Cutaneous Lupus Erythematosus (CLE)
Epidemiology
Systemic lupus erythematosus (SLE) is common with significant morbidity and mortality.
Risk is strongly influenced by sex, with women outnumbering men by at least 9:1.
SLE primarily affects women during childbearing years, indicating a likely hormonal influence. Rare in prepubertal children.
Patients with only cutaneous lesions have a lower female-to-male ratio (approximately 3:1), but female predominance remains.
Ethnicity is a significant risk factor, nearly as influential as sex.
In the US, SLE prevalence is fourfold higher in African-American women than in White women (211 vs. 64 per 100,000).
African-Americans tend to develop SLE at an earlier age and exhibit a higher mortality rate.
Likely similar prevalence in Asian, Latin American, and European White populations compared to US Whites.
Approximately as many patients have cutaneous lupus erythematosus (LE) without concurrent SLE as those with SLE.
Pathogenesis
Pathogenesis of cutaneous lupus erythematosus (LE) involves genetic and environmental factors.
Environmental triggers include ultraviolet radiation (UVR), medications, cigarette smoking, and possibly viruses.
Interaction of these factors causes an inflammatory cascade with cytokine and chemokine responses.
A lichenoid tissue reaction is common, characterized by epidermal basal cell damage and lymphocytic infiltrate in the dermis.
Various genes involved in B and T cell function and immune responses may contribute to disease variability.
UVB and UVA are linked to exacerbation of cutaneous LE, with UVB being a more potent inducer of skin changes.
UVR leads to apoptosis, translocation of antigens, and increased production of autoantibodies and type I interferons (IFNs).
Proinflammatory cytokines such as TNF, IL-1, and IFN-γ are induced by UVR.
Dendritic cells contribute to T cell activation and can prime CD8+ T cells against keratinocyte-derived antigens.
An increase in plasmacytoid dendritic cells and cytotoxic T cells is noted within cutaneous LE lesions.
UV radiation initiates a complex immune response, leading to a positive feedback loop and exacerbation of skin lesions.
Variants and subtypes
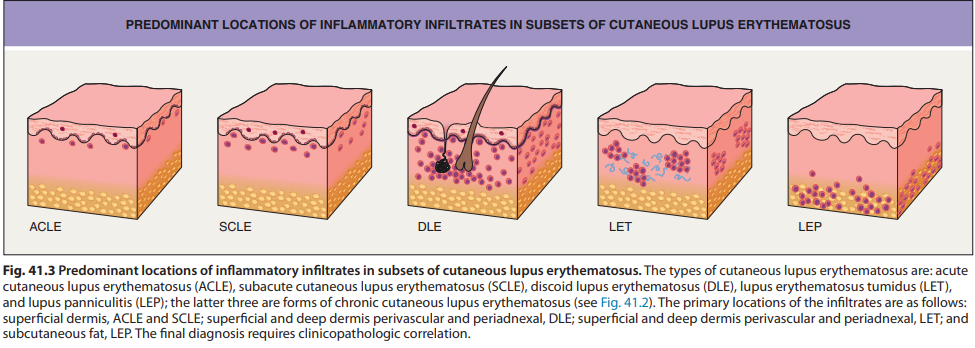
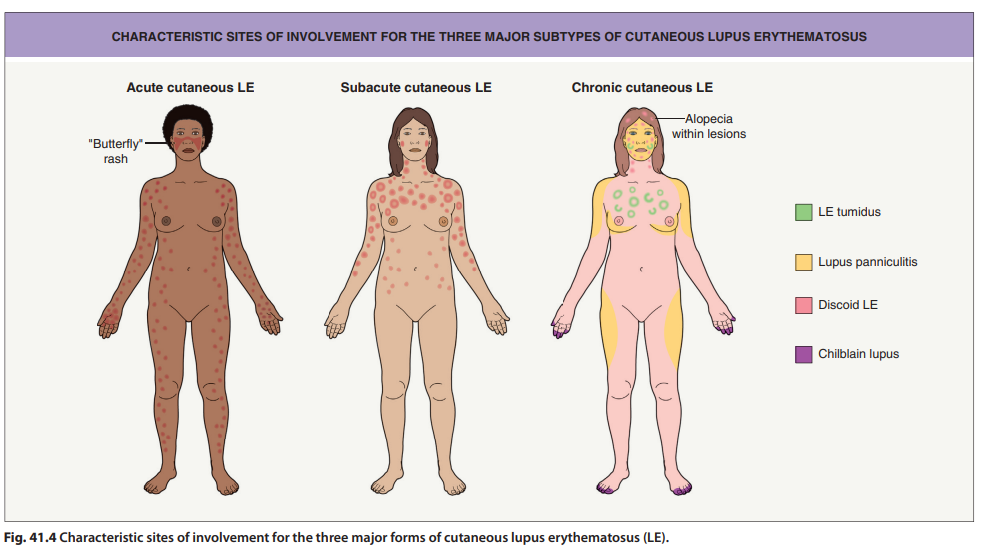
Acute Cutaneous LE (ACLE):
Subacute Cutaneous LE (SCLE):
Chronic Cutaneous LE (CCLE):
Includes several subtypes
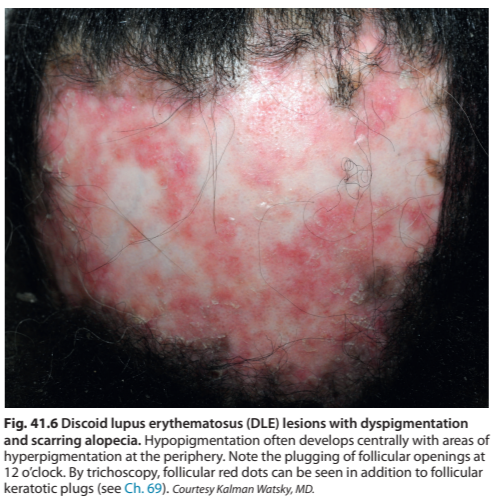
Discoid LE (DLE):
Lesions are frequently long-lived and intensely inflammatory.
Can lead to permanent disfiguring scars.
Active lesions are typically thicker and firmer than surrounding skin due to pronounced superficial and deep dermal inflammatory infiltrate.
Features include follicular plugging, scarring alopecia, and dyspigmentation with hypopigmentation centrally and hyperpigmentation peripherally.
sometimes can also present as vitiligo-like depigmentation
Can rarely also present as hypertrophic (verrucous) DLE - characterised by thick scaling overlying the discoid lesion or occurring at the periphery of the discoid lesion - mainly on extensor surfaces of the arms but face and trunk may also be involved



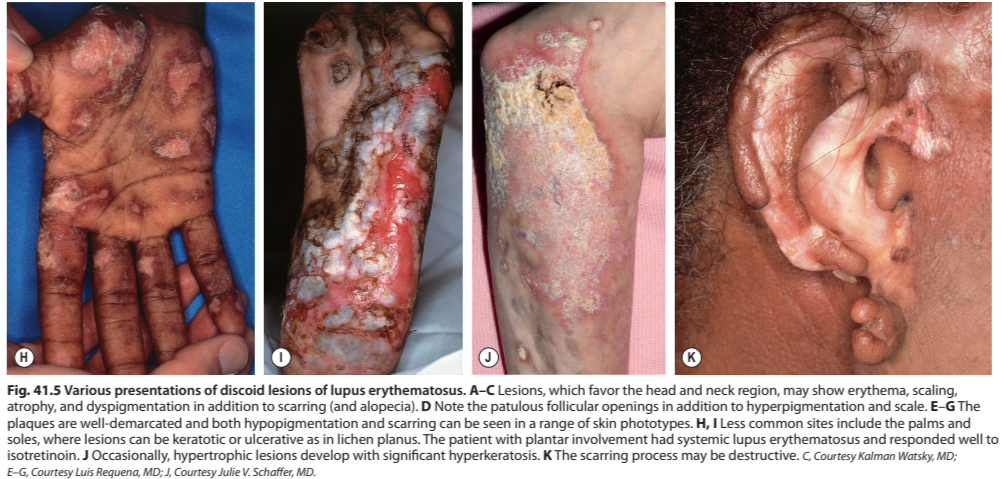
Adnexa are prominently involved.
May be localized or widespread.
Rarely, squamous cell carcinoma can develop in a long-standing discoid lesion.
Lupus Erythematosus Tumidus (LET):
Typically presents with firm, erythematous plaques that lack scale or follicular plugging.
Intense perivascular and periadnexal inflammatory infiltrate within the dermis with mucin deposition.
Lupus Panniculitis (Lupus Profundus):
A variant of lupus panniculitis, with inflammation in the subcutaneous fat.
Chilblain Lupus:
Presents with red or dusky purple lesions on the fingers, toes, elbows, knees and lower legs.
Other Variants:
Neonatal LE: Can present with annular erythematous plaques on the forehead and scalp
Rowell Syndrome: Erythema multiforme-like lesions.
Bullous LE: Blistering eruption similar to toxic epidermal necrolysis or erythema multiforme major.
Diagnostic Criteria:
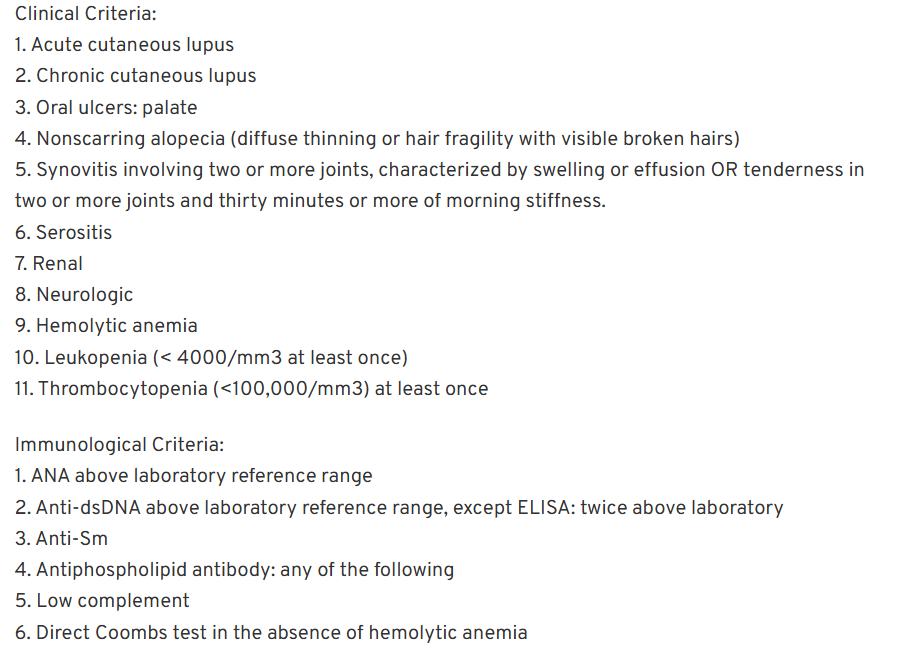
The Systemic Lupus International Collaborating Clinics (SLICC) classification system requires at least 4 of 17 criteria (including at least one clinical and one immunologic criterion), or biopsy-proven lupus nephritis with ANAs or anti-dsDNA antibodies.
The American College of Rheumatology (EULAR/ACR) classification criteria require a score of 10 or more with entry criteria fulfilled.
Diagnosis and Investigations
Histopathology:
SCLE: More obvious interface dermatitis and perivascular inflammation.
DLE: Focal interface dermatitis and dense perivascular lymphoid infiltrates throughout the dermis.
May also show periadnexal inflammation, follicular plugging and scarring.
LET: Prominent dermal mucin deposition and dermal perivascular and periadnexal lymphocytic infiltrates with a lack of epidermal change.
Lupus Panniculitis: Prominent inflammatory infiltrates within the lobules of the subcutaneous fat.
May have overlying changes of DLE.
Some of the more distinctive histologic features include basal cell damage, lymphohistiocytic inflammatory infiltrates admixed with CD123+ plasmacytoid dendritic cells, and periadnexal inflammation (primarily in discoid lesions), follicular plugging, and scarring.
Direct Immunofluorescence (DIF):
Granular deposits of IgM at the dermal-epidermal junction are characteristic of lupus.
Antibody deposits at the dermal-epidermal junction are the most characteristic immunohistologic finding in lesions of cutaneous lupus.
Laboratory Tests:
ANA with profile (anti-dsDNA, -Sm).
Urinalysis.
CBC with differential and platelet count.
Chemistries (BUN, creatinine).
ESR, CRP.
Complement levels (C3, C4).
Antiphospholipid antibodies, PT/PTT.
Autoantibodies to dsDNA and Sm are relatively specific for SLE.
Autoantibodies to SSA/Ro, SSB/La, U1RNP, histones, and ssDNA are common in patients.
A diagnostic algorithm for cutaneous lupus involves initial evaluation, a lesional biopsy for histology and DIF, and systemic evaluation if needed.
Differential Diagnosis
ACLE/Malar Rash: Rosacea, Seborrheic dermatitis, Sunburn, Drug-induced photosensitivity, Dermatomyositis.
SCLE: Psoriasis, Dermatophytosis, Polymorphous light eruption, Granuloma annulare, Pemphigus foliaceus.
Discoid Lesions: Lichen planus, Sarcoidosis, Tinea faciei, Follicular mucinosis, Non-melanoma skin cancer.
Lupus Tumidus: Urticarial vasculitis
Chilblain Lupus: Pernio, acrocyanosis
Treatment/Management
General measures include avoiding photosensitizing medications and smoking cessation.
Sun protection is essential, including sunscreens, protective clothing and sun avoidance.
Careful attention should be given to vitamin D and calcium intake.
Topical corticosteroids, antimalarials and dapsone may also be considered.
Complications
Scarring and disfigurement.
Dyspigmentation.
Scarring alopecia.
Progression to systemic lupus erythematosus (SLE).
Rarely, squamous cell carcinoma in long-standing discoid lesions.
Additional Notes
The three major types of cutaneous LE (ACLE, SCLE, CCLE) are not mutually exclusive.
Drug-induced lupus should be considered in the differential diagnosis of CLE.
Cutaneous lesions of LE can indicate internal disease.
Let me know if you need further clarification or have any additional questions.