Critical Care and Hemodynamic Monitoring Study Guide
Critical Care and Hemodynamic Monitoring
Role of the Critical Care Nurse
Critical care nurses require:
Astute assessment skills.
Clinical judgment.
Ability to provide complex nursing support, including:
Vasoactive medications and titrations.
Polypharmacy.
Mechanical ventilation.
Hemodialysis (HD) or Continuous Renal Replacement Therapy (CRRT) → dialysis 24/7.
Intracranial pressure (ICP) monitoring.
Hemodynamic monitoring (CO, BP, HR and rhythms, RR)
Critically ill patients are at high risk for serious complications.
ICU Admission Criteria
Patients sent to the ICU are typically:
Physiologically unstable.
At risk for serious complications requiring frequent assessments and invasive interventions.
Need intensive nursing support related to IV medications and/or advanced technology.
Some post-surgical patients
Ex. Pt has a lap cholecystectomy that turns into an open cholecystectomy and must leave belly open for a few days.
Critical Care RN Skills
Critical Care Registered Nurses (RNs) require:
Advanced assessment skills with higher frequency, continuous monitoring, and trending patterns.
Cranial nerves, etc.
In-depth knowledge of pathophysiology and pharmacology.
The ability to anticipate, recognize, and act on complications.
Ex. Subtle changes in BP, urine output decreasing every few hours, etc.
Proficiency in managing advanced biotechnology.
Effective communication and collaboration with interdisciplinary team (IDT) members.
Ex. Rounds → all team members involved; how patient did overnight and any concerns for today. Family recommended to be around.
Common Patient Problems in Critical Care
Immobility, which may necessitate restraints or devices.
Most patients are sedated, restrained, or intubated.
Even if pts are ventilated, they need to be mobilized (ex. Sitting on edge of bed for 10-15 mins).
Communication difficulties due to nonverbal status or cognitive impairment.
Nutritional considerations:
Enteral vs. parenteral nutrition.
Enteral: mesenteric ischemia, traumatic injury in abdomen or face = contraindicated.
Enteral preferred. Start early.
Pain management (observed), which can be challenging in nonverbal patients; unmanaged pain can lead to agitation and anxiety.
Pain observation = what does pain seem to be?
Anxiety stemming from fear of the unknown, loss of control/independence, unfamiliar surroundings, and impaired communication.
Sleep disturbances caused by environmental noise and frequent interruptions for assessments and medications.
Lights on during day, lights low or off during night.
Cluster care.
Sensory issues, including delirium from sensory overload → common.
Agitation and Confusion Assessment Scales
Richmond Agitation-Sedation Scale (RASS)
A tool to assess the level of consciousness and agitation in patients. Do this with neuro checks (minimum q4h).
Levels range from:
+4 (violent) to -5 (comatose/completely unresponsive).
Ideal to be between -1 (drowsy & easily arousable) and +1 (slightly anxious, not aggressive).
Scores indicate the degree of agitation or sedation, guiding appropriate interventions.
Confusion Assessment Method for the ICU (CAM-ICU)
Used to assess for delirium in ICU patients.
Involves assessing for:
Acute change or fluctuating course of mental status? (ex. AOx4 → AOx1 = yes, move down flowsheet).
Inattention (e.g., squeeze hand when 'A' is said in a sequence → spell “CASA BLANCA” → allow up to 2 errors, if 2+ errors move down flowsheet).
Altered level of consciousness (RASS score → score other than 0 means ICU delirium)
Disorganized thinking (answering yes/no questions).
A patient is considered delirious if they have features 1 and 2, along with either feature 3 or 4.
Pain Assessment: Critical-Care Pain Observation Tool (CPOT)
A behavioral pain assessment tool for nonverbal patients.
Evaluates:
Facial expressions (0-2) →
0 = Relaxed
1 = Tensed
2 =Grimacing
Body movements (0-2).
0 = Absent or normal movements
1 = Protection (against painful stimuli)
2 = Restlessness and agitation
Compliance with ventilation or vocalization (0-2) (as applicable).
Muscle tension (0-2).
0 = Relaxed
1 = Tense, rigid
2 = Very tense and rigid.
Total score ranges from 0-8, with higher scores indicating greater pain.
Family-Centered Care
Involves family participation in patient care to:
Connect patients to their previous reality.
Offer support and assistance at the bedside.
Provide factual information to the healthcare team.
Function as healthcare decision-makers.
However, be aware that family involvement can sometimes do more harm than good, necessitating patient advocacy.
Addressing family issues includes:
Communicating the plan of care, including medical and nursing goals.
Explaining procedures and tests.
Providing access to their loved ones.
Ensuring cultural sensitivity.
Allowing presence during care, procedures, or resuscitation attempts, and IDT rounds (if appropriate).
Addressing end-of-life issues.
Advocate for pt who has poor prognosis → would an elderly pt want to be full code?
Hemodynamic Monitoring
Basic Terminology**
Systemic Arterial Pressure: Regular BP
**Mean Arterial Pressure (MAP): Calculated as MAP = (SBP + 2DBP) / 3
70 is normal (in ICU there will be acceptable parameters like 60-65)
Pulmonary Arterial Pressure (PAP): Pressure within the arteries of the lungs
Viewing CO values for cardiac pts
**Central Venous Pressure (CVP): Normal range is 2-8 mmHg.
Indicator of fluid volume status and if there’s enough fluid to perfuse the organs.
If CVP is 1, then we are hypovolemic.
If CVP is 12, 13, 15 = hypervolemia, which could lead to fluid overload and potential heart failure if treatment is not initiated.
Pulmonary Artery Wedge Pressure (PAWP): Normal range is 6-12 mmHg.
Pressure we measure when wedging catheter into artery and inflating balloon.
Assesses left ventricular function and reflects the left ventricular and diastolic pressure.
Cardiac Output (CO) / Cardiac Index (CI):
Normal CO range is 4-8 L/min.
CO=SV\cdot HR
CI = CO / BSA
Stroke Volume (SV) / Stroke Volume Index (SVI)
**Systemic Vascular Resistance (SVR): Calculated as SVR=(MAP-CVP)\cdot80/CO
Pulmonary Vascular Resistance (PVR): Resistance in pulmonary vascular bed.
Types of Invasive Pressure Monitoring
Arterial Blood Pressure (ABP) monitoring
Arterial Pressure-Based Cardiac Output (APCO)
Pulmonary Artery Flow-Directed Catheter (Swan-Ganz catheter)
Central Venous Pressure (CVP) / Right Atrial Pressure Measurement
Purposes of Invasive Hemodynamic Monitoring
Early detection, identification, and treatment of life-threatening conditions, such as: Want to identify deterioration quickly
Cardiogenic pulmonary edema
Non-cardiogenic pulmonary edema (ARDS)
Cardiac tamponade
Shock (all types)
Evaluate effectiveness of treatment with:
Drugs (vasoactive medications)
Ex. Norepinephrine → we’ll be titrating up and down based on the patient's blood pressure response
Mechanical ventilatory support
Components of Pressure Monitoring Systems
Bedside monitor: Contains the amplifier to increase signal size.
Transducer: Converts mechanical pressures of the pulse into electrical energy; must be leveled to the phlebostatic axis for accurate readings (flushing device).
Recorder: Records the information.
Zeroing: Calibrates the system to atmospheric pressure.
**Radial is easiest access point
Arterial Line Monitoring
Invasive catheter placed in an artery for continuous arterial pressure monitoring.
Pressure tracing should show a P wave and correlates with ECG (if clotted off → might see tall spikes which means recalibration needed).
Arterial line always red, CVP is blue, pulmonary catheter is yellow.
Placement: Loop around patients thumb to prevent it being pulled out.
Allows visualization of arterial pressure tracing with:
QRS complex on ECG with corresponding arterial waveform
Dicrotic notch
Systolic and end-diastolic pressures
Ulnar artery occlusion test is performed to assess collateral circulation.
Square Wave Test
Performed to assess the dynamic response of the arterial line system.
A fast flush is activated and quickly released, producing a sharp upstroke followed by a rapid downstroke extending below baseline with 1-2 oscillations within 0.12 seconds and a quick return to baseline.
The pressure waveform should be clearly defined, including the dicrotic notch.
If that doesn’t work → Is it clotted?
Complications of Arterial Monitoring
Necrotic tissue
Often happens if wrong medication is given through arterial line.
Hemorrhage
Thrombus formation
Neurovascular impairment
Loss of limb
Infection
Waveform abnormalities:
Normal waveform
Overdamped waveform
Underdamped waveform
Arterial Pressure-Based Cardiac Output (APCO)
A minimally invasive method for continuous CO measurement.
Usually used for cardiac patients who’ve gone through cardioversion.
Attaches to a traditional arterial line.
Assesses the patient's ability to increase SV in response to fluid administration (preload responsiveness).
Helps determine if the patient would benefit from additional IV fluids.
Uses arterial waveform data plus demographic information.
Often used with central venous oxygen saturation (CVO2) catheter.
O2 sat of blood return to the heart after defibrillation
Pulmonary Artery Catheter (Swan-Ganz Catheter)
Used for hemodynamic monitoring but carries a high risk of complications if used without proper knowledge.
Was primarily used to monitor hemodynamic status of patients
Indications for PA Catheter Use
Assessment of response to therapy in mixed types of shock.
Cardiogenic shock
Pulmonary hypertension (PAH)
Myocardial infarction (MI) with complications such as heart failure.
Potentially reversible systolic heart failure.
Severe chronic heart failure requiring vasoactive drug therapy.
Transplantation workup.
Contraindications for PA Catheter Use
Coagulopathy (Clotting disorder)
Huge risk when inserting a catheter because clots will form around it.
Endocardial pacemaker
Endocarditis
Mechanical tricuspid or pulmonic valve
Right heart mass (thrombus or tumor)
PA Catheter Components and Insertion
Components include:
Distal lumen hub
Proximal infusion lumen hub
Balloon inflation valve: measure wedge pressure (only insert air and use catheter it came with)
Thermistor connector
Thermistor sensor
Proximal injectate port
Balloon
Prior to insertion:
Check electrolyte levels and coagulation studies.
Particularly magnesium and potassium electrolytes
INR/PT and PTT
Prepare necessary monitoring equipment.
Insertion sites include the internal jugular (IJ), subclavian, axillary, or femoral vein.
Observe waveforms as the catheter is advanced.
Confirm positioning with chest X-ray.
Secure the catheter and record the measurement at the exit point.
Measured every shift
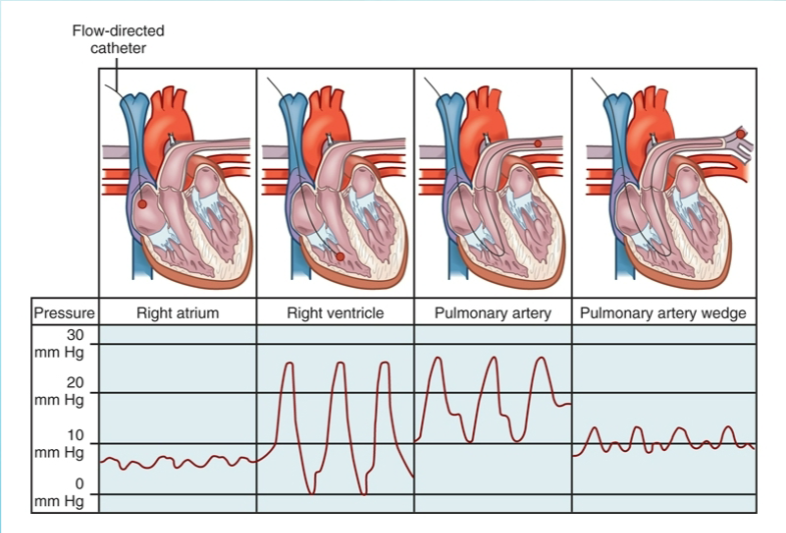
Positional Waveforms During PA Catheter Insertion (in order)
Right atrium
Right ventricle
If cath dislodged here = increased risk for ventricular dysthymia’s
Pull out into right atria (less likely for a dysrhythmia in atria than ventricle → tell provider after)
About 5 cm or so to pull into atria
Pulmonary artery
This is here the cath should sit
Pulmonary artery wedge
Central Venous Pressure (CVP) / Right Atrial Pressure
Reflects fluid volume status.
Usually measured with a CVP catheter in the IJ or subclavian vein.
Can also be measured with a PA catheter.
CVP is the mean pressure at the end of expiration.
High CVP indicates right ventricular failure or volume overload.
Low CVP indicates hypovolemia (ex. trauma or liver failure).
Pulmonary Artery Wedge Pressure (PAWP)
Measured from the distal port of the catheter when the balloon is inflated, "wedging" the catheter in a small PA branch.
PAWP reflects the preload of the left heart.
Normal range: 6-12 mmHg.
Elevated in left-sided heart failure.
High PAWP indicates volume overload
Treatment includes diuretics and inotropes if left ventricular dysfunction is present.
Low PAWP indicates volume deficit
Treatment includes IV fluids.
Systemic Vascular Resistance (SVR) and Pulmonary Vascular Resistance (PVR)
Calculated on monitor, not directly measured with a PA catheter.
Both measure afterload: the resistance the ventricle overcomes to pump blood into the systemic circulation.
SVR: SVR = 800-1200 \frac{dyn \cdot s}{cm^5} : Afterload of the left heart
Low SVR: Use vasopressors to increase vascular tone.
High SVR: Use vasodilators and positive inotropes.
PVR: PVR < 250 \frac{dyn \cdot s}{cm^5} : Afterload of the right heart
Low PVR: Can be due to overuse of vasodilators.
High PVR: Treat the underlying cause (e.g., oxygen, diuretics, bronchodilators).
Nursing Management for Invasive Hemodynamic Monitoring
Integrate data from multiple sources.
Collect baseline data.
Trending upward? Downward?
Assess the patient's appearance.
Perform a full physical assessment.
Recognize early cues of deterioration.
Intervene before a decline occurs.
Complications of Invasive Hemodynamic Monitoring
Infection/sepsis: Prevent with central line bundle, occlusive dressings (change PRN), and Biopatch at the insertion site.
Dislodgment into the right ventricle (RV): Can cause ventricular dysrhythmias; requires immediate notification of the physician and pulling the catheter back into the right atrium.
Air embolism: Caused by overinflating the balloon, leading to rupture.
Thrombus: Clot formation on the end of the catheter can result in pulmonary embolism.
Pulmonary infarction/PA rupture: Considered an emergency, requires immediate notification of the physician.
Can occur when the balloon is left inflated too long or the catheter migrates too far into the pulmonary artery.
Never inflate the wedge balloon beyond its capacity (1-1.5 mL) or for longer than 8-15 seconds.
Mechanical Circulatory Support Devices
Intra-Aortic Balloon Pump (IABP)
Temporary mechanical support device.
Reduces afterload.
Improves coronary blood flow.
IABP therapy = counterpulsation.
Hemodynamics of IABP
Helium is rapidly shuttled into and out of the balloon (about 40 mL).
Helium is less risk for air embolism
Inflation displaces blood superiorly and inferiorly, perfusing coronary arteries and other organs.
Diastole → balloon inflated
Systole → deflate (vacuum-like pressure)
Deflation drops pressure within the aorta, reducing afterload.
ECG rhythm triggers inflation and deflation.
Dicrotic notch in arterial pressure tracing refines timing.
IABP assist ratio is 1:1.
Every heart beat, balloon deflates and inflates
Indications
Acute MI
Ventricular aneurysm accompanied by ventricular dysrhythmias
Acute ventricular septal defect
Acute mitral valve dysfunction
Cardiogenic shock, pre-shock syndrome
Refractory chest pain with or without ventricular dysrhythmias
Short-term bridge to heart transplantation
Unstable angina unresponsive to drug therapy
High-risk cardiac procedures
Cardiac surgery
Contraindications
Irreversible brain damage
Ex. Pt who is brain dead
Moderate to severe aortic insufficiency
Abdominal aortic and thoracic aneurysms
Could lead to an aortic dissection
may become uncoordinated
Aortic dissection
Generalized PVD
Major coagulopathy
Thrombocytopenias
Bleeding risk
End-stage cardiomyopathies
Severe atherosclerosis
Terminal illnesses
Principles of IABC
Flexible catheter inserted into the femoral artery and passed into the descending aorta.
Correct positioning is critical to avoid blocking the subclavian, carotid, or renal arteries.
When inflated, the balloon blocks 85-90% of the aorta.
Complete occlusion can damage the walls of the aorta, red blood cells, and platelets.
When deflated, it creates a vacuum that decreases aortic pressures.
Effects of Inflation
Increases diastolic pressure, enhancing perfusion to distal organs and tissues.
Increases systemic perfusion, improving MAP numbers.
Increases pressure in the aortic root during diastole.
Increases coronary artery perfusion pressure, improving O2 delivery to the myocardium.
Reduces angina and ECG evidence of ischemia; reduces ventricular ectopy.
Effects of Deflation
Decreases afterload due to decreased aortic end-diastolic pressure.
Decreases peak systolic pressure.
Decreases O2 demands due to decreased myocardial workload and O2 consumption.
Increases stroke volume.
Improves cardiac output and reduces left ventricular preload (PAWP=wedge).
Result: Increased urinary output and decreased heart rate
Complications of IABC and Nursing Management
Infection/sepsis
Balloon leak or rupture
Tell physician ASAP
Effects of immobilization
Thrombocytopenia (can destroy platelets)
Increased bleeding risk
Thromboembolism
Blood pools around balloon and causes a clot
Hemorrhage from insertion site
Trauma to the aorta & femoral artery
Frequent extremity neurovascular checks q2h & hourly urinary outputs are essential for early identification of problems!
Nursing Management (Cont’d)
Cardiovascular Assessments
Hemodynamic Monitoring
Heart/Lung Auscultation
ECG evaluation
Look for any changes
Oftentimes get a 12 lead as baseline
Tissue Perfusion
Urinary output a good indicator (especially if it drops below 30/hr)
Neuro Status q2h
As patient improves, 1:1 ratio can decrease with Re-evaluation
Ventricular Assist Devices (VAD)
Support for the failing heart (advanced stages)
Placed into the path of flowing blood to alter the action of one or both ventricles.
May be placed internally or externally.
External is easier and often temporary
Blood is shunted from the left atrium to the device and then to the aorta.
Better mobility than IABP.
Indications
Failure to wean from cardiopulmonary bypass after surgery.
Post-surgical cardiogenic shock.
Recovery after heart transplant.
HF NY Class IV resistant to drug therapy
Contraindications
BSA less than manufacturer’s limits
Irreversible end-stage organ damage
Co-morbidities that make life expectancy less than 3 years
Nursing Management
Nursing care is similar to that of the patient with an IABP.
Observe the patient for bleeding, cardiac tamponade, ventricular failure, infection, dysrhythmias, renal failure, hemolysis, and VTE.
The patient must be mobile and needs an activity plan.
Patients may go home with one. Preparation for discharge is complex and needs in-depth teaching about the device and support equipment, such as battery chargers.
May have dressing around site and needs to be changed every 24-48 hours
Educate when to change battery pack.