Lung Cancer Notes
Lung Cancer
Small-cell and Non-small Cell Lung Cancer
Learning Objectives
Identify populations more at risk for lung cancer, including types of environmental exposure.
Anticipate patients who meet criteria for annual lung cancer screening.
Differentiate between Small Cell Lung Cancer (SCLC) and the three types of Non-small Cell Lung Cancer (NSCLC).
Assess patients for relevant clinical manifestations of lung cancer, both early and advanced.
Demonstrate knowledge of treatment modalities for lung cancer, including surgical resection, radiation, chemotherapy, targeted therapy, and immunotherapy.
Understand the difference between palliative, curative, and adjunctive treatments.
Key Terms
Angiogenesis: The development of new blood vessels.
Apoptosis: Programmed cell death.
Chemotherapy: The treatment of disease by the use of chemical substances, especially the treatment of cancer.
Hemoptysis: Coughing up blood.
Lymphadenopathy: Disease affecting the lymph nodes.
Metastasis: The spread of cancer cells from the primary site to other parts of the body.
Paraneoplastic Syndrome: A syndrome or disorder that is a consequence of cancer in the body but is not directly caused by the physical effects of the tumor.
PET Scan: A type of nuclear medicine imaging that uses small amounts of radioactive material to visualize and measure changes in metabolic processes.
Radiation: The emission of energy as electromagnetic waves or as moving subatomic particles.
Surgical Resection: Surgical removal of tissue or an organ.
Superior Vena Cava Syndrome: Obstruction of the superior vena cava.
Epidemiology
Lung Cancer is the leading cause of cancer-related deaths (25%) in the U.S.
High mortality rate; low cure rate.
Smoking is responsible for 80%-90% of all lung cancers.
Female smokers are at a greater risk than male smokers.
African Americans have the highest incidence of lung cancer and are more likely to die from the disease.
Asian and Pacific Islanders have the lowest rate of lung cancer.
Etiology
Assessment of risk falls into 3 categories:
Smokers (current & primary exposure)
Nonsmokers (former smokers)
Never smokers (secondary or tertiary exposure)
Never smoker considered person who has had less than 100 cigarettes in their lifetime.
Tertiary exposure: Carcinogens leftover on clothes or hair after smoking and someone breathes it in.
Risk is directly related to total exposure to tobacco smoke
Total # of cigs in a lifetime
Pack year history
Age of smoking onset
Depth of inhalation
Primary, secondary, tertiary
Tar & nicotine content
Use of unfiltered cigs
Roll own cigarettes
Increases carcinogens
Theory: people have different genetic carcinogen-metabolizing pathways.
Has to do with HLAs which live on our cells
Other causes of lung cancer include exposure to:
Pollution
Radiation
Residential contaminants (old house):
Radon Gas
Asbestos
Industrial agents:
Radon, coal dust, asbestos, chromium, arsenic, diesel exhaust
Lung Cancer Screening
National Lung Screening Trial Criteria for screening (annually):
50-80 years of age
Current or former smokers with at least a 20-pack year history
Determined by packs per day x # of year smoked.
Ex. Half a pack of day for 10 years → 5 years.
Former smokers who quit within the last 15 years
Spiral CT scan performed if all criteria met → #1 diagnostic.
Key Points:
Lung cancer screening can help find lung cancer at an early stage when it is easier to treat.
At this time, studies have shown that low-dose spiral CT scan is the only lung cancer screening tool that reduces the risk of dying from lung cancer.
Lung cancer screening is not right for everyone.
Pathophysiology
Not well understood.
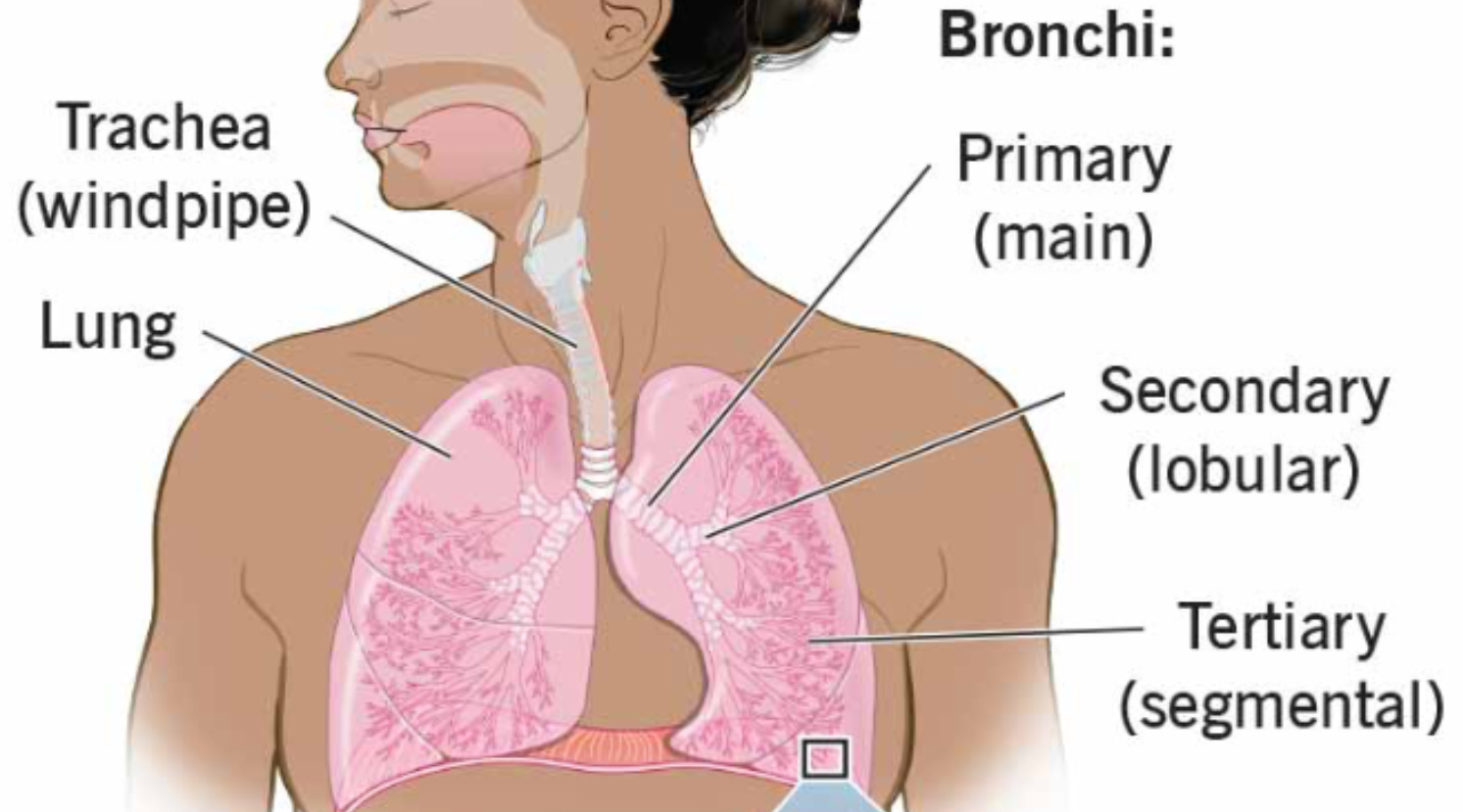
Most lung cancers arise from mutated bronchial epithelial cells.
Located in bronchi (breathing portion of lungs)
Found more in segmental bronchi and in upper lobes.
Can take 8-10 years to reach 1 cm nodule.
Primary Lung cancers are categorized in 2 broad subtypes
Non-small cell (NSCLC) - More Prevelant
Accounts for 84% of lung cancers
Small cell (SCLC)
Accounts for 13% of lung cancers
Non-Small Cell Lung Cancer (NSCLC) → Most Prevalent
Three Main Types
Squamous cell carcinoma
Accounts for 20%-30% of lung cancers
Slow growth, metastasis less common
Almost always associated with smoking
More common in men
Tx: Surgical resection (if amenable)
Adenocarcinoma
Accounts for 30-40% of lung cancers
Moderate growth
Most common in never smokers and in women
Ex. Cocktail waitresses, flight attendants (when smoking was allowed on plane) - people exposed to smoke
Metastatic disease is often present when symptoms occur
Urology may need to be consulted because they can show signs related to GU system
Surgical resection ( if amenable)– doesn’t respond well to chemotherapy
Large Cell Carcinoma
Accounts for 10% of lung cancers
Rapid growth of undifferentiated cells (implant wherever they want to in the body) and often arises in the bronchi
Usually not treated surgically due to high degree of metastasis
Tumor may respond to radiation
Decreases size of the tumors and prevents them from pressing on other structures.
Small Cell Lung Cancer (SCLC)
Accounts for 20% of lung cancers “death sentence” → metastasizes quickly
Rapid growth with poor prognosis
Most malignant form of lung cancer with early metastasis, frequently to brain
May present with ALOC or AMS (more neurological symptoms than respiratory)
Chemotherapy and radiation – palliative (supportive, not curative)
Paraneoplastic Syndrome
Develops as a result of cancer.
Body-wide and caused by a reaction of hormones, cytokines, enzymes, or antibodies that destroy healthy cells.
Excreted by tumor cells (cancer is already existing and it excretes the cells), or
Body’s immune response to the cancer
May manifest before cancer diagnosed
Associated most with SCLC
Examples:
Hypercalcemia
S/S Bone pain, constipation, muscle weakness
SIADH
Hold onto a lot of water
Adrenal Hypersecretion
Adrenals release steroids (testosterone, cortisol, and epinephrine) → pts have too much floating around.
Elevated cortisol = Cushing’s Syndrome (fatigue, purple striae on abdomen, etc)
Polycythemia
Overproduction of RBCs
RBC and hematocrit elevated
Hematocrit shows total volume and percentages of RBCs
Cushing’s syndrome
From too much cortisol
Clinical Manifestations
Common to all lung cancers: symptoms are non-specific and appear late in the disease process.
BIG 3 SIGNS AND SYMPTOMS:
Persistent Cough
Blood-tinged sputum
Because blood going to area or cough breaking open some capillaries
Lobar pneumonia refractory (resistant) to antibiotic tx
Where pt has a blocked off patch of pneumonia in the lobes of a lung and has gotten 1-2 rounds of abx but pt still has symptoms and pneumonia.
Dyspnea
Wheezing
Chest pain
More pleuritic (off to side of lungs)
Late Signs:
Anorexia, unexpected weight loss, fatigue, nausea, vomiting (main)
Hoarseness
Tumor pressing on laryngeal nerve
Unilateral paralysis of diaphragm
May cause respiratory distress (part of the diaphragm is pushed down)
Dysphagia
Superior vena cava obstruction
Affects upper body (may feel fullness in face or head)
Palpable lymph nodes
Metastasis – through direct extension, or blood and lymph system
Common sites: lymph nodes, liver, brain, bones, adrenal glands
Pts often come in for a different symptoms (ex. Bone pain) that ends up being related to lung cancer
Small cell lung cancer can metastasize quickly
Diagnostic Studies
CT scan → best diagnostic tool
How big tumor is and if there’s blood flow into it.
CXR
PET/Bone Scans
Looks for metastasis
Sputum cytology – only 20-30% positive (more of a centralized lung cancer like primary or secondary bronchus which show up with a positive cytology)
Looks at cells under a microscope for abnormal cells
The other lung cancers live further down closer to the alveoli and don’t come up with sputum.
Biopsy – definitive diagnosis
Fine needle aspiration
Insert needle through the chest wall and into lung (risk of pneumothorax)
Bronchoscopy
Camera into bronchi through throat
Thoracoscopy
Make an incision to go in and look through the chest cavity
Thoracentesis
Pleural effusion may develop from cancer itself → this allows provider to grab a sample and send it to lab.
Staging
Non-small cell uses the TNM staging system
T = Tumor
T0 means no evidence of a primary tumor, so it may be that the cells are cancerous but they haven’t developed a tumor.
T1-4 means an ascending degree of tumor size and involvement. (Know that 1 is small and 4 is big)
TX means tumor can’t be measured or undifferentiated (can’t tell what type of cells are there)
TIS (carcinoma in situ) means it’s a very new, small tumor still within its bounds it originally grew. Pts with carcinoma in situ have a better outcome due to surgical resection.
N = Lymph nodes
N0 means no evidence of disease in lymph nodes
N1-4 know that 1 is small and 4 is big)
NX means unable to be assessed
M = Metastasis
M0 means no evidence
M1-4 means degree of metastasis (is it generalized or close to where it’s at vs. widespread)
MX how far it has grown
Small cell; staging unnecessary because this cancer is always considered systemic
Go straight into treatment
Interprofessional Care
Surgical Resection
Treatment of choice in earlier stages of non-small cell lung cancer
Smaller tumors/better outcome
Potentially curative (especially if tumors are small)
50% of tumors are not resectable at the time of diagnosis
Types of Resection:
Pneumonectomy
Take the lung
Lobectomy
Remove lobe of lung (we have 5 lobes)
Segmental or wedge resection
Take segment of lung out (smaller than lobe)
Video-assisted thoracoscopic surgery (VATS)
Most surgeries performed with this
Go in and remove what they need to with a few incisions
Interprofessional Care: Radiation
Treatment for both types
Curative (giving in hopes to cure the disease), palliative (wont cure but helps feels better), or adjunctive (they do this with something else in hopes to cure the pt)
Primary treatment in non-surgical patients
Relief of symptoms/pain from bronchial obstructive tumors, SVC syndrome, bone pain (bone hyperplasia)
Treat metastatic bone pain or cerebral involvement
Performed preoperatively to reduce tumor mass for surgical removal.
Never radiate a child’s brain younger than 5.
Over 5: the tissues are produced but not the functionality.
SBRT
delivers a targeted radiation dose directly to a tumor (Focuses directly on the tumor, unlike radiation)
therapy over 1-3 days
Interprofessional Care: Chemotherapy
Primary treatment in SCLC, or for nonresectable NSCLC
Often done in a combination of 2 or more drugs
Want cell cycle phase nonspecific
Can target cells where they are growing at different stages (cancer cells can go dormant and if we leave them alone, they will grow again).
Helps decrease likelihood of tolerance
Goal: to eliminate or reduce the number of cancer cells
Performed in adjunction with radiation to help shrink tumors, diminish cells, and stop ells from growing, and to eradicate cancer cells.
Two categories of Chemo drugs:
Cell cycle phase non-specific
Cell cycle phase specific
Interprofessional Care: Targeted Therapy
Inhibits tumor growth rather than directly killing cancer cells
Aims to prevent tumor growth
Types:
Blocks growth signals
Blocks kinase protein (responsible for cancer development and growth)
Blocks angiogenesis (A property the body has to create a new blood supply because cancer cells create their own blood supply)
Interprofessional Care: Immunotherapy
Monoclonal Antibodies (“-mabs”)
Take a pre-made antibody and continue producing it until identical
Block PD-1 (T cell protein) to prevent cancer cell from attacking other cells
Boosts immune response against cancer cells; shrinks tumor overtime or slows growth
Utilizes a horse antibody and causes pt to go into an anaphylactic reaction, which we want to shrink their anaphylactic reaction → Allows T cells to work at destroying cancer cells. Interferes with PD-1 and PD-L1.