Chapter 25: The Digestive Tract
Introduction to the Digestive System
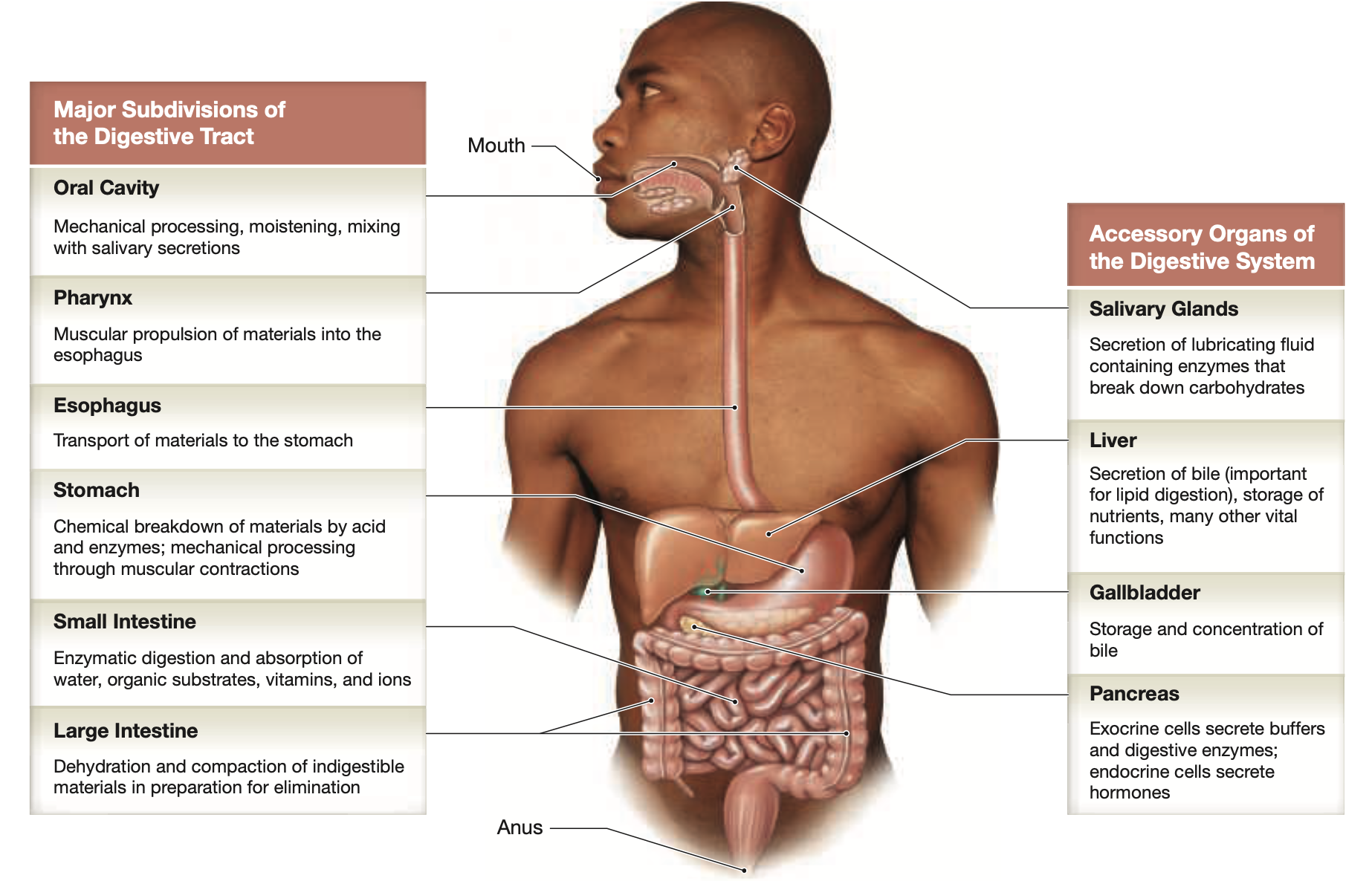
The digestive system comprises the muscular digestive tract and accessory organs.
Think of it as one long tube or canal that starts at the mouth and ends at the anus, facilitating the entire process of food ingestion, digestion, absorption of nutrients, and elimination of waste.
The digestive tract & accessory organs are responsible for:
Ingestion— Bringing foods & liquids into the mouth
Mechanical Processing— Chewing & Swallowing
Digestion— Chemical & enzymatic breakdown of food into nutrients
Secretion— Acids, enzymes, & buffers form GI lining or accessory organs
Absorption— Movement of nutrients from the small intestine to the bloodstream regressive
Compaction— Dehydration of indigestible materials & organic wastes
Excretion— removal of wastes from the digestive tract
25.1 An Overview of the Digestive System
Histological Organization of the Digestive Tract
Major layers of the digestive tract:
Mucosa: inner lining, consisting of mucosal epithelium and lamina propria.
Plicae— Folds of the mucosa that increase surface area for maximum absorption and secretion, particularly prominent in the small intestine.
Submucosa: Composed of areolar tissue (blood supply)
Submucosal Neural Plexuses— networks of neurons located in the submucosa and muscular layers that regulate digestive functions including motility and secretion.
Muscularis Externa (Muscular Layer): Contains smooth muscle fibers.
Myenteric Plexus— a network of nerves located between the muscular layers of the gastrointestinal tract that plays a crucial role in regulating digestive motility and coordinating peristalsis.
Serosa: A serous membrane in the peritoneal cavity.
Muscular Layers and Movement of Digestive Materials
Smooth muscle cells in the digestive tract exhibit plasticity, tolerating extreme stretching.
Contains visceral smooth muscle tissue arranged in sheets with no motor innervation.
Pacesetter cells cause rhythmic contraction waves—
Peristalsis— waves of muscular contractions propel materials through the digestive tract
Essentially pushes things forward through “the tube”
Segmentation— Movements that churn and fragment material with no movement towards a particular area
Essentially smashing materials to increase the efficiency of nutrient absorption and facilitate digestion before they are further broken down in the intestines.
The Peritoneum
The serosa (visceral peritoneum) is continuous with the parietal peritoneum lining the body wall.
Abdominal organs may be:
Intraperitoneal— Organs that are completely enveloped by visceral peritoneum
ie stomach, liver, Ileum
Retroperitoneal— Organs that are located behind the peritoneum and not completely surrounded by it
ie the kidneys and ureters
Secondarily Retroperitoneal— Organs that were originally formed in the intraperitoneal cavity but later become retroperitoneal during embryonic development,
ie the duodenum (first portion of small intestines) and the pancreas
Mesenteries are fused double sheets of peritoneal membrane that suspend digestive tract portions, found within the peritoneal cavity.
Stabilizes organs & blood vessels
25.2 The Oral Cavity
Functions of the Oral Cavity
Sensory analysis of food.
Mechanical processing (teeth, tongue).
Lubrication with mucus and saliva.
Limited digestion via salivary enzymes.
Anatomy of the Oral Cavity
Stratified Squamous Epithelium lines the oral cavity
The oral cavity consists of 2 Palates:
Hard Palate— Separates oral cavity from nasal cavity
Soft Palate— Lies posterior to the hard palate, separates the oral cavity from the nasopharynx, closes off the nasopharynx during swallowing.
Uvula— hangs in the posterior center of soft palate
The tongue facilitates food manipulation and sensory analysis; dorsum of tongue covered in papillae.
Anterior body, posterior root
Frenulum of the tongue— Thin fold of mucous membrane connects the body of the tongue to the mucosa of the oral floor.
Glands: Salivary glands secrete salivary amylase, secretions controlled by the autonomic nervous system
Parotid— The largest of the salivary glands, located near the ear
Sublingual— The smallest salivary glands, situated beneath the tongue
Submandibular— The glands located beneath the jaw
Teeth: Designed for mastication
The Crown (enamel) surrounds the Dentine, which is the hard tissue beneath the enamel and forms the bulk of the tooth structure.
Roots: Embedded in the jawbone, providing stability and support to the tooth
Periodontal ligament— CT that attaches the tooth to the surrounding alveolar bone, allowing for slight movement and providing cushioning during chewing.
Types of teeth:
Incisors: Cutting
Canines (cuspids): Tearing
Premolars (bicuspids): Crushing
Molars: Grinding
Deciduous Teeth (20) are replaced by Permanent Teeth (32)
25.3 The Pharynx
Skeletal Muscles in Swallowing
Pharyngeal constrictor muscles, palatopharyngeus, stylopharyngeus aid swallowing.
The Swallowing (Deglutition) Process
Buccal Phase: The Bolus of food is compressed against the hard palate, tongue forces the bolus into the pharynx, isolating the nasopharynx
Pharyngeal Phase: The palatopharyngeus and stylopharyngeus muscles elevate the larynx, the epiglottis folds and the bolus passes the closed glottis toward the esophagus
Esophageal Phase: The upper esophageal sphincter opens, and perostalic waves push the bolus through the esophagus. The bolus reaches the lower esophageal sphincter and enters the stomach
25.4 The Esophagus
A hollow, muscular tube transporting food and liquids to the stomach.
Lies posterior to the trachea, slightly left of the midline
Esophageal Hiatus— the opening in the diaphragm through which the esophagus passes, allowing it to connect to the stomach.
Histology of the Esophageal Wall
Composed of mucosa, submucosa, muscular layer, and adventitia.
25.5 The Stomach
Major Functions
Temporary storage of ingested matter.
Mechanical breakdown of food.
Chemical digestion utilizing acids/enzyme disruption.
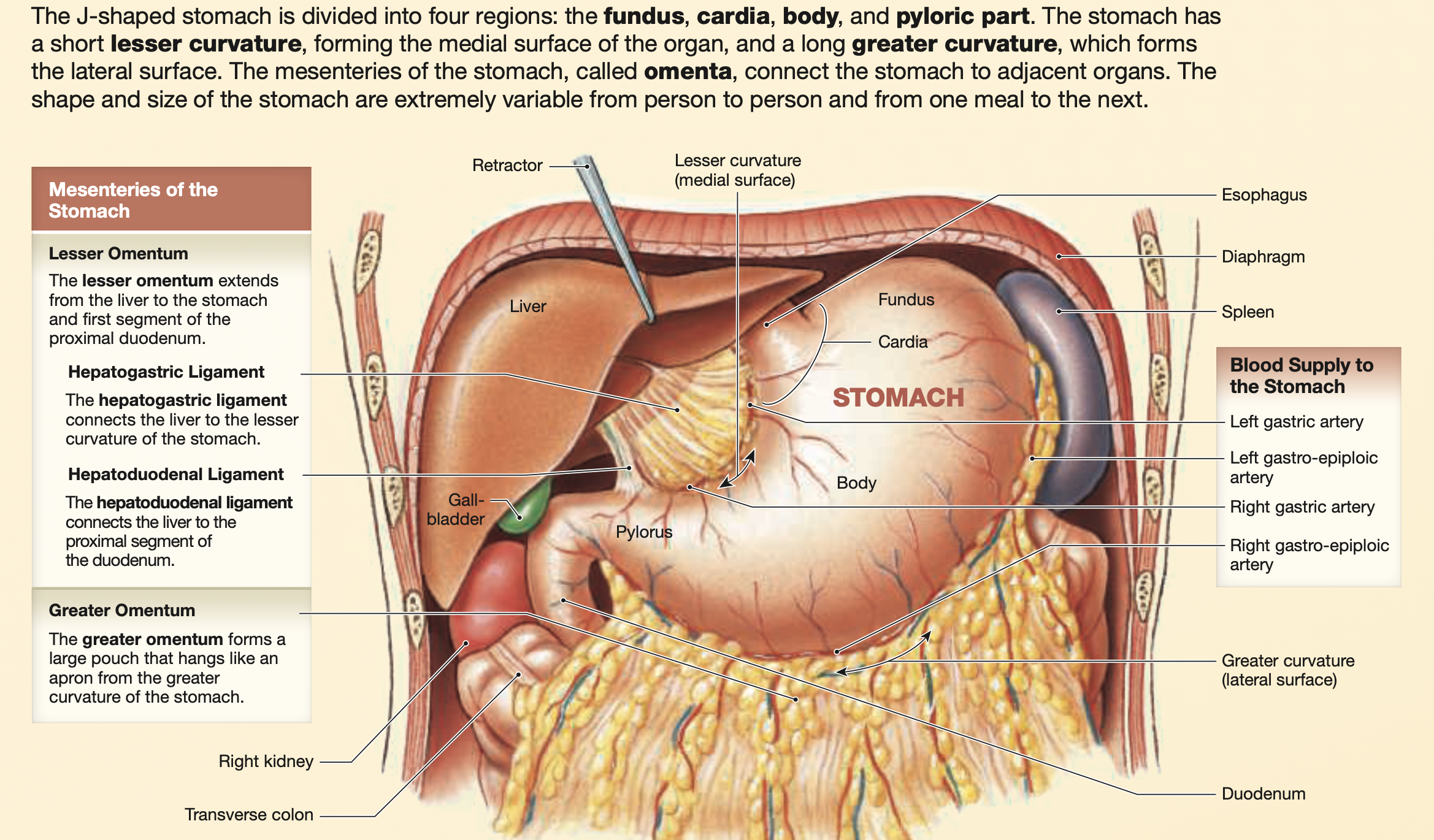
Anatomy of the Stomach
The anterior & posterior surfaces are smooth and rounded, typically extending from T7-L3
Divided into:
Cardia— Superior medial portion of the stomach that connects to the esophagus.
Fundus— The upper portion of the stomach, contacts inferior & posterior portions of the diaphragm
Body (Corpus)— The largest region of the stomach that functions as a mixing tank for ingested food and gastric secretions
Pyloric Part (Plyorus)— The lower portion of the stomach, connecting to the duodenum of the small intestine. Regulates the passage of partially digested food (chyme) into the duodenum via the:
Pyloric Antrum— The wider proximal portion, that connects the stomach to the duodenum
Pyloric canal: The narrower distal portion leading to the pyloric sphincter , which controls the flow of chyme from the stomach into the small intestine.
Muscular layer has three muscle bands:
Longitudinal
Circular
Inner Oblique
Supplied by left gastric, splenic, and common hepatic arteries.
Histology of the Stomach
Lined by simple columnar epithelium and shallow gastric pits.
There are four primary cells within the stomach:
Parietal cells: Secrete intrinsic factor and hydrochloric acid—
Lowers pH, denatures proteins, kills microorganisms
Chief cells: Only in the fundus, Secret pepsinogen, is converted to pepsin by acids.
Pepsin is responsible for the enzymatic digestion of proteins into peptides
G cells: Secrete hormone gastrin—
Stimulates the secretory activity of both parietal and chief cells
Mucous Neck Cells— Produce mucus to protect the gastric lining—
Protects it from the corrosive effects of hydrochloric acid
Regulation of Gastric Activity
Gastric secretions are controlled by the CNS and local hormonal signals.
25.6 The Small Intestine
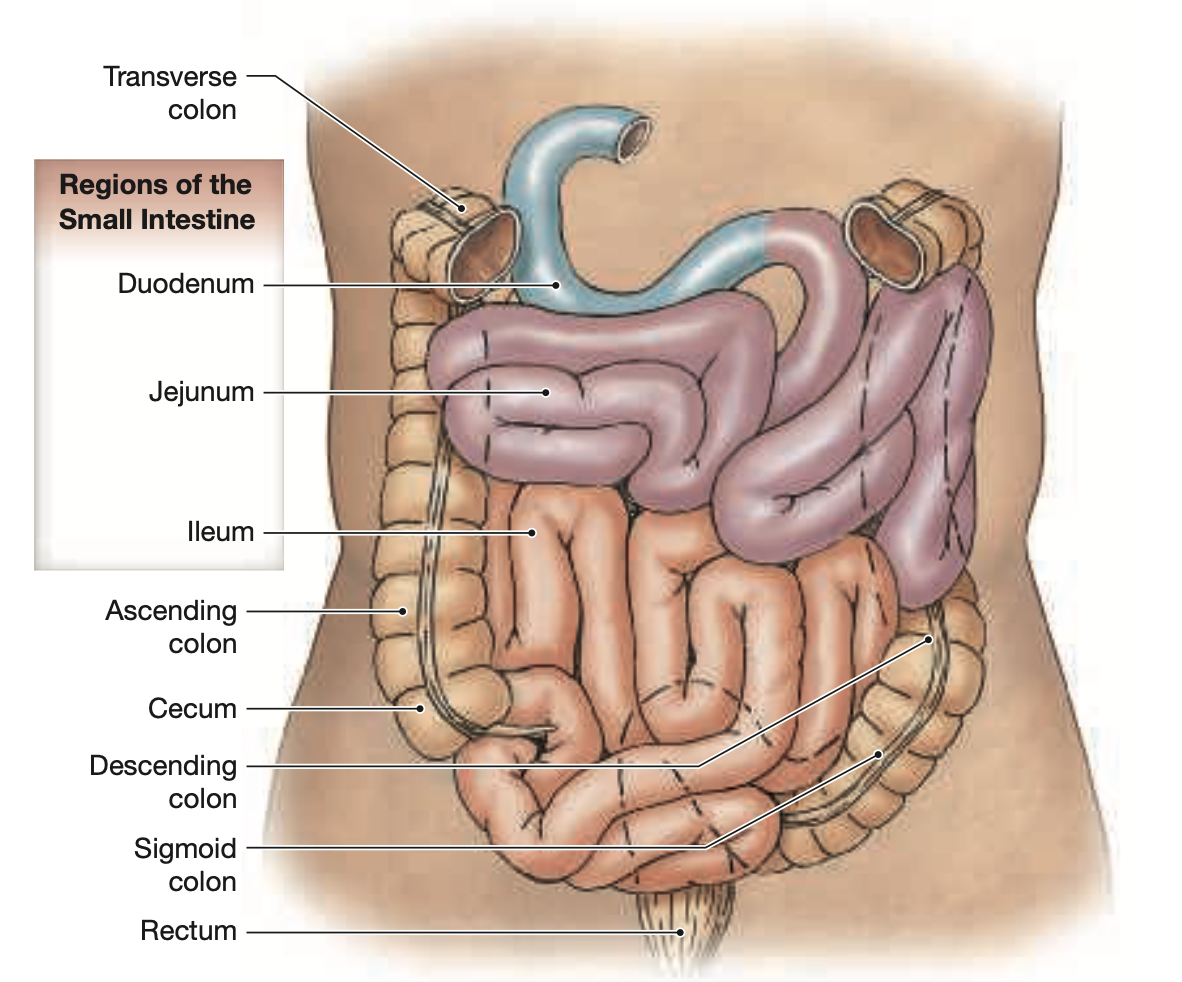
Regions
Comprises the:
Duodenum— The shortest and widest segment of the SI, it is responsible for the initial phase of digestion and the mixing of chyme with digestive juices from the pancreas and bile from the liver.
Jejunum— The middle section of the SI, where the bulk of chemical digestions occurs
Ileum— The final and longest segment of the SI, controls the flow of material from the ileum to the cecum of the LI
Support of the Small Intestine
The small intestine is specialized for absorption, with nearly 90% of bodily absorption taking place here
Supplied by the superior mesenteric artery and vein.
Mesentery proper supports blood, lymphatics, and nerves.
Histology of the Small Intestine
Circular folds and intestinal villi increase absorption surface area.
Lined by intestinal glands (enterocrine, goblet, stem cells).
Duodenum: Contains submucosal glands and receives bile and pancreatic secretions.
Ileum: Contains Peyer's patches (aggregated lymphoid nodules).
Regulation of the Small Intestine
Intestinal juice buffers acid and dissolves digestive enzymes/products.
25.7 The Large Intestine
Main Functions
Reabsorb water and compact feces.
Absorb vitamins from bacteria.
Store fecal material prior to defecation.
The horsed-shaped large intestine begins at the junction with the ileum and ends at the anus
Structure
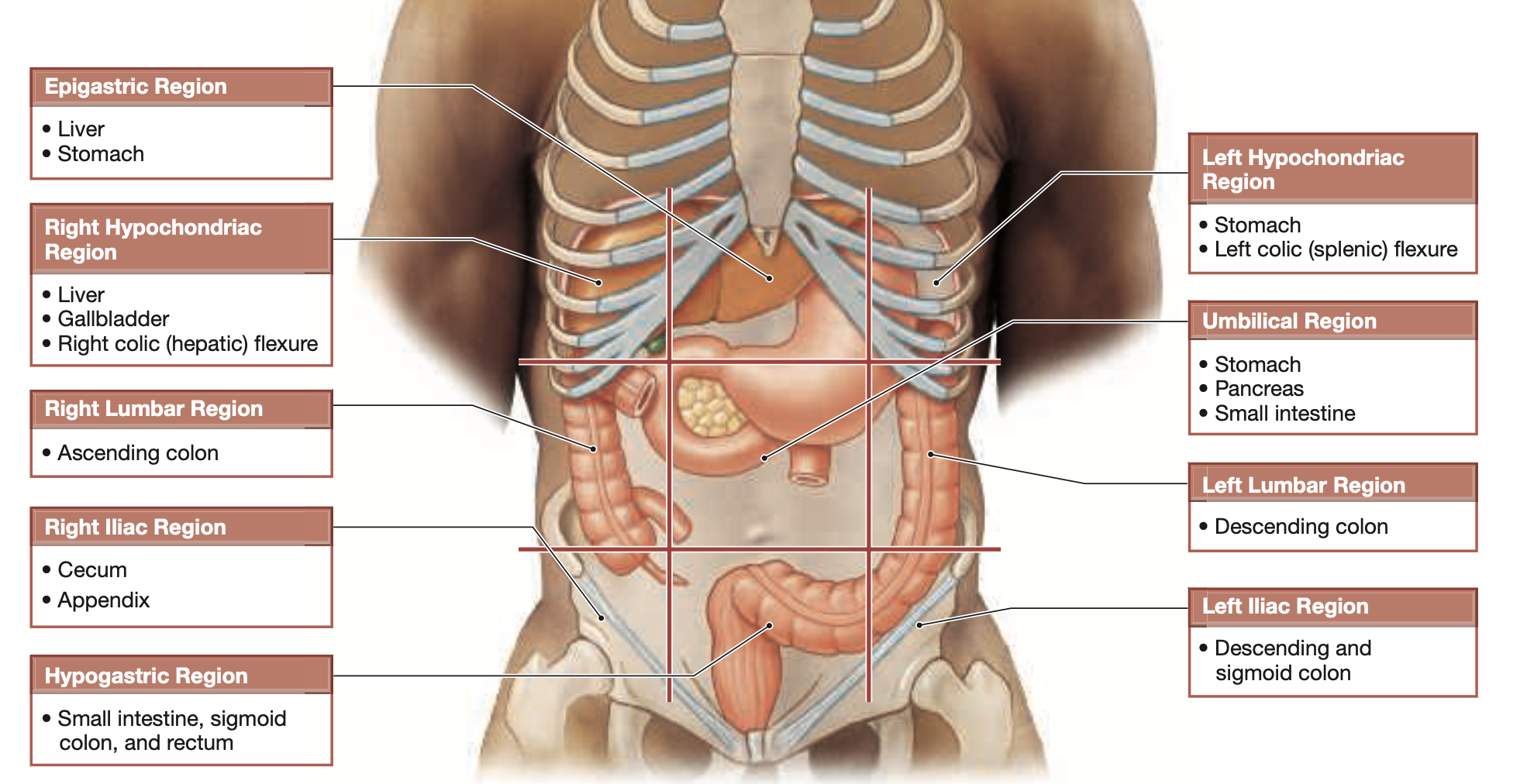
Divided into cecum, colon, and rectum.
Cecum and Appendix
Cecum: Collects and stores materials from the ileum, begins process of compaction
Appendix: A slender, hollow organ attached to the posteromedial surface of the cecum— primarily associated with the lymphatic system.
The Colon
Larger diameter, thinner walls, features haustra (pouches that permit elongation), teniae coli, omental appendices.
Subdivided into:
Ascending— The section that travels upward from the cecum to the hepatic flexure
Transverse— The section that crosses the abdomen from the hepatic flexure to the splenic flexure
Descending— The section that moves downward from the splenic flexure to the sigmoid colon
Sigmoid Regions— The section that leads from the descending colon to the rectum, storing fecal matter until it is ready to be expelled.
The Rectum
Contains internal and external anal sphincters, controls fecal passage.
Rectal wall distension triggers the defecation reflex.
Histology of the Large Intestine
Abundant goblet cells, lack of villi, mucus-secreting intestinal glands.
Unlike the SI, the LI:
Lacks villi
Has an increased number of goblet cells and deeper intestinal glands
Possesses teniae coli within the muscular layer
Regulation of the Large Intestine
Slow peristalsis and haustral churning in the cecum to transverse colon.
25.8 Accessory Digestive Organs
The Liver
The largest visceral organ, responsible for regulating metabolism, serves as blood resivor , bile production
Divided into left, right, quadrate, and caudate lobes.
Hepatic artery and portal vein supply blood; veins drain it.
Basic unit is the liver lobule, containing portal triads and bile canaliculi.
The Gallbladder
A hollow, pear-shaped, muscular sack that stores and concentrates bile before releasing it to the SI— bile salts aid lipid digestion.
Divided into three regions:
Fundus
Body
Neck
Cystic duct connects it to the bile duct.
The Pancreas
Lies posterior to the stomach, extending laterally from the duodenum toward the spleen
Divided into
Head
Body
Tail
The pancreas is a mixed gland with both exocrine and endocrine functions
Pancreatic duct— delivers exocrine secretions to the duodenal ampulla Exocrine function secretes digestive enzymes, endocrine function produces hormones (insulin, glucagon).
25.9 Aging and the Digestive System
Digestion and absorption remain functional in elderly; however, age-related changes may occur, such as decreased epithelial turnover, changes in smooth muscle tone, and increased cancer rates.