Renal system sample exam questions
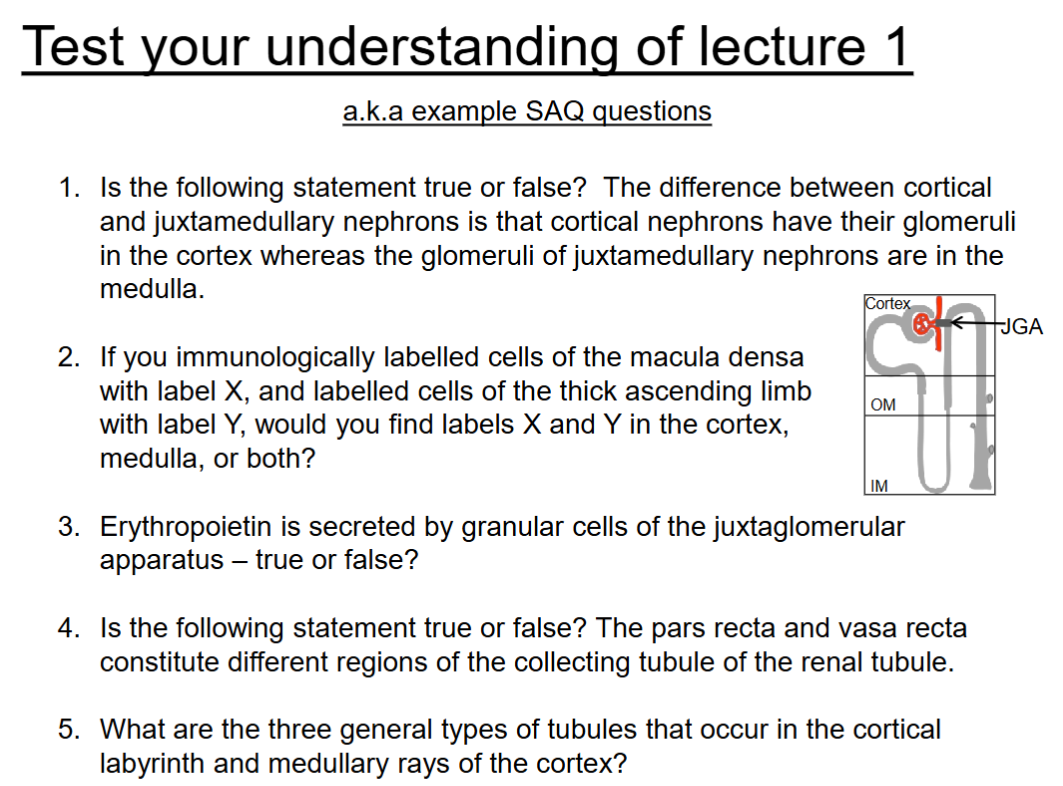
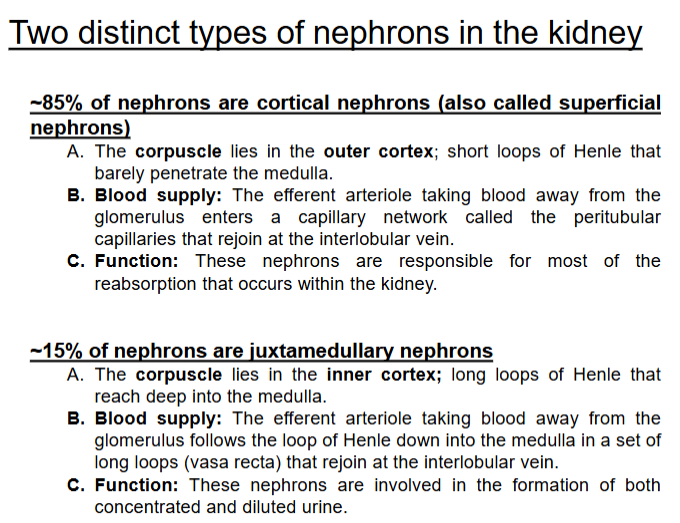
Is the following true or false? the difference between cortical and juxtamedullary nephrons is that cortical nephrons have their glomeruli in the cortex whereas the glomeruli of juxtamedullary nephrons are in the medulla.
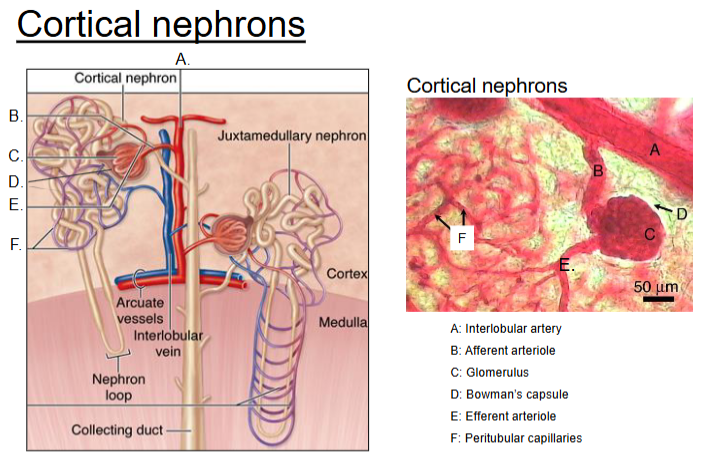
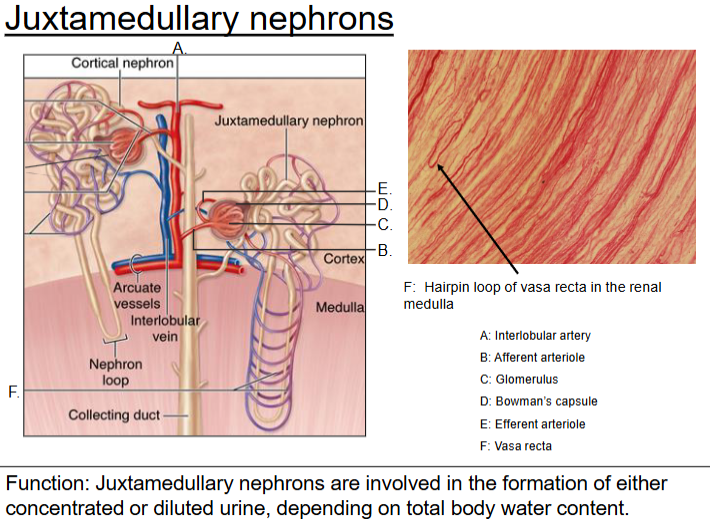
False: Both cortical and juxtamedullary nephrons have their glomeruli in the cortex, not the medulla. Juxtamedullary nephrons are just closer to the border with the medulla and have longer loops that dip deep into the medulla.
If you immunologically labelled cells of the macula densa with label x and labelled cells of the thick ascending limb with label Y, would you find labels X and Y in the cortex, medulla or both?
You would find label X (macula densa) and label Y (thick ascending limb) in the cortex. The macula densa is located at the junction of the thick ascending limb of the loop of Henle and the distal convoluted tubule, both of which are in the renal cortex.
Erythropoietin is secreted by granular cells of the juxtaglomerular apparatus - true or false?
False. Erythropoietin is primarily secreted by peritubular interstitial cells in the renal cortex, not by the granular cells of the juxtaglomerular apparatus. The granular cells are responsible for secreting renin.
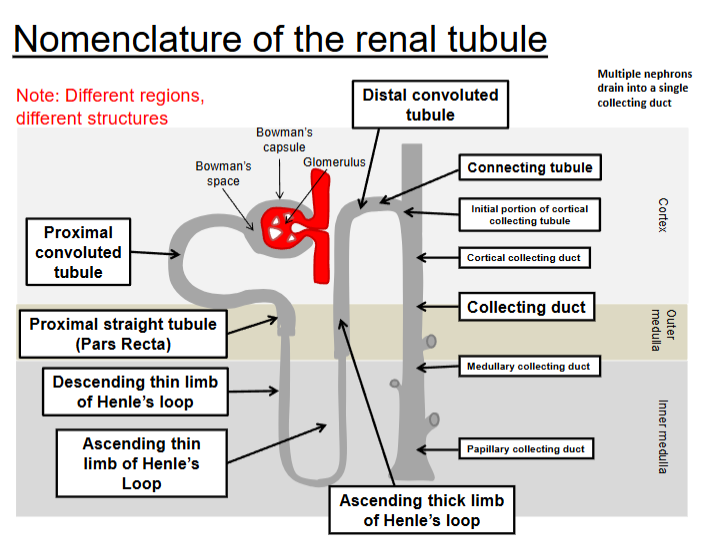
True or false, the pars recta and vasa recta constitute different regions of the collecting tubule of the renal tubule
False. The pars recta refers to a straight portion of the proximal convoluted tubule (PCT) and the distal convoluted tubule (DCT), while the vasa recta are the blood vessels that run parallel to the loop of Henle in the medulla. They are involved in the countercurrent exchange but are not part of the collecting tubule.
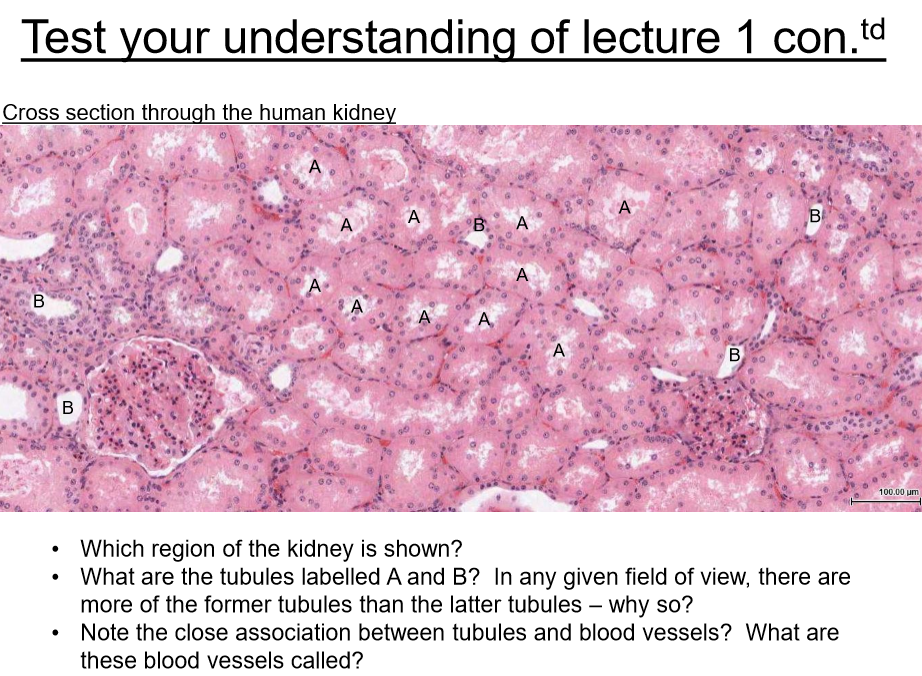
What are the three general types of tubules that occur in the cortical labyrinth and medullary rays of the cortex?
The three general types of tubules are:
Proximal tubules – including both convoluted and straight (pars recta) segments.
Distal tubules – including both convoluted and straight segments.
Collecting tubules/ducts – which transport filtrate toward the renal medulla.
These tubules are distributed within the cortical labyrinth (mainly convoluted segments) and medullary rays (mainly straight segments and collecting ducts).
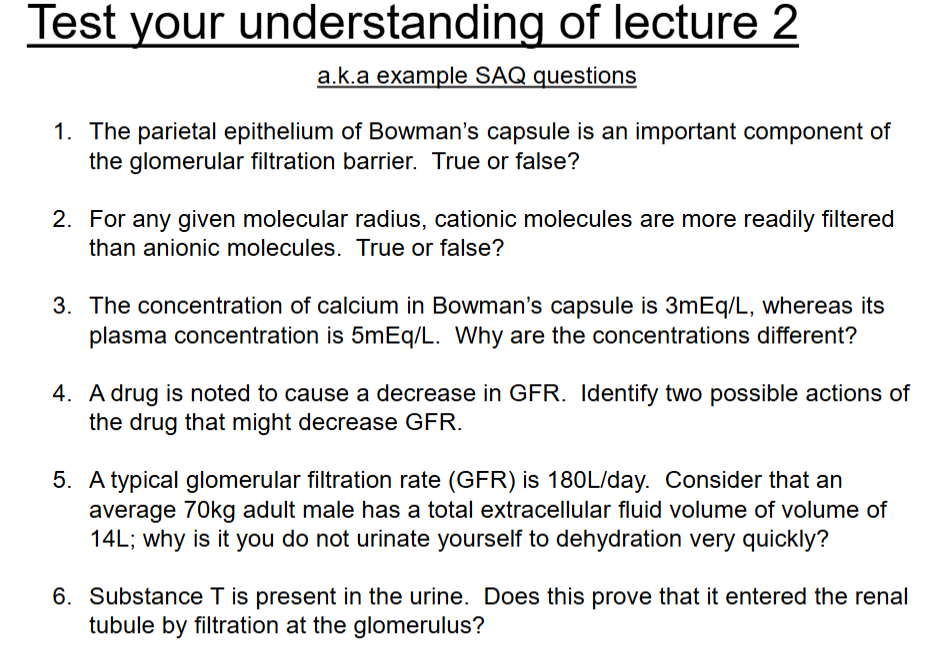
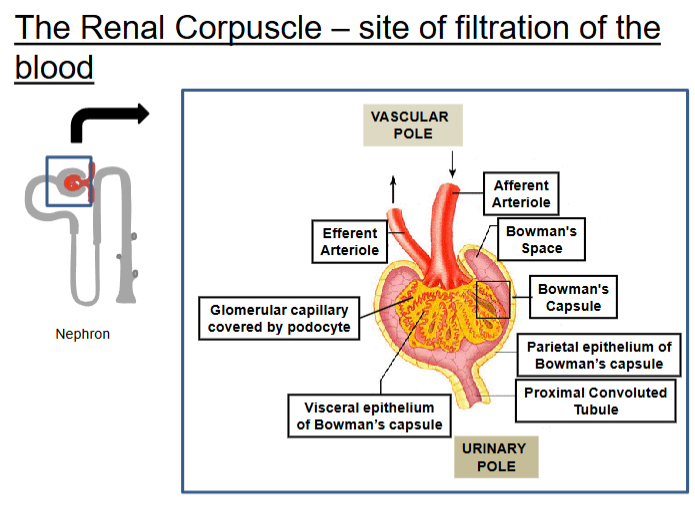
Parietal epithelium of Bowman’s capsule is an important component of the glomerular filtration barrier. True or false?
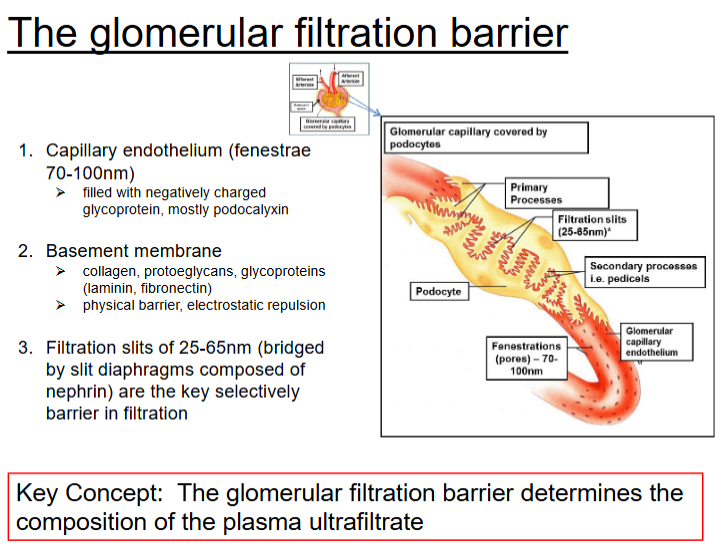
The parietal epithelium of Bowman’s capsule is a simple squamous epithelium that forms the outer wall of the capsule but does not contribute to the glomerular filtration barrier. The actual filtration barrier is formed by:
Fenestrated endothelium of glomerular capillaries
Basement membrane
Podocytes of the visceral epithelium with filtration slits.
For any given molecular radius, cationic molecules are more readily filtered than anionic molecules. True or False?
The glomerular filtration barrier carries a negative charge, primarily due to glycoproteins in the basement membrane and podocyte slit diaphragms. This repels anionic (negatively charged) molecules and favours filtration of cationic (positively charged) molecules of the same size.
The concentration of calcium in Bowman’s capsule is 3mEq/L, whereas its plasma concentration is 5mEq/L. Why are concentration different?
The concentrations differ because approximately 40% of plasma calcium is bound to proteins, primarily albumin, and only free (ionized) calcium is filtered at the glomerulus. Since protein-bound calcium cannot pass through the filtration barrier, the calcium concentration in Bowman’s capsule is lower than in plasma.
A drug is noted to cause a decrease in GFR. Identify two possible actions of the drug that might decrease GFR.
Constriction of the afferent arteriole, which reduces blood flow into the glomerulus.
Dilation of the efferent arteriole, which decreases glomerular capillary pressure.
A typical glomerular filtration rate (GFR) is 180L/day. Consider than an average 70kg adult male has total extracellular fluid volume of 14L, why don’t you urinate yourself to dehydration very quickly?
Although the GFR is approximately 180 L/day, about 99% of the filtrate is reabsorbed along the nephron, particularly in the proximal tubule, loop of Henle, distal tubule, and collecting duct. As a result, only about 1–2 L of urine is excreted per day, preventing loss of extracellular fluid and dehydration.
Substance T is present in urine. Does this prove that it entered the renal tubule by filtration at the glomerulus?
No, the presence of Substance T in urine does not prove it entered the renal tubule by filtration at the glomerulus. It could have entered the tubule by tubular secretion from peritubular capillaries into the nephron. Therefore, further analysis is needed to determine the exact route.
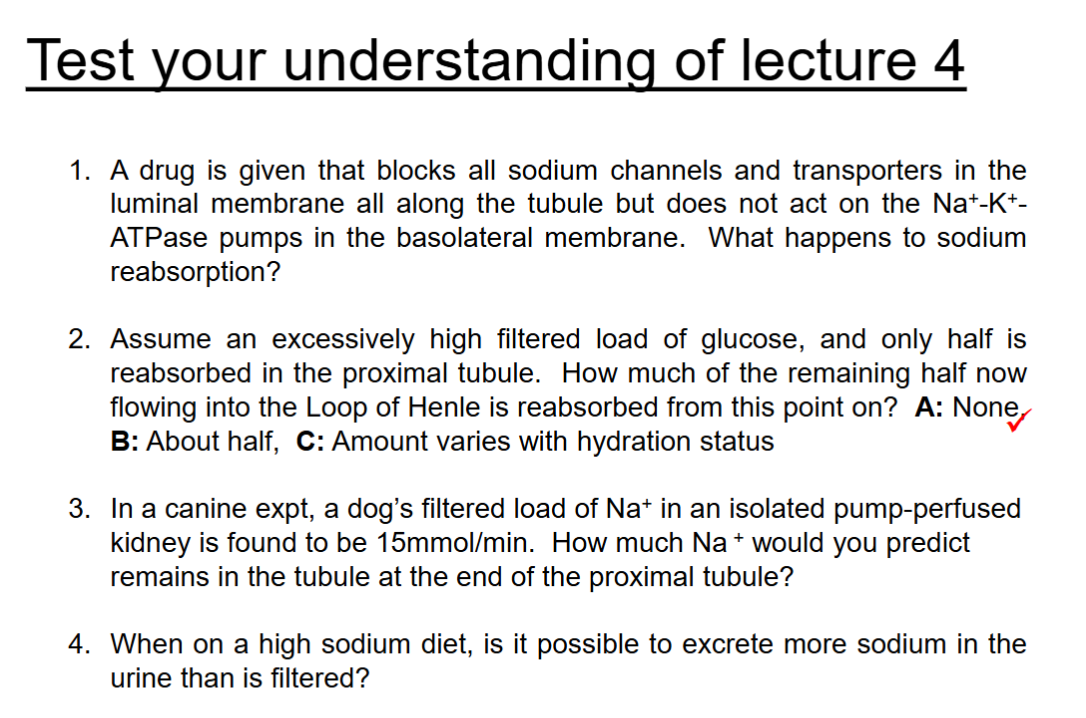
A drug is given that blocks all sodium channels and transporters in the luminal membrane all along the tubule but does not act on the Na+-K+- ATPase pumps in the basolateral membrane. What happens to sodium reabsorption?will not be asked as an SAQ question.Prevents sodium reabsorption, needs sodium to bring out the sodium. No sodium in the pumps.
*Assume an excessively high filtered load of glucose, and only half is reabsorbed in the proximal tubule. How much of the remining half now flow into the Loop of Henle is reabsorbed from this point on?
a. NONE, b. about half, c. amount varies with hydration status
→ possible SAQ
Glucose is only absorbed in the proximal tubule hyperglycemic via sodium0glucose transporters (SG1T2 and SG1T1). Beyond that point there is no significant mechanism for glucose reabsorption.*In a canine expt, a dog’s filtered load of Na+ in an isolated pump-perfused kidney is found to be 15mmol/min. How much Na+ would predict remains in the tubule at the end of proximal tubule? → covered in example question.
When a high sodium diet, is it possible to excrete more sodium in the urine than it is filtered?
No, sodium is always excreted in urine as less or equal amounts filtered by the glomeruli. Sodium is actively transported out of tubular cells by the sodium-potassium ATPase on the basolateral membrane, keeping sodium low. Promotes reabsorption of sodium with a high-sodium diet. The more sodium and water retained, the more it increases blood volume and raises blood pressure leading to hypertension.
Hypertension = Condition where blood pressure in the arteries are consistently too high meaning the heart has to work harder to pump blood. Over time, damages blood vessels and organs. Increasing the risk of heart disease, stroke and kidney problems.
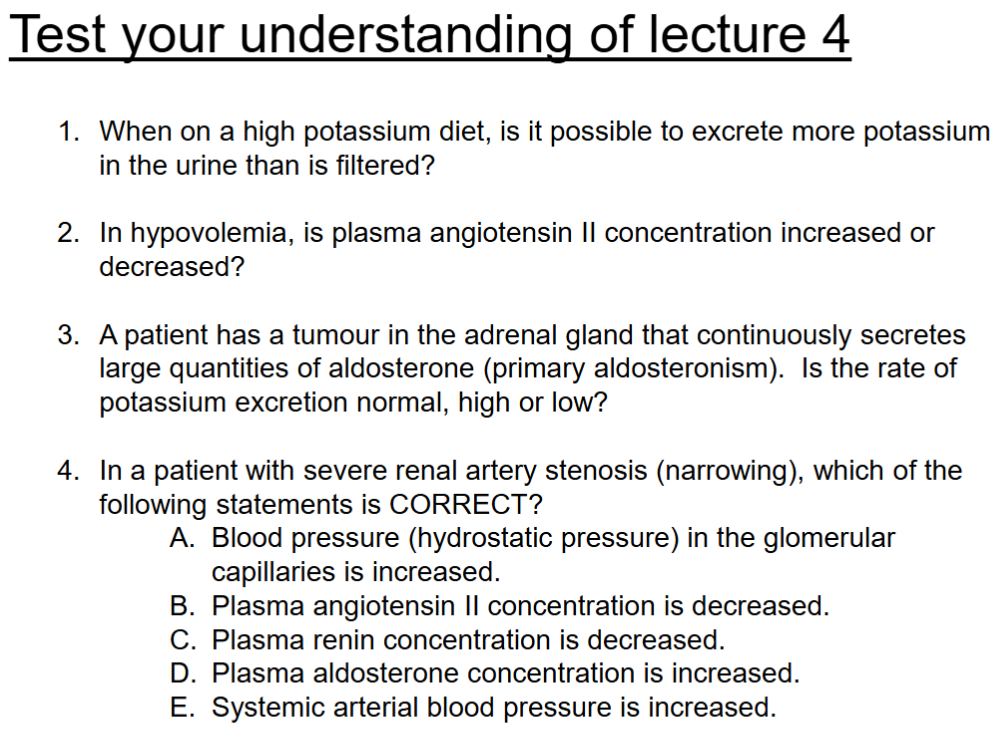
When on a high potassium diet, is it possible to excrete more potassium in the urine than it is filtered?
Yes, Kidneys activate to secrete potassium in the distal tubule and collecting duct, especially under the influece of aldosterone, allowing exretion to exceed the filtered amount.
In hypovolemia, is plasma angiotensin II concentration increased or decreased?
Plasma angiotensin II concetration is increased
Hypovolemia (low blood volume) triggers renin-angiotensin-aldosterone system (RAAS). Kidney angiostensin II helps restore blood volume and pressure, constricting blood vessels and stimulates aldosterone release. Promotes sodium and water retenion (Hypertension).
A patient has a tumour in the adrenal gland that continuously secretes large quantities of aldosterone (primary aldosteronism). Is the rate of potassium excretion normal, high or low?
Rate of potassium excretion in this case would be high. Aldosterone increases sodium reabsorption and potassium excretion in kidneys. Primary aldosteronism (caused by adrenal tumour), excessive aldosterone leads to increased potassium excretion urine. Potentially by hypokalemia (low blood potassium levels)
In a patient with severe renal artery stenosis (narrowing), which of the following is correct?
a. blood pressure (hydrostatic pressure) in the glomerular capillaries is increased
b. plasma angiotensin II concentration is decreased
c. plasma renin concentration is decreased
d. plasma aldosterone concentration is increased
e. systemic arterial blood pressure is increased
d. increased renin leads to more aldosterone, which enhances sodium and water retention to raise blood volume.
e. systemic blood pressure increases because angiotensin II causes vasoconstriction, and aldosterone promotes fluid retention. Both of which elevate BLOOD PRESSURE.
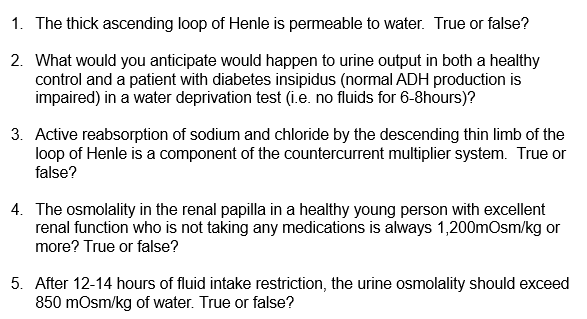
The thick asending loop of Henle is permeable to water. True or False?
False. It is impermeable to water, this segment actively transports sodium, potassium and chloride ions out of the filtrate but doesn’t allow water to pass. Helping to establish concentration gradient in the RENAL MEDULLA, which is essential for the kidney’s ability to concentrate urine.
The thin descending loop of Henle is permeable to water, facilitating water reabsorption.
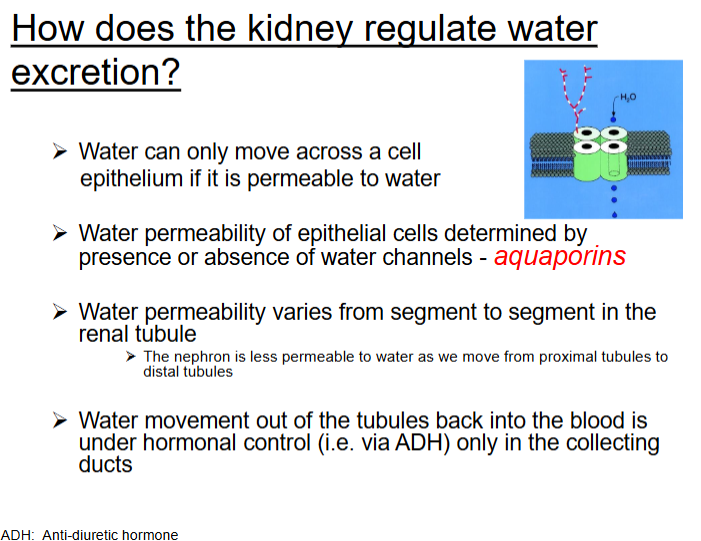
What would you anticipate would happen to urine output in both a healthy control and a patient with diabetes insipidus (normal ADH production is impaired) in a water deprivation test (e.g. no fluids for 6-8 hours)
Healthy Control: In a healthy individual, water deprivation stimulates the secretion of antidiuretic hormone (ADH), which increases the permeability of the collecting ducts to water, allowing water reabsorption. As a result, urine output decreases, and the urine becomes concentrated (high osmolality).
Patient with Diabetes Insipidus (DI): In a patient with diabetes insipidus, where ADH production or function is impaired, the kidneys cannot concentrate urine. Despite water deprivation, the kidneys fail to reabsorb water, leading to the production of large volumes of dilute urine (low osmolality). The urine output remains high.
Active reabsorption of sodium and chloride by the descending thin limb of the loop of Henle is a component to the countercurrent multiplier system. True or False
False. The descending thin limb of the loop of Henle is permeable to water but not to sodium or chloride. The active reabsorption of sodium and chloride occurs in the ascending thick limb of the loop of Henle, which is a key component of the countercurrent multiplier system. This system creates a concentration gradient in the renal medulla.
The osmolality in the renal papilla in a healthy person with excellent renal function is not taking any mdeications and always 1,200mOsm/kg or more? True or False?
True. In a healthy person with normal renal function, the osmolality in the renal papilla can reach 1,200 mOsm/kg or more. This high osmolality is essential for the kidney’s ability to concentrate urine and conserve water, a process supported by the countercurrent multiplier system in the loop of Henle.
After 12-14 hours of fluid intake restriction, the urine osmolality should exceed 850 mOsm'/kg of water. True or False?
True. After 12-14 hours of fluid restriction, a healthy person with normal renal function should be able to concentrate urine to an osmolality exceeding 850 mOsm/kg. This is due to the kidneys' ability to conserve water through the countercurrent multiplier system, which increases urine osmolality in response to dehydration.
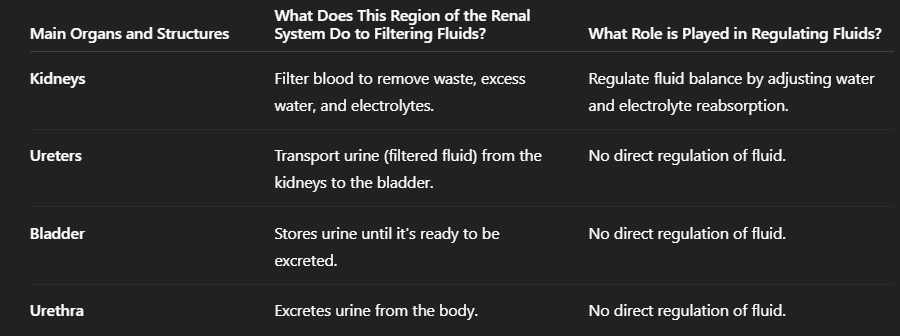
Features | What does this region of the Renal system do to filtering fluids? | How is the structure linked to the function? | What role is played for regulating fluids? |
Main organs and structure: Kidneys, ureters, urethra, bladder | -Kidney = filters blood to remove waste, excess water and electrolytes -Ureters = transport urine (filtered fluid) from the kidneys to the bladder -Bladder= Stores urine until ready to be excreted -Urethra= excretes urine from body | → Kidney= Filter blood - Shape: Bean-shaped → Ureters= - Transport urine from kidneys to bladder - Shape: Tubular → Bladder= - Store urine before micturition - Shape: Hollow, distensible organ → Urethra - Transports urine outside the body - Shape: Tubular, varying length | -Kidney= regulates fluid balance by adjusting water and electrolytes reabsorption -Role: Filter blood, regulate fluid, electrolytes, and pH. Reabsorb water and ions, excrete waste. Histology: Glomerulus: Fenestrated capillaries for filtration. Proximal tubules: Cuboidal epithelium with microvilli for reabsorption. Loop of Henle: Squamous epithelium for passive water movement, cuboidal for active ion transport. Distal tubule: Cuboidal epithelium for fine fluid regulation. Collecting ducts: Columnar epithelium with aquaporins (regulated by ADH). Ureters Role: Transport urine from kidneys to bladder. Histology: Transitional epithelium allows stretching. Smooth muscle layers for peristalsis. Bladder Role: Store urine; regulate volume before micturition. Histology: Transitional epithelium for stretch. Detrusor muscle (smooth muscle) expels urine. Urethra Role: Transport urine outside the body. Histology: Transitional epithelium near the bladder, stratified squamous at the opening. Skeletal muscle in external sphincter for voluntary control. |
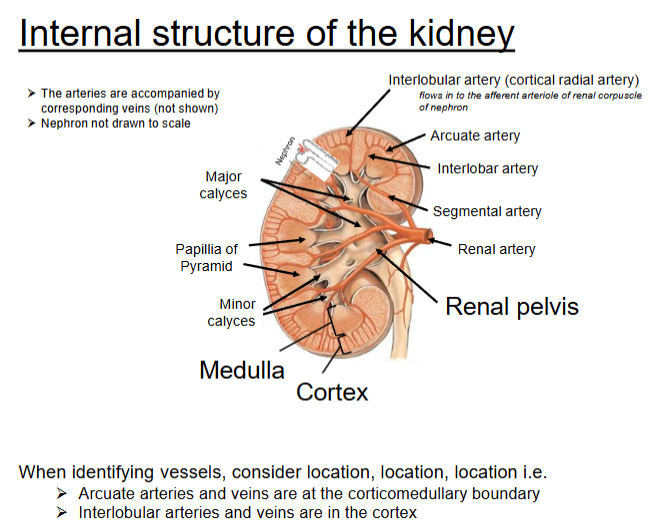
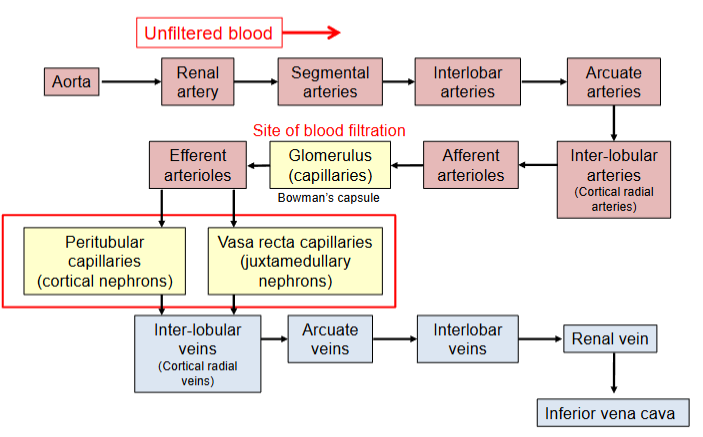
Anatomical components of Kidney: Cortex, medulla, pelvis, arteries, veins, capsule, nephrons | -Cortex= contains glomeruli and proximal/distal convoluted tubules, site of filtration (formed in glomeruili, reabsorption and secretion begin in tubules), filtrates water, electrolytes and small solutes move into tubules. -Medulla= contains loops of Henle and collecting ducts, concentrates urine and further reabsorption of water and salts -Pelvis= collects urine from collecting ducts, funnels urine into the ureter -Renal arteries= brings unfiltered oxygenated blood into the kidney, deliver blood to glomeruli for filtration -Renal veins= carry filtered, deoxygenation blood AWAY from the kidney -Nephron= functional units of kidney (~1 million+ per kidney), preform filtration (glomerulus, reabsorption, secretion and urine formation, spans both cortex and medulla. | → Cortex= - Outer region of kidney - Glomeruli: Fenestrated capillaries for rapid filtration → Medulla= - Inner region with renal pyramids - Thin limbs of Henle: Simple squamous for passive exchange → Pelvis= - Funnel-shaped space at hilum - Transitional epithelium (urothelium) for stretch and protection → Renal arteries= -Branch from aorta, enter kidney at hilum - Endothelium: Simple squamous, smooth muscle for autoregulation of blood flow and GFR → Renal veins= -Drain filtered blood from kidneys to inferior vena cava - Thin-walled, larger lumen than arteries → Capsule= - Tough fibrous layer surrounding the kidney. - Dense irregular connective tissue with collagen fibers for strength and durability → Nephron= - ~1 million per kidney, span cortex and medulla -Glomerulus: Fenestrated capillaries + podocytes | → Cortex= - Initial blood filtration (glomeruli) - Glomeruli: Fenestrated capillaries for filtration → Medulla= Maintains osmotic gradient (loops of Henle) - Thin limbs of Henle: Simple squamous epithelium for passive movement → Renal arteries= - Deliver blood to kidneys - Endothelium: Simple squamous + smooth muscle for autoregulation of blood flow → Renal veins= - Remove filtered blood from kidneys -Thin-walled vessels: Simple squamous endothelium → Nephrons - Glomerulus: Fenestrated capillaries + podocytes |
Functions of kidney
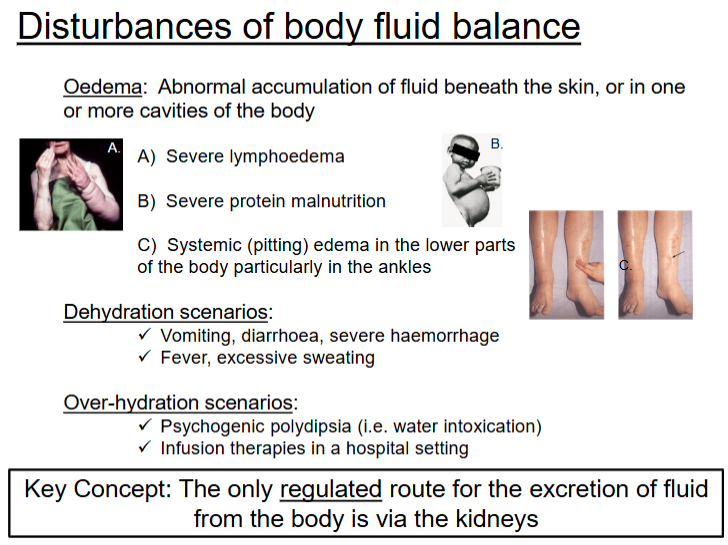
Regulation of water and electrolyte balance
vary output of water in ruine to match intake
independently vary output of different minerals (Na, K, Mg) depends on intake
Excretion of metabolic waste and bioactive substances
Excretes urea (from protein), uric acid (from nucleic acids)
Excretes drugs and hormones
Regulation of arterial blood pressure
Regulates blood volume
Renin production (Renin-Angiotensin-Aldosterone System (RAAS)
Regulation of erythrocyte (red blood cells) production
Kidney major site of Erythropoletin (EPO) production - released by fibrolast-like cells in the interstitium of the renal cortex and outer medulla
released when local tissue oxygen levels are reduced
EPO stimulates the bone marrow to increase production of erythrocytes and haemoglobin
Regulation of Vit D production
active form of vit D (calcitriol) is made in the kidneys
promotes calcium and phosphate absorption from the gut
rate of synthesis is regulated by hormones that control calcium and phosphate balance
Gluconeogensis (glucose synthesis)
synthesis of glucose from non-cabrohydrate sources
occurs during periods of fasting
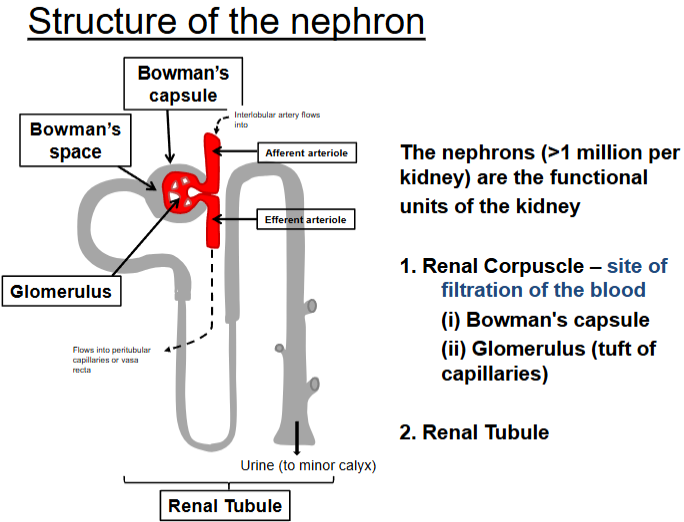
Nephron regulation in the body in internal environment
The nephron regulates the internal environment of body by filtration (at the renal corpuscle) followed by selective modification of the filtrate as it passes through different regions of nephron
Regulation of the plasma composition occurs via three processes:
filtration
reabsorption
secretion
Urine formation
begins with the filtration of plasma from the glomerular capillaries into bowman’s space, termed as glomerular filtration and the filtrate is called glomerular filtrate or ultra filtrate
Selectively of filtration barrier determined by:
molecular size of intravascular components
electrical charge of filtration barrier components