Mechanical Ventilation
Mechanical Ventilation Overview
Definition: Mechanical ventilation is a process involving the delivery of fraction inspired oxygen (FIO2) at ≥21% into lungs via a mechanical ventilator, capable of achieving up to 100% oxygen concentration.
Purpose: Supports patients with impaired breathing until they can breathe independently, optimizing gas exchange by maintaining alveolar ventilation and oxygen delivery.
Indications for Use: Patients with respiratory failure or compromised airway (e.g., decreased PaO2, increased PaCO2, persistent acidosis). Situations prompting mechanical ventilation include as a result of respiratory failure caused by the following:
Thoracic/abdominal surgery
Drug overdose
Neuromuscular disorders
Inhalation injury
COPD
Multiple trauma
Shock
Coma
Multisystem failure
Ventilator Classifications
Negative-Pressure Ventilators: Older forms like iron lungs, rarely used today; work by creating intermittent sub-atmospheric pressure around the chest.
Positive-Pressure Ventilators: Most common in acute care, pushing air into lungs during inhalation, leading to raised intrathoracic pressure.
Types of Positive-Pressure Ventilators:
Volume-Cycled: Delivers a preset tidal volume (VT) per breath (normally 6-10 mL/kg).
Pressure-Cycled: Delivers air until a set pressure is achieved, but the volume may vary.
High-Frequency Oscillatory Ventilation (HFOV): Very high respiratory rates (180-900 breaths/min) with low tidal volumes, used for serious lung conditions (e.g., ARDS, atelectasis).
This mode is used to open the alveoli for atelectasis and ARDS. Protects the lung from pressure injury.
Ability to support gas exhange at a fixed mean airway pressure while limiting the risk of ventilator induced lung injury.
Noninvasive Positive-Pressure Ventilation (NIPPV): Uses face or nasal masks, avoiding intubation; useful for various respiratory failures (e.g., COPD, pulmonary edema).
Decreases risk of nosocomial infections such as pneumonia.
Eliminates intubation.
Most comfortable mode with pressure support.
Eases WOB and enhances gas exchange.
Containdicated for pts with resp. arrest, serious arrhythmias, cognitive impairment, or head/facial trauma.
Continuous Positive Airway Pressure (CPAP) provides positive pressure to the airways throughout the respiratory cycle.
Used with a leak-proof mask to keep alveoli open, preventing resp. failure.
Effect tx for obstructive sleep apnea bc the positive pressure acts as a splint, keeping upper airway and trachea open during sleep.
To use CPAP, the pt must be breathing independently.
Bilevel Positive Airway Pressure (BiPAP) ventilation offers independent control of inspiratory and expiratory pressures while providing pressure support ventilation (PSV).
Delivers 2 levels of positive airway pressure provided via a nasal or oral mask, nasal pillow, or mouthpiece with a tight seal and a portable ventilator.
Inspiration can be initiated by either by the patient or the machine if it is programmed with a back up rate.
BiPAP is used often for pts who require ventilatory assistance at night: COPD or sleep apnea.
Ventilator Modes
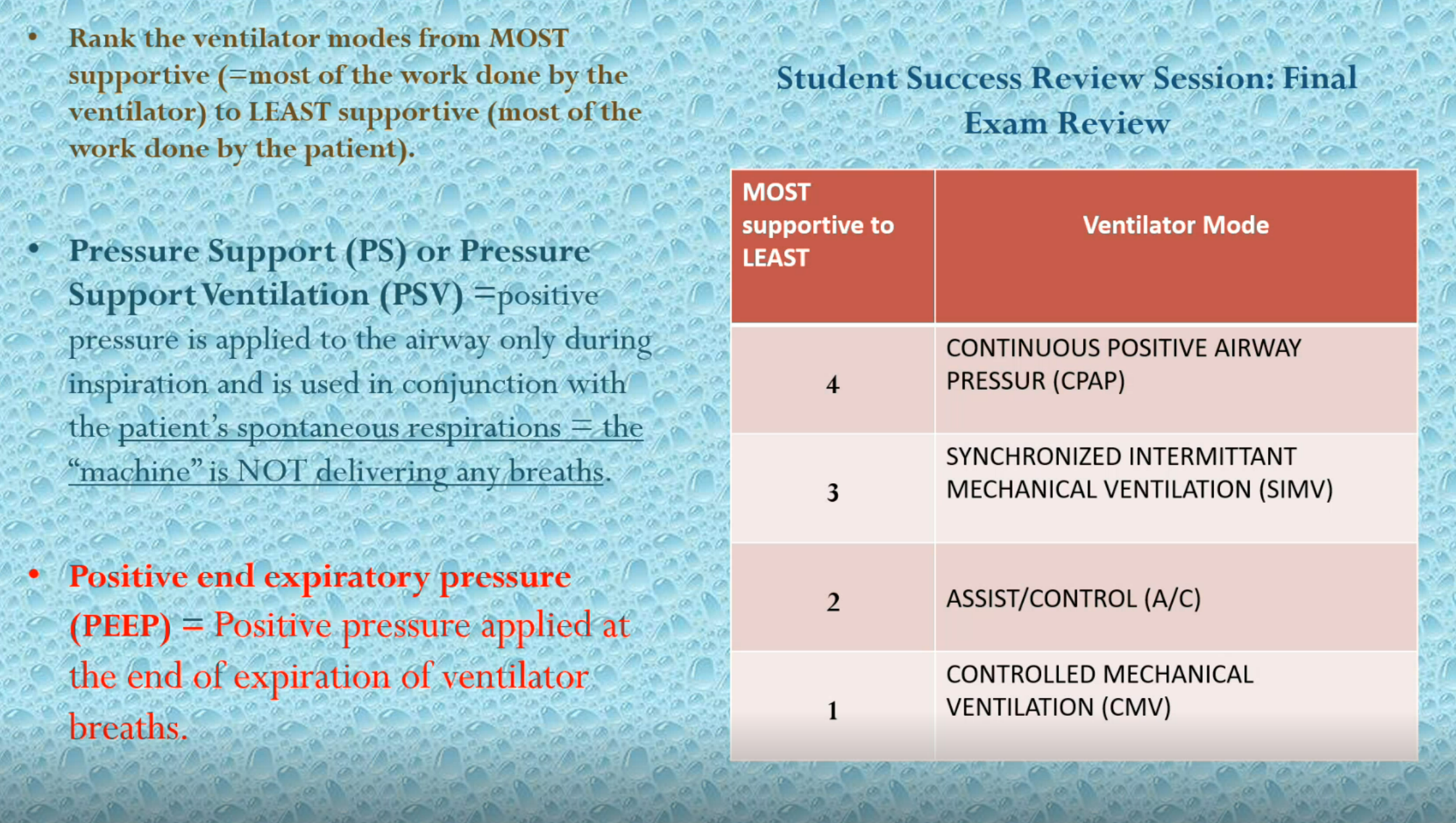
1# Controlled Mechanical Ventilation (CMV): Provides full support at a set tidal volume and rate.
2# Assist-Control (A/C): Delivers preset breaths; supports patient-initiated breaths regardless of timing. Assist control mode a set tidal volume and set rate are delivered. If the patient attempts to breath → the ventilator will sense it and then automatically deliver the present TV. EVERY breath - whether delivered by the ventilator or if initiated by the patient - will be at a TV of a predetermined value, ensuring consistent ventilation regardless of the patient's effort.
Delivers like 90% of the WOB
3# Intermittent Mandatory Ventilation (IMV): Mix of assisted and spontaneous breaths, allowing patient effort but limiting tidal volume on unassisted breaths.
4# Synchronized Intermittent Mandatory Ventilation (SIMV): Similar to IMV, but synchronizes with patient respiration, reducing dyssynchrony.
Allows the patient to breathe spontaneously at their own rate and depth - patient does more of the WOB.
Ventilator delivers each breath in synchrony with patient’s own breathing
Can be used to help wean the patient from the ventilator
GOAL → “normalize” the ABGs → get the patient off the ventilator.
**When you’re trying to wean the patient off using SIMV, you must discontinue or reduce sedation so they can do the work of breathing.
**Clinical Note: If the patient’s resp and HR increased, became restless and O2 sat decreased → STOP THE WEANING PROCESS and go back to the previous setting.
5# Pressure Support Ventilation (PSV): Applies pressure during spontaneous breaths to help overcome resistance.
6# CPAP: Delivers continuous positive airway pressure throughout the breathing cycle, assisting in maintaining alveolar recruitment and improving oxygenation. Patient does most of the WOB.
Ventilator rate: Trick question… IT’S NONE!!!!!!!!!!! Patient must do all of the support. But this mode gives pressure support.
Weaning from Mechanical Ventilation
Process involves gradual removal of ventilator support based on patient readiness and safety. Criteria include stable vital signs, adequate spontaneous breathing, and ability to maintain oxygenation.
Monitoring During Weaning: Vital signs, oxygen saturation, heart rate, and respiratory pattern should be closely monitored, with adjustments made as needed based on patient performance.
Common Complications and Risks
Ventilator Malfunction: Emergency protocols for manual ventilation must be in place.
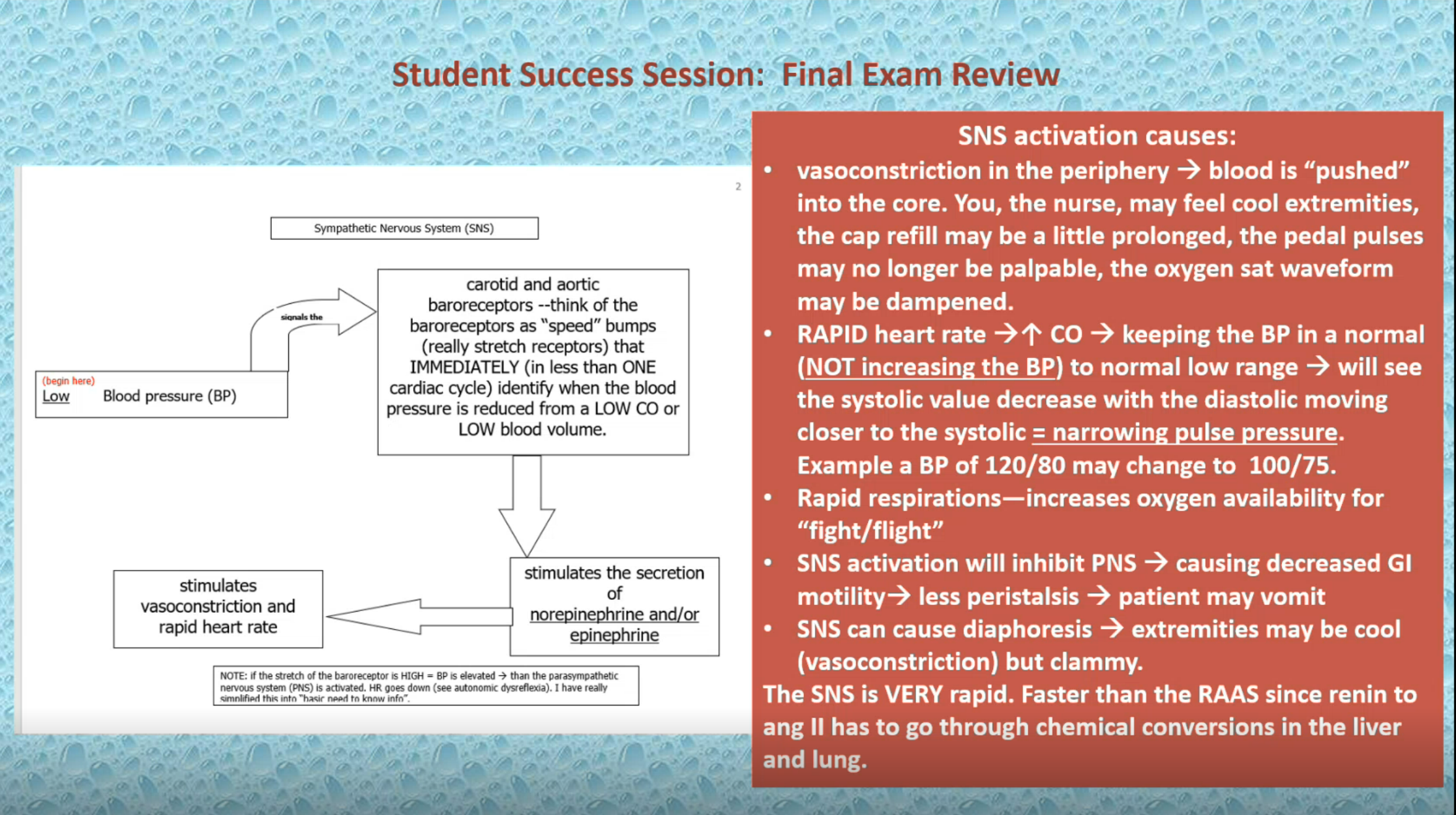
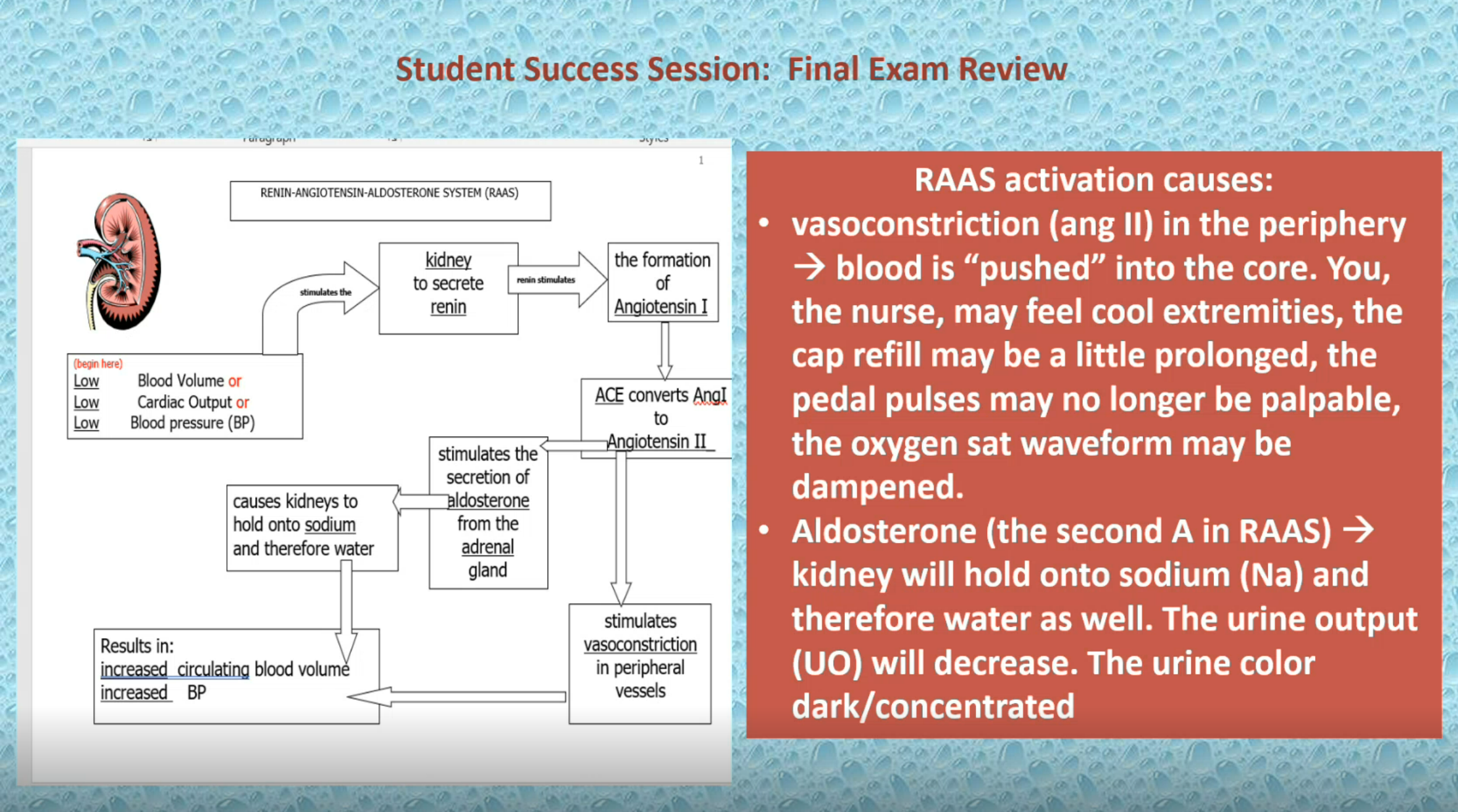
Cardiovascular Issues: Increased intrathoracic pressure can lead to decreased venous return, affecting cardiac output and tissue perfusion.
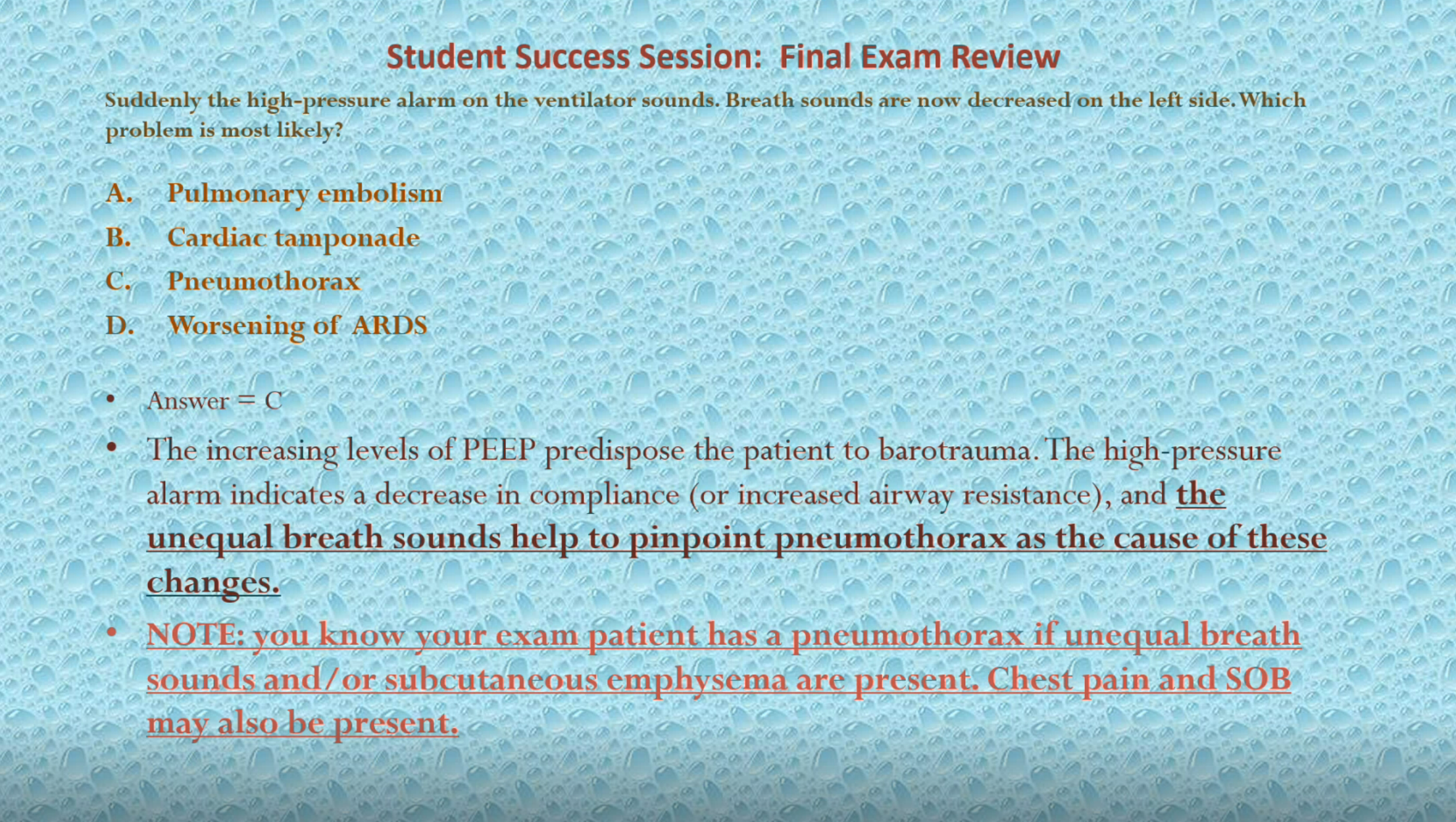
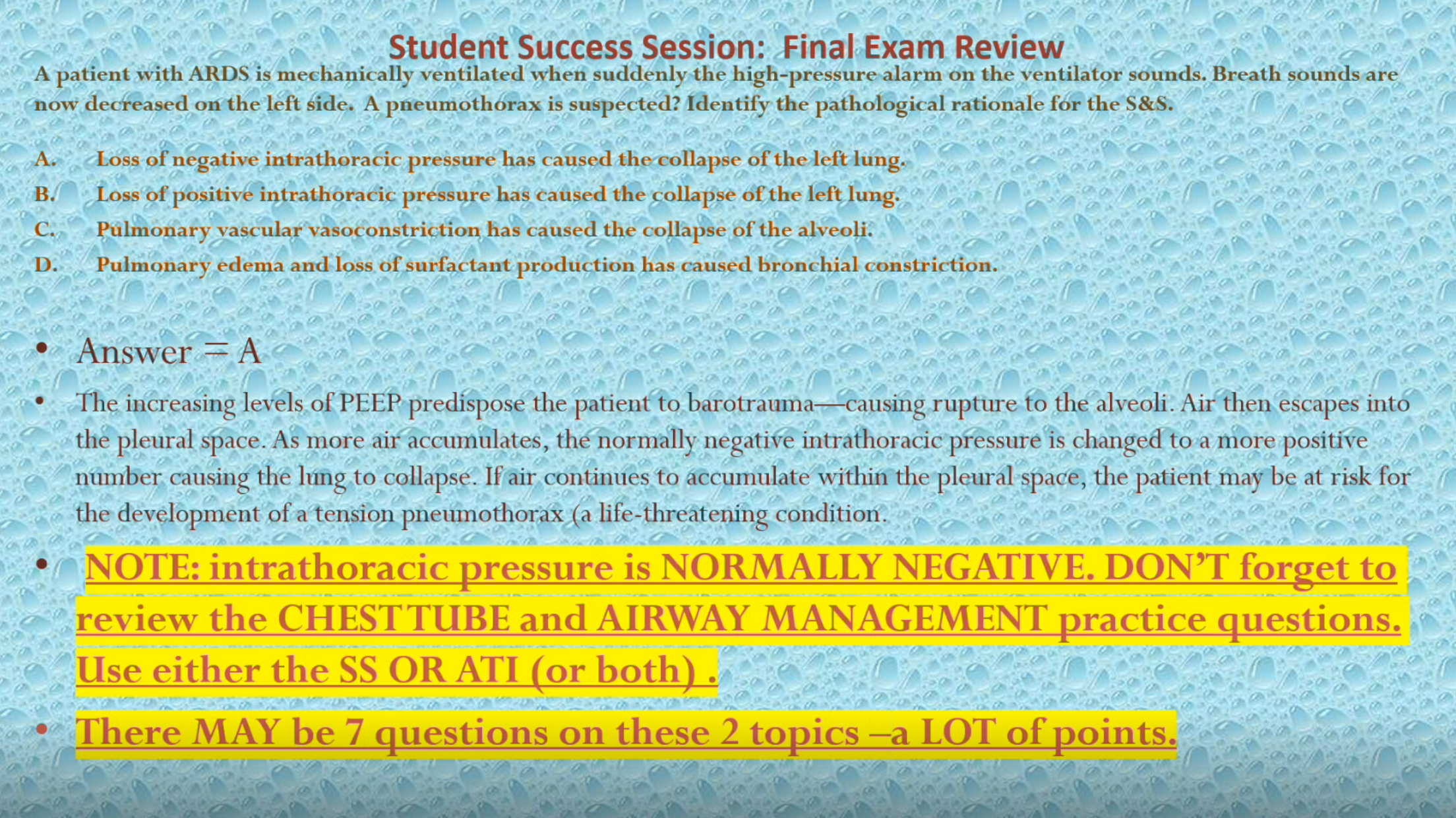
Barotrauma/Pneumothorax: Excessive positive pressures can damage lung tissue, potentially leading to pneumothorax.
Infection Risks: Patients on mechanical ventilation are at high risk for pneumonia (HAP/VAP); prevention measures include maintaining head position, oral hygiene, and minimizing infection risk factors.
Sedation and Neuromuscular Blocking Agents (NMB)
Sedation: Used judiciously to relieve anxiety/pain without suppressing respiratory drive; Propofol is a common choice.
ALL PATIENTS MUST RECEIVE CONCURRENT SEDATION AND ANALGESIA IF USING A PARALYTIC DRUG.
Monitoring Train-of-four (TOF): Assessing neuromuscular blockade via peripheral nerve stimulation to avoid complications from excessive NMB.
Uses a peripheral nerve stimulator to deliver four successive stimulating currents to elicit muscle twitches.
A baseline is established by increasing hte impulse level up tuntil the unsedated/unparalyzed patient has 4/4 muscle twitches.
Goal:
1-2 twitches out of 4
0 twitches means that the pt has too much pf the drug!
Neuromuscular blockade (paralysis):
Provides synchrony with ventilator; helps manage high airway pressures
Improves oxygenation
Sedation & Analgesia:
Paralyzed patient can hear, see, think, and feel → but NOT move a muscle = no blinking, winking or nodding
IV sedation and analgesia must be administered concurrently.
Nursing Interventions
Monitor patient respiratory status closely and maintain communication about ventilation settings.
Regular assessments, including arterial blood gases (ABG), pulmonary function, and patient comfort, are crucial for effective management.
Ventilator Modes
Controlled Mechanical Ventilation
Provides full ventilatory support at a set tidal volume (VT) and rate.
Used when the patient cannot initiate breaths on their own.
Assist-Control (A/C)
Delivers preset breaths; supports patient-initiated breaths regardless of timing.
Ensures that the patient receives the minimum number of breaths per minute.
Intermittent Mandatory Ventilation (IMV)
A combination of assisted and spontaneous breaths.
Allows for patient effort, but limits tidal volume on unassisted breaths.
Lowers mean airway pressure, which can assist in preventing barotrauma.
However, dyssynchrony like “fighting the ventilator” or “bucking the ventilator” may increase.
Synchronized Intermittent Mandatory Ventilation (SIMV)
Similar to IMV, but synchronizes mandatory breaths with the patient's own respiratory efforts. Delivers a preset tidal volume and # of breaths/min. Between ventilator-delivered breaths, the pt can breathe spontaneously w/ no assistance from the ventilator on those extra breaths. MAchine can sense pt breathing efforts and doest not initiate a breath in opposition to the patient’s efforts.
Reduces dyssynchrony and enhances patient comfort and effort during ventilation.
Pressure Support Ventilation (PSV)
Provides pressure during spontaneous breaths to help overcome the resistance of the ventilator circuit and improve tidal volume.
Useful for weaning patients off mechanical ventilation as it allows for more spontaneous breathing.
Pressure support is reduced as the patient’s strength increases.
More WOB is involved from being intubated and spontaneously breahting through the ETT (straw) and the long ventilator tubing, but it is necessary to wean the patient OFF the vent.
**PSV helps on inhalation.
As the patient inhales, the vent helps push the air into the lungs. The patient can receive a lot of help (20) or less help (any number less than 20).
Key Ventilator Settings
Tidal Volume (VT)
Volume of air delivered with each breath, typically set between 6-10 mL/kg of ideal body weight depending on the patient’s size and underlying condition.
Respiratory Rate (RR)
Number of breaths delivered per minute; typically set based on the patient's needs, ranges can vary widely but often fall between 12-20 breaths/min.
Fraction Inspired Oxygen (FIO2)
Percentage of oxygen delivered to the patient; can be adjusted from 21% (room air) to 100% based on arterial blood gas (ABG) results.
Positive End-Expiratory Pressure (PEEP)
Pressure maintained in the airways at the end of expiration to prevent alveolar collapse; typically set between 5-15 cm H2O to improve oxygenation and compliance.
Advantages:
Alveolar recruitment (alveolar recruitment = keeping the alveoli open and available for gas exchange)
Improve gas exchange
Decrease WOB
Decrease FIO2
With PEEP, the alveoli remain open instead of collapsing at the end of expiration. Think of a balloon (lungs) filling with air (inspiration), squeeze out the air (exhale) from the balloon and the balloon will collapse or close. With PEEP, the balloon stays open allowing for decreased work on the next inhalation AND there is increased time that O2 can diffuse into the blood (we want that). If oxygenation can go up, we could/should be able to decrease the FIO2 - we don’t really want to deliver that HIGH amount of supplemental O2 for very long BUT we really would like for our patient not to be an anaerobe.
GOAL: Ensure the PaO2 is > 60mm/hg (normal is 80-100mm/hg) and the SpO2 is > 90%.
Disadvantages
Decrease venous return
Decreased cardiac output
Barotrauma = inflate the alveoli (balloon) with too much air/pressure and pop goes the balloon.
Barotrauma → The patient (at the least) will develop a pneumothorax. Since the chest wall is closed all the air that enters from the trachea → into that “popped” alveoli goes out into the chest/thoracic cavity. As more breaths are taken and more air gathers in the thoracic cavity with no place to escape, the air will take up all the space that the lung should have. The lung collapses and as the (let’s say right) thorax fills with air; the heart is pushed to the left. The heart no longer has space to fill and pump (work) and the left lung space may now become threatened - has now become a tension pneumothorax.
Why decreased venous return? - Think normal respirations - diaphragm drops down, chest muscles pull our chest wall/rips up and out →increasing the diameter in our thoracic cavity → increased diameter causes a DROP in pressure → we essentially create a vacuum and suck air into our lungs (REMEMBER THIS). At the same time as air is being sucked into our lungs, venous blood is being sucked up and INTO the right atrium → yes on inspiration air is sucked into our lungs AND blood is sucked UP and into our heart. PEEP = POSITIVE pressure. We have reduced the negative pressure that created our vacuum/sucking power. Less blood is sucked into our RA (less venous return) → less going to the Left side → decreased CO.
Peak Inspiratory Pressure (PIP)
The maximum pressure delivered during inhalation; important for preventing barotrauma.
Inspiratory Time (Ti)
Duration of time for each breath; adjusted based on the needs of the patient and the mode of ventilation being used.
Flow Rate
Speed at which the tidal volume is delivered, can be set to improve patient comfort and synchronization with breathing pattern.
WOB
Referes to inspiratory effort needed to overcome the elasticity and viscosity of the lungs along with the airway resistance. The mode is determined by the patient’s ventilatory status, respiratory drive, and ABGs.
Alarms
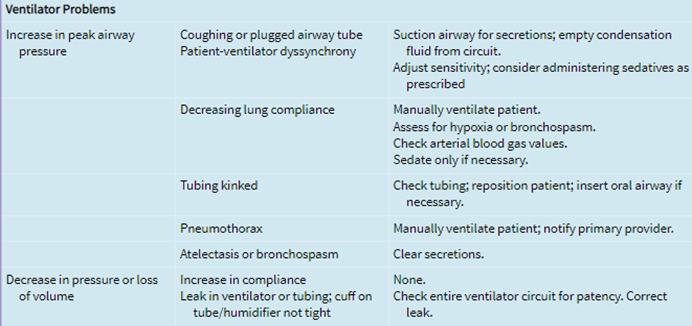
High-pressure limits: Regulates the maximal pressure the ventilator can generate to deliver the VT. When the pressure limit is reached, the ventilator terminates the breath and spills the undelivered volume into the atmosphere. Causes are:
Coughing or plugged airway tube secretions, coughing, or gagging which may require suctioning the airway for secretions or emptying condensation fluid from circuit.
Patient-ventilator dyssynchrony which may need adjusting.
Decrease lung compliance which may require manually ventilating the pt, assessing for hypoxia or bronchospasm, getting ABGs, fixing the issues, and sedation if needed.
Kinked or compressed tubing.
Think of a balloon - how much force/effort does it take to blow up a balloon. Same thing for a patient - the resp therapist (RT) will assess how much pressure or force it will take for the ventilator to blow air into the person’s lungs. If the lungs are stretchy (compliant) the ventilator will use a little bit of effort, if the lungs are stiff (noncompliant) the ventilator will use a LOT of force. When a patient is first placed on a ventilator, the lung compliance is assessed by the RT and then an alarm limit is set on the ventilator. In other words - this patient’s lungs are getting stiffer - the ventilator alarm is sounding because the set amount of pressure is exceeded while the volume of gas is being delivered making the ventilator use more force as air is blown into the lungs of this patient → lungs are less compliant (less stretchy/elastic) AND are offering MORE resistance.
Causes of high pressure → secretions, development of ARDS (see above), biting the tube, kinks in the tube, and coughing. RESISTANCE TO AIRFLOW; lungs are not stretching.
Low-pressure limit: Regulates the minimal pressure the ventilator can generate to deliver the breath. This alarm will occur when:
Total or partial ventilator disconnect - look for the missing link and reconnect.
Loss of airway - check by assessing breath sounds, may need to remove tube and manually ventilate.
ET tube/trach cuff leak - if you hear the cleint speaking, grunting; notify respiratory therapist to increase pressure.
Low resistance to the flow of air entering the lungs. Lungs are balloons → there should be SOME resistance to the flow of air. If not consider →
LEAK anywhere in the system → ET tube cuff/balloon, the tubing is disconnected somewhere in the system, the ventilator tubing is disconnected at the ETT.
What nursing assessment would you expect to find for Respiratory Failure with Mechanical Ventilation?
Diminished breath sounds (on the side of the pneumo)
SubQ emphyema (on the side of the pneumo) → crepitus
You know your (exam) patient has a pneumo when unequal breath sounds or SubQ air/emphysema are present.
Tracheal deviation with a tension pneumo
As the heart is pushed to one side → decreased CO → decreased BP
ARDS or Acute Respiratory Distress Syndrome:
Is caused by diffuse injury to the alveolar-capillary membrane. As a result of capillary damage, capillary permeability increases and fluid crosses into the alveolar space. When the alveolar space is filled with fluid, blood cannot be oxygenated. In addition, the alveolar cells that produce surfactant are damaged. As a result the lungs become less compliant or less elastic.
Common risk factors for ARDS include:
Sepsis
Aspiration of gastric contents
Pneumonia
Multiple transfusions
Trauma
Shock States
Cardiopulmonary bypass
Near drowning.
ARDS carries a 50% mortality rate. If the patient has any of these risk factors, health care providers must be attuned to the early clinical manifestations of ARDS
VAP Best Practices:
Hand hygiene and universal precautions
HOB elevated 30-45 degrees
Teeth and tongue brushing with chlorhexidine product twice daily
Moisture to lips and oral mucosa Q 2-4 hrs.
Oral suction as needed and before every position change
Subglottic suctioning
Ensure that the respiratory therapist maintains the endotracheal balloon pressure at 20mm/Hg (± 5mmHg) and avoids routine ventilator circuit tubing changes.