EX 3: Circulatory System
Chapter 42: Circulation
Overview of circulation pathways:
From body to lungs
From lungs to heart
From heart back to body
Lecture Objectives
Establish the link between circulatory systems and gas exchange
Explore the evolution of circulatory systems in the animal kingdom
Explain the steps in the phases of heart contraction
Detail the components of blood, vessels, their exchange, transport and the concept of pressure
Relationship Between Structure and Function in Gas Exchange and Circulation
Specialized structures such as lungs or gills:
Mediate gas exchange with the environment.
Highly branched, thin-walled vessels:
Maximize exchange surface area to facilitate diffusion of gases.
A pump (the heart) drives fluid flow, while wide, thick-walled vessels enable circulation throughout the body.
Circulatory Systems and Diffusion
Circulatory systems link exchange surfaces with body cells.
Diffusion allows small molecules to move between cells and their surroundings, which is efficient over short distances.
In simple organisms, cells are often in direct contact with the environment.
In complex organisms, the circulatory system is interconnected with gas exchange mechanisms for body cells.
Gastrovascular Cavities
Simple animals may lack a circulatory system entirely.
Example: Cnidarians possess gastrovascular cavities:
These have thin walls (only two cells thick) for both digestion and circulation.
Example: Flatworms also have a gastrovascular cavity:
Their flat body shape minimizes diffusion distances.
Open and Closed Circulatory Systems
A circulatory system consists of:
Circulatory fluid
A set of interconnecting vessels
A muscular pump (the heart)
Open circulatory system:
The circulatory fluid bathes the organs directly.
Closed circulatory system:
Blood remains confined to vessels, distinct from interstitial fluid.
Both systems have their evolutionary advantages:
Open systems require less energy, seen in insects, arthropods, and some mollusks (hemolymph bathes organs directly).
Closed systems allow for larger organisms and better distribution of blood (seen in annelids, cephalopods, and vertebrates).
Vertebrate Circulatory Systems
The cardiovascular system in humans and other vertebrates has a closed circulatory system comprising:
The heart
Blood vessels
Three main types of blood vessels:
Arteries: Carry blood away from the heart.
Veins: Return blood to the heart.
Capillaries: Sites of chemical exchange between blood and interstitial fluid.
Arteries:
Branch into arterioles and lead to the capillary beds.
Veins:
Branch into venules returning blood from capillaries to heart.
Not distinguished by oxygen content but by blood flow direction.
Heart Structure and Blood Flow
Vertebrate hearts typically consist of two or more chambers:
Blood enters through atria and is pumped out through ventricles.
Number of chambers varies in different vertebrates:
Single circulation: Blood passes through two capillary beds before returning to the heart (e.g. in sharks, rays, bony fishes with a two-chambered heart).
Double circulation: Found in amphibians, reptiles, and mammals with separate circuits for oxygen-poor and oxygen-rich blood.
Types of Circulation
Single circulation examples: Fish
Blood flows from the heart through gill capillaries, then directly to the body.
Double circulation examples:
Amphibians: Oxygen-poor blood circulates through lungs & skin; oxygen-rich blood is delivered to body tissues.
Reptiles & Mammals:
Oxygen-poor blood flows through the pulmonary circuit to lungs; oxygen-rich blood goes through the systemic circuit.
Evolutionary Variation in Double Circulation
Amphibians and reptiles can go long periods without gas exchange or can rely on skin respiration.
Example: Amphibians have a three-chambered heart (two atria, one ventricle) to separate blood flow.
Example: Turtles and lizards also have a three-chambered heart with an incomplete septum.
Crocodilians: Have a complete septum dividing ventricles allowing for adaptation to aquatic environments.
Mammalian & birds Circulation
Four-chambered heart:
Two atria and two ventricles; left side pumps oxygen-rich blood, right side pumps oxygen-poor blood.
Essential for meeting the higher oxygen demands of endotherms versus ectotherms.
Process of Mammalian Circulation
Right ventricle pumps blood to lungs via pulmonary arteries.
Blood flows through lung capillaries, loading O2 and unloading CO2.
Oxygen-rich blood returns to left atrium via pulmonary veins.
Blood moves into left ventricle and is pumped to body tissues via systemic circuit.
Blood leaves left ventricle via aorta, supplying branches to:
Coronary arteries (heart muscle)
Capillary beds in brain and limbs
Abdominal organs
Capillaries rejoin into venules, then veins.
Superior vena cava collects oxygen-poor blood from head and forelimbs.
Inferior vena cava collects blood from the trunk and hind limbs and empties into the right atrium.
Blood flows into right ventricle to start the cycle again.
The Mammalian Heart: Anatomy and Function
The human heart is approximately the size of a clenched fist, composed of cardiac muscle.
Two atria (thin-walled) function as collection chambers.
Two ventricles (thicker walls) contract forcefully to pump blood.
Cardiac Cycle
The heart operates in a rhythmic cycle characterized by:
Systole: Contraction phase
Diastole: Relaxation phase
Cardiac Output
Defined as the volume of blood pumped into systemic circulation per minute, dependent on:
Heart Rate: Number of beats per minute
Stroke Volume: Amount of blood pumped per contraction
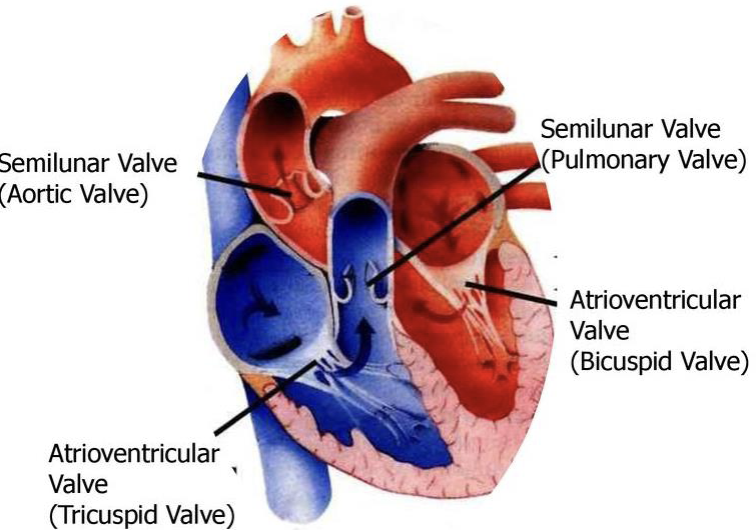
Heart Valves
Four valves prevent backflow:
Two atrioventricular (AV) valves separate atria and ventricles.
Two semilunar valves control blood flow to aorta and pulmonary artery.
The characteristic “lub-dup” sounds of a heartbeat are due to blood recoil against the valves:
First sound (
lub) for AV valves; second sound (dup) for semilunar valves.
Backflow through defective valves causes a heart murmur.
blood always passes through the tricuspid before bicuspid valve
Cardiac Rhythm and Autonomy
Some cardiac muscle cells are autorhythmic (contract without nervous system signals).
The sinoatrial (SA) node acts as a pacemaker, regulating contraction rates.
Electrocardiogram (ECG or EKG) records electrical impulses during the cardiac cycle.
Blood Vessel Structure and Function
All blood vessels have a central lumen lined with an epithelial layer.
Endothelium: Smooth lining that minimizes resistance
Capillaries are barely larger than a red blood cell with thin & leaky walls to facilitate material exchange.
Structure of Arteries and Veins
Arteries:
Thick elastic walls to accommodate high blood pressure from heart pumping.
They carry blood away from the heart to various parts of the body, delivering oxygen and nutrients to tissues.
Because of this the walls need to be thick
Veins:
Thinner walls do not require a thick structure due to lower pressure and feature valves to ensure unidirectional flow.
They carry blood back to the heart
Veins are sandwiched between skeletal muscle and contain valves that prevent backflow during venous return, allowing for effective blood circulation even against the force of gravity.
Blood Pressure
Blood flows from high to low pressure regions.
Blood pressure is the force exerted on vessel walls.
Recoil of elastic arterial walls helps maintain pressure.
Higher resistance in smaller capillary diameters dissipates pressure.
Blood Pressure during Cardiac Cycle
Systolic Pressure: Highest recorded pressure in arteries during ventricular contraction.
Diastolic Pressure: Pressure in arteries during ventricular relaxation, lower than systolic pressure.
Both regulated through homeostatic mechanisms via vasoconstriction(more pressurre) and vasodilation(less pressure).
Measurement of Blood Pressure
Sphygmomanometer: Measures blood pressure; process involves inflating a cuff, further steps include listening for blood flow resumption and cessation to measure systolic and diastolic values.
Capillary Function
Exchange of substances between blood and interstitial fluid occurs across capillary cell walls.
Blood pressure pushes fluid out, while osmotic pressure (from blood proteins) draws fluid back in, resulting in a net loss from capillaries (more fluid leaves than returns).
Lymphatic System
The lymphatic system returns excess interstitial fluid from capillaries aka lymph, which drains into veins in the neck.
balances fluid levels in body
Valves in lymph vessels prevent backflow.
Edema: Swelling caused by lymphatic flow disruptions.
Lymph Nodes: Organs filtering lymph, part of immune response; swollen nodes signify infection presence.
Blood Composition & Functions
Blood is connective tissue consisting of cells suspended in a liquid matrix known as plasma (45% cell volume, 55% plasma).
Plasma Components
Inorganic Salts (Electrolytes): Dissolved ions that influence blood composition.
Proteins:
Maintain osmotic balance, assist lipid transport, and immune functions.
Composition is similar to interstitial fluid but contains higher protein concentrations.
Cellular Elements of Blood
Red Blood Cells (Erythrocytes): Most numerous, contain hemoglobin for O2 transport (each hemoglobin binds four O2) and lack nuclei and mitochondria in mammals. Iron allows oxygen to bind to hemoglobin efficiently, facilitating the delivery of oxygen to tissues throughout the body.
White Blood Cells (Leukocytes): Five types involved in immune defense through phagocytizing(eating) pathogens/bacteria or inducing immune responses.
Platelets: Cellular fragments essential for blood clotting; the coagulation process involves converting fibrinogen to fibrin to form clots. It forms liquid blood into a solid to patch up a cut.
Blood Disorders
Sickle-cell Disease: Result of mutated hemoglobin that distorts erythrocytes into sickle shapes, leading to vascular blockage and pain.
Stem Cells and Blood Component Replacement
All blood cell types develop from stem cells in the red marrow of bones like ribs, vertebrae, and pelvis.
Hormone erythropoietin (EPO) stimulates production of erythrocytes, especially in low oxygen conditions; recombinant EPO can be used clinically, e.g. in anemia.
Cardiovascular Diseases
Disorders affecting heart and blood vessels range from minor functional disturbances to severe issues like heart attacks and strokes.
Atherosclerosis: Buildup of fatty deposits (plaques) leading to arterial hardening and potential blockage, causing cardiac events(heart attack).
also results in blood clots
Heart Attack and Stroke
Heart Attack: Damage or death of cardiac tissue due to blocked coronary arteries(first place blood goes through from left ventricle).
Stroke: Death of brain tissue from ruptured or blocked cerebral arteries.
Angina Pectoris: Chest pain due to partial coronary artery blockage.
Risk Factors and Treatments for Cardiovascular Disease
High LDL/HDL ratio increases heart disease risk, which can be improved through lifestyle changes like exercise and dietary choices.
Statins help reduce LDL cholesterol and heart attack risks.
Aspirin can reduce inflammation and prevent heart attack and stroke risks.
Hypertension contributes significantly to heart disease and can be managed via diet, exercise, and medications.