Chapter 1
Pharmacology: study of the actions of drugs and their effects on a living organism.
Neurpharmacology: study of drug-induced changes in nervous system cell functioning. Study of drug actions and their effects on living organisms.
Psychopharmacology: emphasizes drug-induced changes in mood, thinking, and behaviour.
Neuropsychopharmacology: identifies chemical agents that act on the nervous system to change behaviour affected by injury, disease, and environmental factors.
Psychoactive drug: a chemical substance that crosses the blood-brain barrier and acts primarily upon the CNS, where it alters brain function, resulting in changes in behaviour.
Drug Action: specific molecular changes produced by a drug when it binds to a particular target site or receptor.
Drug Effects: Alterations in physiological or psychological functions associated with a specific drug.
Textbook
Placebo Effect
Placebo: A Substance that is pharmacologically inert, yet in many instances produces both therapeutic and side effects.
Belief in a drug may produce real physiological effects despite the lack of chemical activity.
Such as: gastric acid secretion, blood vessel dilation, and hormonal changes.
Double-blind experiment: Type of experiment in which neither the patient nor the observer knows the treatment received by the patient.
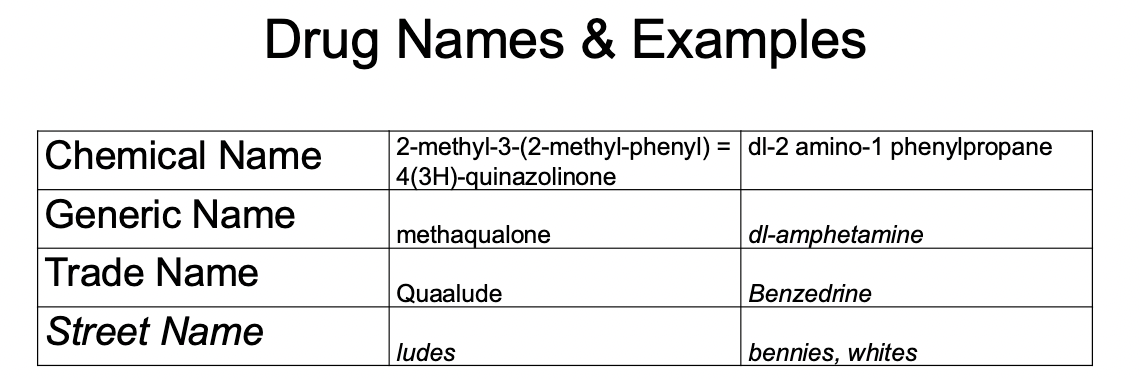
Four Names of Drugs
The chemical name
identifies the drug molecules and how they are joined together.
derived from organic chemistry.
e.g., 7-chloro-1,3-dihydro-1-methyl-3-phenyl-2H-1,4-
benzodiazepin-2-one
Generic/Nonproprietary Name
official legal name of the drug
resembles the chemical name
conventions: barbiturates end in -al (e.g., secobarbital); local anesthetics and in -caine (e.g., procaine)
First letter is not capitalized (e.g., diazepam)
e.g., SKF 10,47 or RU 486
Trade/Brand Name
aka: brand name or proprietary name
describes the formulation (active ingredients & excipients)
used by the medical profession (e.g., Valium, Prozac; first letter capitalized)
patented
One drug can have many different trade names (after the patent expires), and other drug companies can sell it.
active ingredients in the drug.
different fillers (colour)
Street Name
Unofficial/slang name applied by users
many
regional and temporal
cannabis/marijuana — weed, boo, gigglewee, mu, hemp, kif, ganga, pot
Oxycotin= oxies, Percocets= percs
MDMA= E
Classification by Behavioural Impact
Psychoactive Drugs
CNS stimulants: Amphetamine, cocaine, nicotine
Produce increased behavioural arousal, alertness, and sense of well-being in the individual.
CNS depressants: Barbiturates, alcohol,
include a variety of drugs that depress CNS function and behaviour to cause a sense of relaxation and drowsiness.
Some of the sedative-hypnotics are useful for their sedating qualities and for their ability to induce sleep.
Analgesics: Morphine and codeine
frequently have CNS-depressant qualities, although their principal effect is to reduce the perception of pain.
The most important drugs in this class are the narcotics.
Narcotics, or opiates, such as morphine or codeine, are derived from the opium poppy; the synthetic narcotics (sometimes called opioids) include heroin, meperidine (Demerol), methadone, and fentanyl.
Hallocinogenics: Mescaline, LSD, and psilocybin
are examples of hallucinogenic drugs that alter an individual's perception, mood, and cognitive processes.
Psychotherapeutics: Prozac, Throazine.
Used to treat clinical disorders of mood or behaviour.
Dosage
Drug effects are related to drug concentration in the body, not just dosage.
One focus of the course = factors that change the relationship between dosage and drug concentration in the body.
Dosages are prescribed based on body weight (mg/kg).
mg/kg methods account for factors such as body composition and metabolic rate.
Dosage Response Curve (DRC)
Graph is used to display the amount of biological change in relation to a given drug dose.
Describes the extent of biological or behavioural effect (response in population) produced by a given drug concentration (dose).
A graph of the degree of drug response as a function of dosage
range from no effect to the highest effect
horizontal axis (x) =dose
vertical axis (y) =effect
e.g., the effect of alcohol on the rate of speech
When plotted on a semi-log scale, the curve takes on a classic S-shape. At low doses, the drug-induced effect is slight because very few receptors are occupied. As the dose of the drug is increased, more receptors are occupied, and a greater biobehavioral response occurs.
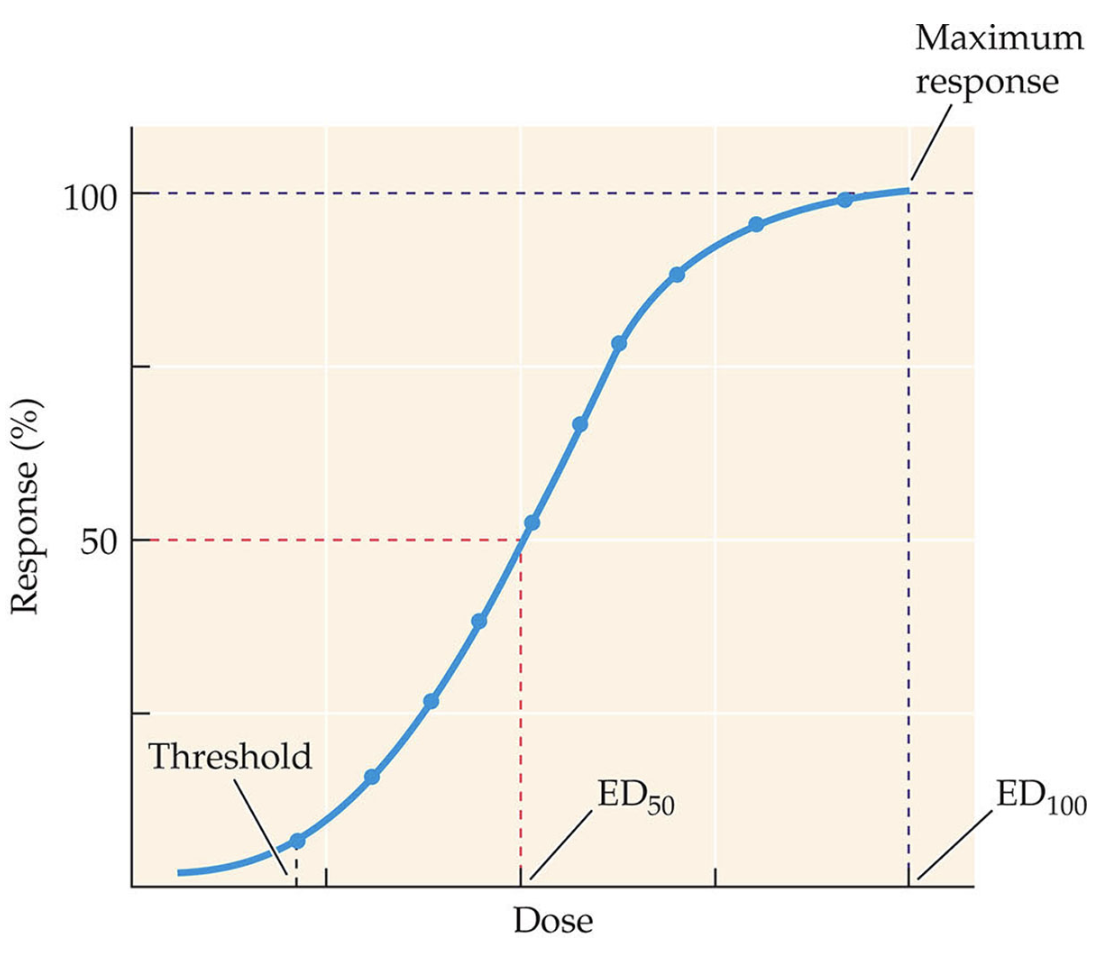
Dose Effect Curve
(sometimes also called the Does Response Curves)
required when a binary response variable is used
example, does aspirin completely stop a headache? (yes/no)
plot the percentage of each dosage group experiencing the given effect
ED 50 -median effective dose (effective in 50% of people)
LD 50 -median lethal dose (lethal in 50% of the population); usually based on animal research
TD 50 -median toxic dose(toxic in 50% of the population); provides crucial information for assessing the safety margin of a drug compared to its effectiveness.
Hyperreactors and hyporeactors are terms used to describe individuals who exhibit varying responses to a drug, where hyperreactors require lower doses for an effect, while hyporeactors need higher doses, complicating the understanding of individual dose-response relationships.
women who are pregnant, ethnicity, genes, and age.
e.g., caffeine can have differing effects based on these factors, with some individuals experiencing heightened sensitivity leading to adverse effects at lower doses. ‘
Drug Saftey
(uses dose-effect curves)
safer when LD is far from ED
Therapeutic Index (TI) = LD 50/ ED 50
Higher TI means a safer drug
Examples 1) LD 50 =100, ED 50 =5
2) LD 50 =100, ED 50 =50
also: TI -TD 50/ED 50
Therapeutic drug monitoring protocols
Potency vs. Effectiveness
Describe the extent of a drug’s effects
Potency
A more potent drug has a lower ED 50
More potent drugs require less of the drug for the effect (but not necessarily clinically relevant) & likely have a greater affinity for the drug receptor.
Cheaper, safer, fewer side effects
Effectiveness
The drug that has the highest maximum effect is more effective
Primary Effect vs. Side Effect
Primary/Main/Therapeutic Effects
The effect for which the drug is taken.
Side Effects
Any other drug effects (harmful or beneficial), harmful effects = adverse effects.
Non-specific Drug Effects
Effects not due to the chemical activity of the drug but due to the person’s background (e.g., drug history), expectations, perceptions, attitudes, and other factors.
Placebo: expectations, but not because of the drug
Drug Interactions (Combining Drugs)
Agonistic- shifts the ED50 to the right; reduces the effect
Drug A, causes drug B to have less of a particular effect.
Naloxone antagonizes the effects of opioid
competitive antagonists; both drugs are trying to act on the same receptor.
non-competitive antagonists differ in that they reduce the effect of an agonist regardless of the concentration of the agonist at the receptor, often by binding to a different site on the receptor.
Competitive Antagonists:
A drug that binds to a receptor but has little or no efficacy. When it competes with an agonist for receptor sites, it reduces the effect of the agonist.
Naloxone on the analgesic effect of morphine. Naloxone can be overcome by increasing the amount of morphine administered.
Noncompetitive antagonists:
Drugs that reduce the effect of an agonist, but do not compete at the receptor site.
The drug may bind to an inactive portion of the receptor, disturb the cell membrane around the receptor, or interrupt the intercellular processes initiated by the agonist-receptor association.
Additive/Agonistic — drugs that have similar/equivalent effects; effects are higher than from either drug alone.
20 mg drug A + 20 MG DRUG B =40 mg drug A
Superaddtive
shifts the Ed50 to the left, but the resultant effect is greater than the simple sum of the two drug effects (e.g., aspirin & phenytoin)
aka —potentiation; often involves pharmacokinetic effects (competition for depot binding - come back to this later).
Antagonists
Competitive antagonists —The 2 drugs compete to bind to the same receptors (e.g., naloxone & heroin).
Important tools in pharmacology
Noncompetitive antagonists —2 drugs do not compete to bind to the same receptor, but one drug impairs the binding of the other drug in another way.
Physiological antagonism —2 drugs have different mechanisms of action (not the same receptor), but they reduce each other’s effectiveness.
Lecture 2
Outline
Pharmacokinetics
Routes of administration
Absorbtion
Distributioon
Metabolism (Liver)
Elimination/Excretion (Kidneys)
Administration: What happens after the administration of a particular drug dose that leads to individual differences in the Drug Effects?
Pharmacokinetics and pharmacodynamics contribute to variability in the relationship between drug dose and response.
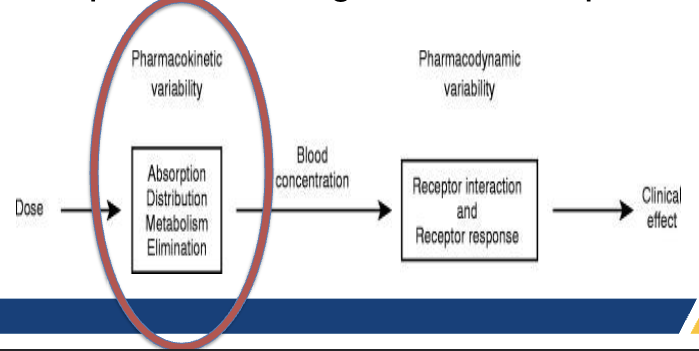
Pharmacokinetics:
Factors that contribute to the administration, absorption, distribution, inactivation/metabolism, and excretion of a drug.
Site of Action
Specific and limited places in the body where the drugs have been absorbed.
Routes of Administration
Methods used to get a drug from the outside of the body to some place under the skin.
Paternan:
Injections (IV, IM, IP, SC)
Inhaltion
Gases
Smoke and solids
Transdermal
Enteral: Gastrointestinal tract
Oral
Rectal
Injection Routes of Administration
Injection through the skin into different parts of the body using a hypodermic needle.
Vehicle
The liquid used to dissolve a drug so that it can be injected
Normal or physiological saline (0.9% sodium chloride)
Bolus
Small bubble of a drug and vehicle at the point of injection
Advantages
Simpler, unconscious, combative, not willing (naloxone), fast acting.
Disadvatages
Too much administered, overdose, infection, phobias.
Subcutaneous (s.c.)
Injection right under the skin (arm, thigh).
Hormonal contraceptives (Arm implant)
Intramuscular (i.m.)
Depot injections (anti psychotics) diffuse slowly out of the muscle, long acting.
Bigger muscles, slower absorption.
Antibiotics, biological (vax), hormones
Intraperitoneal (i.p.)
Paritanium (liver, spleen, intestines)
Used in animal research
Intravenous (i.v.)
The drug is injected directly into the bloodstream.
No fast pass metabolism
Other special injection methods:
intrathecal, intraventricular, intracranial, epidural, infusion pump under scalp, viral vectors (future).
Intercranial
Epidural
Ceriberal spinal
Directly into the brain
Infusions pump
Brain infection
Viral vectors
gene therapy, injects viruses that contain DNA to encode certain protein.
Absorption from Injection Sites (Stages)
Absorption affected by:
volume of blood flow to an area
exercise
temperature
R Heart —> Arteries —> Capillaries —> Veins —> L Heart
Capillaries
permeates most body tissues because it allows nutrients and oxygen to get to different parts of the body.
drugs get into the bloodstream through capillary walls throuhg diffusion.
Inhalation of Gases -bypassing first pass metabolism
The body has a good system for taking oxygen from the air and distributing it quickly through the circulatory system.
Lungs
Large surface area; large # capillaries
Inhaled gases are directly absorbed through capillary walls and transported to the heart and brain.
A main artery goes from the heart to the brain.
Diffusion (controls dosage)
Inhalation of Smoke & Solids
Burn material and inhale active materials in the smoke or aash
Drugs dissolve on the moist surfaces of the lungs and diffuse into the blood (e.g., tobacco smoke). Nicotine dissolves on the moist surfaces of the lungs, then diffuses into the blood.
Vaping is considered an aristol??
Transdermal Administration
Epidermis
layer of skin that is the main barrier to absorption
packed with keratin
only penetrated by lipid-soluble substances (dissolve easily in lipids or fat).
Methlyphenidate (Treat ADHD)
E.g., nicotine patch, hormonal contraceptive patch, HT, hormone patches for menopause, anti-depressant patches.
for small lipophillic (dissolves in fat) miolecules that can passively diffuse trhough skin.
Transdermal vaccination delivery (pandemics)
Ultrasound-enhanced transdermal delivery (to increase pore size of skin).
Topical
Applied to mucous membrane (eyes, oral cavity, ears, nasopharynx, vagine, colon, urethra, rectum).
buccal membranes of the mouth (into the blood) (floor of the mouth, cheeks, gums/gingiva, palatal mucosa, lining of the lips).
Faster effect, doesn’t pass through metabolism.
Intranasal administration
tobacco snuff, cocaine, nicotine spray
lungs or mucous membranes to the blood or the digestive system
Enteral Routes
Rectal Administration
Suppositories can be placed in the rectum and are absorbed into the blood through the digestive system.
Can avoid some first-pass metabolism
Lower rectum - drug goes into the portal vein (goes to the liver before general circulation).
Upper rectum - drug goes into the portal vein (goes to the liver before general circulation).
Oral Administration
P.o. peroral
digestive system (stomach, intestines best absorbs the drug)
Related routes
Intranasal can get into the digestive system
Buccal membranes of the mouth (into the blood)
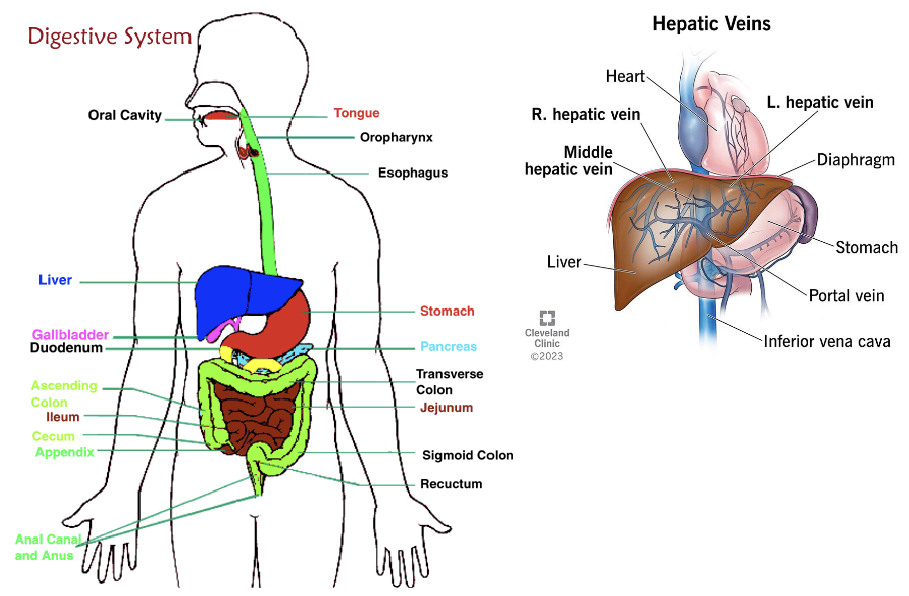
First Pass Metabolism: blood circulation from the GI tract goes directly to the liver (via portal vein) before going to the blood that supplies the body and brain; due to enzymes in the GI tract and hepatic portal system, the oral route results in lower drug levels eventually reaching the brain.
The Digestive System
intestines are lined with capillaries to absorb nutrients from food.
The faster the drugs get to the intestines = the faster absorption
Most drugs are not fully absorbed until they reach the small intestine.
Lipid barrier between food (or frug) and blood (i.e., cell membranes)
A drug passes through the cell membrane to get into the blood.
Lipid solubility
determines absorption and speed of entry into the blood and brain
measured by the oil/water partition coefficient
Factors that determine lipid solubility
properties of the drug
degree of ionization (electric charge) (ions are not lipid soluble)
pH
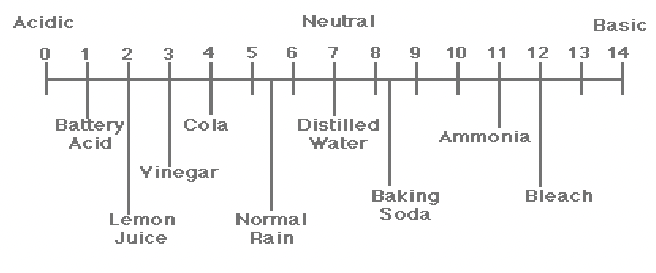
pH is important to understand as pH (of the drug, the digestive system, and the blood) affects ionization, lipid solubility, and rates of absorption.
Determinants of Ionization
1) pH of solvent (is the drug dissolved in acid or base?)
2) whether the drug is a weak acid or a weak base
3) pKa of the drug
The pH at which half of its molecules are ionized
drugs are generally more ionized in a solvent with an opposite pH (e.g., acids are more ionized in basic/alkaline solutions; bases are ionized in
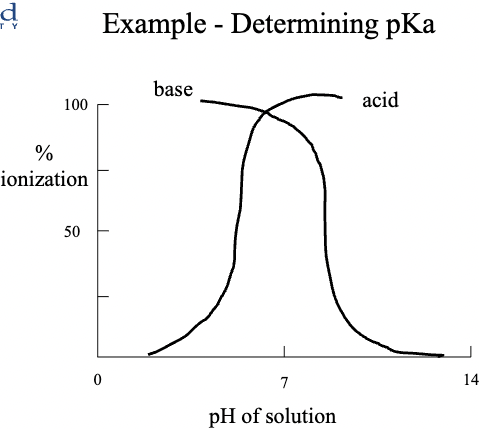
The percentage of ionization determines the rate of absorption.
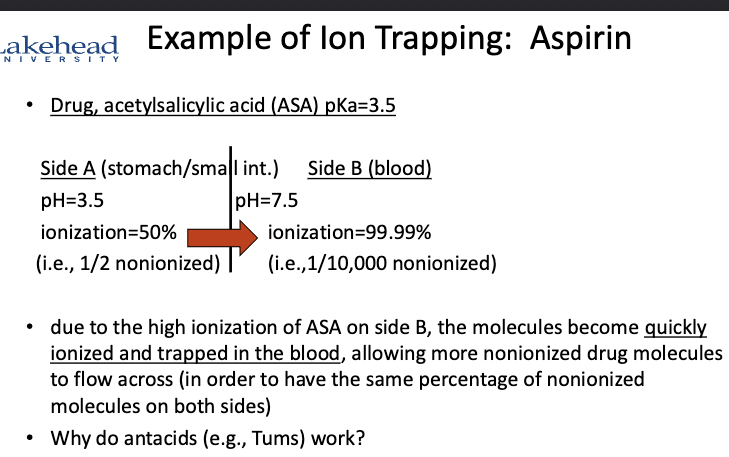
Ion Trapping
The tendency for acidic drugs to get trapped on the basic side of the membrane and basic drugs to get trapped on the acidic side of the membrane.
Only nonionized molecules can diffuse through the membrane (until equal concentration on both sides)
Drug Distribution
Where the drugs go in the body
Concentrated in places with the highest blood flow (heart, brain, kidneys, liver)
Factors Affecting
1./ Lipid Solubility
Highly lipid-soluble drugs tend to concentrate in the lipids (body fat), are inactive, released slowly.
Cannabis can test positive on a drug test a month later.
Water-soluble drugs concentrate in body water.
Most drugs are inactive when in body fat.
2./ Active & Passive Trasport
Passive transport mechanisms
a non-lipid soluble molecule may attach itself to a molecule that readily diffuses across the membrane 9high to low)
Active transport mechanisms
works against normal diffusion
energy expended to move molecules from low to high concentrations.
Drug receptors are often on the outside of cells (hormone receptors are inside cells).
3./ The three Barriers:
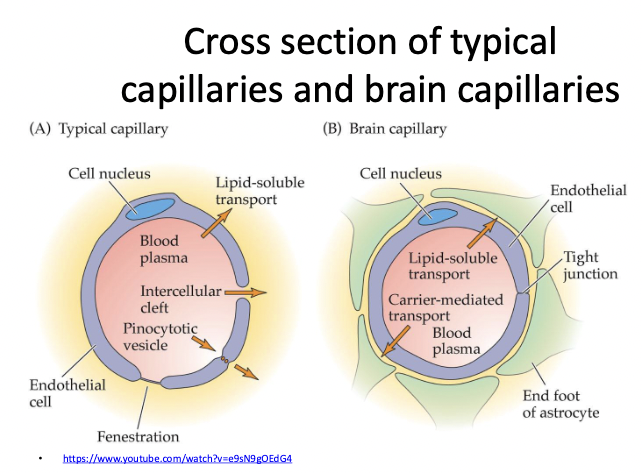
Blood Brain Barrier:
Special cells in the CNS that wrap themselves around capillaries and block the pores through which drugs normally diffuse; selectively permeable.
Placental Barrier
Lipid-soluble drugs cross more easily
Fetuses’ blood levels of all drugs reach 75-100% of the mother’s in 5 min.
Generally, all psychoactive drugs will be present in featu’s blood supply
Depot or Protein Binding (e.g., albumin)
Large protein molecules in blood cannot diffuse through capillaries
Some drugs bind to them and cannot exert while bound
drugs also bind to muscle fat (inactive sites = depot sites) (e.g., THC)
Individual differences in depot binding account for differences in sensitivity to drugs
Protein binding can cause drug interactions (anticonvulsant phenytoin binds to proteins, but aspirin binds more readily and displaces it, raising phenytoin blood levels).
Placental Barrier
Generally, all psychoactive drugs will be present in the fetus at a concentration similar to that in the mother’s bloodstream.
Metabolism and Excretion (Drug Fate)
How the body gets rid of the drug (liver, kidney, skin through sweat).
The speed of these 2 processes determines the duration of he drug’s effects.
Organs Involved
Liver
primarily involved in metabolism/biorransformation
Intestins, kidneys, lungs, and skin can also play a role in metabolism.
Kidney
primarily involved in excretion
but intestines/bile (feces), lungs (saliva), and skin (sweat) can also play a role. Most drugs leave the body through urine.
Liver cells = hepatocytes
Chemical factory controlled by enzymes (primarily on the smooth endoplasmic reticulum)
Breaks down drugs into ions, which are more easily excreted by the kidneys
Enzyme
Catalyst, ends in “ase”
speeds up chemical reactions
Example: alcohol dehydrogenase
Prodrug
The drug doesn’t help until it’s metabolized.
Aldopa (dopamine drug), Vivance (ADHD).
Kidneys
filters everything out and reabsorbs what is needed and what is soluble
The nephron is the functional unit of the kidney
Reabsorption (into blood) is already pH
Manipulation of urine pH can affect excretion (ion-trapping -bases are generally excreted)
Acidic drugs - sodium bicarbonate
Basic drugs - iv ammonia chloride
First Pass Metabolism
metabolism before the drug is fully absorbed
It can occur in drugs that pass through the digestive system
Drug molecules that are absorbed from he digestive system pass into he blood that goes to the liver before
5 Factors that Alter Drug Metabolism
Stimulation of Enzyme Systems
a.k.a. enzyme induction
Previous exposure to a specific drug that uses that enzyme can lead to higher levels of that enzyme
Metabolic toeralnce
Example: alcohol dehydrogenase, people who drink alcohol tend to have higher levels of alcohol dehydrogenase.
Some drugs use the same enzyme systems.
Depression of Enzyme Systems
When two drugs that require the same enzymes for metabolism are taken simultaneously, the metabolism of each will be depressed.
Competition for enzymes.
Example: alcohol & Antabuse ( for quitting alcohol, makes you sick if you drink) both require aldehyde dehydrogenase.
Age
Babies and elderly people often have poor metabolism
The metabolism of specific drugs seems to change with age
Genetic Polymorphisms
Genetic differences between people can lead to differences in the production of drug-metabolizing enzymes.
e.g., caffeine - slow metabolizers have higher risks of heart attack with coffee intake.
Carriers of the CYP1A2×1F allele
Species
Example - alcohol dehydrogenase
Guinea pig > human > rat/mouse
Phenylbutazone (treats race horses)
Half-lives: 3.6 hours vs. 3 days
Cytochrome P450 Enzyme Family
The major system involved in drug metabolism (e.g., alochol, tranquilizers, barbituaretes, antiaziety drugs, androgen, estrogen, PCBs).
Exposure to any of the above substances is associated with an increased production og CYP-450 (enzyme induction)
Other substances can inhibit enzymes (e.g., buspirone) (BuSpar) and grapefruit juice (furanocoumarin - inhibits CYP-3A4).
CYP-3A4 catalyzes about 50% of drug biotransformations, with CYP-2D^ and CYP2C each catalyzing about 20% more.
Drug Clearance & Rate of Excretion
Fastest when blood levels of drugs are high
First order kinetics — exponential elimination (constant fraction removed per time period), most drugs.
Exception: Zero-order kinetics — drug cleared at a constant rate regardless of concentration (alcohol - 1.0 oz of 100 proof alcohol per hour).
Half-Life (t 1/2)
time taken to reduce drug concentration in blood by 50%
Usually takes 6 half-lives for 98% of dthe rug to be eliminated.
Ideal t ½ for a drug taken 1x/day is 8 hours (88% eliminated in 24 hours).
Other Non-specific Factors that may affect drug response
Weighs
Sex and hormonal status
diesease
nutrition
biorhytms