AUBF-lec W2 Intro to Urine
WEEK 2: INTRODUCTION TO URINE
URINE
- A fluid biopsy. It gives an idea what are the metabolic processes happening in the kidney and other organs.
- It is very easy to collect, analyze, and interpret in the organ the sample
- It is an ultrafiltrate of plasma
- Most of the biofluid are considered as ultrafiltrate of plasma
- We can evaluate and monitor our body’s homeostasis and metabolic processes digest through urine examination
- Kidney – Only organ that can be evaluated by such non-invasive means (urine)
URINALYSIS
- According to CLSI, Urinalysis is the testing of urine with procedures commonly performed in an expeditious (mark by speed and efficiency), reliable, accurate, safe, and cost-effective manner (We are only relying on the physical observation of the medtech, reagent strip, and microscope)
- Manual urinalysis procedure: 30 minutes
- Automated urinalysis procedure: 6 minutes
- There are some machines that has microscope inside. Thus, can do microscopic examination or sediment examination and result can be generated on computer
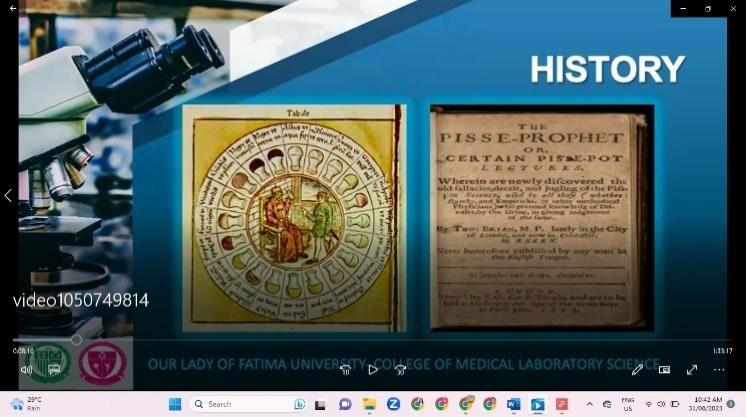
History of Urinalysis
- Analyzing urine was actually the beginning of laboratory medicine.
- References to the study of urine can be found in the drawings of cavemen and in Egyptian hieroglyphics, such as the Edwin Smith Surgical Papyrus.
- They were able to obtain diagnostic information from such basic observations as color, turbidity, odor, volume, viscosity, turbidity, and even sweetness
- Both physical and chemical examination (taste-testing and ant testing)
- Taste-testing – there is a presence of sugar if it is sweet
- Ant-testing – observing whether urine attract ants or not
*** Early physician that
examining the urine and
compare it with bladder-shaped
flasks (found on the shelf) to
know and diagnose the patient’s
disease without seeing the
patient itself.
5th BC | Hippocrates wrote a book on “Uroscopy” |
|---|---|
Middle Ages | Physicians concentrated their efforts very intensively on the “Art of Uroscopy” where urinalysis is included |
1140 AD | Color charts were developed to describe significance of 20 different colors.
|
1627 |
|
1694 |
|
17th century |
|
1827 | Richard Bright introduced urinalysis as part of a doctor’s routine patient examination |
Color chart (Left) and
Pisse-Prophet Book
(Right)
Importance of Urinalysis
- Two unique characteristics of a urine:
- Readily available and easily collected.
- Advantage of urinalysis (normal excreted) unlike other specimen that its collection is invasive (e.g: Blood (Venipuncture, CSF (Lumbar puncture)
- Contains information, which can be obtained by inexpensive laboratory tests (e.g., metabolic function), about many of the body’s major metabolic functions.
- We only rely on Medtech’s skill
- We can have preventive medicine
- Ex: The doctor will ask for glomerular filtration rate test (creatinine clearance), by looking creatinine level in urine, we’ll be able to know whether the kidneys are functioning are well or not
Reasons for performing Urinalysis
- Aiding in diagnosis of disease
- By examining the urine, we screen a particular
- In need of correlation of different result
- Ex: To confirm diabetes mellitus, one will check for the fasting blood sugar and HBA-1C (amount of sugar inside the RBC). We will check the presence of glucose (Chemical Examine); Increase specific gravity and volume/polyuria (Physical Examination)
- Screening asymptomatic population for undetected disorders (especially for metabolic diseases)
- Ex: Inborn errors of metabolism was discovered particularly phenylketonuria due to urinalysis (changes in urine odor – instead of aromatic, it is mousy)
- Monitoring the progress of disease & effectiveness of therapy (to know if treatment is effective)
- Ex: If patient is already taking insulin, the glucose level of urine and blood will be lowered
- A patient is doing dialysis (remove toxic waste in body), the creatinine in urine will be monitored.
*** Creatinine was monitored whether the kidney is functioning well or not. If there is kidney problem, this is low as kidney cannot filter it. Thus, it will accumulate in the blood
- Monitor treatment plan
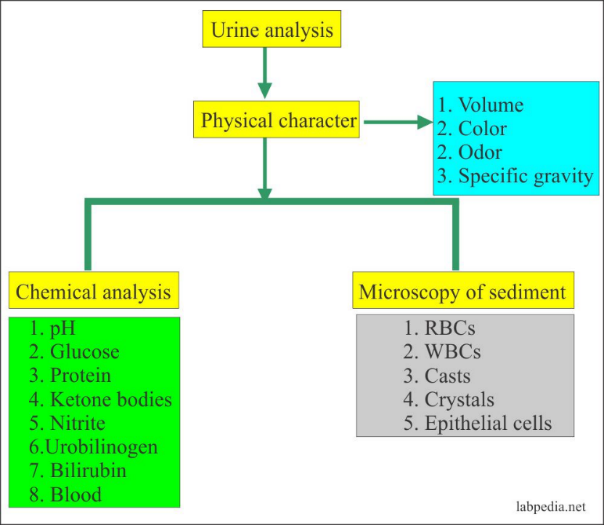
4 Parts of Routine Urinalysis
- Specimen Evaluation - Accept or reject the specimen
- Check for any reason of rejection
- Physical Examination - Check for the physical characteristic of the urine
- Chemical Examination - Detect the presence of different analytes present and serves as a confirmatory for the physical examination
- Sediment Examination – Microscopic.
- It also serves as the gold standard
- It will confirm the result of physical and chemical examination
Example:
Physical Examination: Color is red
Chemical examination: (+) Blood
Sediment Examination: Presence of RBC
*** Should be step-by-step

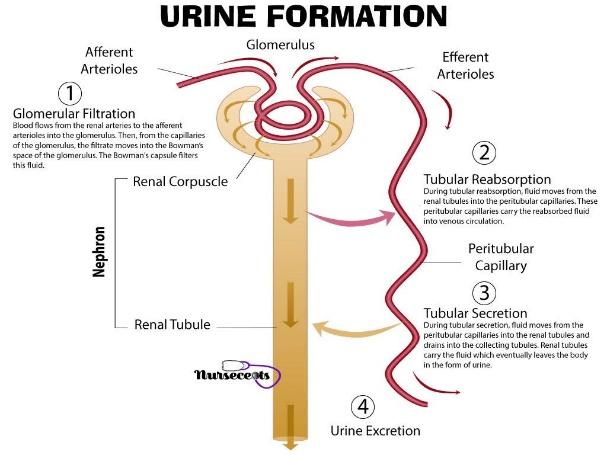
URINE FORMATION
- Filtering the blood/plasma
- Main purpose of kidney is to remove toxic waste, unnecessary substances in blood
- Converts approximately 170,000 mL of filtered plasma to 1,200 mL to 1,500 mL of average daily urine output (each day)
- Normal Urine Output per day: 600-2,000ml
- Plasma is filtered by glomerulus (a capillary found in the kidney used for filtration)
- The kidneys continuously form urine as an ultrafiltrate of plasma
URINE COMPOSITION
- Depend on the diet or hydration of individual)
- Urine will reflect the body’s metabolism
- 95% water + 5% solutes (urine composition of a hydrated person)
- Variation in solute concentration may be due to:
- Dietary intake – Depends on what we are eating
- Sugar is not present in a normal diet as it was being reabsorbed by kidney
- Ex. high sodium and glucose level)
- Physical activity
- Ex. High/extensive physical activity 🡪 high/increase metabolic processes (muscle metabolism)🡪 more biproduct produce (creatinine)
- Body’s metabolism (results to high waste products)
- Endocrine functions
- Production of hormone necessary for urine regulation
- Antidiuretic hormone/vasopressin – water regulation (its release depends to the hydration of individual)
- If patient is hydrated – Low Vasopressin
- If patient is dehydrated – Increase Vasopressin
- Aldosterone – salt regulation
- Body’s position (prolonged standing can cause increase protein due to increase blood pressure making protein was pushed to glomerulus, orthostatic or postural proteinuria)
- Protein are not normally seen in urine
Solutes
Chief Organic Solutes |
|
|---|---|
Chief Inorganic Solutes |
The principal salt of urine is sodium chloride |
Other substances present |
|
Formed elements present |
|
Composition of Urine Collected for 24 hours
Organic Component | Amount | Remark |
|---|---|---|
Urea | 25.0 to 35.0 g | 60%–90% of nitrogenous material; derived from metabolism of amino acids into ammonia |
Creatinine | 1.5 g | Derived from creatine, nitrogenous substance in muscle tissue |
Uric acid | 0.4 to 1.0 g | Common component of kidney stones; derived from catabolism of nucleic acid in food and cell destruction |
Hippuric acid | 0.7 g | Benzoic acid is eliminated from the body in this form; increases with high vegetable diets |
Other substances | 2.9 g | Carbohydrates, pigments, fatty acids, mucin, enzymes, hormones; depending on diet and health |
Inorganic Component | Amount | Remark |
|---|---|---|
Sodium chloride (NaCl) | 15.0 g | Principal salt; varies with intake |
Potassium (K) | 3.3 g | Occurs as chloride, sulfate, and phosphate salts |
Sulfate (SO4 2) | 2.5 g | Derived from amino acids |
Phosphate (PO4 3) | 2.5 g | Occurs primarily as sodium compounds that serve as buffers in the blood |
Ammonium (NH4) | 0.7 g | Derived from protein metabolism and glutamine in kidneys; amount varies depending on blood and tissue fluid acidity |
Magnesium (Mg2) | 0.1 g | Occurs as chloride, sulfate, phosphate salts |
Calcium (Ca2) | 0.3 g | Occurs as chloride, sulfate, phosphate salts |
- To determine whether a fluid is urine, components of the specimen (creatinine, urea, sodium, and chloride) as they are significantly higher in urine than in other body fluids. Protein and glucose are not present in a normal urine specimen
- Oliguria, a decrease in urine output (less than 1 mL/kg/hr in infants, less than 0.5 mL/kg/hr in children, and less than 400 mL/day in adults
- Anuria, cessation of urine flow, may result from any serious damage to the kidneys or from a decrease in the flow of blood to the kidneys
- Nocturia is an increase in the nocturnal excretion of urine
- Polyuria, an increase in daily urine volume (greater than 2.5 L/day in adults and 2.5 to 3 mL/kg/day in children)
SPECIMEN HANDLING
- Urine specimen is so readily available and easily collected often leads to laxity in the treatment of the specimen after its collection.
- Changes in urine composition take place not only in vivo but also in vitro
- Requiring correct handling procedures
SPECIMEN INTEGRITY
- Maintain integrity by proper handling and preservation
- Specimens should tested within 2 hours
- A specimen that cannot be delivered and tested within 2 hours should be refrigerated or have an appropriate chemical preservative added.
- Notice that most of the biochemical changes are related to the presence and growth of bacteria
- Urine that passes through the urethra is no longer sterile due to normal flora
- Some bacteria utilizes some substances present in urine (ex: glucose)
- Urine is still sterile if it is still in kidney to urinary bladder)
Changes in Unpreserved Urine
ANALYTE | CHANGE | CAUSE |
|---|---|---|
Color | Modified/darkened | Oxidation or reduction of metabolites |
Clarity | Decreased | Bacterial growth and precipitation of amorphous material (Ex: amorphous urates and amorphous phosphate) |
Odor | Increased ammonia smell | Bacterial (contains urease enzyme) multiplication causing breakdown of urea to ammonia |
pH | Increased (alkaline) | Breakdown of urea to ammonia by urease-producing bacteria/loss of CO2 |
Glucose | Decreased | Glycolysis and bacterial use |
Ketones | Decreased | Volatilization and bacterial metabolism |
Bilirubin | Decreased | Exposure to light/photo oxidation to biliverdin |
Urobilinogen | Decreased | oxidation to biliverdin |
Nitrite | Increased | Multiplication of nitrate-reducing bacteria |
Red and white blood cells and casts | Decreased | Disintegration/lyse in dilute alkaline urine |
Bacteria | Increased | Multiplication |
Trichomonas | Decreased | Loss of motility, death |
- Urobilin gives the specific dark color of the urine
- Unpreserved urine has dark color and contains dust or chalk-like (amorphous material) at the bottom of the container
- Unpreserved urine forms crystal called Ammonium Biurate also known as thorny apple
SPECIMEN PRESERVATION
- Most routinely used method of preservation:
- Refrigeration (2⁰C to 8⁰C)
- During transport, ice box must be 2⁰C to 10⁰C
- If there are no ice box, chemical preservatives may be used
- Decreases bacterial growth and metabolism
- There is no best preservative. One must choose a preservative depending on what is wanted to test and to preserve
- There is no single preservative that can preserve all components of urine
URINE PRESERVATIVES
Preservatives | Advantages | Disadvantages | Additional Information |
|---|---|---|---|
Refrigeration |
|
|
|
Thymol |
|
| -- |
Boric Acid |
|
|
|
Formalin (formaldehyde) |
|
|
|
Toluene |
|
| -- |
Sodium fluoride |
|
|
|
Phenol |
|
|
|
Commercial preservative tablets |
|
|
|
Urine Collection Kits4 (Becton, Dickinson, Rutherford, NJ) |
| -- | -- |
Gray C&S tube |
|
|
|
Yellow plain UA tube |
|
|
|
Cherry red/yellow top tube |
|
|
|
Saccomanno Fixative |
| -- |
|
- Saccomanno Fixative is used for histopathological studies that is a combination of alcohol and carbo wax.
- When observing cancer cells, abnormal epithelial cells such bladder cells, renal tubular epithelial cells – irritation in renal tubules that indicates kidney disease when seen in significant amount since renal tubules are not normally shed
- We can use commercially prepared transport tubes but we need to make sure that
- It should not be bactericidal (it must be bacteriostatic)
- It should inhibit urease (To avoid the conversion of urea to ammonia)
- Preserved the formed elements
- It should not interfere with the chemical test
SPECIMEN COLLECTION
- Urine (biohazardous substance) Standard Precautions
- Clean, dry, leak-proof, disposable containers
- Sterile containers for culture and sensitivity (Lid has seal)
- Check the requisition for
- Properly applied screw-top lids
- Wide mouth (4 to 5 cm), flat bottom
- Clear plastic (50 mL to 100 mL capacity)
- 12 mL microscopic
- Repeat analysis
- There should be room for swirling
- Usually require the patient to submit at least 10-15ml or average of 12ml of urine (for the routine examination)
- There should be an extra amount for repeat or additional testing
- Usually ½ or ¾ of the container (usually 30 -35ml)
Specimen Label
- Patient’s name
- Identification number (if hospital-based)
- Date and time of collection (to make sure urine is fresh; prolonged urine must be rejected)
- Patient’s age and location (room number)
- Physician’s name (optional)
- Others (as required by institutional protocol)
- Attached to the body of the container, not to the lid
- Should not become detached if the container is refrigerated or frozen
*** Compare with requisition form
*** Patient are the one who label urine container
*** if unlabeled or mislabeled, reject
*** Label immediately after collection; do not pre-label as it prone to mislabeling
Requisition Form
- Requisition form (manual/pen and paper or computerized)
- Pen and paper is not used nowadays especially in tertiary hospital as they now have Laboratory Information System
- Match the information on the specimen label
- Additional information on the form (check the note of physician):
- Method of collection (ex: suprapubic aspiration for culture and cytology studies. Be careful as it is very invasive)
- Type of specimen – it depends on the type of specimen of what will be the test (ex: first morning for glucose monitoring)
- Interfering medications – there are some drugs which causes changes (physical, color/ pigment, chemical examination) with the urine. (ex. Ascorbic Acid causes false-negative results in certain parameters in chemical examinations)
- Patient’s clinical information
- Time specimen is received in the laboratory -Take note, not just the time that the urine is being collected, but also the time it is received in the laboratory.
Specimen Rejection
- Unlabeled containers
- Theoretically speaking, if the specimen is labeled at the lid of the container, we reject it.
- Nonmatching labels and requisition forms
- Specimens contaminated with feces or toilet papers
- Containers with contaminated with contaminated exteriors.
- Specimens of insufficient quantity
- Depends on the patient’s condition (ex. The patient has kidney stone or kidney tumor, expect that the patient will not provide enough urine volume. In those cases, we can accept the specimen)
URINE CONFIRMATION
***Sometimes, we doubt if the urine submitted is true or not. We can confirm it through the parameters listed below:
Parameter | |
|---|---|
Specific Gravity | 1.003-1.035 |
pH | 4.0-8.0 |
Temperature | 32.5oC to 37.5oC |
Creatinine | Approximately 50x more than that of plasma |
- The normal specific gravity of the urine is 1.003-1.035, but in some textbook, 1.002 is still considered as urine. This instance may possibly happen if the patient has diabetes insipidus. If it became 1.000, the specimen submitted is a distilled water not urine.
- pH should be between 4.0-8.0. It should not be too much acidic or too much alkaline, if so, the specimen might be adulterated.
- Temperature of the urine should be near the body temperature. Freshly voided urine should be warm to touch.
- Creatinine is normally seen in the urine because it is a metabolic byproduct of the muscle. It is a toxic waste product of our body. Urine creatinine should be 50x more than the plasma creatinine so, creatinine should not accumulate in our body.
- If creatinine in urine is lower than the creatinine in blood, this means that glomerular filtration rate or the kidney function has been affected hence, kidney disease.
- If creatinine in urine is higher than that in blood, the toxic product is not secreted, we have to do dialysis. That’s why toxic products like urea and creatinine should not accumulate in our body.
TYPES OF URINE SPECIMEN COLLECTION
*** The type of urine specimen that we use depends on what is the test to be done.
*** The three basic types of urine specimen; first morning, random, and timed specimen.
Random Urine
- Most commonly received specimen because of its ease of collection and convenience
- If you want to do screening test you can use random urine. There is no preparation needed before collection. It may be collected at any time, but the actual time of voiding should be recorded.
- Useful for routine screening tests to detect obvious abnormalities
- This type of urine specimen can be used for routine screening test or if you want to detect abnormalities (ex. If you have diabetes mellitus, even in random urine the specific gravity and glucose is increased
- The problem here is there is a physical activity before the collection it is possible to have abnormal results
- Dietary intake before collection will also reflect with the result
First Morning Urine
- Ideal screening specimen
- Also known as the 8-hour specimen.
- If you wanted to observe formed elements and analytes that may not be present in the random urine, then you can use first morning urine because this is the most concentrated.
- Remember that first morning urine will reflect all the metabolism that happen a day before the collection.
- We instruct our patient to collect the specimen immediately upon arising, then deliver it to the laboratory within 2 hours.
- Preventing false-negative pregnancy tests and for evaluating orthostatic proteinuria
- This specimen is useful in ensuring the correct result for pregnancy test to detect enough Hcg level.
- This is also useful in evaluating orthostatic proteinuria. We have two types of proteinuria: orthostatic and true proteinuria. True proteinuria is clinically significant while orthostatic is a postural proteinuria (prolong standing). To differentiate check the random urine and the first morning urine, if true proteinuria both random and first morning is positive while in orthostatic proteinuria it is positive only in random urine.
Fasting Specimen (Second morning)
- A fasting specimen differs from a first morning specimen by being the second voided specimen after a period of fasting.
- This specimen will not contain any metabolites form food ingested before the beginning of the fasting period
- but if you want to check the metabolites from the food before the beginning of the fasting use the first morning specimen instead. (ex. You fasted at 8 pm and your urine will be tested at 6 am, before 8 pm if you wanted to check the metabolites before fasting use first morning urine)
- It is recommended for glucose monitoring
2-hour Postprandial Specimen
- Specimen is tested for glucose, and the results are used primarily for monitoring insulin therapy in persons with diabetes mellitus
- A more comprehensive evaluation of the patient’s status can be obtained if the results of the 2-hour postprandial specimen are compared with those of a fasting specimen and corresponding blood glucose tests.
- Literally, 2 hours after eating you have to check for the glucose level. Usually, done in patients who are taking insulin injection. (ex. The patient eats and inject insulin, then we will check whether the insulin therapy is effective. After injecting insulin, the glucose level should decrease that way we can tell the effectiveness of the said therapy).
Glucose Tolerance Specimens
- The urine is tested for glucose and ketones, and the results are reported along with the blood test results as an aid to interpreting the patient’s ability to metabolize a measured amount of glucose and are correlated with the renal threshold for glucose
- Collection of these specimens is an institutional option
- Tested alongside with the blood. For the blood we have what we call Oral glucose Tolerance Test (OGTT) wherein we have multiple collections of fasting blood (1-hour, 2-hour, 3-hour specimen). In OGTT, the patient will be instructed to drink glucose solution to detect gestational diabetes. In every hour you have to collect blood and aside from the blood you should also collect urine. Then, we monitor if the glucose decreases or not.
- It is optional to do urine glucose tolerance test, it is more commonly done with blood (OGTT).
Timed Specimens
- Measuring the exact amount of a urine. A carefully timed specimen must be used to produce accurate quantitative results
- It is a basic type of urine specimen so, if you wanted to quantify certain solute (i.e., organic solutes; urea, creatinine), we use timed specimen.
- Be careful in timing the specimen to provide accurate quantitative result.
- Required when the concentration of the substance to be measured changes with diurnal variations and with daily activities such as exercise, meals, and body metabolism.
- This is used specially for some of the solute which exhibit diurnal variations such as steroids, catecholamines, electrolytes, etc. Meaning they are higher in the morning and lower in the afternoon
- 4 types of timed specimen
- 24-hour – if you want to identify the solutes present
- 12-hour – for Addis count
- 4-hour – nitrite determination (this is the time required for the nitrate to be reduced to nitrite by nitrate reducing bacteria) (nitrite is used for the evaluation of UTI)
- Afternoon urine – for urobilinogen (specifically collected at 2-4pm because urobilinogen is acid labile and during the afternoon our body experiences alkaline tide)
24-Hour (Timed) Urine Specimen Collection Procedure |
|---|
|
Common Errors Associated With Timed Urine Collections |
|---|
|
Catheterized Specimen
- The most commonly requested test on a catheterized specimen is a bacterial culture.
- If a routine urinalysis is also requested, the culture should be performed first to prevent contamination of the specimen.
- Ex. You received a urine sample, it is written in the requisition form that you threw routine urinalysis, and culture and sensitivity, the sample should be given to the bacteriology section to avoid contamination.
- A less frequently encountered type of catheterized specimen measures functions in the individual kidneys. Specimens from the right and left kidneys are collected separately by passing catheters through the ureters of the respective kidneys.
- TWO TYPES
- Urethral – goes from the urethra up to the urinary bladder. Usually done when patient have UTI, and cystitis.
- Ureteral – goes up to the urinary bladder. Usually done when the patient has pyelonephritis (a progressive disease if cystitis left untreated). Ureteral is also used to locate where is the infection (left or right kidney)
Midstream Clean-Catch Specimen
- Less contaminated by epithelial cells and bacteria and, therefore, is more representative of the actual urine than the routinely voided specimen. Patients must be provided with appropriate cleansing materials, a sterile container
- Less invasive than catheterized specimen, if you wanted to do culture and sensitivity. This is safer and less traumatic method for obtaining urine. The problem is we compare it to suprapubic and catheterized specimen, it contains a little bacteria and cells, not totally free from bacteria and epithelial cells.
- To collect, the patient needs to catch the mid portion of the urine. The first portion should be discarded because it has the greatest number of bacteria and cells which can cause false-positive result
- Strong bacterial agents, such as hexachlorophene or povidone-iodine, should not be used as cleansing agents.
- Mild antiseptic towelettes are recommended (Castile Soap Towelettes)
- In collecting this specimen, you need to cleanse the urethra opening both male and female using towelettes. Towelettes should be free from bacterial agents, remember we just need to cleanse the area not kill microorganisms
Clean-Catch Specimen Collection: Female Cleansing Procedure |
|---|
Instruct the patient to:
|
Clean-Catch Specimen Collection: Male Cleansing Procedure |
|---|
Instruct the patient to:
|
Suprapubic Aspiration
- Aspiration provides a sample for bacterial culture that is completely free of extraneous contamination.
- Most invasive, if you want to collect sterile urine. There are two ways to do this: suprapubic and catheterized
- If the patient has seizures it is better to use suprapubic but, if the patient is unconscious it is better to use catheterized specimen.
- Make sure that the specimen collected does not have extraneous contamination because this sample is also used in bacterial culture as well.
- To collect, guided by an ultrasound machine, the doctor will insert directly, puncturing the urinary bladder.
- The specimen can also be used for cytologic examination
Prostatitis Specimen
***It is used to evaluate whether a male patient has infection in his prostate gland
- Three-Glass Collection (most commonly used)
- Quantitative cultures are performed all specimens, and the first and third specimens are examined microscopically.
- In here, we have to collect three urine samples: glass 1, glass 2, and glass 3. Glass 1 is a random urine voided pre-massage. Glass 2 is the control where we will need a midstream clean-catch (for UTI). Glass 3 is for the post- massage.
- In prostatic infection, the third specimen will have a white blood cell/high-power field count and a bacterial count 10 times that of the first specimen. Macrophages containing lipids may also be present.
- To examine, the 3 glasses will be cultured. Then, the first and the third specimen should be examined microscopically to detect if there is a presence of bacteria and WBC. If glass 3 has 10x higher bacteria and WBC, then it is prostatitis.
- If 2nd glass has growth, then the patient has UTI. However, there are instances where glass 2 and 3 are both positive, this is still not considered as prostatitis because we don’t know if the growth is caused by UTI or prostatitis
- Stamey - Mears four-glass localization method
- Initial voided urine (VB1)
- midstream urine (VB2)
- expressed prostatic secretions (EPS)
- Post-prostatic massage urine specimen (VB3)
- In here, we added the expressed prostatic secretions (EPS) from the prostate gland.
- Using the three-glass specimen, there are instances that we cannot differentiate UTI from prostate gland.
- EPS does not have urine, it’s just prostatic fluid. So, if the patient has prostatitis, WBC and bacteria will be seen in high numbers in EPS followed by the VB3 which will then be followed by either VB1 or VB2. If the patient has UTI, WBC and bacteria will be seen highest in VB2 followed by VB2, then VB3 and less in EPS.
- We only perform 4-glass if he 3-glass gives off inconclusive results, by doing this we can now determine whether the problem is in the prostate or not.
- Pre- and post-massage test (PPMT)
- A positive result is significant bacteriuria in the post-massage specimen of greater than 10 times the pre-massage count
- Also known as the Two-glass method.
- In PPMT, we have to check the bacteria and WBC of the pre-massage and post massage
- If the patient has prostatitis, WBC and bacteria will increase 10x higher at the post massage.
Drug Specimen Collection
- most vulnerable part of a drug-testing program.
- The chain of custody (COC) is the process that provides this documentation of proper sample identification from the time of collection to the receipt of laboratory results.
- We have to follow the COC starting from the collection up to the releasing of the result. The client must be accompanied by the drug test analyst during the collection. There’s also a medical review officer to confirm information.
- that no tampering of the specimen occurred, such as substitution, adulteration, or dilution.
- Even one drop of water, can cause false-negative result in drug testing. It also requires free skin to inspect if the client has an adulterant. Usually, collection room are waterless but if they do the water may contain bluing agent. In here, we usually check for methamphetamine (shabu) and Tetrahydro cannabinol (marijuana)
- Witnessed or unwitnessed
- Witnessed: drug suspects
- Volume: 30-45 mL (excess urine will be used for confirmatory)
- Temperature: 32.5oC to 37.5oC
- It is better to use fresh urine than the aged one.
Urine Drug Specimen Collection Procedure |
|---|
|