Renal Blood Flow & Autoregulation
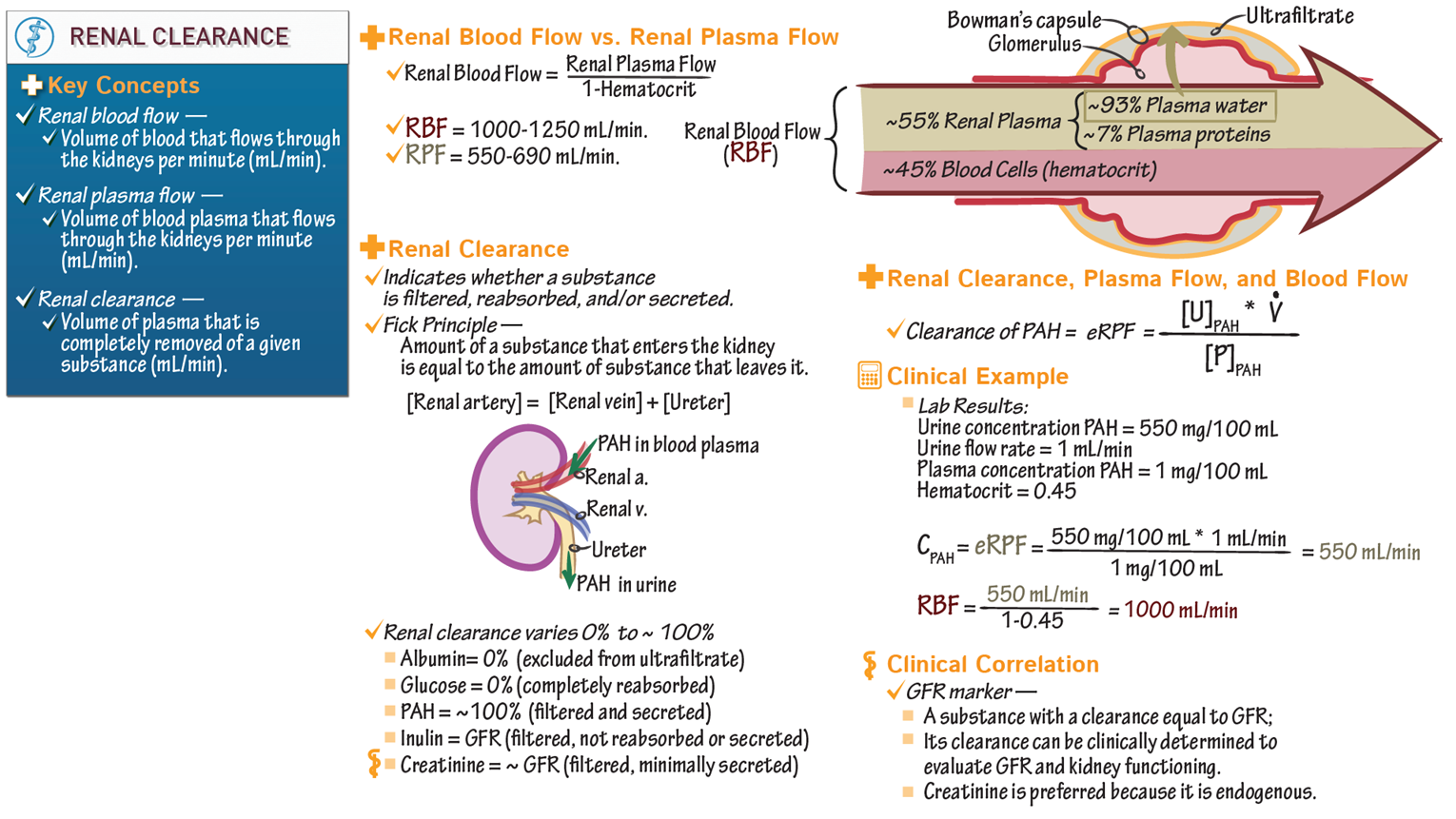
Renal Blood Flow (RBF)
measures the amount of blood AND plasma passing through kidneys
RBF can be estimated via RPF and hematocrit
Renal Plasma Flow (RPF)
measures the amount of PLASMA that passes through the glomerulus
Plasma contains NO CELLS
RPF can be measured using creatinine or PAH
Renal plasma clearance
the volume of plasma that is completely removed of a substance
the rate at which the kidneys can clear a substance from the blood reflects total renal plasma flow.
albumin & glucose 0% bc cant cross glomerulus
Renal clearance of Creatinine
volume of plasma that is completely removed of creatinine
should be 100%
creatinine filtered across the glomerulus but not reabsorbed by the nephrons

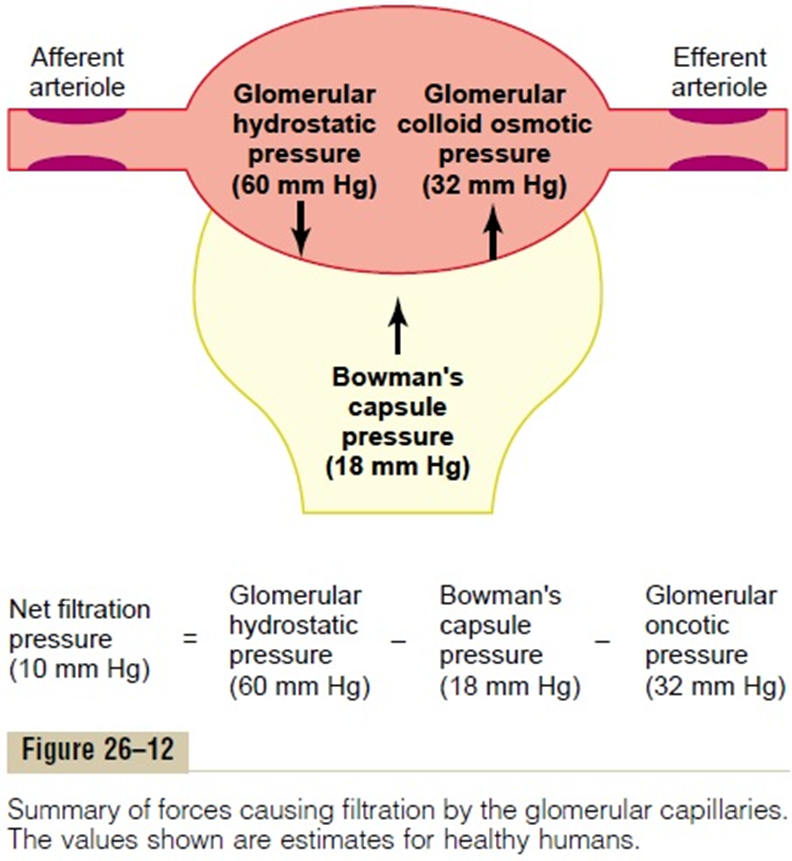
Constriction of afferent arteriole
RPF: dec
GFR: dec
FF: no change
dec glomerular hydrostatic pressure
Constriction of efferent arteriole
RPF: dec
GFR: inc
FF: inc
inc glomerular hydrostatic pressure
inc proteins in plasma
RPF: no change
GFR: dec
FF: dec
inc oncotic pressure
Constriction of ureter
RPF: no change
GFR: dec
FF: dec
due to inc Bowmans capsule hydrostatic pressure
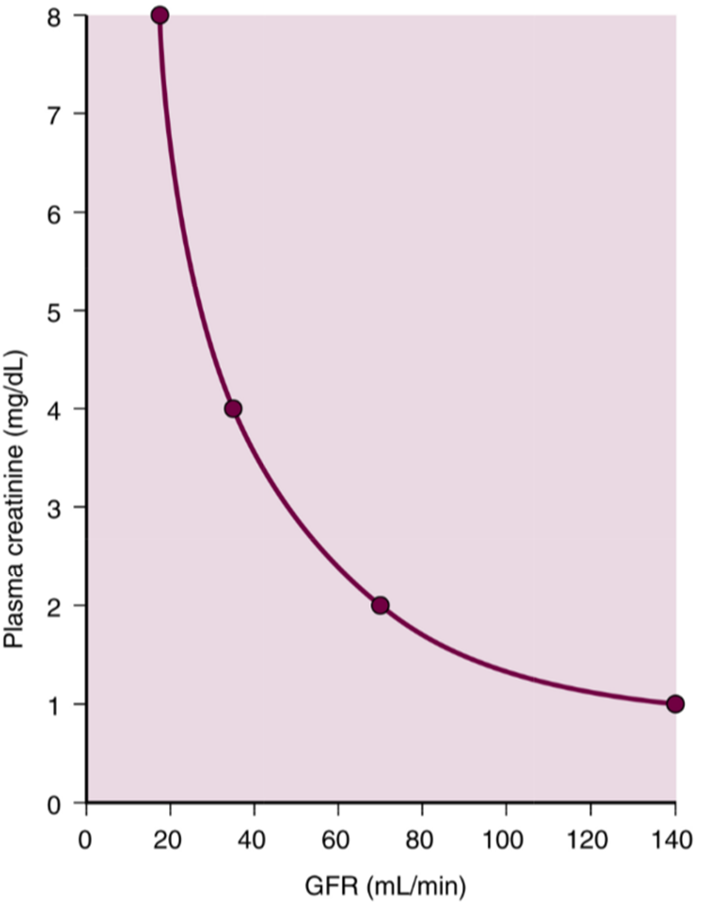
GFR = creatinine clearance
GFR = Creatinine in urine x urine vol / creatinine in blood
filtered across the glomerulus but not reabsorbed by the nephrons
Production of creatinine is in steady state in healthy person.
Production, filtration, and ultrafiltrate excretion measurements are matched if GFR is normal
An INCREASE in plasma creatinine = inability to filter and excrete it
often caused by low GFR
Blood Urea Nitrogen (BUN)
Urea is byproduct of protein catabolism
partially reabsorbed along the nephron
Reabsorption increases as water reabsorption increases
Used to increases osmotic gradient
Determinant of kidney function
Typically excreted from the body
RAAS and ADH activated in the setting of perfusion problem ADH reabsorbes water and urea, which is why BUN is High in perfusion problems
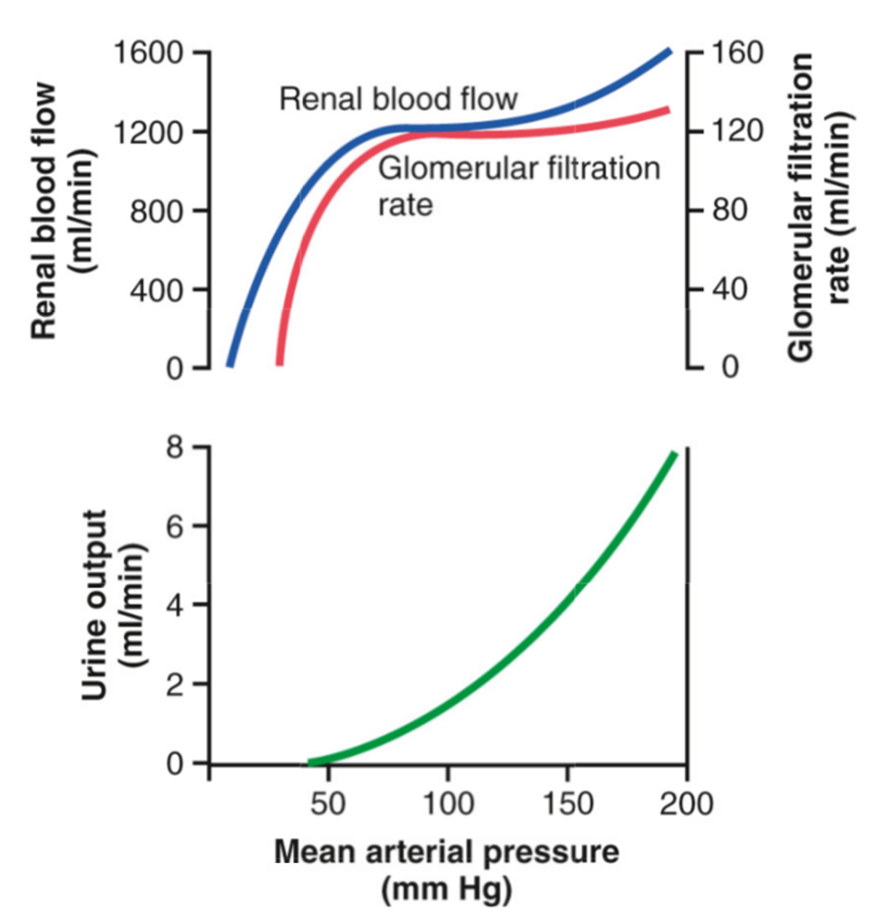
Autoregulation
Kidney can control its own blood flow in response to change in perfusion pressure
v wide range
hormones, sns, angiotension II, and ANP all effect autoregulation
Mechanisms of autoregulation
Myogenic response
At the level of the smooth muscle
Reacts to blood flow/pressure changes, mechanical
Tubuglomelur feedback
The nephron senses its own perfusion blood flow and adjusts
Reacts to ultrafiltrate flow changes/Intraglomerular pressure
RAAS
Renin released from kidney, causes release of others
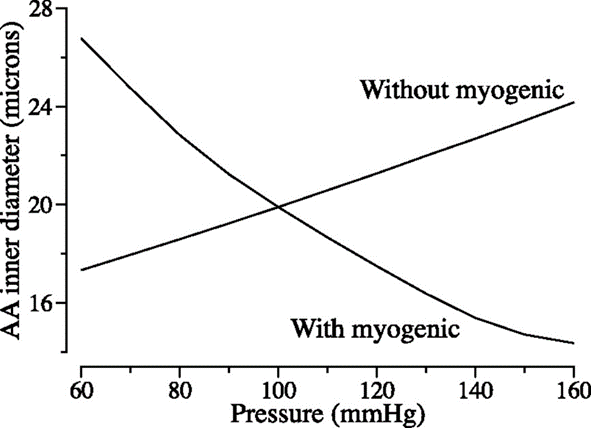
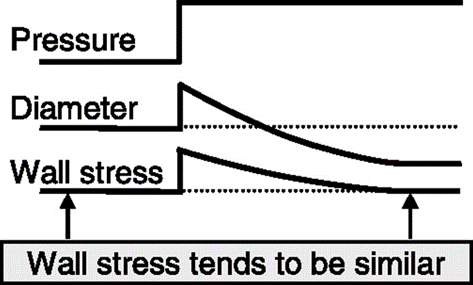
Myogenic response
Response of smooth muscles to stretch
Increase transmural pressure of vessel and decreases diameter of vessel
Maintains constant flow by changing resistance
Prevents high pressure from damaging the glomerulus
increased Na = constrict afferet = dec hydrostatic= dec GFR
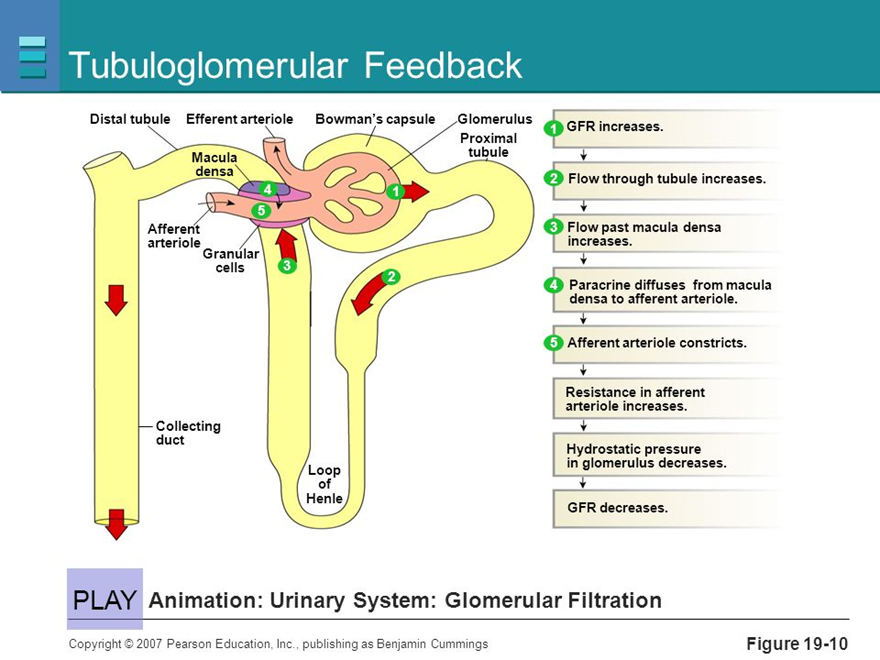
Tubuglomelur feedback
Links tubular sodium concentration to GFR and blood pressure
High Na = high BP → High GFR → High Tubular Na
Occurs at the Juxtaglomerular Apparatus
Macula Densa (right next to DCT)
Sodium sensor in DCT
high pressure/Na = inc adenosine (ADO)
Adenosine bind to A1 receptors to constrict afferent arteriole
inhibits renin release
to dilatate efferent arterioles
RAAS
Renin released by the JGA when
Arterial pressure is low
Tubular Sodium decreases
Effective circulating volume (ECV) decreases
Ang II and aldosterone inc pressure
Ang II : constricts EFFERENTS arteriole and stimulates release of ADH
Aldosterone increases Na reabsorption
ADH released in setting of hypoperfusion
Reabsorbs free water and urea
ALL INCREASE VOL AND PRESSURE
PRERENAL = PERFUSION PROBLEM
Vasoactive compounds
Norepinephrine and Epinephrine
Constrict AFFERENT and EFFERENT
dec GFR and RBF
Endothelin
vasoconstrictor
dec GFR and RBF
Nitric Oxide
Vasodilators
inc GFR and RBF
ANP/BNP
Inhibits renin, which causes naturesis (excretion of Na)
Prostaglandins
Vasodilators of AFFERENTS
Nonperfusion AKI
Kidney uses lots of ATP, thus produces lots of CO2
BUN is not elevated
Renal Ischemia can lead to loss of autoregulation due to death of cells in JGA
Most damage will occur in the sites of greatest active transport
Proximal tubule
Thick ascending limb of JG nephron
Macula Densa
Produces “Skip Lesions” where part of the nephron is damaged, but the rest is fine.
