DP 2 Biology - topics 6.4, D.6 & 11.3
Topic 6.4: Gas Exchange & D.6 Transport of Respiratory Gases
Why do organisms need a system for Gas exchange:
Provide O2 for aerobic cellular respiration
remove waste from bloodstream
exchange btw environment and cells
need high SA
need moist membrane
Respiratory System:
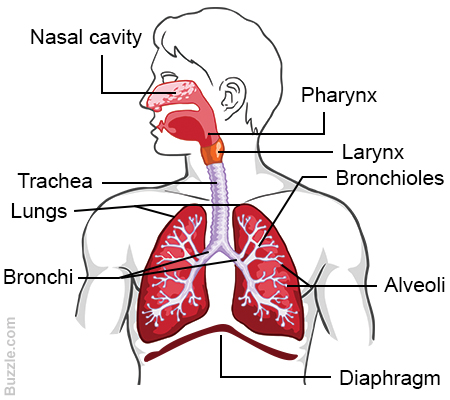
What is the path that air must take to travel into the lungs?
air enters through the nasal and oral cavities & is warmed
it passes the traches and into the branching of the Bronchi
The Bronchi then is further branched into Bronchioles which conduct air into the alveoli
Ventilation: Muscular pumping mechanism that moves air in and out of the lungs efficiently, thereby maintaining a concentration gradient for diffusion
How does it help?
Helps keep a gradient to allow for diffusion btw the air in alveoli & adjesten capillaries
How do the features of the alveoli specialized for gas exchange:
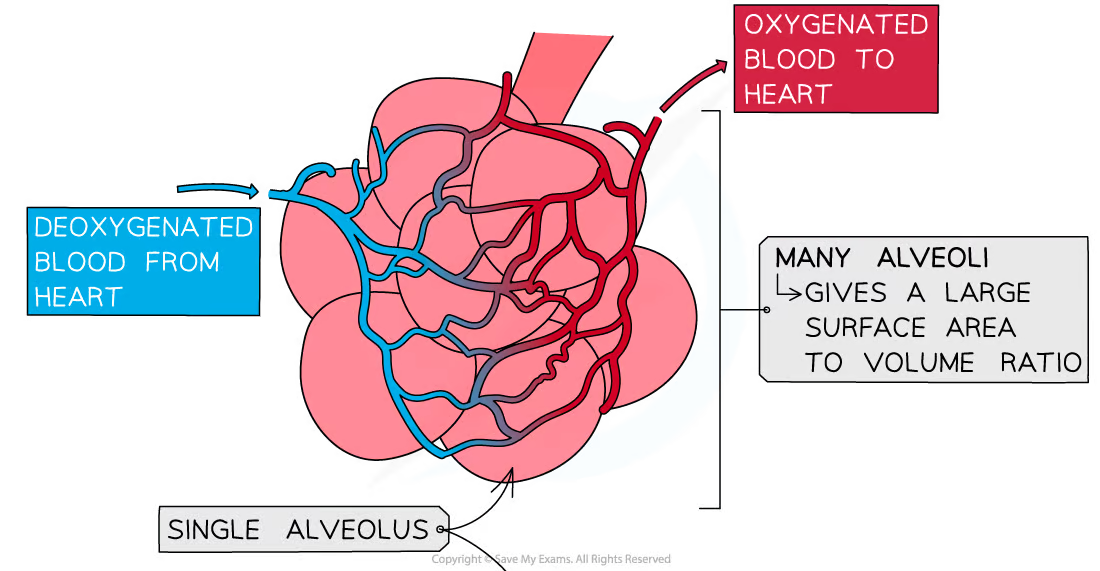
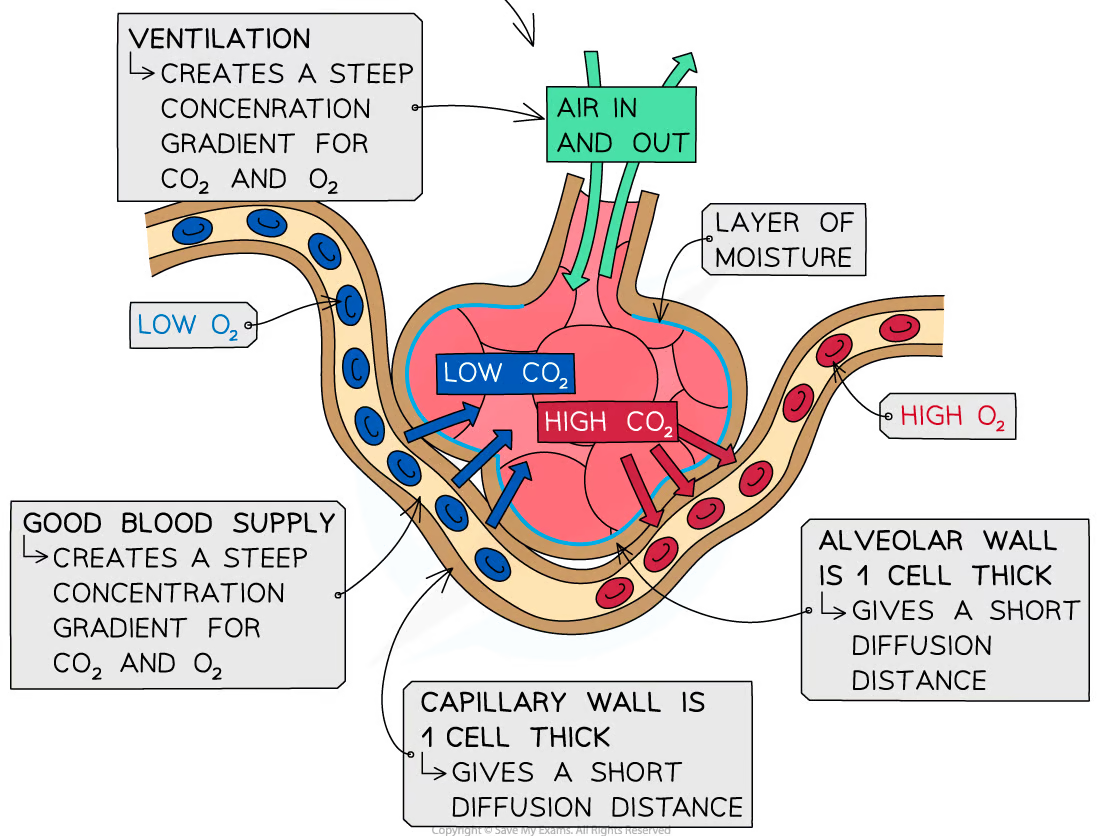
During Inhale: O2 passes from alveoli to blood bia diffussion
During Enhale: CO2 passes from blood to alveoli bia diffussion
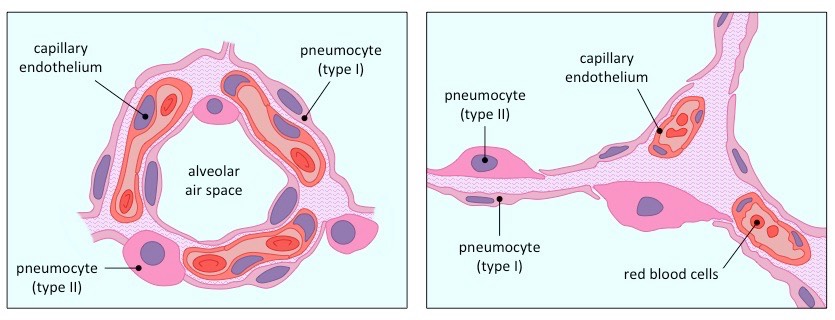
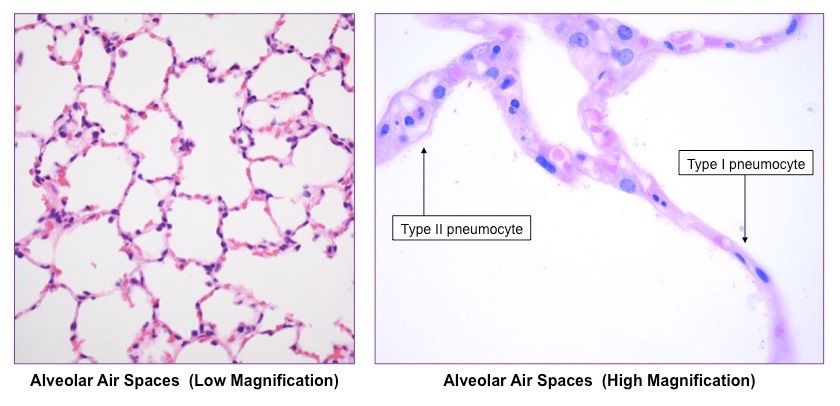
Pneumocytes: Cells of the Alveoli:
2 major types of cells that compose the structure of an alveolus:
Type 1:
extremely thin alveolar cells adapted to carry out gas exchange.
flattened cells
Type 2:
secret a solution containing surfactant that creates a moist surface inside the alveoli (helps disolve gasses) to prevent the sides of the alveolus adhering to each other by reducing surface tension.
the film of moisture allows O2 in the alveolus to dissolve and then diffuse to the blood in the alveolar cappillaries also providing an area form which CO2 can evaporate into the air and be exhaled.
What if a baby is born prematurely?
Because their pneumocytes have not produced enough surfactant they can suffer drom respiratory disstress syndrome. Which is treated by giving the baby oxigen as well as one or more doses of surfactant, extracted form animal lungs.
Hemoglobin & Oxigen Dissociation Curbes:
Background information about Hemoglobin:
Made of 2 alpha and 2 beta tertiary structures to create a Quaternary protein
Has iron as co-factor (heme group)
Holds onto both O2 and CO2 when transported arround body
What are Oxigen Disspciation Curbes?
they are graphs that show hemoglobin’s affinity for oxigen.
the degree in which oxigen binds to hemoglobin is determined by the partial preasure of O2 (pO2)
How does the location where O2 is being used change the affinity of hemoglobin?
at low pO2, few heme groupd are bound to oxigen, so hemoglobin doesn’t carry much O2
at higher pO2 more heme groups are bound to O2 making it easyer for more O2 to be picked up
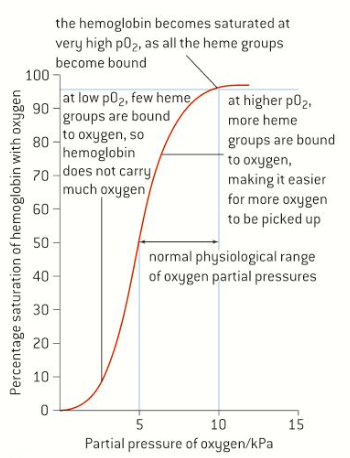
The dissocation curve shown in Figure 1 descrives the saturation of hemoglobin by O2 at different pO2
*note that the significant change in saturation over a narrow range of pO2. This narrow range typifies O2 pressures surrounding cells under normal metabolism. At low pO2, such as might occur in the muscles, O2 will dissociate form Hemoglobin. At high pO2, such as might occur in the lungs, the hemoglobin will become saturated.
Carbon Dioxide transport in the Blood:
CO2 is carried in solution and bound to hemoglobin in the blood.
CO2 is carried in 3 forms though plasma:*
Dissolved as CO2 (CO2 + H20 = Carbon dioxide + water)
Reversibely converted into bicarbonate ions (HCO3^-) that are dissolved in plasma proteins (HCO3^- + H^+ = Bicarbonate Ion)
Bound to plasma proteins (H2CO3 = Carbonic Acid)
*the three reactions are reversible.
CO2 formed during cellular respiration is converted into a more soluable and less toxic bicarbonate ion. The reaction occurs in red blood cells and is catalysed by the enzime Carbonic anhydrase.
In the tissues where CO2 is generated, the reaction leans more onto creating more bicarbonate ions as well as H+ ions. Which lowers the pH of the blood. In lungs, when CO2 leaves the blood the reaction is triven back to converting to CO2
(more H^+ ions = lower pH = more acidic (pH - __p__otential __H__idrogen)
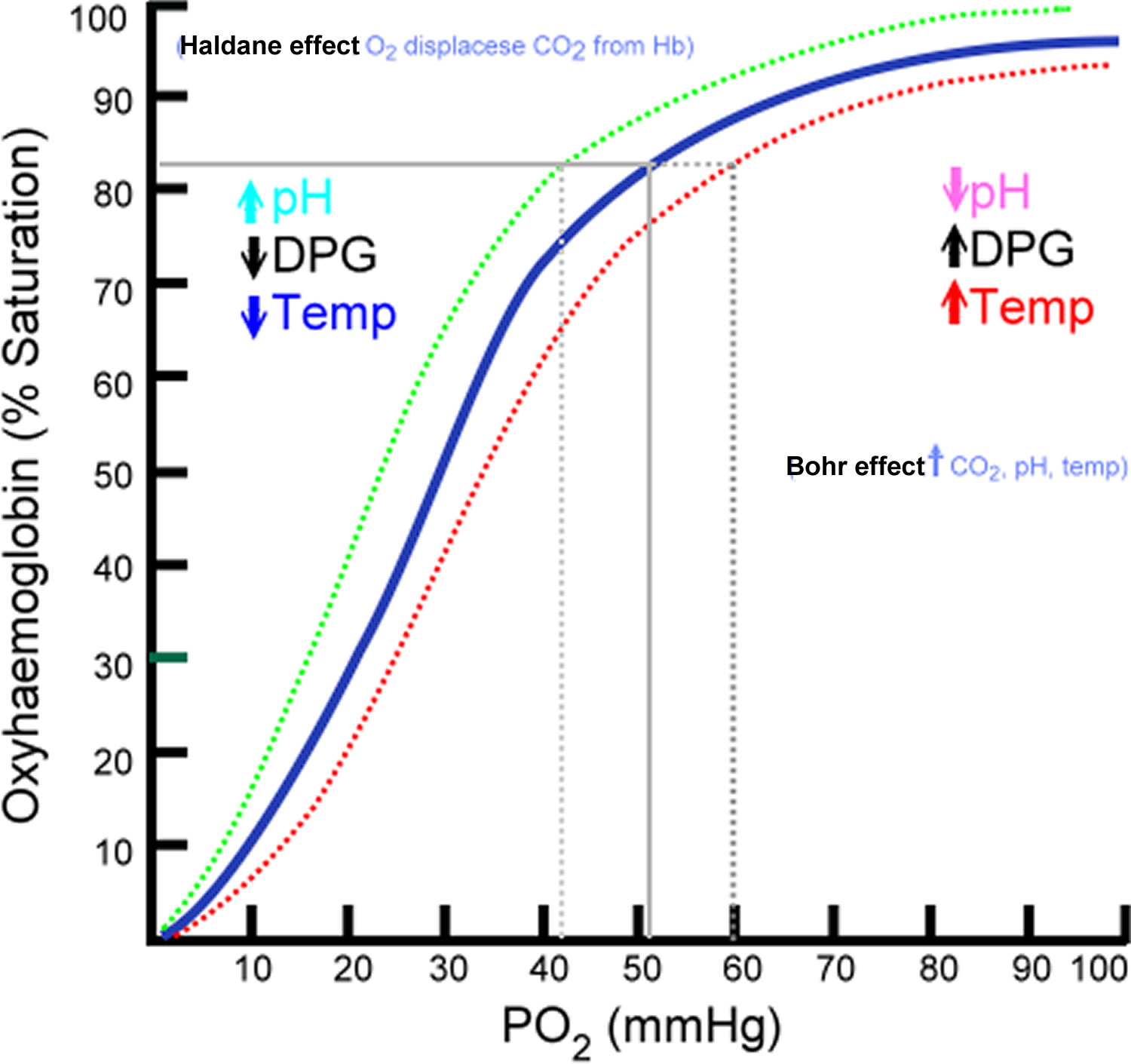
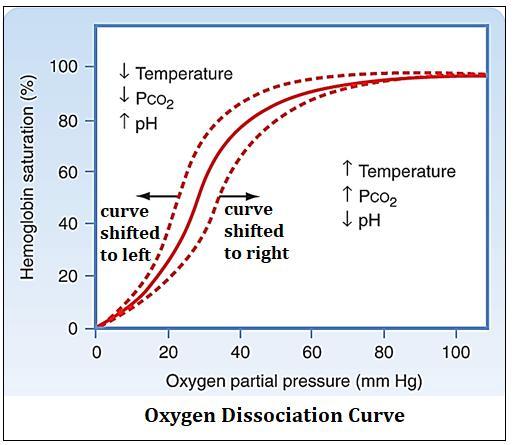
How does the amount of CO2 impact the affinity of oxigen in Hemoglobin (AKA The Bohr Shift)
Bohr Shift - ecplains the increased release of O2 by hemoglobin in respiring tissues.
Increased metabolism results in higher release of CO2 into blood lowering its pH (an increase of CO2 causes the release of more H+ ions causing the pH drop). The increase in acidity shifts the pO2 curve to the right resulting in a decreased in affinity of the hemoglobin for O2: that is, a greated release in O2 form hemoglobin at the same partial preasure of O2.
This is know as the Bohr shift which ensures that respiring tissue have enough O2 when they need for it is greatest.
Summarized form: The Bohr shift is caused by the response of red blood cells to a shift in their environment (a decrease in pH, aka more acid) where they maximize the hemoglobin-oxygen binding capacity in the lungs while simultaneously optimizing oxygen delivery to the tissues with the greatest demand.
Graph representation of The Bohr Shift:
CO2 & ventilation rate:
During active exersise the rate of ventilation adapts in response to the amount of CO2 in the blood.
But what triggers this? What monitors and regulates the pH of blood?
Chemoreceptors in the Medulla Oblongata (brain) as well as the nerves near the heart detect the lower pH. In case of sensing a drop in pH they response through increaseing ventilation (signal to diaphragm and lung muscles), meaning remove the CO2, which also mean increase the O2.
Exersise increases metabolism leading to an increase in CO2 production as waste product in cellular respiration. The increase of CO2 leads to a drop in the pH of blood since CO2 dissolves in water to form carbonic acid further dissociating into H+ and HCO^-. Chemoreceptors are able to detect the chift in pH and under high levels of CO2 it triggers and increase in the ventilation rate to get the body rid of the buildup of it. (Hyperventilation)
Hyperventilation - mechanism in response of vigorous exercise as a mechanism to maintain blood pH and rid the body of the CO2.
Adaptations for human populations living at high altitudes: (think the Sherpa population in Nepal)
greater lung SA
greater vital capacities
oxygen dissociation curves shifts to the right encouraging release of oxygen into tissues.
Types of Hemoglobin:
Hemoglobin vs Myoglobin
Hemoglobin:
Description: Made of 2 α and 2 β tertiary structures to create a Quaternary protein. Has iron as a cofactor (heme - group). Found in red blood cells. Holds onto both O2 and CO2 when transported around the body.
Myoglobin:
Description: A specialized O2 transport protein in muscles that has a much higher afinity ofr O2 and will only release it when the pO2 is prerry low (for example in the muscles during heavy exersice)
Graph:
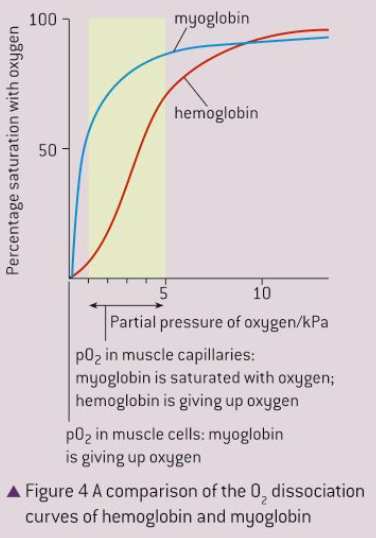
Why are they different?
Hemoglobin has 4 chains with 4 heme groups, while myoglobin only has 1. The release of each O2 form hemoglobin triggers a conformational change which causes the hemoglobin to more rapidly release subsequent O2 molecules.
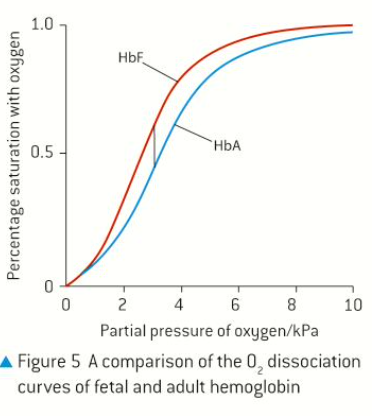
Adult Hemoglobin vs Fetal Hemoglobin:
Adult Hemoglobin (HbA)
Fetal Hemoglobin (HbF):
Description: Has a higher affinity along all pressures, which ensures that O2 is transferred to the fetus from the mother’s blood across the placenta. (this causes the slope of the curbe for HbF to be higher than HbA)
Graph:
Pulmonary diseases:
Lung cancer:
Causes:
genes & smokeing
Consequences:
Tumors reduce SA/reduce function, take nutrients away from healthy tissue (due to quick growth & division) and take up space.
Emphysema
What is it?
It’s a lung condition that causes shortness of breath. In people with emphysema, the air sacs in the lungs (alveoli) are damaged. Over time, the inner walls of the air sacs weaken and rupture — creating larger air spaces instead of many small ones. This reduces the surface area of the lungs and, in turn, the amount of oxygen that reaches your bloodstream**.**
Cause/s:
Smoking
Consequences:
Damage to alveoli = reduced SA
There are less capillaries to perform the gas exchange.
Because of these, individuals have a more difficult time breathing, feel tired, low energy, etc.
Treatments:
The damage that is done is not reversible, but refraining from smoking can stop any further damage.
People with this kind of damage will need to use an oxygen tank to help deliver a higher concentration of O2 to their lungs.
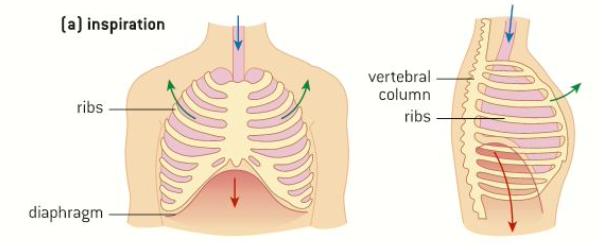
Ventilation:
What role do muscles play in it?
assist in the movement of air into and out of the lungs by creating preasure differences.
Antagonistic Muscle Pairs:
When a muscle is contracted, it shortens.
When a muscle is relaxed, it elongates.
Muscles work in pairs—so when one contracts, a second muscle is elongated by the first.
Negative pressure:
Negative pressure breathing.
air is pulled into lungs
during inhale.
Diaphragm moves down & expands chest cavity.
Rib Cage moves up and out to expand chest cavity.
Inhalation
Goal: Increase the volume of chest cavity---this will reduce pressure causing air to be sucked in!
Giaphragm - moves down & expands chest cavitie
External intercostal muscles - contract, pulling ribcage up and out
internal intercostal muscles - relax
rib cage - expand
Volume of chest cavitie - increase
Pressure in chest cavitie - decrease
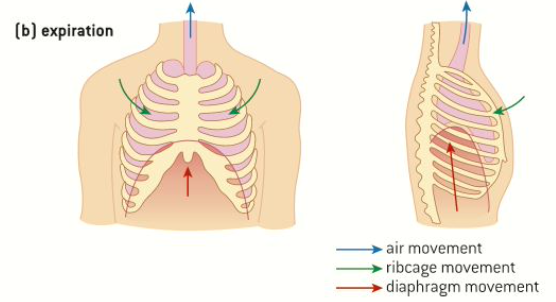
Exhalation:
Giaphragm - moves up (relaxes)
External intercostal muscles - relax
Internal intercostal muscles - contract (move ribcage down and in)
only work when contract
rib cage - down and in
Volume of chest cavitie - decrease
Pressure in chest cavitie - increase
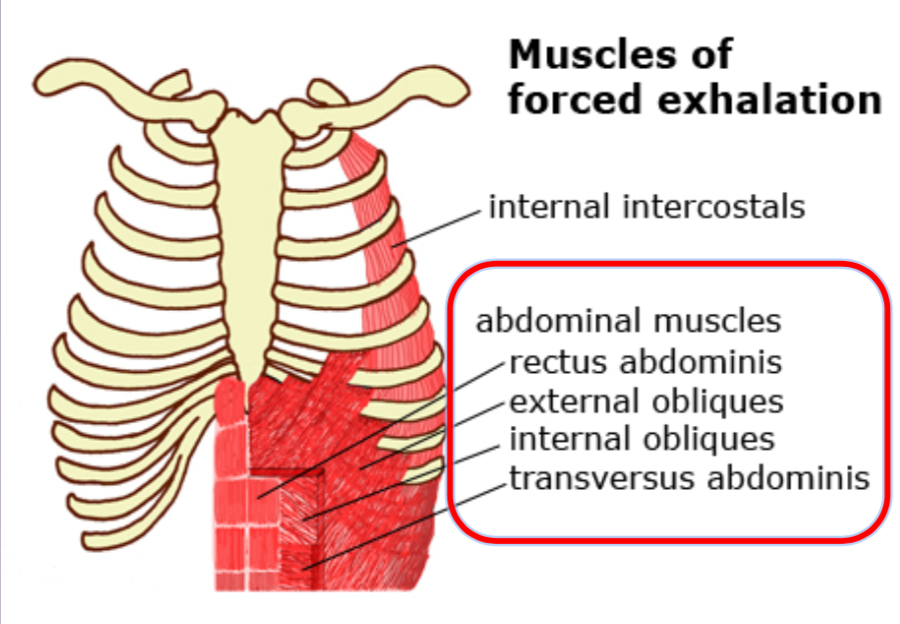
What happens during forced exhalation?
During forced exhalation, abdominal muscles contract which pushes diaphragm up and forces more air out
Topic 11.3: The Kidney & Osmoreculation
Terms:
Excretion - the removal of waste products of metabolic pathways from the body. This is necessary to maintain homeostasis.
Osmolarity - the solute concentration of a solution.
Osmoregulators - the active maintenance of the solute concentration of an organism's fluids to manage an organism's water content
Animals are osmoregulators; we use kidneys to make sure blood stays at consistent concentration
Paramecium use contractile vacuoles to regulate the amount of water in their cell
Osmoconformer - an organism whose body fluid solute concentration is the same as the solute concentration of its external environment.
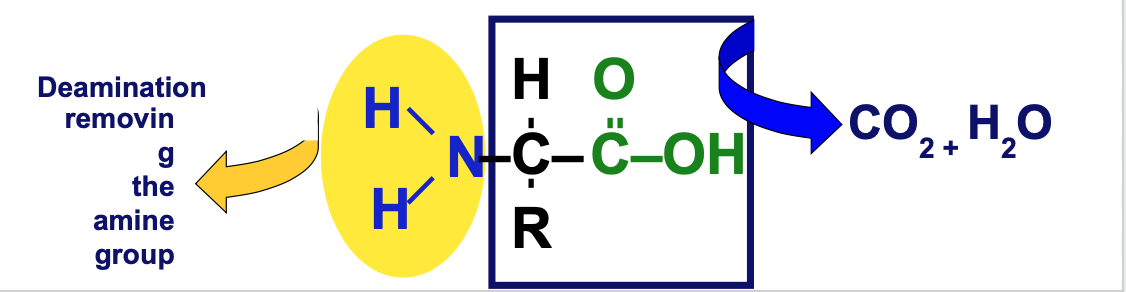
How is neutrogenous waste formed?
What waste products?
what do we digest our food into…
carbohydrates = CHO → CO2 + H2O
lipids = CHO → CO2 + H2O
proteins = CHON → CO2 + H2O + N
nucleic acids = CHOPN → CO2 + H2O + P + N
relatively small amount in cell
Nitrogenous waste disposal:
When amino acids are broken down, amine group is released which forms ammonia (NH3)
very toxic must dilute it & get rid of it… fast!
How you get rid of nitrogenous wastes depends on:
who you are (evolutionary relationship)
where you live (habitat)
How do different animals excrete the nitrogenous waste?
Aquatic organisms (Fish)
can afford to lose water
ammonia
most toxic
Terrestrial (Mammals)
need to conserve water
urea
less toxic
Terrestrial egg layers (birds)
Shells not permeable to dissolved urea
uric acid
least toxic
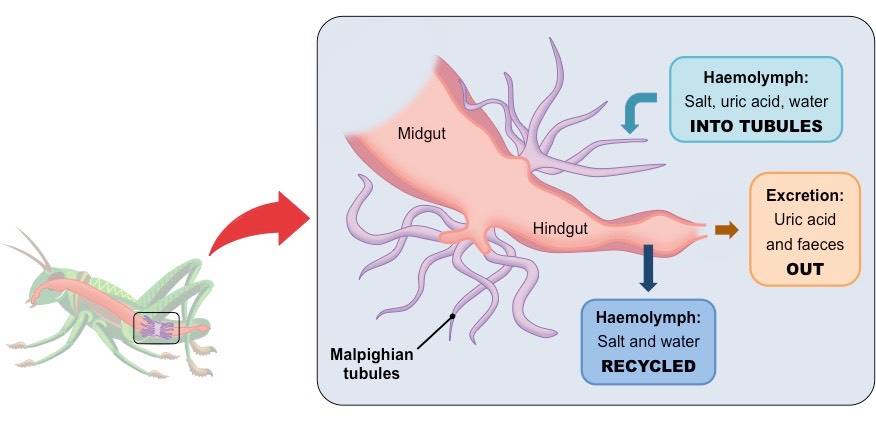
How are nitrogenous wastes excreted in arthropods (insects)
The Malpighian tubule system in insects carries out osmoregulation and removal of nitrogenous wastes.
Anthropods have a circulating fluid, know as hemolymph, that combines the characteristics of tissue fluid & blood. Osmoregulation is a form of homoeostasis whereby the concentration of hemolymph, or blood in the case of animals with closed circulatory systems, is keptwithin a certain rance.
Insects have tubes that branch off form their interstinal tract. Cells lining the tubules actively transport ions and uric acid form the hemolymph into the lumen of the tubules. This draws water by osmosis from the hemolymph through the walls of the tubules into the lumen. The tubules empty their contents into the gut. In the hindgut most of the water and salts are reavsorved while the nitrogenous waste is excreted with feces.
Simpler definition: Malpighian tubes are blind ended ducts that branch off their intestinal tract. The cells here actively transport compounds to osmoregulate.
Kidney anatomy:
Function of the kindey:
Filtration: Kidneys process about 120-150 quarts of blood to sift out about 2 quarts of waste products and extra water.
Osmoregulation: prevent the buildup of wastes and extra fluid in the body and keep levels of electrolytes stable (Na+, K+, PO4)
Blood composition in renal artery and vein:
Renal Artery:
higher amounts
Renal Vein:
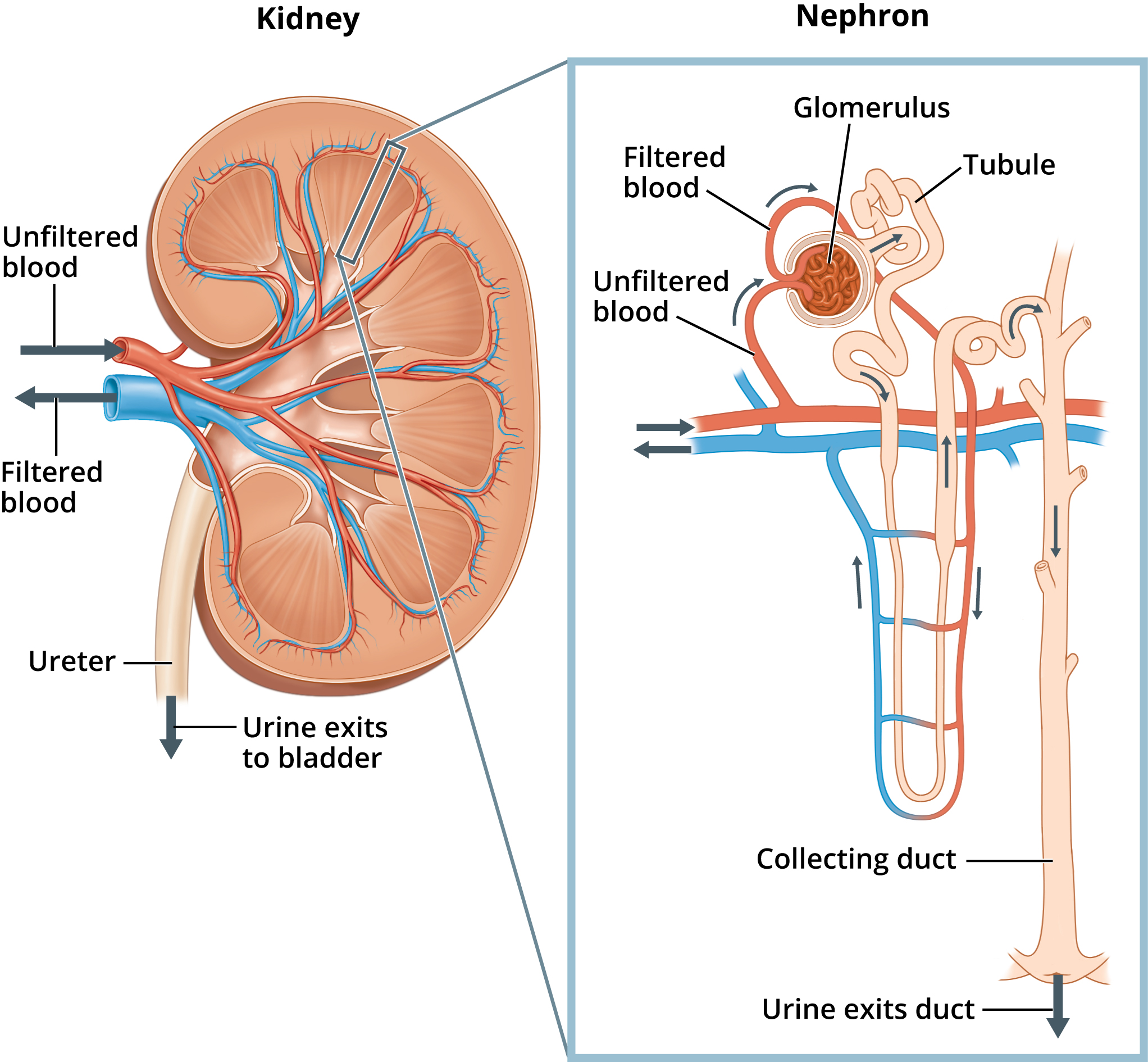
Nephron anatomy:
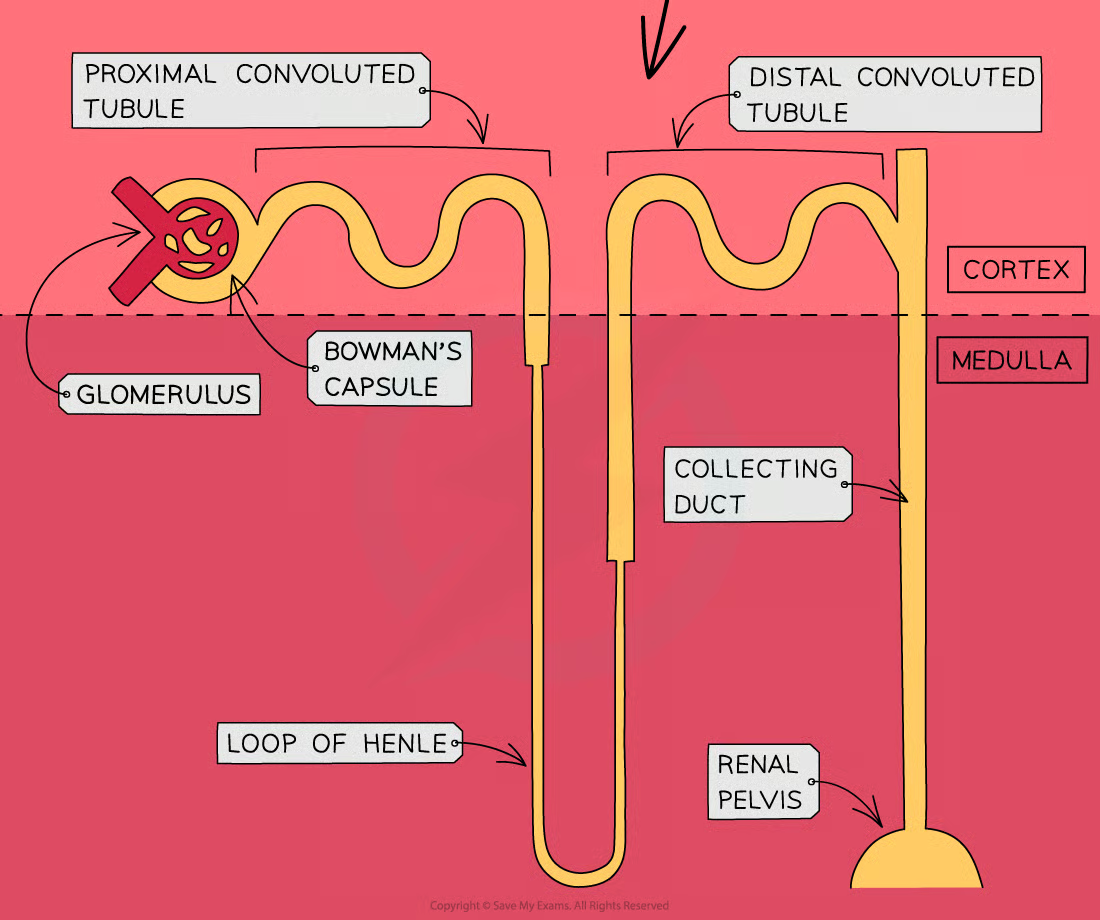
Functions: