitive impairment=transitional stage between normal cognitive aging and dementia in which the person has short-term memory impairment and challenges with complex cognitive functions
Sundowner syndrome=nocturnal confusion
Arrhythmia=abnormal heart rate or rhythm
Atherosclerosis=hardening and narrowing of arteries due to plaque buildup in vessel walls
Homans’ sign=pain when the affected leg is dorsiflexed, usually associated with deep phlebitis of the leg
Hypertension=consistent blood pressure reading of ≥130 systolic and/or ≥90 diastolic
Physical deconditioning=decline in cardiovascular function due to physical inactivity
Postural (orthostatic) hypotension=decline in systolic blood pressure of 20 mm Hg or more after rising and standing for 1 minute
Agnostic=a person who claims not to know with certainty whether or not God exists
Atheist=a person who believes God does not exist
Faith=belief in God, a higher power, or system of religious beliefs
Lack of spiritual well-being=a disruption to the beliefs or practices related to one’s faith or relationship with God or other higher power, causing spiritual needs to be unfulfilled
Religion=human-created structures, rituals, symbolism, and rules for relating to God/higher power
Spirituality=relationship and feelings with that which transcends the physical world
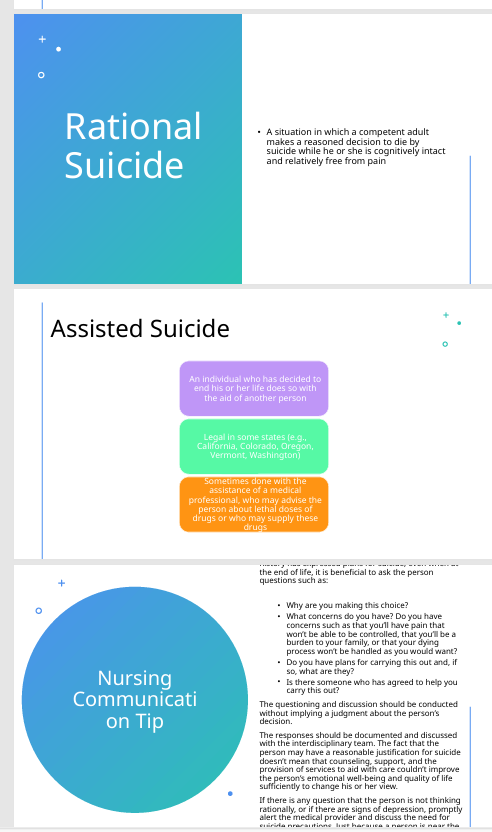
Assisted suicidesuicide committed with the help of another individual
Do not resuscitate (DNR)=medical order advising providers not to initiate cardiopulmonary resuscitation in the event of cardiac or respiratory arrest
End of life=period when recovery from illness is not expected, death is anticipated, and focus is on comfort
Hospice care=program that delivers palliative care to dying individual and support to dying person and that person’s family and caregivers
Palliative care=care that relieves suffering and provides comfort when cure is not possible
Rational suicide=decision by competent terminally ill person to end his or her life
Consent=granting of permission to have an action taken or procedure performed
Durable power of attorney=allows competent individuals to appoint someone to make decisions on their behalf in the event that they become incompetent
Duty=a relationship between individuals in which one is responsible or has been contracted to provide service for another
HIPAA=Health Insurance Portability and Accountability Act of 1996, assures confidentiality of health information and consumers’ access to their health records
Injury=physical or mental harm to another or violation of a person’s rights resulting from a negligent act
Malpractice=deviation from standard of care
Negligence=failure to conform to the standard of care
Private law=governs relationships between individuals and/or organizations
Public law=governs relationships between private parties and the government
Standard of care=the norm for what a reasonable individual in a similar circumstance would do
Autonomy=to respect individual freedoms, preferences, and rights
Beneficence=to do good for patients
Confidentiality=to respect the privacy
Ethics=a system of moral principles that guides behaviors
Fidelity=to respect our words and duty to patients
Justice=to be fair, treat people equally
Nonmaleficence=to prevent harm to patients
Veracity=truthfulness
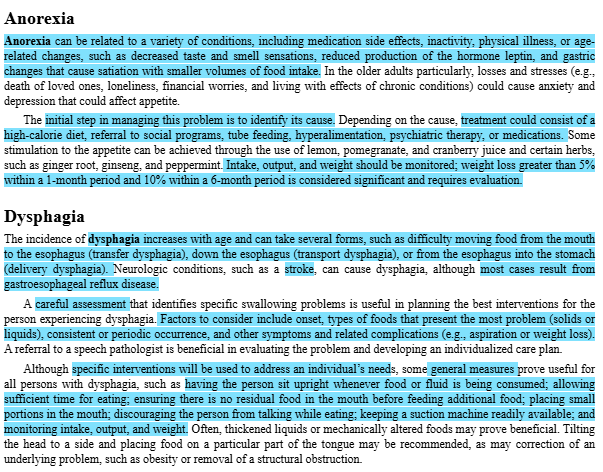
Anorexia=lack of appetite
Cholelithiasis=the formation or presence of gallstones in the gallbladder
Diverticulitis=inflammation or infection of the pouches of intestinal mucosa
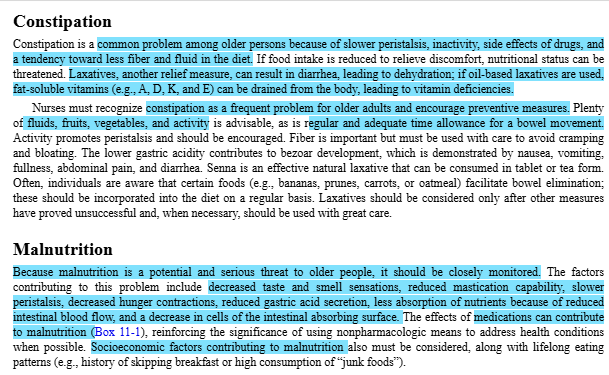
Dysphagia=difficulty swallowing
Esophageal dysphagia=difficulty with the transfer of food down the esophagus
Fecal incontinence=involuntary passage of stool
Flatus=gas in intestinal tract
Gingivitis=inflammation of the gums surrounding the teeth
Hiatal hernia=portion of the stomach protrudes through an opening in the diaphragm
Oropharyngeal dysphagia=difficulty transferring food bolus or liquid from the mouth into the pharynx and esophagus
Periodontal disease=inflammation of the gums extending to the underlying tissues, roots of teeth, and bone
Presbyesophagus=age-related changes to the esophagus causing reduced strength of esophageal contractions and slower transport of food down the esophagus
Established incontinence=involuntary loss of urine that can have an abrupt or sudden onset and is chronic
Functional incontinence=loss of voluntary control of urine due to disabilities that prevent independent toileting, sedation, inaccessible bathroom, medications that impair cognition, or any other factor interfering with the ability to reach a bathroom
Glomerulonephritis=condition in which there is inflammation of the glomeruli, which filter blood as it passes through the kidneys
Mixed incontinence=involuntary loss of urine due to a combination of factors
Neurogenic (reflex) incontinence=loss of control of voiding due to inability to sense the urge to void or control urine flow
Nocturia=voiding at least once during the night
Overflow incontinence=involuntary loss of urine due to an excessive accumulation of urine in the bladder
Stress incontinence=involuntary loss of urine when pressure is placed on the pelvic floor (e.g., from laughing, sneezing, or coughing)
Transient incontinence=involuntary loss of urine that is acute in onset and usually reversible
Urgency incontinence=involuntary loss of urine due to irritation or spasms of the bladder wall that cause a sudden elimination of urine
Urinary incontinence=involuntary loss of urine
Anorexia=loss of appetite
Dysphagia=difficulty swallowing due to difficulty moving food from the mouth to the esophagus (transfer dysphagia), down the esophagus (transport dysphagia), or from the esophagus into the stomach (delivery dysphagia)
Insomniainability to fall sleep, difficulty staying asleep, or premature waking
Nocturnal myoclonus=condition characterized by at least five leg jerks or movements per hour during sleep
Phase advance=falling asleep earlier in the evening and awakening earlier in the morning
Restless legs syndrome=neurological disorder characterized by an uncontrollable urge to move the legs when one lies down
Sleep apnea=disorder in which at least five episodes of cessation of breathing, lasting at least 10 seconds, occur per hour of sleep, accompanied by daytime sleepiness
Sleep latency=delay in the onset of sleep
Chapter 11
List age-related factors that affect dietary requirements in late life.
decreased caloric need and decreased metabolic rate among other factors listed in Table 11.1 on p148 in book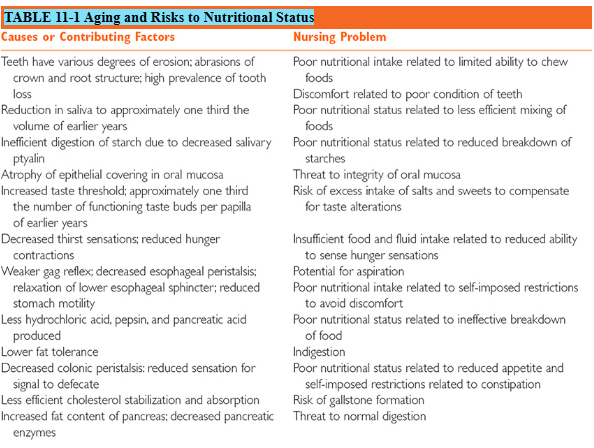
Discuss risks to nutritional status in older adults.
ALSO IN TABLE 11.1Identify risks associated with the use of nutritional supplements.
TABLES 11.3 AND 11.4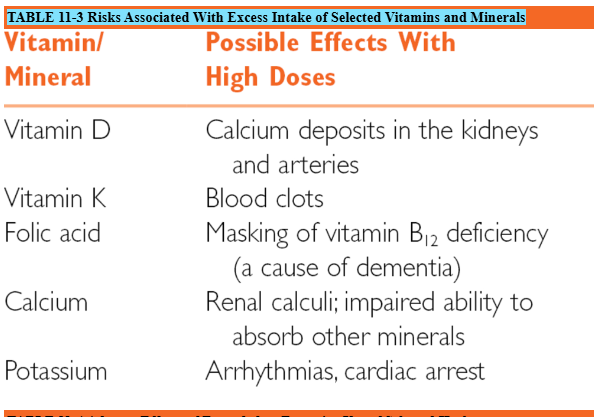
Describe the special nutritional needs of aging women.
decrease fat and alcohol intake, greater osteoporosis risk (TUMS= great way for quick calcium to help prevent)Describe age-related changes affecting hydration in older adults.
confusion, don’t want to use the restroom, fear, not “in the mood” etc…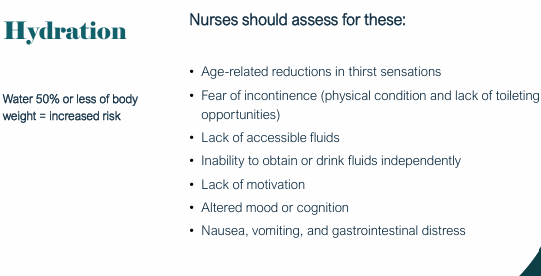
Discuss dehydration needs of older adults including: Overview, Causative or contributing factors, Goal, and Interventions
Describe oral health problems that could influence nutritional status
they need to be brushing, recognize periodontal disease, etc
Discuss recommended oral hygiene for older adults.
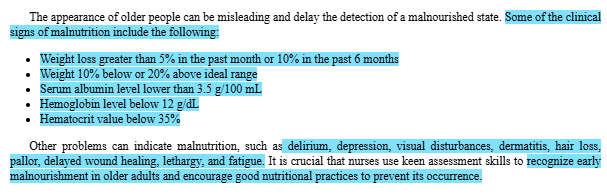
Discuss threats to good nutrition including: Indigestion and Food tolerance, Anorexia, Dysphagia, Constipation, and Malnutrition
REMEMBER TO USE FIBER AND STIMULANTS FOR CHRONIC CONSITPATION… OR AN OSMOTIC LAXITIVE
WATCH THE I&Os!
WEIGHT LOSS…WATCH FOR MORE THAN FIVE PERCENT IN ONE MONTH OR MORE THAN SIX PERCENT IN SIX MONTHSList the clinical signs of malnutrition
WEIGHT LOSS OF MORE THAN FIVE PERCENT IN ONE MONTH OR MORE THAN TEN PERCENT IN SIX MONTHS
WEIGHT DECREASED BY 10 OR 20 PERCENT RANGE
SERUM ALBUMIN LESS THAN 3.5 G/100ML (THINK PROTEIN DEFICIT)
HEMOGLOBIN COUNT BELLOW 12G/DL OR HEMATOCRIT VALUE BELOW 35 PERCENT (THINK IRON DEFICIT)Describe the basic components of the nutritional assessment.
from book:
ASSESSMENT GUIDE 11-1NUTRITIONAL STATUS
HISTORY
Review health history and medical record for evidence of diagnoses or conditions that can alter the purchase, preparation, ingestion, digestion, absorption, or excretion of foods.
Review medications for those that can affect appetite and nutritional state.
Review the type and amount of any nutritional supplements used.
Ask the patient to describe his or her diet, meal pattern, food preferences, and restrictions.
Ask the patient if there has been any change in appetite, digestion, food consumption, or ability to chew or swallow.
Request that the patient keep a diary of all food intake for a week.
PHYSICAL EXAMINATION
Inspect hair. Hair loss or brittleness can be associated with malnutrition.
Inspect skin. Note persistent “goose bumps” (vitamin B6 deficiency), pallor (anemia), purpura (vitamin C deficiency), brownish pigmentation (niacin deficiency), red scaly areas in folds around the eyes and between the nose and corner of the mouth (riboflavin deficiency), dermatitis (zinc deficiency), and fungal infections (hyperglycemia).
Test skin turgor. Skin turgor, although poor in many older adults, tends to be best in the areas over the forehead and sternum; therefore, these are preferred areas to test.
Note muscle tone, strength, and movement. Muscle weakness can be associated with vitamin and mineral deficiencies.
Inspect eyes. Ask about changes in vision and night vision problems (vitamin A deficiency). Note the patient’s percentile rank.
Inspect oral cavity. Note dryness (dehydration), lesions, condition of the tongue, breath odor, and condition of teeth or dentures.
Ask about signs and symptoms: sore tongue, indigestion, diarrhea, constipation, food distaste, weakness, muscle cramps, burning sensations, dizziness, drowsiness, bone pain, sore joints, recurrent boils, dyspnea, dysphagia, anorexia, and appetite changes.
Observe person drinking or eating for difficulties.
Biochemical Evaluation
Obtain blood sample for screening of total iron binding capacity, transferrin saturation, protein, albumin, hemoglobin, hematocrit, electrolytes, vitamins, and prothrombin time.
Obtain urine sample for screening of specific gravity.
Anthropometric Measurement
Measure and ask about changes in height and weight. Use age-adjusted weight chart for evaluating weight. Note weight losses of 5% within the past 1 month and 10% with the past 6 months.
Determine triceps skinfold measurement (TSM). To do so, grasp a fold of skin and subcutaneous fat halfway between the shoulder and elbow and measure with a caliper. Note the patient’s percentile rank.
Measure the midarm circumference (MC) with a tape measure (using centimeters) and use this to calculate midarm muscle circumference (MMC) with the formula:
The standard MMC is 25.3 cm for men and 23.2 cm for women. MMC below 90% of the standard is considered undernutrition; below 60% is considered protein–calorie malnutrition.
PSYCHOLOGICAL EXAMINATION
Test cognitive function.
Note alterations in mood, behavior, cognition, and level of consciousness. Be alert to signs of depression (can be associated with deficiencies of vitamin B6, magnesium, or niacin).
Ask about changes in mood or cognition.
Chapter 12
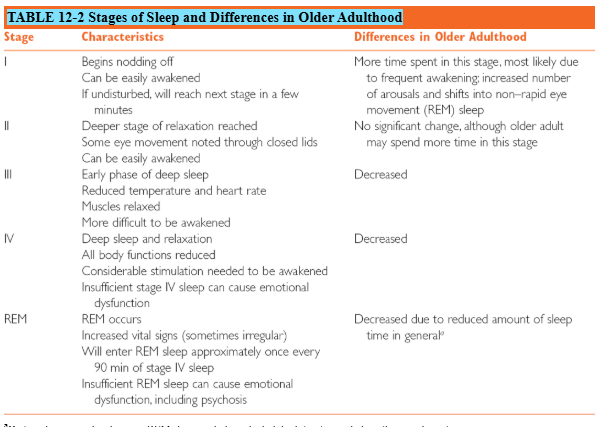
Identify the characteristics and differences in each stage of sleep in older adulthood.
MORE TIME IN STAGE ONE AND TWO WITH LESS TIME IN THREE AND FOUR/REM SLEEP WHICH ALSO LEADS TO MORE AWAKENING DURING SLEEP BECAUSE LESS DEEP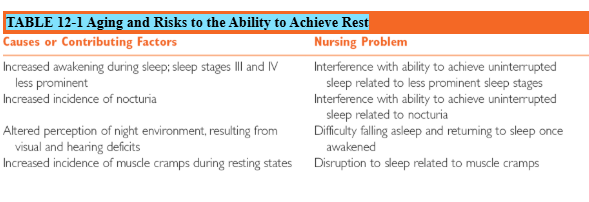
Circadian Sleep–Wake CyclesOlder adults are more likely to fall asleep earlier in the evening and awaken earlier in the morning, a behavior referred to as phase advance . The quantity of sleep does not change, but the hours in which it occurs may. This change can prove frustrating for older adults who find themselves nodding off during evening activities and wide awake in the early morning hours when everyone else is asleep. In addition, daytime naps may be needed to compensate for reductions in nighttime sleep. Adjusting schedules to accommodate the altered biorhythms could prove useful. Increasing natural light is also useful in pushing the circadian rhythm toward a later hour of sleep.
Describe the following sleep disturbances:
Insomnia
Nocturnal myoclonus
Phase advance: more likely to fall asleep earlier in the evening and awaken earlier in the morning, a behavior referred to as phase advance .
Restless legs syndrome
Sleep apnea
Sleep latency
3. Describe medical conditions that may affect sleep in older adults.
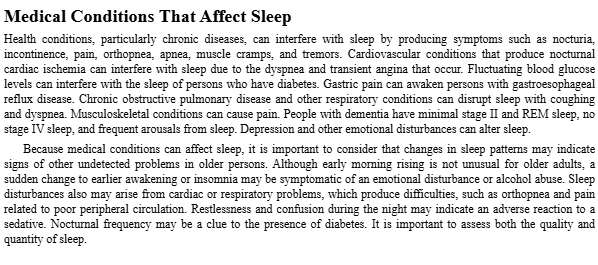
4. Identify drugs that affect sleep in older adults.
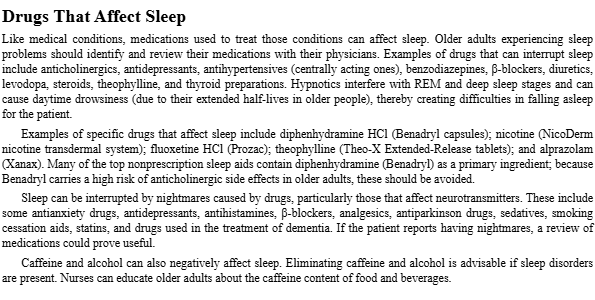
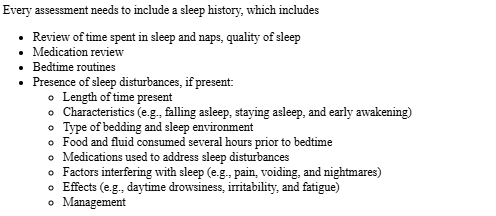
Discuss what is included in a sleep history.
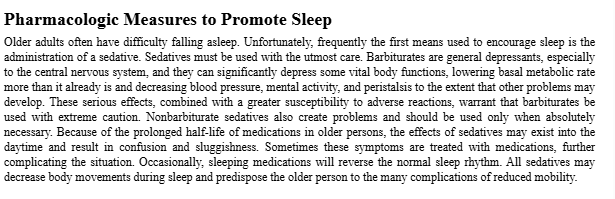
Describe pharmacological measures to promote sleep.
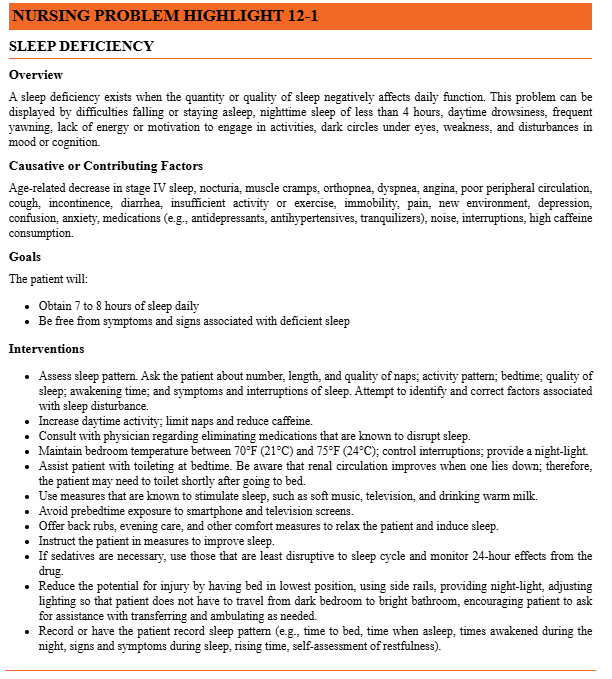
Discuss Sleep deficiency including:
Causative or contributing factors
Goals
Interventions
Identify non-pharmacological measures to promote sleep.
Activity and rest schedules
Environment
Food and supplements
Stress management
Discuss compensatory measures for stress control.
Chapter 8:
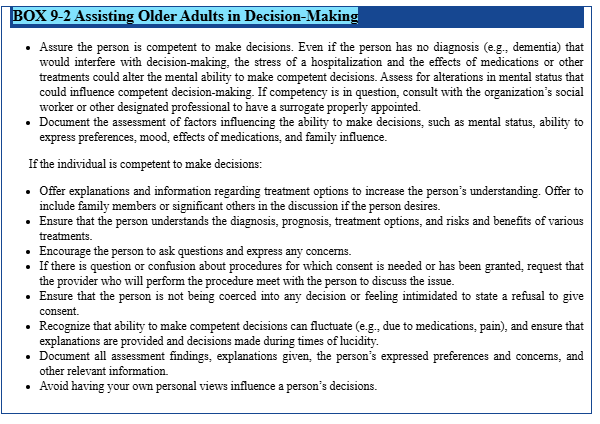
Define these terms: patient competency, guardianship, durable power of attorney, DNR, elder abuse, and neglectful injury
Describe the importance of patient competency and nursing actions when it is questionable.
LOOK FOR QUESTIONABLE SIGNS, MAKE SURE TO BE AN ADVOCATE, ASK ABOUT POA AND IF ITS DURABLE, WE DON’T DETERMINE, CONTACT THE FAMILY ESPECIALLY ABOUT POA OR GUARDIANSHIP, GO TO THE PROVIDER
Differentiate between guardianship and durable power of attorney.
Describe what do not resuscitate means.
NO NOT RECECITATE= DNR ORDER, MAKE SURE TO EDUCATE PATIENT ON AND ALLOW FOR THEIR OWN INFORMED DECESION, MUST BE FROM THE PROVIDER
List 3 reasons why an older adult may choose a DNR order.
RELIGOUS REASONS? HAVE SOMETHING THAT WOULD CAUSE MORE HARM TO THE PATIENT IF RECECITATED THAN IF NOT, ETCDescribe types of elder abuse and indications of possible abuse or neglect during routine interactions with older adult patients.
WE ARE MANDADATED REPORTERS, BE ON THE LOOKOUT FOR THE S/S OF ELDER ABUSE LISTED BELOW
Chapter 8: Legal and Ethical Considerations in Geriatric CareDefinitions
Patient Competency: The ability of a patient to make lawful decisions. This is assessed by providers; nurses advocate for autonomy when capacity is questionable.
Guardianship: A legal status where a court-appointed individual is authorized to make decisions for an incompetent older adult, typically involving legal proceedings.
Durable Power of Attorney (DPOA): A legal document designating someone (an agent) to act on another's behalf, which remains in effect even if the principal becomes incompetent.
Do Not Resuscitate (DNR): A medical order indicating that cardiopulmonary resuscitation (CPR) should not be attempted if the patient’s heart stops or they stop breathing.
Elder Abuse: A real and multifaceted issue that includes physical, emotional/psychological, sexual, and financial exploitation, neglect, abandonment, and self-neglect.
Neglectful Injury: This term implies harm resulting from neglect, a type of elder abuse characterized by failing to provide for an older adult's basic needs (e.g., food, hydration, hygiene, medical care), leading to physical or emotional harm or risk of harm.
Importance of Patient Competency and Nursing Actions When Questionable
Importance: Respect for patient freedoms, preferences, and rights (autonomy) is paramount. Competency ensures that decisions made reflect the patient's true wishes and values.
Nursing Actions When Questionable:
Nurses do not determine competency; providers assess capacity and document these assessments.
Advocate for patient autonomy.
Involve providers and legal teams; seek evaluations.
Involve family and potentially initiate guardianship or Power of Attorney (POA) processes.
Ensure informed consent processes are followed, especially when decision-making capacity is unclear.
Differentiating Between Guardianship and Durable Power of Attorney
Guardianship:
Court-appointed process.
Typically used when the person cannot make lawful decisions.
Involves legal proceedings and a public record.
Durable Power of Attorney (DPOA):
A legal document (usually drafted by an attorney) designating an agent to act on another’s behalf.
Remains in effect when the principal becomes incompetent.
An administrative/legal document outside of court unless contested.
Preferred for ongoing representation of older adults who lose decision-making capacity.
Meaning of Do Not Resuscitate (DNR) Order
A DNR order is a medical instruction specifying that CPR (cardiopulmonary resuscitation) should not be performed if a patient's heart stops beating or they stop breathing.
It is a specific medical order, not a cessation of all care.
Requires provider involvement and patient or patient representative consent.
Documentation and identification (e.g., labeled charts, wristbands, room signs) are crucial.
In home settings, a DNR or living will should be easily accessible for EMS.
Reasons for Choosing a DNR Order
Older adults may choose a DNR order to:Maintain quality of life: Prioritize comfort and dignity in end-of-life care over aggressive medical interventions.
Avoid unwanted invasive procedures: Prevent interventions like chest compressions, intubation, or defibrillation that may be painful, prolong suffering, or cause further decline without a meaningful benefit.
Respect personal autonomy and values: Exercise their right to self-determination regarding medical treatment decisions, aligning medical care with their personal beliefs about life and death.
Types of Elder Abuse and Indications of Possible Abuse or Neglect
Types of Elder Abuse:
Physical abuse: Intentional use of physical force that results in bodily injury, pain, or impairment.
Emotional/psychological abuse: Infliction of anguish, pain, or distress through verbal or nonverbal acts (e.g., intimidating, humiliating, threatening).
Sexual abuse: Nonconsensual sexual contact of any kind with an older adult.
Exploitation: Illegal or improper use of an older adult's funds, property, or assets.
Neglect: Failure to provide for the older adult's basic needs (e.g., food, water, medicine, clothing, shelter, personal safety, hygiene).
Abandonment: Desertion of an older adult by a person who has assumed responsibility for their care.
Self-neglect: An older adult's behaviors that threaten their own health or safety, often due to physical or mental impairment.
Indications of Possible Abuse or Neglect During Routine Interactions:
Delay in seeking medical care for serious conditions.
Malnutrition and dehydration without an apparent medical cause.
Unexplained bruising, poor hygiene, or inadequate grooming.
Inappropriate administration of medications (e.g., over-sedation).
Recurrent UTIs or other infections without clear medical cause.
Strong urine odor, bed sores, or other physical signs of neglect (e.g., soiled clothing/bedding).
Social isolation or loneliness, which can be a form of neglect or self-neglect if it leads to harm.
Unexplained financial strain or sudden changes in financial status.
Caregiver stress or reluctance to leave the older adult alone with others.
Chapter 9:
Evaluate an ethical dilemma (p. 127) using measures to help nurses make ethical decisions.
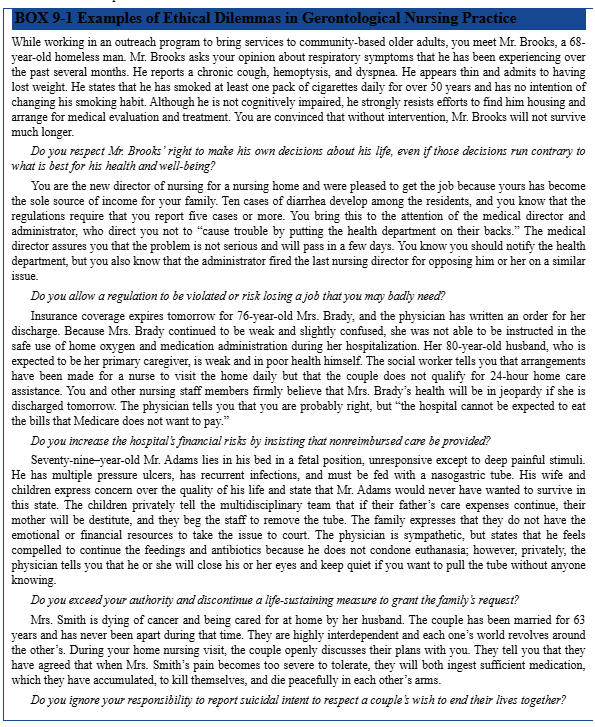
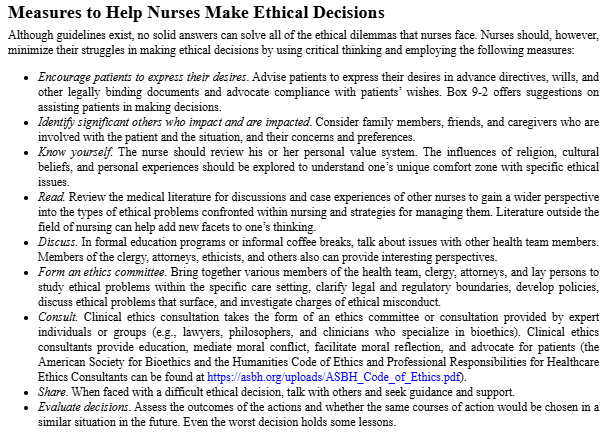
Chapter 9: Ethical Decision-MakingEvaluating an Ethical Dilemma Using Measures to Help Nurses Make Ethical Decisions (Case Scenario Example) When evaluating an ethical dilemma, such as the case of Mr. J (referred to by the full note), nurses should employ a structured decision-making process:
Nurse's Role: Be impartial, provide comprehensive information, support patient autonomy, and assess for financial and social implications related to the decision.
Considerations:
Financial Impact: How will the decision affect the patient's and spouse's financial well-being?
Patient and Spouse Values: Understand and respect the core values and preferences of both the patient and their significant other.
Potential Conflicts: Identify any disagreements or conflicts of interest among patient, family, and healthcare team.
Need for Additional Information: Gather all relevant medical evidence, explore alternative options, and consult with other professionals (e.g., social work, ethics committee).
Possible Actions:
Facilitate open and honest discussion among all parties involved.
Obtain more information or clarification from healthcare providers and other resources.
Refer to appropriate counseling (e.g., financial, ethical, spiritual).
Involve family members in a constructive manner, ensuring their understanding.
Protect the rights of both the patient and the spouse, ensuring informed consent and shared decision-making.
Document all discussions, assessments, interventions, and decisions thoroughly.
Important Attitude: Maintain self-awareness and emotional regulation. Recognize personal biases and values to ensure professional conduct and impartial care delivery.
Chapter 18:
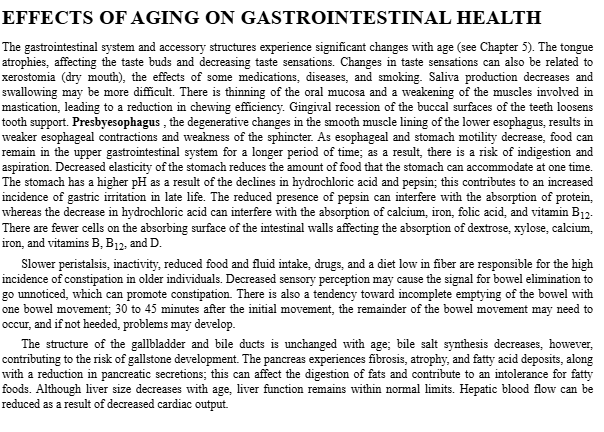
Analyze aging-related changes and their effects on gastrointestinal health by creating a summary table.
Educate a simulated patient about GI health promotion, highlighting what you consider to be the top 3 must-dos to maintain proper GI function.
FLUID, FIBER, AND ACTIVITY!!! REMMEBER TO CHEW! KEEP UP WITH PROPER ORAL CARE!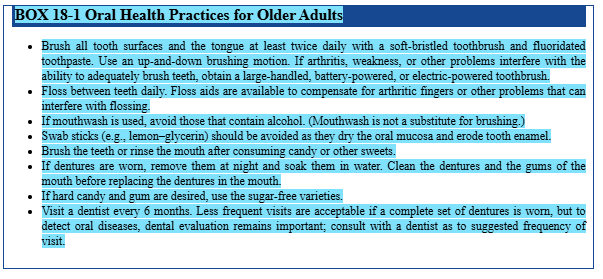
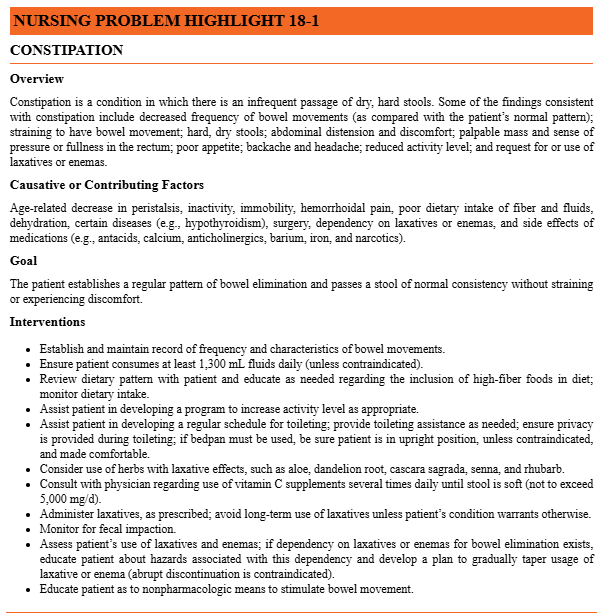
Discuss causative and contributing factors that can lead to chronic constipation in older adults.
Explain the nursing management, including interventions, for an older adult with chronic constipation.
Chapter 18: Gastrointestinal Health in Older Adults
Aging-Related Changes and Their Effects on Gastrointestinal Health: Summary Table
GI System Component | Age-Related Change | Effects on GI Health |
|---|---|---|
Oral Cavity/Pharynx | Tissue atrophy, decreased saliva production, decreased taste/smell, decreased chewing efficiency | Difficulty chewing and swallowing (dysphagia), altered nutrition, reduced appetite, increased risk of aspiration. |
Esophagus | Decreased motility, decreased lower esophageal sphincter (LES) pressure | Increased risk of gastroesophageal reflux (GERD) and heartburn. |
Stomach | Gastric mucosal atrophy, decreased blood flow, changes in acid production | Impaired digestion and absorption of nutrients (e.g., B12, iron), increased risk of gastritis. |
Small Intestine | Decreased digestive enzyme secretions, decreased motility, slower transit time | Reduced nutrient absorption, increased risk of small bowel bacterial overgrowth. |
Large Intestine | Decreased motility, changes in nerve supply and muscle tone, longer transit time, decreased sensation to defecate | Increased risk of constipation, fecal impaction, and diverticular disease. |
Liver | Shrinks in size, reduced regenerative capacity, decreased protein synthesis | Altered drug metabolism (pharmacokinetics), reduced capacity to recover from injury. |
General GI Function | Dehydration, decreased physical activity | Worsened GI function and motility, increased constipation. |
GI Health Promotion: Top 3 Must-Dos
For a simulated patient, the top 3 must-dos to maintain proper GI function are:Consume adequate fiber: A high-fiber diet (fruits, vegetables, whole grains) is crucial for maintaining regular bowel movements and promoting gut health.
Ensure adequate fluid intake: Hydration is essential to keep stool soft and prevent constipation. Recommend drinking water throughout the day.
Engage in regular physical activity: Movement increases GI motility, helping to prevent constipation and promote overall digestive health.
Causative and Contributing Factors to Chronic Constipation in Older Adults
Chronic constipation in older adults is a common problem with multiple contributing factors:Decreased GI Motility: Age-related slowing of the large intestine and colon transit time.
Dehydration: Insufficient fluid intake leads to harder, drier stools.
Polypharmacy: Many medications commonly used by older adults (e.g., opioids, anticholinergics, iron supplements, calcium channel blockers, diuretics) can cause constipation as a side effect.
Dietary Factors: Low fiber intake and poor nutritional choices.
Inactivity/Immobility: Lack of physical activity reduces bowel stimulation.
Dental Issues: Poor dentition or ill-fitting dentures can make chewing difficult, leading to a reduced intake of fiber-rich foods.
Underlying Medical Conditions: Conditions like hypothyroidism, diabetes, neurological disorders (e.g., Parkinson's), and strictures can contribute.
Ignoring the Urge to Defecate: Suppressing the urge due to pain, inconvenience, or lack of privacy can lead to stool hardening.
Nursing Management and Interventions for Chronic Constipation
Nursing management for older adults with chronic constipation includes:Assessment: Regularly assess bowel movements. Inquire about stool frequency, consistency, and any straining. Screen for signs of fecal impaction (hard stool with leakage of liquid stool around it).
Non-Pharmacologic Interventions (First-Line):
Increase Fiber: Educate on high-fiber foods; consider fiber supplements if dietary intake is insufficient.
Increase Fluids: Encourage adequate hydration throughout the day.
Increase Physical Activity: Promote mobility and exercise suitable for the patient's capabilities.
Regular Toilet Scheduling: Establish a consistent time for toileting, ideally after meals, leveraging the gastrocolic reflex.
Positioning: Ensure proper positioning for defecation to facilitate bowel emptying.
Pharmacologic Interventions (Cautious Use):
Use laxatives and stool softeners judiciously; educate on appropriate use to avoid dependence.
Consider bulk-forming agents, osmotic laxatives, or stimulants as prescribed.
Avoid soap suds enemas in older adults; consider other types (e.g., saline, mineral oil).
Review polypharmacy to identify and potentially deprescribe constipation-inducing medications in collaboration with the healthcare team.
Probiotics/Prebiotics: Discuss the potential role of these in maintaining gut flora.
Patient Education: Provide non-judgmental education on bowel health, prevention strategies, and when to seek medical attention.
Safety: Emphasize safe practices around rectal stimulation if necessary, highlighting the risks of unsafe techniques.
Collaboration: Coordinate with dietitians, pharmacists, and physicians to optimize management plans.
Chapter 19:
Analyze aging-related changes and their effects on urinary elimination by creating a summary table.
URINARY FREQUENCY… RESULT OF NORMAL PROCESSES OF AGING
Educate a simulated patient about urinary system health promotion, highlighting what you consider to be the top 3 must-dos to maintain proper GI function.
Define these terms: Urinary incontinence, transient incontinence, established incontinence, stress incontinence, urgency incontinence, overflow incontinence, neurogenic incontinence, functional incontinence, and mixed incontinence.
Explain the nursing management, including assessment, goals, and nursing actions, for an older adult with urinary incontinence.
Chapter 19: Urinary System and Incontinence in Older AdultsAging-Related Changes and Their Effects on Urinary Elimination: Summary Table
Urinary System Component
Age-Related Change
Effects on Urinary Elimination
Bladder
Decreased bladder capacity
Increased frequency of urination, particularly nocturia.
Bladder Control
Increased involuntary contractions (bladder spasms)
Higher urge to urinate, leading to urgency.
Women (Estrogen Decline)
Thinning of urethral mucosa, altered pelvic floor muscle tone
Contributes to urinary urgency, frequency, and stress incontinence.
Men (Prostate)
Prostate enlargement (BPH)
Obstruction of urine flow, leading to urgency, frequency, weak stream, incomplete emptying.
Kidneys
Reduced size, fewer nephrons, decreased mass, decreased GFR
Decreased renal clearance, affecting drug handling and increasing sensitivity to nephrotoxic agents.
Nocturnal Urine Production
Increases
More common nocturia (waking to urinate at night).
Urinary System Health Promotion: Top 3 Must-Dos
For a simulated patient, the top 3 must-dos to maintain proper urinary function are:Maintain adequate hydration: Drink sufficient fluids throughout the day to keep urine dilute and flush the urinary system, but avoid excessive intake close to bedtime to minimize nocturia.
Practice regular toileting and bladder training: Establish a routine for voiding, and for those with urge symptoms, gradually increase the time between voids to help retrain the bladder.
Perform pelvic floor muscle exercises (Kegels): These exercises strengthen the muscles that support the bladder and urethra, which is particularly beneficial for stress incontinence and overall bladder control.
Definitions of Urinary Incontinence Types
Urinary incontinence is not an expected age-related change; it is a disease/disorder that requires investigation and treatment.Urinary Incontinence (UI): Involuntary leakage of urine.
Transient Incontinence: Acute, temporary, and reversible episodes of incontinence, often caused by temporary factors such as infection, medications, or delirium. (Not explicitly defined in the provided notes but inferred as temporary).
Established Incontinence: Chronic or persistent incontinence, often linked to underlying genitourinary or neurological conditions. (Not explicitly defined in the provided notes but inferred as chronic).
Urge Incontinence: Involuntary urine loss accompanied by a sudden, strong desire to void (urgency); often linked to an overactive bladder.
Stress Incontinence: Involuntary urine leakage with physical exertion, such as coughing, laughing, sneezing, or lifting.
Overflow Incontinence: Leakage of urine from an overly full bladder, often due to urethral obstruction or weakened bladder muscles, resulting in constant dribbling.
Neurogenic (Reflex) Incontinence: Involuntary urine loss due to central nervous system or peripheral nerve damage, leading to an inability to sense urgency or control flow.
Functional Incontinence: Incontinence caused by functional barriers to reaching the toilet (e.g., mobility limits, cognitive impairment, environmental barriers), rather than a primary urinary tract problem.
Mixed Incontinence: A combination of two or more types of incontinence, most commonly urge and stress incontinence.
Nursing Management for an Older Adult with Urinary Incontinence
Nursing management follows the nursing process, including assessment, goal setting, and interventions:Assessment:
Gather a thorough history: prostate status (men), prior radiation, estrogen therapy or replacement (women), pelvic floor integrity, and current medications (especially anticholinergics).
Perform a Post-Void Residual (PVR) measurement using a bladder scanner (PVR > 100\,mL often indicates overflow incontinence).
Conduct a urinalysis to check for infection, blood, or other abnormalities.
Evaluate for functional barriers: assess mobility, bathroom accessibility, caregiver support, and cognitive status.
Goals:
Reduce incontinence episodes.
Improve bladder control and capacity.
Enhance quality of life and dignity.
Prevent complications such as skin breakdown and UTIs.
Nursing Actions (Interventions):
Distinguish Incontinence Types: Tailor interventions based on the specific type(s) of incontinence (urge, overflow, functional, mixed).
Pelvic Floor Muscle Training (PFMT): Teach Kegel exercises and refer to physical therapy for stress incontinence.
Lifestyle Modifications:
Fluid management: Ensure adequate hydration but manage timing (e.g., reduce intake before bed).
Caffeine and alcohol reduction: These can irritate the bladder.
Weight management: Reduces pressure on the bladder and pelvic floor.
Constipation management: Address constipation as it can worsen urinary symptoms.
Bladder Training and Scheduled Voiding: For neurogenic or functional incontinence, implement scheduled toileting and prompt prompts for cognitively impaired individuals. Gradually increase voiding intervals for urge incontinence.
Pharmacologic Considerations: Educate patients about prescribed medications and monitor for side effects; collaborate with the healthcare team to optimize regimens and consider deprescribing anticholinergics when possible.
Environmental and Caregiving Strategies: Remove barriers to bathroom access, ensure assistive devices are within reach, provide appropriate toileting equipment.
Avoid Routine Catheterization: Minimize catheter-associated infections; educate about when catheterization is necessary.
Patient Education: Provide information on incontinence causes, management strategies, and prevention.
Interdisciplinary Collaboration: Work with physical therapists, dietitians, and social workers to provide comprehensive care.
Chapter 30
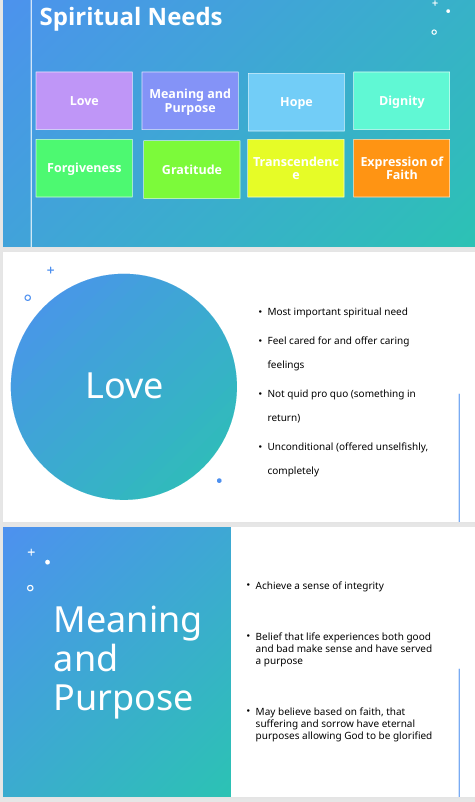
1. Differentiate between spirituality and religion in the context of holistic nursing care.
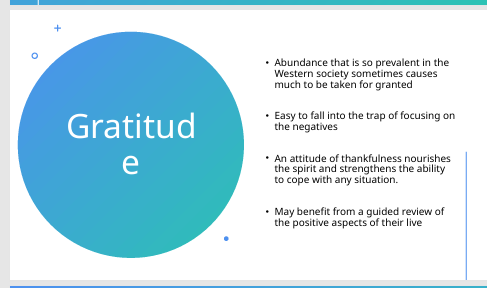
2. Discuss common spiritual needs of older adults, including love, purpose, hope, dignity, forgiveness, gratitude, transcendence, and faith.

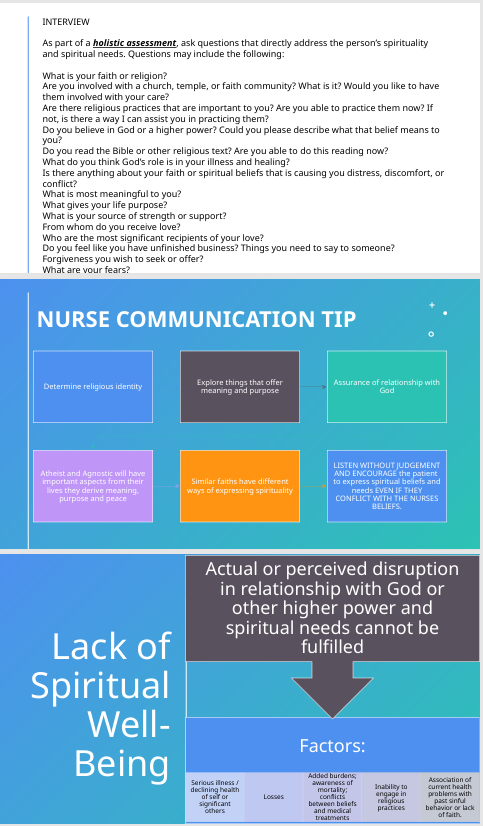
3. Conduct a basic spiritual assessment by exploring patients’ faith beliefs, practices, and community affiliations.
4. Demonstrate respect for and support of patients’ spiritual beliefs by providing opportunities for expression, promoting hope, and assisting in finding meaning in challenging circumstances.
Chapter 36
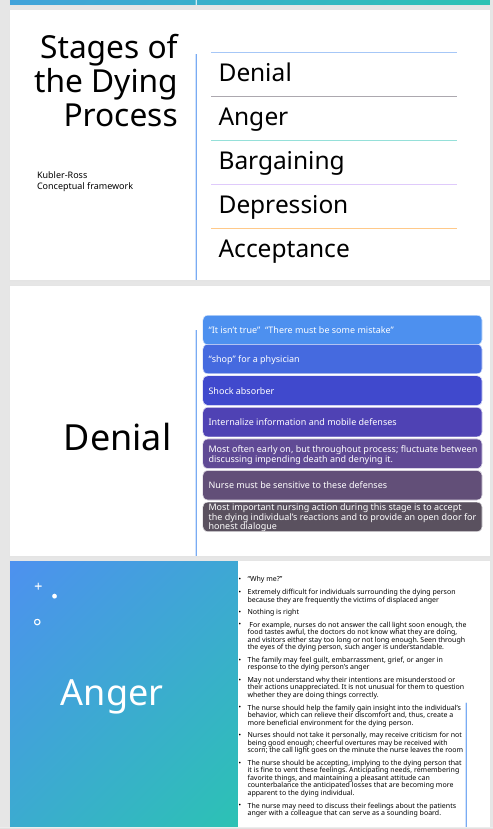
5. Explain the role of the gerontological nurse in providing holistic support—physical, emotional, and spiritual—during the dying process.
6. Describe the stages of the dying process.
7. Apply the Kübler-Ross framework to identify appropriate nursing interventions for patients at different stages of the dying process.
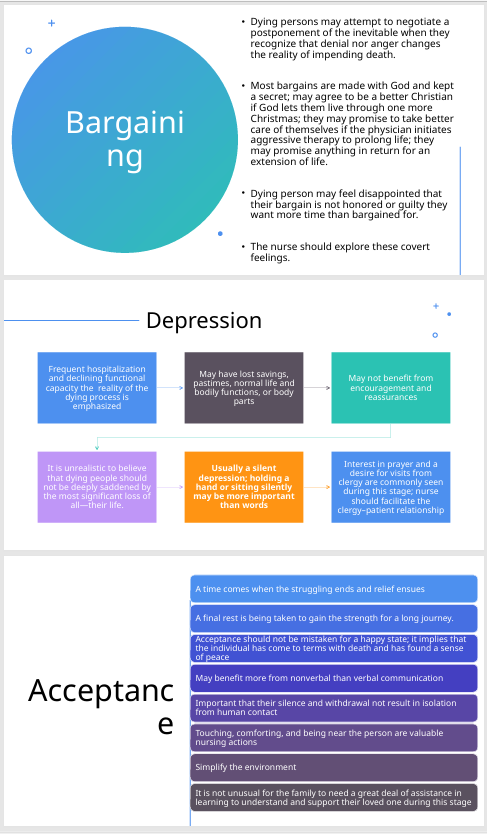
8. Discuss ethical considerations related to rational suicide and assisted suicide, including the importance of assessment, counseling, and supportive care.
9. Identify common physical signs and symptoms that occur as death approaches including pain, respiratory distress, constipation, poor nutritional intake.
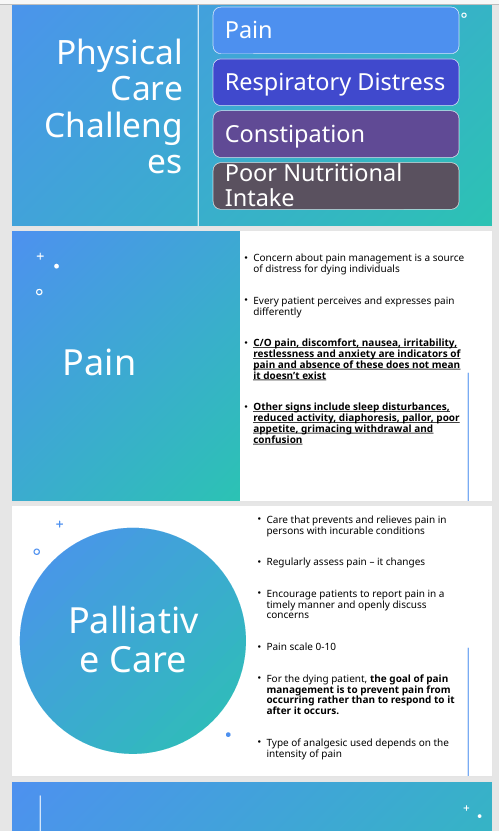
10. Identify appropriate nursing interventions for comfort and dignity.
11. Discuss strategies to support family, friends, and healthcare staff experiencing grief associated with the dying process.
Chapter 17
12. Describe common age-related changes in the cardiovascular system of older adults.
13. Recognize the increased risk of cardiovascular disease in women.
14. Explain lifestyle practices that promote cardiovascular health in later life.
15. Discuss the following cardiovascular conditions including cues (signs and symptoms), risk factors, management for:
1. Hypertension (HTN)
2. Hypotension
3. Congestive heart failure (CHF)
4. Pulmonary emboli (PE)
5. Coronary Artery Disease (CAD)
6. Angina
7. Myocardial infarction
8. Hyperlipidemia
9. Arrhythmias
10. Atrial Fibrillation
11. Peripheral Vascular Disease
12. Arteriosclerosis
13. Diabetic problems
14. Aneurysms
15. Varicose Veins
16. Venous thromboembolism
16. Identify risk factors for pulmonary emboli in older adults.
17. Explain how atypical presentations can delay diagnosis.
18. Recognize that most adults over 70 have some degree of coronary artery disease.
19. Discuss atrial fibrillation as the most common sustained arrhythmia in older adults.
20. Identify the major contributing factor to ischemic stroke.
21. Differentiate between atherosclerosis and arteriosclerosis in older adults.
22. Discuss ways to promote circulation.
23. Discuss foot care for persons with peripheral vascular disease.
24. Describe complications of vascular changes, including varicosities, falls, ulcerations, and infections.
25. Apply nursing interventions to promote cardiovascular health in older adults.
Chapter 30: Spirituality in Holistic Nursing Care
Differentiate between spirituality and religion in the context of holistic nursing care.
Spirituality: The relationship and feelings that connect humans to the divine, transcending the physical world.
Religion: A human-constructed system describing structures, rituals, and rules for relating to God or a higher power.
Nursing focus: Supporting spirituality and meaning, not converting beliefs.
Discuss common spiritual needs of older adults, including love, purpose, hope, dignity, forgiveness, gratitude, transcendence, and faith.
Meaning and purpose: Supported by Erik Erikson’s theory, achieving integrity in late life is aided by a spiritual need for meaning and purpose; helps individuals believe in the future and stay committed to their beliefs even when facing pain or adversity.
Hope: A spiritual need that helps people believe in the future and remain committed to those who suffer.
Most important spiritual need: Unconditional [need], suggesting unconditional acceptance or love.
Conduct a basic spiritual assessment by exploring patients’ faith beliefs, practices, and community affiliations.
Spiritual assessment: Distinguishing between assessing spirituality and interventions to support spiritual practices.
Visible cues of spirituality: Physical or symbolic signs (e.g., rosary or Bible present) that indicate spiritual practice or needs.
Demonstrate respect for and support of patients’ spiritual beliefs by providing opportunities for expression, promoting hope, and assisting in finding meaning in challenging circumstances.
Core nurse goal in spiritual care: Not conversion, but helping the patient discuss spiritual issues and maintain practices.
Interventions: Respect rituals, provide scripture, arrange clergy support, facilitate discussions on spiritual issues, and accommodate patient practices.
Providing uninterrupted time for prayer/reflection/meditation: An aspect of honoring solitude.
Supporting spirituality can enhance health and healing.
Chapter 36: End-of-Life Care
Explain the role of the gerontological nurse in providing holistic support—physical, emotional, and spiritual—during the dying process.
Nurse’s broad goals: Ensure comfort, support meaning and dignity, and respect patient and family wishes.
Physical support: Nonpharmacologic end-of-life pain or comfort measures (e.g., massage, acupuncture).
Spiritual support: Meeting spiritual needs can support health and healing even near end of life; provide uninterrupted time for prayer/reflection/meditation.
Emotional support: Supporting open expression of grief, providing follow-up support groups, and advocating for consumer protection in funeral decisions (e.g., avoiding coercive or costly funeral expenses).
Describe the stages of the dying process.
No specific stages of dying are described in the provided notes.
Apply the Kübler-Ross framework to identify appropriate nursing interventions for patients at different stages of the dying process.
The Kübler-Ross framework is not discussed in terms of application or interventions in the provided notes.
Discuss ethical considerations related to rational suicide and assisted suicide, including the importance of assessment, counseling, and supportive care.
Not covered in the provided notes.
Identify common physical signs and symptoms that occur as death approaches including pain, respiratory distress, constipation, poor nutritional intake.
The notes only mention "pain or comfort measures" in end-of-life care, without explicitly listing common physical signs of approaching death.
Identify appropriate nursing interventions for comfort and dignity.
Interventions: Provide nonpharmacologic pain or comfort measures (e.g., massage, acupuncture).
Patient-centered care: Provide uninterrupted time for prayer/reflection/meditation, avoid pressuring patients, and support their rituals.
Care planning should include honoring viewing preferences, open expression of grief, follow-up support groups, and consumer protection in funeral decisions.
Discuss strategies to support family, friends, and healthcare staff experiencing grief associated with the dying process.
Strategies: Provide follow-up support groups and resources for bereavement.
Chapter 17: Cardiovascular System in Older Adults
Describe common age-related changes in the cardiovascular system of older adults.
Valves become thicker and more rigid.
Aorta may dilate.
Myocardial muscle becomes less efficient.
Diastolic filling and systolic filling are slower; overall reduced pump efficiency.
Recognize the increased risk of cardiovascular disease in women.
No specific information provided in the notes on increased risk for women.
Explain lifestyle practices that promote cardiovascular health in later life.
Diet: Low fat, high fiber; fruits/vegetables; complex carbohydrates; omega-{3} fatty acids (fish 2x/week); reduce red meat and highly processed foods; limit alcohol. Emphasize DASH diet (fruits, vegetables, whole grains, low sodium). Prefer olive oil (omega-{6}), avoid trans fats; ensure adequate hydration and fiber.
Exercise: 30 minutes moderate activity most days or 20 minutes vigorous activity 3 days/week; promote stair climbing and parking farther away. Essential warm-up and cool-down for cardiac patients; avoid abrupt high-intensity starts.
Smoking cessation: Implement stress management techniques (yoga, meditation); consider acupuncture to assist quitting smoking.
Discuss the following cardiovascular conditions including cues (signs and symptoms), risk factors, management for:
Hypertension (HTN)
Thresholds: Hypertension defined as systolic > 130 mmHg or diastolic > 80 mmHg. Hypertensive crisis occurs at SBP \ge 180 mmHg or DBP \ge 120 mmHg.
Symptoms: Morning headaches (in the back of the head), nosebleeds, dizziness or confusion with extremes of BP.
Management: Blood pressure readings should be repeated at multiple times and in different positions (lying, sitting, standing); use the arm with the higher reading for subsequent measurements.
Hypotension
Causes: Anaphylactic shock, hypovolemia, hypoglycemia, hyperglycemia, orthostatic hypotension.
Orthostatic Hypotension: A drop in blood pressure when standing, significant if \ge 20 mmHg systolic or \ge 10 mmHg diastolic drop.
Congestive heart failure (CHF)
Mentioned as a condition contributing to altered tissue perfusion. (No detailed cues or management provided in the notes).
Pulmonary Embolism (PE)
Risk factors: Prolonged immobilization.
Symptoms: Sudden shortness of breath, a sense of impending doom, low-grade fever.
Management: Includes heparin, warfarin, thrombolysis with alteplase in some cases, and sometimes surgical clot retrieval. Long-term anticoagulation (e.g., clopidogrel with aspirin) is common.
Coronary Artery Disease (CAD)
Description: Same as ischemic heart disease; risk increases with aging.
Cues: Angina is chest pain due to myocardial oxygen supply-demand mismatch.
Triggers: Classic triggers include exertion and cold exposure (e.g., shoveling snow).
Angina
Description: Same as chest pain.
Atypical presentations: Possible reflux-like symptoms or digestion-related pain.
Management: Nitroglycerin use (vasodilates); up to 3 doses every 5 minutes for 15 minutes. Seek further care if relief occurs but symptoms recur or persist.
Myocardial Infarction (MI)
Management: Post-MI rehabilitation emphasizes warm-up and cool-down during exercise to prevent injury; gradual progression of activity.
Hyperlipidemia
Assessment: Involves measurement of LDL, HDL, and triglycerides; requires fasting for 12 hours before lipid testing.
Targets: HDL goal is > 60 mg/dL; triglycerides are measured after fasting.
Management: First-line pharmacotherapy is statins.
Arrhythmias
General arrhythmias are not detailed, but Atrial Fibrillation is specifically discussed.
Atrial Fibrillation (AFib)
Description: The most common chronic cardiac arrhythmia; often asymptomatic, detected via EKG or irregular pulse. Types include paroxysmal, persistent, and permanent.
Major risk: Stroke due to blood pooling and clot formation in the atria.
Management: May include rate control, cardioversion, or ablation.
Peripheral Vascular Disease (PVD) / Peripheral Artery Disease (PAD)
Description: PVD includes slow progression of circulation problems, commonly affecting the lower extremities. PAD specifics include claudication, numbness, and weakness.
Cues: Claudication (pain with walking due to insufficient leg perfusion), hair loss on legs, stasis ulcers on lower extremities, medial lower leg ulcers.
Interventions: Stop smoking, exercise, monitor lower-extremity pulses, and proper foot care.
Complication: Diabetes complicates healing and increases the risk of amputation.
Arteriosclerosis
Atherosclerotic heart disease is mentioned as contributing to altered tissue perfusion. (No direct differentiation or detailed discussion of arteriosclerosis itself).
Diabetic problems
Contributes to altered tissue perfusion. Complicates healing and increases the risk of amputation in PAD.
Aneurysms
Abdominal aortic aneurysm (AAA): Pulsations in the abdomen may indicate an aneurysm; risk if dissection occurs.
Management: Early detection allows repair; otherwise, there is a high mortality risk.
Varicose Veins
Description: Dilated, tortuous veins in the legs.
Venous Thromboembolism (VTE)
Description: Includes Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE).
Risk factors: Increased with prolonged immobilization.
Prevention: Leg elevation, compression stockings, and early ambulation when possible.
Identify risk factors for pulmonary emboli in older adults.
Risk factor: Prolonged immobilization.
Explain how atypical presentations can delay diagnosis.
Atypical presentations of angina/chest pain (e.g., reflux-like symptoms, digestion-related pain) are possible and can delay diagnosis.
Recognize that most adults over 70 have some degree of coronary artery disease.
Coronary Artery Disease (CAD) risk increases with aging. (The specific statistic "most adults over 70" is implied rather than explicitly stated).
Discuss atrial fibrillation as the most common sustained arrhythmia in older adults.
Atrial fibrillation (AFib) is the most common chronic cardiac arrhythmia.
Identify the major contributing factor to ischemic stroke.
Atrial fibrillation (AFib): A major risk for stroke due to blood pooling and clot formation in the atria.
Differentiate between atherosclerosis and arteriosclerosis in older adults.
Atherosclerotic heart disease is mentioned as contributing to altered tissue perfusion, but a specific differentiation between atherosclerosis and arteriosclerosis is not provided.
Discuss ways to promote circulation.
Interventions for PVD: Stop smoking, exercise, and monitor lower-extremity pulses.
Prevention of VTE: Leg elevation, compression stockings, and early ambulation.
General cardiovascular health recommendations: Diet, exercise, smoking cessation, and stress management.
Discuss foot care for persons with peripheral vascular disease.
Proper foot care is a key intervention for Peripheral Artery Disease (PAD).
Describe complications of vascular changes, including varicosities, falls, ulcerations, and infections.
Complications: Varicose veins (dilated, tortuous veins), stasis ulcers on lower extremities (due to poor perfusion), medial lower leg ulcers (in PAD), and edema from venous pooling.
Diabetes complicates healing and increases the risk of amputation.
Orthostatic hypotension, a condition related to vascular changes, can increase the risk of falls.
Apply nursing interventions to promote cardiovascular health in older adults.
Prevention framework: Primary (prevent disease in healthy individuals), Secondary (support those diagnosed to avoid complications), and Tertiary (maximize function and rehabilitation to prevent disability).
Clinical assessment: Employ a head-to-toe assessment approach, looking for redness, edema, pallor, and nail bed changes. Inquire about changes in function, physical or mental status, dizziness, exercise tolerance, alcohol or drug use, and vitamins/supplements.
Blood pressure and cardiovascular checks: Performed in multiple positions and arms; using the arm with the higher reading for subsequent measurements.
Documentation practices: Emphasize the importance of asking clarifying questions during patient interviews.
Spirituality and Erikson: integrity and meaning
Erik Erikson’s theory (referenced as Ericsson in some notes): achieving integrity in late life is supported by a spiritual need for meaning and purpose
Key concept: meaning and purpose helps individuals believe in the future and stay committed to their beliefs even when facing pain or adversity
Question-and-answer example:
Question: According to Erikson, achieving integrity in late life is supported by this spiritual need.
Answer: Meaning and purpose
Point value: 100
Related concept: hope as a spiritual need helps people believe in the future and remain committed to those who suffer
Question: The spiritual need that helps people believe in the future and commit to those who suffer is what?
Answer: Hope
Point value: 300
Spiritual concepts and terms observed in the session
Spirituality: The relationship and feelings that connect humans to the divine transcending the physical world
Question: The relationship and feelings that connect humans to the divine transcending the physical world. What is spirituality?
Answer: Spirituality
Spiritual distress vs. crisis: Disruption in beliefs or practices relating to faith leaving spiritual needs unfulfilled (category: Definitions and concepts)
Visible cues of spirituality: Physical or symbolic signs (e.g., rosary or Bible present) that indicate spiritual practice or needs
Question: A patient wearing a rosary or keeping a Bible nearby is providing this type of clue.
Answer: A visible cue (of spirituality)
Spiritual assessment vs. addressing spiritual needs: Distinguishing between assessing spirituality and interventions to support spiritual practices
Core nurse goal in spiritual care: Not conversion, but helping the patient discuss spiritual issues and maintain practices
Time for prayer/reflection/meditation as a practice: Providing uninterrupted time for these activities is an aspect of honoring solitude
Most important spiritual need: Unconditional [need]; context suggests unconditional acceptance or love
Meaning and purpose as a core construct: Finding meaning and purpose is central to addressing spiritual needs
Other items mentioned: care planning should include honoring viewing preferences, open expression of grief, follow-up support groups, and consumer protection in funeral decisions (example given: advocate to avoid coercive or costly funeral expenses)
World religions and related concepts (examples from the session)
Kosher: Orthodox Jewish dietary law that prohibits mixing meat and dairy
Sabbath observance: Seventh-day Adventists observe Saturday as Sabbath
Prayer direction in Islam: Prayer must be performed facing the holy city Mecca (Mecca is the intended answer in the session, noted as Magna in the prompt)
Meditation and enlightenment: Buddhism practice includes meditation and following the Eightfold Path (eightfold path referenced as “eight path eightfold path”)
Religion as a human-constructed system: A term describing structures, rituals, and rules for relating to God or a higher power
Nursing interventions to address spiritual needs (evidence-based framing in the session)
Examples of interventions: Respect rituals, provide scripture, arrange clergy support
Evidence-based premise cited: Supporting spirituality can enhance health and healing
Nursing role emphasis: Facilitate discussions on spiritual issues and accommodate patient practices
Key educational point for practice: The nurse’s goal is not conversion but to support the patient’s spiritual needs and practices
In Islam, prayer direction; in Judaism, kosher; in Adventism, Sabbath; general care includes spiritual assessment and ongoing support
End-of-life care and care planning themes (highlights from the session)
Nonpharmacologic end-of-life pain or comfort measures: Two examples discussed (e.g., massage, acupuncture) as part of a broader list
Evidence-based nursing focus: Meeting spiritual needs can support health and healing even near end of life
Patient-centered care: Provide uninterrupted time for prayer/reflection/meditation; avoid pressuring patients; support their rituals
The nurse’s broad goals: Ensure comfort, support meaning and dignity, and respect patient and family wishes
Cardiovascular aging and disease: key concepts and clinical signs
Aging effects on the cardiovascular system:
Valves become thicker and more rigid
Aorta may dilate
Myocardial muscle becomes less efficient
Diastolic filling and systolic filling slower; overall reduced pump efficiency
Conditions contributing to altered tissue perfusion:
Atherosclerotic heart disease, hypertension, congestive heart failure (CHF)
Varicose veins, diabetes, cancer, renal failure
Blood dyscrasias: anemia, thrombosis, transfusion needs
Causes of hypotension that compromise perfusion:
Anaphylactic shock, hypovolemia, hypoglycemia, hyperglycemia, orthostatic hypotension
Orthostatic hypotension: drop in blood pressure when standing; significant if exceeds certain thresholds
Tachycardia as a compensatory response to poor perfusion
Peripheral symptoms of poor perfusion:
Claudication (pain with walking due to insufficient leg perfusion)
Edema from venous pooling
Hair loss on legs; hair on toes/feet may indicate perfusion level
Stasis ulcers on lower extremities
Respiratory signs of poor perfusion: dyspnea, rapid respirations
Capillary refill and cool/cold extremities as perfusion checks
Restlessness as a sign of hypoxia/poor perfusion
General cardiovascular health recommendations:
Diet: low fat, high fiber; fruits/vegetables; complex carbohydrates; omega-3 fatty acids (fish 2x/week); reduce red meat and highly processed foods; limit alcohol
Exercise: 30 minutes moderate activity most days or 20 minutes vigorous activity 3 days/week; promote stair climbing and parking far away
Smoking cessation; stress management (yoga, meditation); consider acupuncture to assist quitting
Nutrition tips: prefer olive oil (omega-6), avoid trans fats; ensure adequate hydration and fiber
CRP as an inflammatory marker: elevated CRP indicates higher risk of cardiovascular issues; confounding conditions exist (e.g., RA, lupus)
Lipids and cholesterol management:
LDL, HDL, triglycerides; fasting for 12 hours before lipid testing
Target: HDL > 60; triglycerides measured after fasting
First-line pharmacotherapy: statins
Blood pressure basics:
Normal ranges and hypertension thresholds discussed; readings should be repeated at multiple times and in different positions
Positions for BP measurement: lying, sitting, standing; reading differences > 20 mmHg systolic or > 10 mmHg diastolic may indicate positional hypotension
Two-arm checks and using the arm with the higher reading for subsequent measurements
Heart sound and pulse examination:
Five heart valve areas to listen to: aortic, pulmonic, Erb’s point, tricuspid, mitral
Apical impulse location: fifth intercostal space at the midclavicular line; count apical pulse for a full minute
Documentation of pulses: 0 = absent, 1 = thready, 2 = normal, 3 = strong, 4 = bounding
Pulses to assess bilaterally for symmetry; brachial pulse location: medial to the biceps region
Hypertension specifics observed in the session:
Normal BP definitions used in the session: “greater than 130 systolic and greater than 80 diastolic” signifying hypertension per the material
Stage classifications (informal ones referenced): crisis when SBP ≥ 180 or DBP ≥ 120; other stages noted via rising SBP/DBP
Common symptoms of hypertension: morning headaches in the back of the head; nosebleeds; dizziness or confusion with extremes of BP
Myocardial infarction and ischemic heart disease:
Angina and chest pain are the same concept; atypical presentations possible (reflux-like symptoms, digestion-related pain)
Nitroglycerin use: vasodilates; up to 3 doses every 5 minutes for 15 minutes; seek further care if relief occurs but symptoms recur or persist
Post-MI rehab emphasis: warm-up and cool-down during exercise to prevent injury; gradual progression of activity
Atrial fibrillation (AFib):
Most common chronic cardiac arrhythmia; often asymptomatic, detected via EKG or irregular pulse
Types: paroxysmal, persistent, permanent
Major risk: stroke due to blood pooling and clot formation in the atria; management may include rate control, cardioversion, or ablation
Peripheral vascular disease (PVD) / Peripheral artery disease (PAD):
PVD includes slow progression of circulation problems; commonly affects lower extremities
PAD specifics: claudication, numbness, weakness; medial lower leg ulcers
Interventions: stop smoking, exercise, monitor lower-extremity pulses, proper foot care; diabetes complicates healing and risk of amputation
Abdominal aortic aneurysm (AAA):
Pulsations in the abdomen may indicate aneurysm; risk if dissection occurs
Early detection allows repair; otherwise high mortality risk
Varicose veins and venous thromboembolism (VTE):
Varicose veins: dilated, tortuous veins in the legs
VTE includes DVT and PE; risk increased with prolonged immobilization; prevention includes leg elevation, compression stockings, and early ambulation when possible
Pulmonary embolism (PE) management observed in session:
Treatments include heparin, warfarin, thrombolysis with alteplase in some cases, sometimes surgical clot retrieval
Long-term anticoagulation (e.g., clopidogrel with aspirin) is common
PE symptoms can include sudden shortness of breath and a sense of impending doom; fever may be low-grade
Coronary artery disease / Ischemic heart disease:
CAD is the same as ischemic heart disease; risk with aging; angina is chest pain due to myocardial oxygen supply-demand mismatch
Classic trigger scenarios include exertion and cold exposure (e.g., shoveling snow)
Diet, lipids, and diet-related risk reduction details:
Emphasize DASH diet (fruits, vegetables, whole grains, low sodium)
Focus on omega-3 fatty acids from fish; limit saturated fats and trans fats; encourage complex carbohydrates and fiber
Exercise prescription and rehabilitation emphasis for cardiac patients:
Warm-up and cool-down are essential; avoid abrupt high-intensity starts
Overall prevention framework:
Levels of prevention: Primary (prevent disease in healthy individuals), Secondary (support those diagnosed to avoid complications), Tertiary (maximize function and rehabilitation to prevent disability)
General clinical assessment tips and exam practice:
Head-to-toe assessment approach; look for redness, edema, pallor, nail bed changes
History questions: changes in function, physical or mental status, dizziness, exercise tolerance, alcohol or drug use, vitamins/supplements
Blood pressure and cardiovascular checks should be performed in multiple positions and arms
Documentation practices and the importance of asking clarifying questions during patient interviews
Formulas, numbers, and key thresholds (as referenced in the transcript)
Blood pressure thresholds (as presented in the session):
Hypertension threshold mentioned: > 130 systolic or > 80 diastolic
Hypertensive crisis threshold (mentioned in context): SBP ≥ 180 or DBP ≥ 120
Orthostatic hypotension definition used: a drop in blood pressure of ≥ 20 mmHg systolic or ≥ 10 mmHg diastolic upon standing
Apical pulse assessment:
Location: fifth intercostal space at the midclavicular line
Duration: count for a full minute
Pulse grading (qualitative scale):
0: absent, 1: thready, 2: normal, 3: strong, 4: bounding
Lipids and cardiovascular markers (fasting values):
HDL goal: > 60 mg/dL
Triglycerides: measured after fasting (typically ~12 hours)
LDL targets and total cholesterol not explicitly quantified in the transcript, but statins are noted as first-line therapy for hyperlipidemia
Five valve areas for auscultation (names to memorize):
Aortic, Pulmonic, Erb’s point, Tricuspid, Mitral
ch22, 27, 28
After reading these chapters, you should be able to:
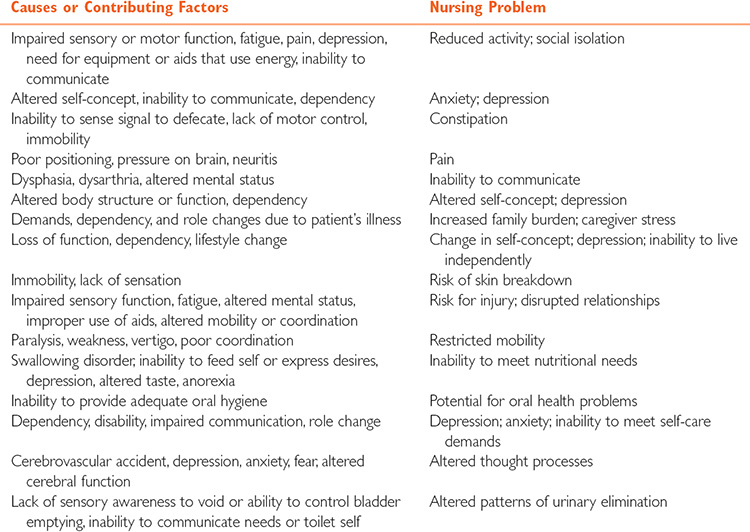
1. Describe effects of aging on nervous system.
FROM BOOK:
With age, loss of nerve cell mass causes some atrophy of the brain and spinal cord, and brain weight decreases. The number of nerve cells declines, each cell has fewer dendrites, and some demyelinization of the cells occurs. These changes slow nerve conduction. Response and reaction times are slower; reflexes become weaker.
Plaques, tangles, and atrophy occur in the brain to varying degrees; there is not always a relationship between these changes and cognitive function. Free radicals accumulate with age and may have a toxic effect on certain nerve cells. Cerebral blood flow decreases about 20% as fatty deposits gradually accumulate in the blood vessels, and decreases are even greater in persons with small-vessel cerebrovascular disease due to diabetes and hypertension; this contributes to an increased risk of strokes. The brain has a greater ability to compensate after injury than does the spinal cord, but this ability to compensate declines with age.
Intellectual performance tends to be maintained until at least age 80 in the absence of neurologic or vascular disease, although a slowing in central processing delays the time required to perform tasks. Verbal skills are well maintained until age 70, after which there is a gradual reduction in vocabulary, a tendency to make semantic errors, and abnormal prosody (rhythm and intonation). Other age-related changes in intellectual function are subtle but can be detected as difficulty learning, especially languages, and forgetfulness in noncritical areas.
The general lack of replacement of neurons affects the sensory organs’ function, which becomes less acute with age. The number and sensitivity of sensory receptors, dermatomes, and neurons decrease, resulting in dulling of tactile sensation. There is also some decline in the function of cranial nerves mediating taste and smell. Increased levels of taste, sound, scents, touch, and lighting are required for perception by older persons as compared with younger adults.
It must be remembered that these changes do not affect all individuals similarly. Genetic makeup, diet, lifestyle practices, and other factors influence the health and function of the neurologic system.

2. List risk factors for neurologic problems in older adults.
FROM PP:
FROM BOOK:
3. Describe measures to promote neurologic health, promote independence, and reduce risk of injury in older adults.
4. Identify signs and symptoms of neurologic disorders in older adults.
5. Describe symptoms, unique features and nursing care for patients with Parkinson’s disease, transient ischemic attacks, and cerebrovascular accidents in older adults.
FROM PP:
FROM BOOK:
6. List measures that promote mental health for older adults.
7. Describe symptoms and care for an older adult with depression.
FROM PP:

FROM BOOK:
8. Identify indications of suicidal thoughts in older adults.
FROM PP:
FROM BOOK:
9. Describe interventions to reduce anxiety in older adults.
FROM PP:
10. Discuss signs of substance abuse in older adults. Identify nursing actions to manage disruptive behavior associated with mental health conditions in older adults.
FROM PP:
11. Differentiate delirium from dementia.
FROM PP:
12. Identify factors that cause delirium.
FROM PP:
13. Describe characteristics, symptoms, and management of dementia.
FROM PP:
14. List causes of dementia.
15. Outline nursing considerations for older adults with dementia.
Normal aging: neurological function in older adults
Normal aging changes (not pathological): progression over time in the nervous system
Neuron loss: begins after about age 25; more nerve cells lost as age increases
Neurotransmitters: fewer neurotransmitters available in aging brain
Nerve conduction and reaction time: slower in older adults
Brain atrophy: brain size and neurons decrease with age; space increases on imaging
Plaques: plaques form in nerve cell bodies during aging
Cerebral blood flow: slows somewhat with age
Hippocampus changes: memory retrieval and storage rely on the hippocampus; aging leads to changes there
Activating system changes: sleep-cycle regulation alterations
Sensory decline: receptors decrease in number and sensitivity; cranial nerves show aging-related changes
Vision, hearing, taste, smell, vibratory sensation: often diminished
Temperature sensation: less able to sense temperature changes; environment safety considerations
Balance and postural control: increased risk for postural hypertension and falls; sensitivity to medications that lower blood pressure on standing up
Intellectual maintenance: intellect generally preserved; many argue wisdom and emotional intelligence may improve or stay strong into later years; verbal skills often preserved until around age 70, then vocabulary can decline
Overall nursing task: distinguish normal aging from pathological changes; monitor for differences in presentation and degree
Clinical manifestations linked to normal aging (summary):
Sleep changes: less REM sleep; longer time in stages 1–2; easier to wake; daytime sleepiness may increase
Learning: altered ability to learn new information quickly, though learning is still possible with effort
Memory: storage/retrieval affected via hippocampus; occasional difficulty recalling names or words is common and usually gradual
Vision/hearing changes: sensory deficits impact communication and safety
Taste/smell changes: can influence nutrition; adapt to maintain intake
Postural hypertension and balance issues: greater risk with antihypertensive or diuretic therapies; careful drug management needed
Temperature regulation: environmental safety importance
Cognitive function and intellect: intelligence maintained; some decline in processing speed, but not necessarily loss of intellect
Functional status: slower task performance; need for supports or assistive devices as needed
Red flags requiring further evaluation (nursing alarm signs):
New headaches, new vision changes
Sudden deafness or tinnitus
Rapid mood or personality changes
Altered consciousness or cognition
New clumsiness or unstable gait
Numbness or tingling in extremities or unusual nerve sensations
Parkinson's disease (PD)
Pathophysiology: decreased dopamine in basal ganglia; balance between acetylcholine and dopamine disrupted
Neurotransmitter role: acetylcholine is excitatory; dopamine enables smooth, controlled movement
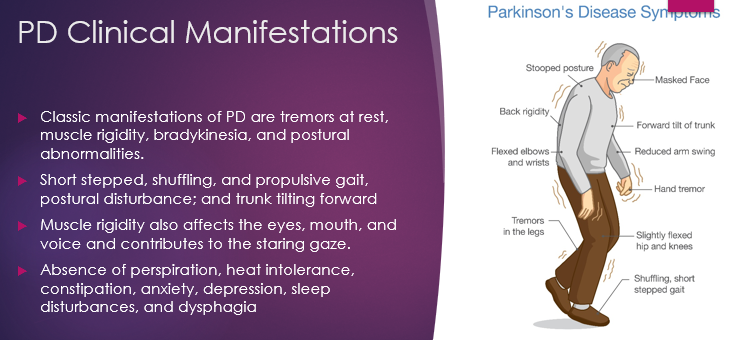
Classic motor symptoms: resting tremor (often initial), bradykinesia (slowness of initiation), impaired postural reflexes
Typical body presentation: stooped/forward-leaning posture, rigid back, shuffling gait, masked facial expression
Common risk factors: genetic (autosomal dominant defect on chromosome 4) and environmental factors; potential drug/toxin exposure; trauma history
Non-motor features: heat intolerance, constipation, depression; decreased perspiration; dysphagia risk with disease progression
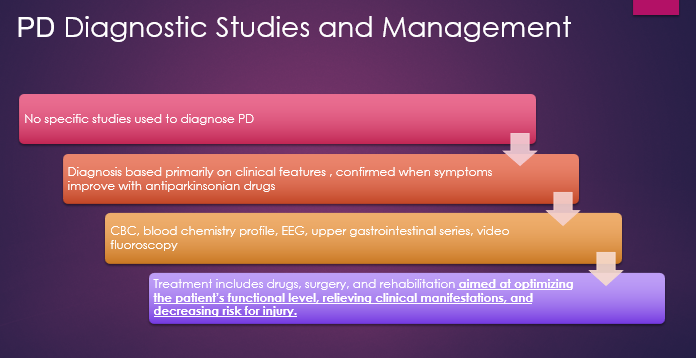
Diagnosis: clinical presentation; no definitive lab test; responds to dopaminergic therapy
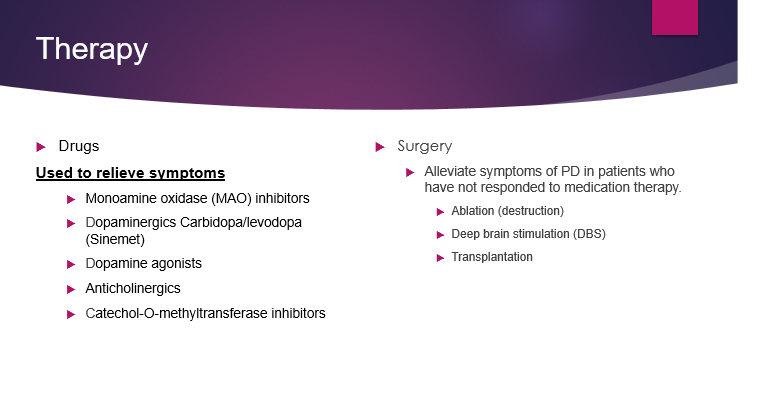
Treatments (not curative; symptom management):
Dopaminergic therapy: carbidopa-levodopa (Sinemet) — levodopa precursor to dopamine; carbidopa inhibits peripheral breakdown
Dopamine agonists and anticholinergics to mitigate symptoms and side effects
Catechol O-methyltransferase (COMT) inhibitors to prolong dopamine effect
Surgical options (for selected patients):
Ablation and deep brain stimulation (DBS) reduce aberrant neural activity
Transplantation and stem cell approaches under investigation
Nursing goals and interventions: maintain cognition and function, prevent injuries from impaired movement, minimize falls, safety-focused teaching
Nursing care plan elements:
Active range of motion exercises twice daily
Ambulation with assistive devices (walker/c cane) and PT consult when mobility declines
OT consult for activities of daily living and adaptive devices
Speech/swallow therapy for dysphagia and communication challenges
Nutritional assessment and support; monitor weight and dietary needs
Psychological support; address caregiver burden; community resources
Safety and management emphasis: prevent falls, plan for evolving needs, enable independent function where possible
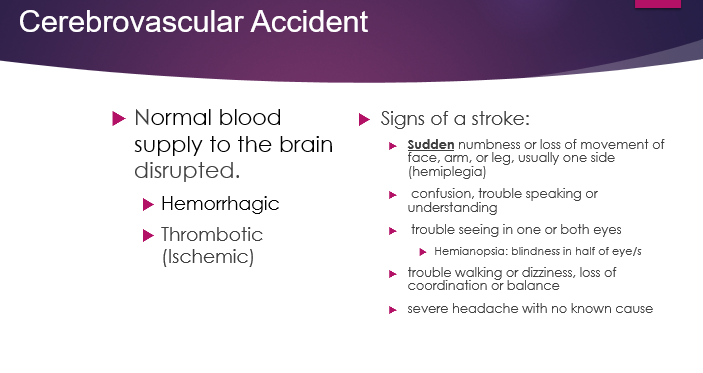
Cerebrovascular accident (CVA) / Stroke
Types: hemorrhagic stroke (bleed due to vessel rupture or malformation) vs ischemic/thrombotic stroke (clot obstructs blood flow)
Onset pattern: hemorrhagic strokes often have abrupt onset; ischemic strokes may have sudden onset or evolve over minutes to hours
Common presenting symptoms: sudden unilateral facial, arm, or leg numbness or weakness (usually on one side); confusion or trouble speaking; trouble seeing in one or both eyes (hemianopsia); trouble walking, dizziness, loss of coordination; severe headache may occur
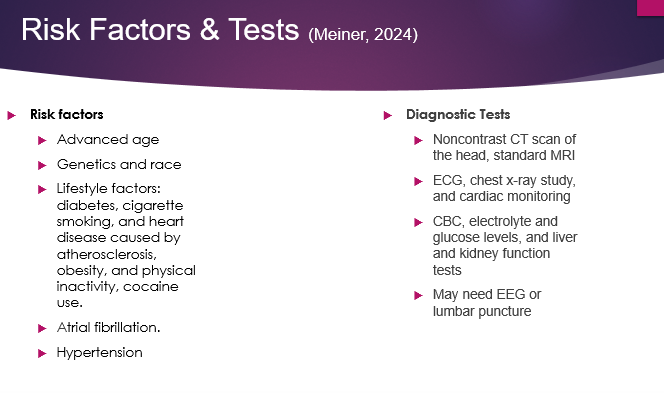
Risk factors: advanced age; genetics; African American ethnicity; diabetes; cigarette smoking; heart disease; obesity; physical inactivity; cocaine use; atrial fibrillation (AFib); hypertension (most important modifiable risk factor)
Acute management in hospital: emergency CT scan; continuous monitoring (cardiac and other vitals); labs; possibly EEG; airway protection; head of bed elevated to reduce intracranial pressure (ICP)
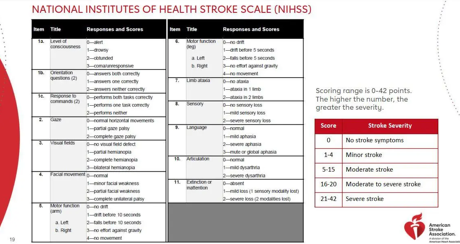
Neuro assessment and scales: NIH Stroke Scale or similar tools; assess level of consciousness, orientation, commands, gaze, visual fields, motor function, sensory, language, and cognition
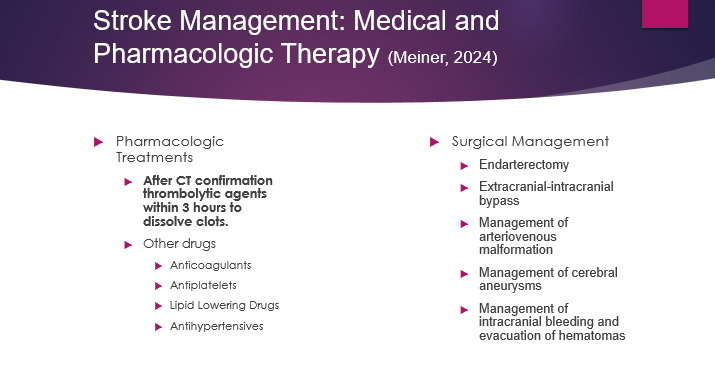
Reperfusion therapy: thrombolytic therapy within a 3-hour window (time is brain); earlier treatment yields better outcomes; later guidelines may vary by stroke type and facility
Medications and interventions:
Anticoagulants or antiplatelets depending on etiology (AFib, clotting risk, etc.)
Lipid-lowering agents and antihypertensives for long-term secondary prevention
Indirect vascular procedures (carotid endarterectomy or extracranial bypass) and brain surgery for certain conditions (aneurysms, malformations, intracranial bleeding)
Acute nursing interventions: keep head elevated, monitor vitals, turn and ROM every 2 hours, encourage use of unaffected arm for ADLs, ensure swallow safety and resumption of oral intake after swallow study
Speech and language concerns: aphasia types (receptive vs expressive); visual field deficits (hemianopia); adapt patient/family education to language abilities
Outcomes and family/community planning: stroke prevention education, access to resources, and long-term rehabilitation planning
Priority considerations: safety and prevention of secondary injury; test-tasks often emphasize safety as the highest priority in acute care
Mental health and substance use in older adults
Depression in older adults: prevalent; 20–25% of adults aged 55+ have a mental health disorder (depression is especially common)
Causes and contributing factors: chronic illnesses, aging-related losses (bereavement, relocation, retirement), changes in social roles and income, societal undervaluation of older adults; medications may contribute to depression
Screening and assessment: Geriatric Depression Scale (GDS-15); 15 yes/no questions; scores >5 suggest depression requiring further evaluation
Key signs: fatigue, constipation, psychomotor retardation, persistent depressed mood, anhedonia, low energy, social withdrawal, neglect of hygiene or self-care, somatic complaints; altered cognition common in depression and can mimic dementia
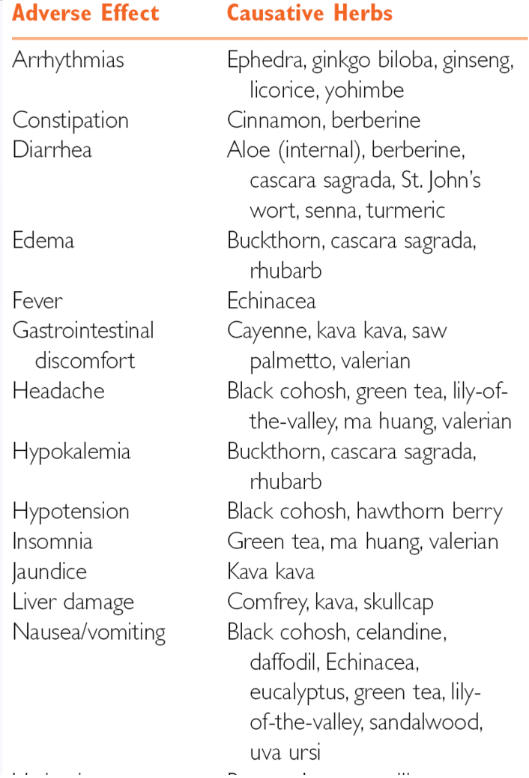
Treatment considerations: prefer SSRIs over tricyclic antidepressants (TCAs) due to anticholinergic side effects and safety concerns in older adults; avoid combining SSRIs with St. John’s wort; consider psychotherapy and nonpharmacologic approaches (acupuncture, guided imagery, light therapy, sleep, exercise, nutrition)
Start low, go slow: gradual dosing and small increases to minimize side effects and falls risk; expect SSRIs to take ~2 weeks or more to show effect
Suicide risk: high among older adults; ~29% of suicide deaths occur in older adults; highest risk in men aged 85+ and older white men; risk factors include bereavement, chronic illness, social isolation, and retirement
Suicide risk assessment and response: use structured tools (e.g., National Institute of Mental Health resources) to assess frequency of thoughts, plan, past attempts, symptoms, social support; determine disposition (emergency psychiatric evaluation, inpatient care, or nonurgent follow-up); safety planning and no-suicide contracts when appropriate
Alcohol use in older adults: SMAST-G screening; two or more positive responses suggests an alcohol problem; recommended limits typically not more than one standard drink per day for older adults; withdrawal management and potential interactions with medications required; benzodiazepines for alcohol withdrawal can be dangerous in older adults
Anxiety in caregivers and patients: coaching and coping strategies; relaxation and deep breathing; modify perceptions of stress; psychotherapy and nonpharmacological approaches preferred; meds should be a last resort in older adults due to safety concerns
Substance abuse in older adults: not rare; may involve prescription opioids and other substances; increased risk of falls, cognitive impairment, self-neglect; discuss strategies for safe medication use and monitoring; do not overlook prescription misuse and social factors that sustain abuse
Delirium vs dementia (two “d’s”) and nursing care
Delirium: acute, abrupt global cognitive impairment with fluctuating mental status; may be worse at night; disorganized thinking; inattention; altered alertness; can include agitation or hypoactivity; hallucinations common in hospital settings
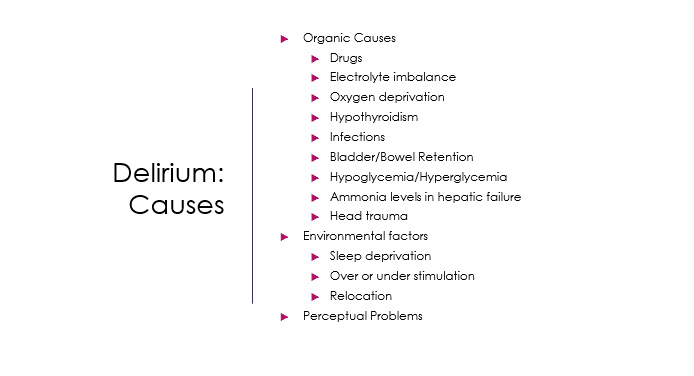
Causes of delirium: drugs, electrolyte and acid-base imbalances, oxygen delivery/deficiency (hypoxia), hypothyroidism, infections, bladder/bowel retention, hypoglycemia/hyperglycemia, sleep deprivation, sensory deprivation or overstimulation, environmental factors, ICU-related factors
Assessment and criteria: Hartford Institute criteria (common nursing tool) look for: acute change in mental status; agitation or lethargy; fluctuating or altered level of consciousness; memory impairment or disorganized thinking; inattentiveness; change in behavior; criteria usually require multiple signs; delirium is a medical emergency and must be addressed promptly
Management principles: identify and treat the underlying cause (medication changes, electrolytes, oxygenation, infection, catheter-related issues, hypothyroidism, etc.); minimize stimuli and provide orientation; reassurance and consistent care; limit restraints and sedating medications; use antipsychotics like haloperidol only as a last resort due to safety concerns in older adults
Dementia co-occurring with delirium: delirium often superimposed on dementia; do not assume delirium is simply a manifestation of baseline dementia; obtain history and observe for changes; educate families and involve them in care planning
Nursing practice points: environment optimization (calm, well-lit, predictable routines); involve family; provide 24-hour sitter if needed; prioritize safety and reorientation; document delirium status per unit protocol
Dementia and Alzheimer’s disease (AD)
Dementia overview: progressive, irreversible cognitive deterioration with personality changes and functional decline; DSM-5 defines major neurocognitive disorder as dementia; mild neurocognitive disorder (MCI) is cognitive decline not yet affecting ADLs/IADLs
Common etiologies: dementia is a syndrome with multiple diseases causing it; Alzheimer’s disease accounts for 60–80% of dementia cases; Lewy body dementia (5–10%); vascular dementia (5–10%); frontotemporal dementia (FTD) (5–10%); other diseases such as AIDS and Parkinson’s may contribute
Alzheimer’s disease pathology: beta-amyloid plaques and tau tangles damage neurons and disrupt neurotransmission; plaques are amyloid beta fragments; tau proteins stabilize neurons but become tangled in AD
Common dementia progression patterns: Alzheimer’s disease tends to show a gradual, steady decline; vascular dementia often shows a stepwise decline after each cerebrovascular event
Frontotemporal dementia (FTD): earlier onset (often <60); affects frontal lobes; early behavioral changes or language impairment; different from AD in initial symptomatology
Lewy body dementia (LBD): alpha-synuclein inclusions (Lewy bodies); parkinsonian symptoms along with cognitive fluctuations and early visual hallucinations; often overlaps with Parkinson’s disease symptoms
Other causes and mimics: depression, drugs, vitamin/mineral deficiencies, thyroid disorders, metabolic issues, infections, exposure to toxins; reversible conditions must be ruled out before confirming dementia
Risk factors for AD and dementia (modifiable and non-modifiable):
Non-modifiable: age, family history, ApoE4 allele (two copies confer higher risk; up to ~10x baseline risk) 10\times; early-onset dementia linked to strong family history/genetics
Modifiable risk factors (Lancet Commission 2020): reduced incidence of dementia by addressing multiple factors; key factors include 40\% risk reduction if addressed collectively: less education, hearing loss, hypertension, physical inactivity, diabetes, obesity, low social contact, depression, tobacco, head injury, and potentially excessive alcohol
Prevention and screening: primary care uses MMSE, MoCA, or Mini-Cog; screening alone is not diagnostic; family observations are crucial and should be weighed alongside screening tests; if abnormal, refer to neuropsychology, neurologist, or geriatrician for comprehensive evaluation; imaging (CT/MRI) and labs to evaluate reversible causes
Diagnosis advances: traditional lumbar puncture (cerebrospinal fluid beta-amyloid and tau) and PET scans; newer blood-based tests measuring amyloid/tau ratios show promise for Alzheimer’s-specific diagnosis; these tests may guide prognosis and treatment decisions in the future
Stages and assessment tools for dementia: use scales such as the Alzheimer’s Association staging (1–4), Global Deterioration Scale (one to seven), MMSE (higher is better), and Allen scale (higher score indicates better function in some scales); clinicians should know which scale is being used when interpreting results
Mild cognitive impairment (MCI): cognitive decline not severe enough to interfere with daily activities; can progress to dementia or remain stable
Treatments and emerging therapies for AD:
Symptom management: cholinesterase inhibitors (e.g., donepezil) and memantine to modulate glutamate activity; these do not cure AD but can slow symptoms in some individuals
Disease-modifying therapies (recent advances): monoclonal antibodies that target amyloid plaques, such as
Leqembi (lecanemab)
Donanemab
Other agents (e.g., aducanumab) discussed in the literature; these therapies can slow cognitive decline by approximately 25\%-30\% over 18\text{ months} but carry risks of amyloid-related imaging abnormalities (ARIA) and require regular MRIs and monitoring
Administration and monitoring: IV infusions every two weeks (then potential subcutaneous maintenance later); frequent MRI surveillance (e.g., every 4 weeks during active treatment) due to ARIA risk; cost and insurance coverage remain significant barriers in many settings
Nonpharmacologic approaches for dementia care: cognitive stimulation therapy, communication therapies, behavioral therapy to limit triggers, reality orientation, validation therapy, reminiscence therapy; safety planning; establishing regular routines; balancing independence with caregiver support; simple, stage-appropriate communication; meaningful activities to improve quality of life
Neuropsychiatric symptoms in dementia: common behaviors include resisting care, repetitive actions, delusions, sexual disinhibition, wandering, suspiciousness; management requires a person-centered approach and may include diverting attention, environmental adjustments, and boundary-setting; antipsychotics carry higher mortality and should be used cautiously as a last resort
Sexual disinhibition: common in dementia; set clear boundaries and maintain professional boundaries; acknowledge feelings but keep care focused on medical needs
Wandering and agitation: use distraction, safety measures, and engaging activities; explain to family and staff the importance of reducing triggers and enhancing routines
Communication strategies: keep messages simple; tailor to the person’s stage; involve family; use reminiscence and validation approaches to reduce distress
Caregiver support and ethics: emphasize a balance between independence and dependence, supporting caregivers to reduce burnout; involve community resources and patient safety planning; consider ethical issues around autonomy, consent, and quality of life
Diagnostic and assessment tools (summary)
Screening instruments in primary care: MMSE, MoCA, and Mini-Cog; high scores do not rule out MCI or early dementia; family observations are equally important
Neuropsychology referral: detailed testing by a neuropsychologist or neurologist can differentiate mild cognitive impairment from dementia and identify reversible factors
Imaging and labs: CT or MRI to identify stroke, tumors, or hydrocephalus; labs to rule out reversible causes (thyroid function, vitamin deficiencies, infections, metabolic disorders)
Biomarkers and diagnostics (emerging): blood-based amyloid/tau measures; CSF biomarkers; PET imaging for amyloid/tau; potential for earlier and more accessible diagnosis, with implications for treatment
Staging and progression evaluation: use multiple scales; recognize that scores can vary by education and baseline functioning; family input remains critical for accurate staging and monitoring
Practical and ethical implications for nursing practice
Early identification and safety: prioritize safety in all neurological and cognitive issues; assess for risk of falls, aspiration, and functional decline; implement prevention measures
Interdisciplinary care: collaborate with PT/OT, speech-language pathology, nutrition, social work, and bereavement/caregiver support services
Patient-centered care: tailor care plans to the patient’s goals and stage of disease; respect preferences while ensuring safety and quality of life
Education and resources: connect families with community resources, respite care, adult day services, home health, and legal services; discuss advance care planning when appropriate
Ethical considerations: balance autonomy with safety in dementia care; manage behavioral symptoms with least restrictive approaches; avoid unnecessary aggressive pharmacologic interventions
Quick reference: key numbers and terms (LaTeX-ready)
Onset age for neuron loss: after 25 years
Time window for thrombolysis in acute stroke: 3\ hours
Alzheimer’s disease prevalence among dementia patients: 60\%-80\%
Lewy body dementia prevalence: 5\%-10\%
Vascular dementia prevalence: 5\%-10\%
Frontotemporal dementia prevalence: 5\%-10\%
Modifiable risk factors reduction potential (Lancet Commission 2020): 40\% reduction in dementia incidence when addressed
ApoE4 allele risk: two copies increase risk by about 10\times baseline
Monoclonal antibodies for Alzheimer's (emerging): approximate reduction in cognitive decline 25\%-30\% over 18\text{ months}; ARIA risk; frequent MRI monitoring
Geriatric Depression Scale (GDS-15) threshold: score > 5 suggests depression requiring further evaluation
Alcohol screening (SMAST-G): two or more “Yes” answers indicates an alcohol problem
Suicide statistics: older adults account for about 29\% of suicide deaths; highest in men 85+; risk factors include bereavement, illness, isolation, retirement
End of notes
Describe effects of aging on nervous system
Normal Physiological Changes:
Neuron loss: begins after about age 25 and increases with age.
Neurotransmitters: fewer available in the aging brain.
Nerve conduction and reaction time: slower in older adults.
Brain atrophy: decrease in brain size and neuron count; space increases on imaging.
Plaques: form in nerve cell bodies.
Cerebral blood flow: slows somewhat.
Hippocampus changes: affects memory retrieval and storage.
Activating system changes: alters sleep-cycle regulation.
Sensory decline: receptors decrease in number and sensitivity; cranial nerves show aging-related changes; vision, hearing, taste, smell, vibratory sensation often diminished.
Temperature sensation: reduced ability to sense temperature changes, implying environmental safety considerations.
Balance and postural control: increased risk for postural hypotension and falls; sensitivity to blood pressure-lowering medications.
Intellectual maintenance: generally preserved; wisdom and emotional intelligence may improve or stay strong; verbal skills often preserved until around age 70, then vocabulary can decline.
Clinical Manifestations Linked to Normal Aging (Summary):
Sleep changes: less REM sleep; longer time in stages 1–2; easier to wake; increased daytime sleepiness.
Learning: altered ability to learn new information quickly, though still possible with effort.
Memory: storage/retrieval affected via hippocampus; occasional difficulty recalling names or words is common and usually gradual.
Vision/hearing changes: sensory deficits impact communication and safety.
Taste/smell changes: can influence nutrition; adapt to maintain intake.
Postural hypotension and balance issues: greater risk with antihypertensive or diuretic therapies; careful drug management needed.
Temperature regulation: environmental safety importance.
Cognitive function and intellect: intelligence maintained; some decline in processing speed, but not necessarily loss of intellect.
Functional status: slower task performance; potential need for supports or assistive devices.
List risk factors for neurologic problems in older adults
Parkinson's Disease (PD):
Genetic (autosomal dominant defect on chromosome 4).
Environmental factors; potential drug/toxin exposure; trauma history.
Cerebrovascular Accident (CVA) / Stroke:
Non-modifiable: advanced age, genetics, African American ethnicity.
Modifiable: diabetes, cigarette smoking, heart disease, obesity, physical inactivity, cocaine use, atrial fibrillation (AFib), hypertension (most important modifiable risk factor).
Alzheimer’s Disease (AD) and Dementia:
Non-modifiable: age, family history, ApoE4 allele (two copies confer higher risk; up to \sim10\times baseline risk); early-onset dementia linked to strong family history/genetics.
Modifiable (Lancet Commission 2020): reduced incidence of dementia by addressing multiple factors; key factors include 40\% risk reduction if addressed collectively: less education, hearing loss, hypertension, physical inactivity, diabetes, obesity, low social contact, depression, tobacco, head injury, and potentially excessive alcohol.
Describe measures to promote neurologic health, promote independence, and reduce risk of injury in older adults
General Nursing Actions:
Distinguish normal aging from pathological changes; monitor for differences in presentation and degree.
Prioritize safety in all neurological and cognitive issues; assess for risk of falls, aspiration, and functional decline; implement prevention measures.
Interdisciplinary care: collaborate with PT/OT, speech-language pathology, nutrition, social work, and bereavement/caregiver support services.
Patient-centered care: tailor care plans to the patient’s goals and stage of disease; respect preferences while ensuring safety and quality of life.
Education and resources: connect families with community resources, respite care, adult day services, home health, and legal services; discuss advance care planning when appropriate.
Ethical considerations: balance autonomy with safety in dementia care; manage behavioral symptoms with least restrictive approaches; avoid unnecessary aggressive pharmacologic interventions.
Parkinson's Disease Interventions:
Maintain cognition and function, prevent injuries from impaired movement, minimize falls, safety-focused teaching.
Nursing care plan elements: active range of motion exercises twice daily; ambulation with assistive devices (walker/cane) and PT consult when mobility declines; OT consult for activities of daily living and adaptive devices; speech/swallow therapy for dysphagia and communication challenges; nutritional assessment and support; monitor weight and dietary needs; psychological support; address caregiver burden; community resources.
Safety and management emphasis: prevent falls, plan for evolving needs, enable independent function where possible.
Stroke Prevention:
Stroke prevention education.
Acute nursing interventions: keep head elevated, monitor vitals, turn and ROM every 2 hours, encourage use of unaffected arm for ADLs, ensure swallow safety and resumption of oral intake after swallow study.
Priority considerations: safety and prevention of secondary injury; test-tasks often emphasize safety as the highest priority in acute care.
Dementia and Alzheimer’s Disease Nonpharmacologic Approaches (also promoting mental health):
Cognitive stimulation therapy, communication therapies, behavioral therapy to limit triggers, reality orientation, validation therapy, reminiscence therapy.
Safety planning; establishing regular routines; balancing independence with caregiver support.
Simple, stage-appropriate communication; meaningful activities to improve quality of life.
Identify signs and symptoms of neurologic disorders in older adults
Red Flags Requiring Further Evaluation (Nursing Alarm Signs):
New headaches, new vision changes.
Sudden deafness or tinnitus.
Rapid mood or personality changes.
Altered consciousness or cognition.
New clumsiness or unstable gait.
Numbness or tingling in extremities or unusual nerve sensations.
Parkinson's Disease (PD) Symptoms:
Classic motor symptoms: resting tremor (often initial), bradykinesia (slowness of initiation), impaired postural reflexes.
Typical body presentation: stooped/forward-leaning posture, rigid back, shuffling gait, masked facial expression.
Non-motor features: heat intolerance, constipation, depression; decreased perspiration; dysphagia risk with disease progression.
Cerebrovascular Accident (CVA) / Stroke Symptoms:
Common presenting symptoms: sudden unilateral facial, arm, or leg numbness or weakness (usually on one side); confusion or trouble speaking; trouble seeing in one or both eyes (hemianopsia); trouble walking, dizziness, loss of coordination; severe headache may occur.
Dementia Symptoms:
Progressive, irreversible cognitive deterioration with personality changes and functional decline; memory impairment, disorganized thinking, inattentiveness, change in behavior.
Frontotemporal dementia (FTD): earlier onset (often <60); affects frontal lobes; early behavioral changes or language impairment.
Lewy body dementia (LBD): parkinsonian symptoms along with cognitive fluctuations and early visual hallucinations (due to alpha-synuclein inclusions/Lewy bodies).
Neuropsychiatric symptoms: resisting care, repetitive actions, delusions, sexual disinhibition, wandering, suspiciousness.
Delirium Symptoms:
Acute, abrupt global cognitive impairment with fluctuating mental status; may be worse at night; disorganized thinking; inattention; altered alertness; can include agitation or hypoactivity; hallucinations common in hospital settings.
Describe symptoms, unique features and nursing care for patients with Parkinson’s disease, transient ischemic attacks, and cerebrovascular accidents in older adults
Parkinson's Disease (PD):
Symptoms: Resting tremor, bradykinesia, impaired postural reflexes, stooped/forward-leaning posture, rigid back, shuffling gait, masked facial expression, non-motor features like heat intolerance, constipation, and depression; dysphagia risk with progression.
Pathophysiology: Decreased dopamine in basal ganglia; balance between acetylcholine (excitatory) and dopamine (smooth movement) disrupted.
Treatments (symptom management): Dopaminergic therapy (carbidopa-levodopa), dopamine agonists, anticholinergics, Catechol O-methyltransferase (COMT) inhibitors. Surgical options include ablation and deep brain stimulation (DBS).
Nursing Care: Maintain cognition and function, prevent injuries from impaired movement, minimize falls, safety-focused teaching. Implement active range of motion exercises, ambulation with assistive devices, and consults for PT, OT, speech/swallow therapy. Provide nutritional assessment and support, psychological support, and address caregiver burden.
Transient Ischemic Attacks (TIA):
While not detailed as a separate section in the notes, TIAs are considered mini-strokes with temporary symptoms that resolve. They share common risk factors with CVA/Stroke and are often a warning sign for a future stroke. Nursing care focuses on identifying risk factors and implementing stroke prevention strategies as outlined under CVA management.
Cerebrovascular Accident (CVA) / Stroke:
Types: Hemorrhagic stroke (bleed) vs Ischemic/Thrombotic stroke (clot).
Onset: Hemorrhagic strokes often have abrupt onset; ischemic strokes may have sudden onset or evolve over minutes to hours.
Common Presenting Symptoms: Sudden unilateral facial, arm, or leg numbness or weakness; confusion or trouble speaking; trouble seeing in one or both eyes (hemianopsia); trouble walking, dizziness, loss of coordination; severe headache may occur.
Risk Factors: Advanced age, genetics, African American ethnicity, diabetes, cigarette smoking, heart disease, obesity, physical inactivity, cocaine use, atrial fibrillation (AFib), hypertension (most important modifiable risk factor).
Acute Management in Hospital: Emergency CT scan; continuous monitoring (cardiac and other vitals); labs; possibly EEG; airway protection; head of bed elevated to reduce intracranial pressure (ICP).
Neuro Assessment: NIH Stroke Scale or similar tools; assess level of consciousness, orientation, commands, gaze, visual fields, motor function, sensory, language, and cognition.
Reperfusion Therapy: Thrombolytic therapy within a 3\ hour window (time is brain); earlier treatment yields better outcomes, though guidelines may vary.
Medications and Interventions: Anticoagulants or antiplatelets depending on etiology; lipid-lowering agents and antihypertensives for long-term secondary prevention. Indirect vascular procedures (carotid endarterectomy or extracranial bypass) and brain surgery for certain conditions (aneurysms, malformations, intracranial bleeding).
Acute Nursing Interventions: Keep head elevated, monitor vitals, turn and ROM every 2 hours, encourage use of unaffected arm for ADLs, ensure swallow safety and resumption of oral intake after swallow study.
Speech and Language Concerns: Aphasia types (receptive vs expressive); visual field deficits (hemianopia); adapt patient/family education to language abilities.
Outcomes and Planning: Stroke prevention education, access to resources, and long-term rehabilitation planning. Safety and prevention of secondary injury are highest priorities.
List measures that promote mental health for older adults
For Depression: Psychotherapy and nonpharmacologic approaches (acupuncture, guided imagery, light therapy, sleep, exercise, nutrition).
For Anxiety: Coaching and coping strategies; relaxation and deep breathing; modify perceptions of stress; psychotherapy and nonpharmacological approaches preferred.
For Dementia: Cognitive stimulation therapy, communication therapies, behavioral therapy to limit triggers, reality orientation, validation therapy, reminiscence therapy; promoting meaningful activities.
Describe symptoms and care for an older adult with depression
Symptoms: Fatigue, constipation, psychomotor retardation, persistent depressed mood, anhedonia, low energy, social withdrawal, neglect of hygiene or self-care, somatic complaints. Altered cognition is common and can mimic dementia.
Causes and Contributing Factors: Chronic illnesses, aging-related losses (bereavement, relocation, retirement), changes in social roles and income, societal undervaluation of older adults; certain medications may contribute.
Screening: Geriatric Depression Scale (GDS-15); scores > 5 suggest depression requiring further evaluation.
Treatment Considerations and Care:
Prefer SSRIs over tricyclic antidepressants (TCAs) due to anticholinergic side effects and safety concerns in older adults.
Avoid combining SSRIs with St. John’s wort.
Consider psychotherapy and nonpharmacologic approaches (acupuncture, guided imagery, light therapy, sleep, exercise, nutrition).
"Start low, go slow" with gradual dosing and small increases to minimize side effects and falls risk.
Expect SSRIs to take \sim2\ weeks or more to show effect.
Identify indications of suicidal thoughts in older adults
Suicide Risk Factors:
High among older adults, accounting for \sim29\% of suicide deaths.
Highest risk in men aged 85+ and older white men.
Specific risk factors include bereavement, chronic illness, social isolation, and retirement.
Assessment and Response:
Use structured tools (e.g., National Institute of Mental Health resources) to assess frequency of thoughts, plan, past attempts, symptoms, and social support.
Determine disposition (emergency psychiatric evaluation, inpatient care, or nonurgent follow-up).
Implement safety planning and no-suicide contracts when appropriate.
Describe interventions to reduce anxiety in older adults
Coaching and coping strategies.
Relaxation and deep breathing techniques.
Modifying perceptions of stress.
Psychotherapy and nonpharmacological approaches are preferred.
Medications should be a last resort in older adults due to safety concerns.
Discuss signs of substance abuse in older adults. Identify nursing actions to manage disruptive behavior associated with mental health conditions in older adults
Signs of Substance Abuse:
Alcohol Use: SMAST-G screening; two or more positive responses suggests an alcohol problem. Recommended limits typically not more than one standard drink per day for older adults.
General Substance Abuse: Not rare; may involve prescription opioids and other substances; increased risk of falls, cognitive impairment, self-neglect.
Nursing Actions for Substance Abuse:
Withdrawal management and attention to potential interactions with medications (for alcohol withdrawal, benzodiazepines can be dangerous in older adults).
Discuss strategies for safe medication use and monitoring; do not overlook prescription misuse and social factors that sustain abuse.
Managing Disruptive Behavior Associated with Mental Health Conditions (e.g., in Dementia):
Common behaviors include resisting care, repetitive actions, delusions, sexual disinhibition, wandering, and suspiciousness.
Management requires a person-centered approach and may include diverting attention, environmental adjustments, and boundary-setting.
Antipsychotics carry higher mortality and should be used cautiously as a last resort.
For sexual disinhibition: Set clear and professional boundaries; acknowledge feelings but keep care focused on medical needs.
For wandering and agitation: Use distraction, safety measures, and engaging activities; explain to family and staff the importance of reducing triggers and enhancing routines.
Utilize communication strategies: Keep messages simple; tailor to the person’s stage; involve family; use reminiscence and validation approaches to reduce distress.
Differentiate delirium from dementia
Delirium:
Acute, abrupt global cognitive impairment with fluctuating mental status; may be worse at night.
Characterized by disorganized thinking, inattention, altered alertness; can include agitation or hypoactivity.
Hallucinations are common, especially in hospital settings.
Dementia:
Progressive, irreversible cognitive deterioration with personality changes and functional decline.
DSM-5 defines major neurocognitive disorder as dementia; mild neurocognitive disorder (MCI) is cognitive decline not yet affecting ADLs/IADLs.
Key distinction: Delirium is acute and fluctuating, while dementia is progressive and irreversible.
Co-occurring Conditions:
Delirium often superimposed on dementia; do not assume delirium is simply a manifestation of baseline dementia. Obtain history and observe for changes; educate families and involve them in care planning.
Identify factors that cause delirium
Drugs (medication changes, polypharmacy).
Electrolyte and acid-base imbalances.
Oxygen delivery/deficiency (hypoxia).
Hypothyroidism.
Infections (e.g., UTIs, pneumonia).
Bladder/bowel retention.
Hypoglycemia/hyperglycemia.
Sleep deprivation.
Sensory deprivation or overstimulation.
Environmental factors (unfamiliar surroundings, ICU).
Describe characteristics, symptoms, and management of dementia
Characteristics and Symptoms:
Progressive, irreversible cognitive deterioration with personality changes and functional decline.
Memory impairment, disorganized thinking, inattentiveness, and changes in behavior (e.g., resisting care, repetitive actions, delusions, wandering, suspiciousness).
Management (Nonpharmacologic Approaches):
Cognitive stimulation therapy, communication therapies, behavioral therapy to limit triggers, reality orientation, validation therapy, reminiscence therapy.
Safety planning; establishing regular routines; balancing independence with caregiver support; simple, stage-appropriate communication; meaningful activities to improve quality of life.
Management (Pharmacologic Approaches for Alzheimer's Disease):
Symptom management: Cholinesterase inhibitors (e.g., donepezil) and memantine to modulate glutamate activity; these can slow symptoms but do not cure AD.
Disease-modifying therapies (recent advances): Monoclonal antibodies targeting amyloid plaques, such as Leqembi (lecanemab) and Donanemab.
These therapies can slow cognitive decline by approximately 25\%-30\% over 18\text{ months} but carry risks of amyloid-related imaging abnormalities (ARIA) and require frequent MRI surveillance (e.g., every 4 weeks during active treatment).
Administration typically involves IV infusions every two weeks.
List causes of dementia. Outline nursing considerations for older adults with dementia
Causes of Dementia (Etiologies):
Alzheimer’s disease: Accounts for 60\%-80\% of dementia cases; characterized by beta-amyloid plaques and tau tangles.
Lewy body dementia (LBD): 5\%-10\% of cases; involves alpha-synuclein inclusions (Lewy bodies), parkinsonian symptoms, cognitive fluctuations, and early visual hallucinations.
Vascular dementia: 5\%-10\% of cases; often shows a stepwise decline after each cerebrovascular event.
Frontotemporal dementia (FTD): 5\%-10\% of cases; earlier onset (often <60); affects frontal lobes, leading to early behavioral changes or language impairment.
Other diseases: AIDS and Parkinson’s disease may contribute.
Other causes and mimics (reversible conditions to be ruled out): Depression, drugs, vitamin/mineral deficiencies, thyroid disorders, metabolic issues, infections, exposure to toxins.
Nursing Considerations for Older Adults with Dementia:
Environment Optimization: Create a calm, well-lit, and predictable routine-based environment.
Family Involvement: Involve family in care planning and provide education; offer a 24-hour sitter if needed.
Safety and Reorientation: Prioritize patient safety, assess for fall/aspiration risk, and provide consistent reorientation.
Documentation: Document delirium status according to unit protocol, especially when superimposed on dementia.
Support and Resources: Emphasize balancing independence with caregiver support to reduce burnout; connect families with community resources like respite care, adult day services, home health, and legal services; discuss advance care planning.
Behavioral Management: Manage neuropsychiatric symptoms (e.g., resisting care, wandering, agitation, sexual disinhibition) with a person-centered approach, diversion, environmental adjustments, and boundary-setting. Use antipsychotics cautiously as a last resort due to higher mortality risk.
Communication: Use simple messages, tailor communication to the person’s stage, involve family, and employ reminiscence and validation approaches to reduce distress.
Ethical Considerations: Balance autonomy with safety; manage behavioral symptoms with the least restrictive approaches; avoid unnecessary aggressive pharmacologic interventions.