Shock Sepsis MODS DIC / Hemodynamic notes
Shock Overview
Definition: Life-threatening condition with inadequate tissue perfusion to deliver oxygen and nutrients. All types of shock result in inadequate or decreased tissue perfusion. In other words, not enough oxygen is delivered to the cells.
Consequences: Cell dysfunction and death; can lead to Multiple Organ Dysfunction Syndrome (MODS) and death.
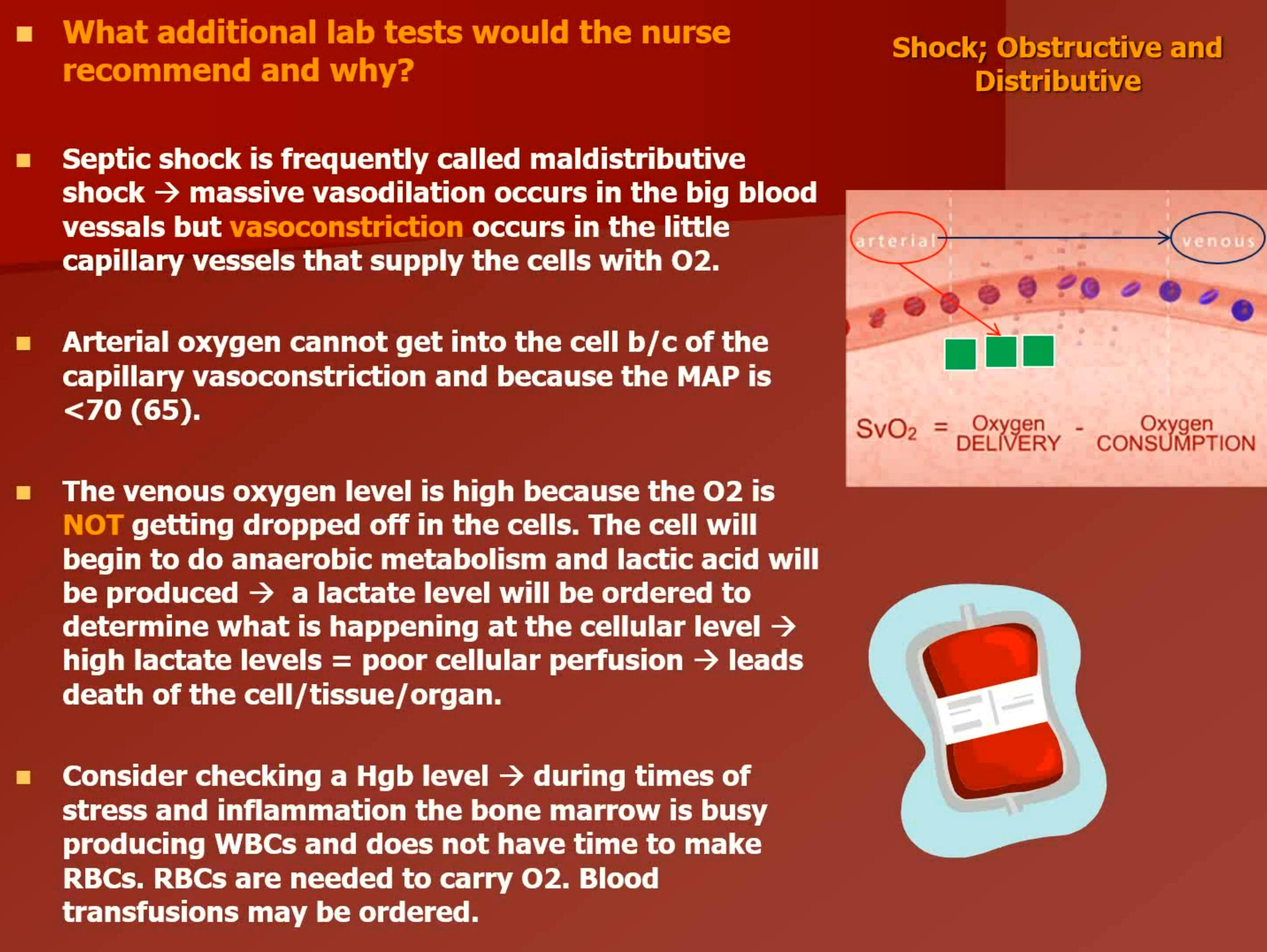
Perfusion = tissue oxygenation → w/o tissue oxygenation cell moves to anaerobic metabolism → LACTIC ACID IS PRODUCED → blood pH moves to acidosis → decreased cell function → death of cell/tissue.
Pathophysiology: Hypoperfusion of tissues, hypermetabolism, and activation of the inflammatory response.
Types of Shock:
Hypovolemic Shock
Cardiogenic Shock
Obstructive Shock
Distributive Shock (includes septic shock)
An appropriate force is necessary to ensure that blood flows to the heart and other organs while achieving oxygen delivery to the cells. To ensure this driving force, the mean arterial pressure (MAP) must be maintained. MAP represents the average pressure throughout the entire cardiac cycle. While caring for a patient in the ciritcal care unit, notice that the MAP is calculated for you and displayed on the monitor screen. Though sources vary, let’s use a MAP of 65 as the low end of normal. To ensure tissue oxygenation a MAP of 65mm/hg must be maintained.
Calculate the MAP → (systolic + diastolic + diastolic) / divided by 3
Multiple Organ Dysfunction Syndrome (MODS)
Definition: Presence of altered functions of two or more organs requiring interventions for support.
Causes: Can arise from any type of shock, most commonly sepsis.
Assessment: Rapid recognition and response to shock and sepsis vital for recovery.
Shock Classification and Physiological Responses
Classification: Based on underlying disorders (e.g., hypovolemic, cardiogenic, obstructive).
Common Responses to Shock:
Cellular changes (anaerobic metabolism due to oxygen deprivation)
Vascular responses (vasodilation or vasoconstriction)
Blood pressure changes (decreased MAP affects perfusion)
Pathophysiology of Shock
Cellular Impact:
Energy through anaerobic metabolism leads to low energy yields and acidosis.
Cellular swelling, impaired membranes, and eventual cell death.
Metabolic Changes:
Stress hormones (catecholamines, cortisol) released leading to hyperglycemia.
Gluconeogenesis mobilizes glucose; depletion of glycogen stores can lead to organ failure.
Regulation of Blood Pressure and Perfusion
Regulatory Mechanisms:
Autoregulation: Vasodilation/vasoconstriction based on tissue oxygen demands.
Baroreceptors and chemoreceptors: Monitor blood pressure and blood gas concentrations.
Hormonal control: Renin-angiotensin system and aldosterone impact volume and pressure.
Mean Arterial Pressure (MAP): Must exceed 65 mm Hg for effective tissue perfusion.
Stages of Shock
Compensatory Stage (Stage 1):
Normal blood pressure; sympathetic activation maintains cardiac output.
Signs: Cool, pale skin; reduced urine output; increased respiratory rate; metabolic acidosis present.
Interventions focus on identifying and treating underlying cause quickly.
Progressive Stage (Stage 2):
MAP falls; hypotension present.
Multiple system failure begins; tissue hypoperfusion worsens leading to lactic acidosis.
Significant risk for adverse outcomes.
Irreversible Stage (Stage 3):
Severe organ damage; persistent low BP despite treatment.
Complete organ failure and imminent death.
Vital Signs Monitoring
Key Indicators:
Systolic BP < 100 mm Hg or drop of 40 mm Hg from baseline is critical.
Serial monitoring of pulse pressure; decreased pulse pressure can indicate shock before BP changes.
Central venous oximetry monitoring used to evaluate oxygen saturation and perfusion.
Management Strategies for Shock
General Management:
Fluid resuscitation (crystalloids and colloids); early intervention critical for positive outcomes.
Nutritional support addressing increased caloric needs.
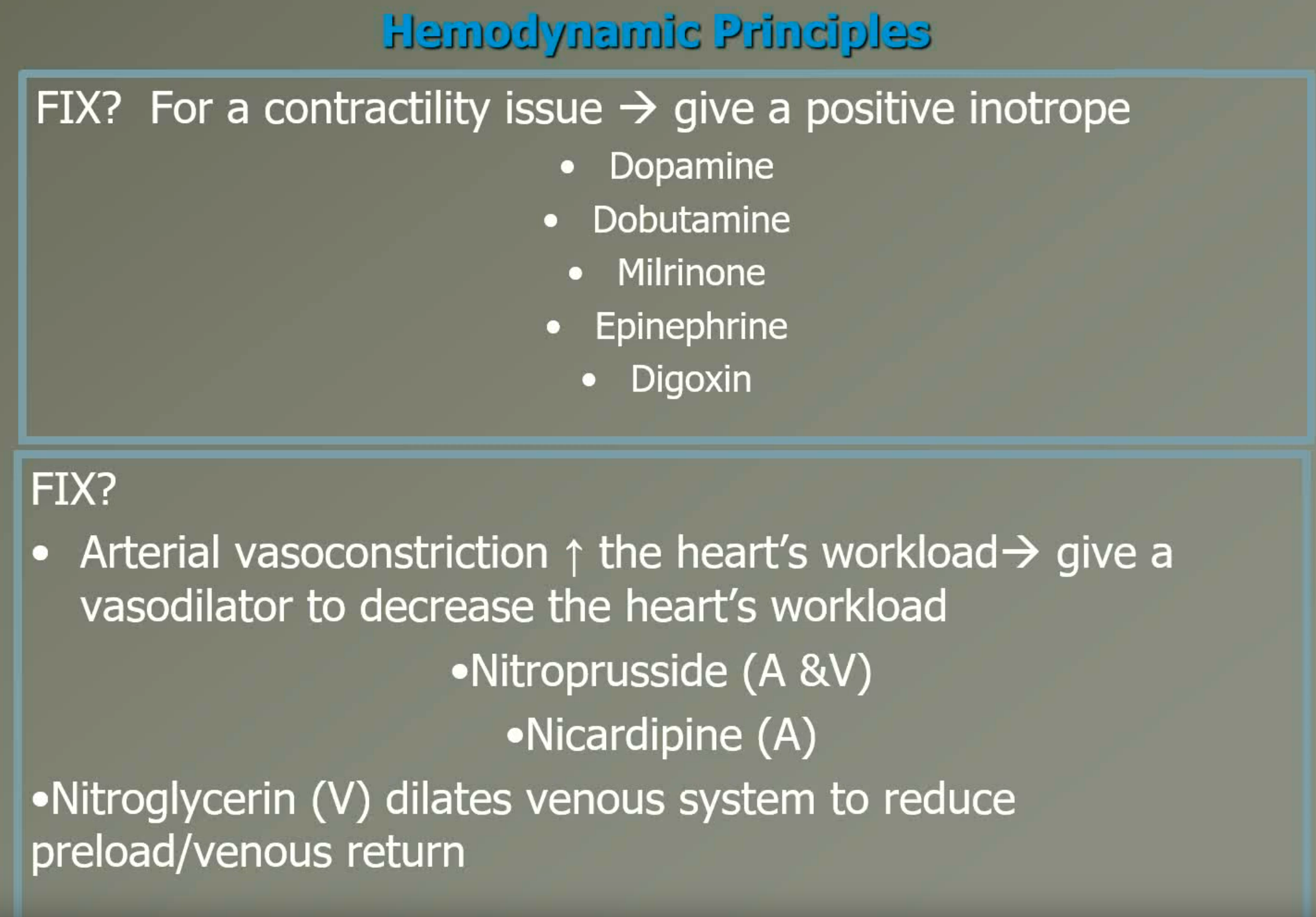
Vasoactive medications to improve hemodynamics when fluid alone is insufficient.
Fluid Resuscitation:
Crystalloids like 0.9% saline and lactated Ringer’s for volume expansion.
Blood transfusions indicated if there is significant blood loss or coagulation issues.
Prevention and Nursing Interventions
Nursing Role:
Close monitoring of vital signs and signs of shock.
Early identification of at-risk patients; education on advanced directives.
Supportive measures for patient comfort and family involvement.
Specific Interventions:
Administer IV fluids and medications; monitor for complications such as fluid overload or infection.
Provide emotional support and clarity in treatment goals to patients and families.
Specific Types of Shock
Hypovolemic Shock: Caused by fluid volume loss; treatment focuses on volume replacement and underlying cause correction.
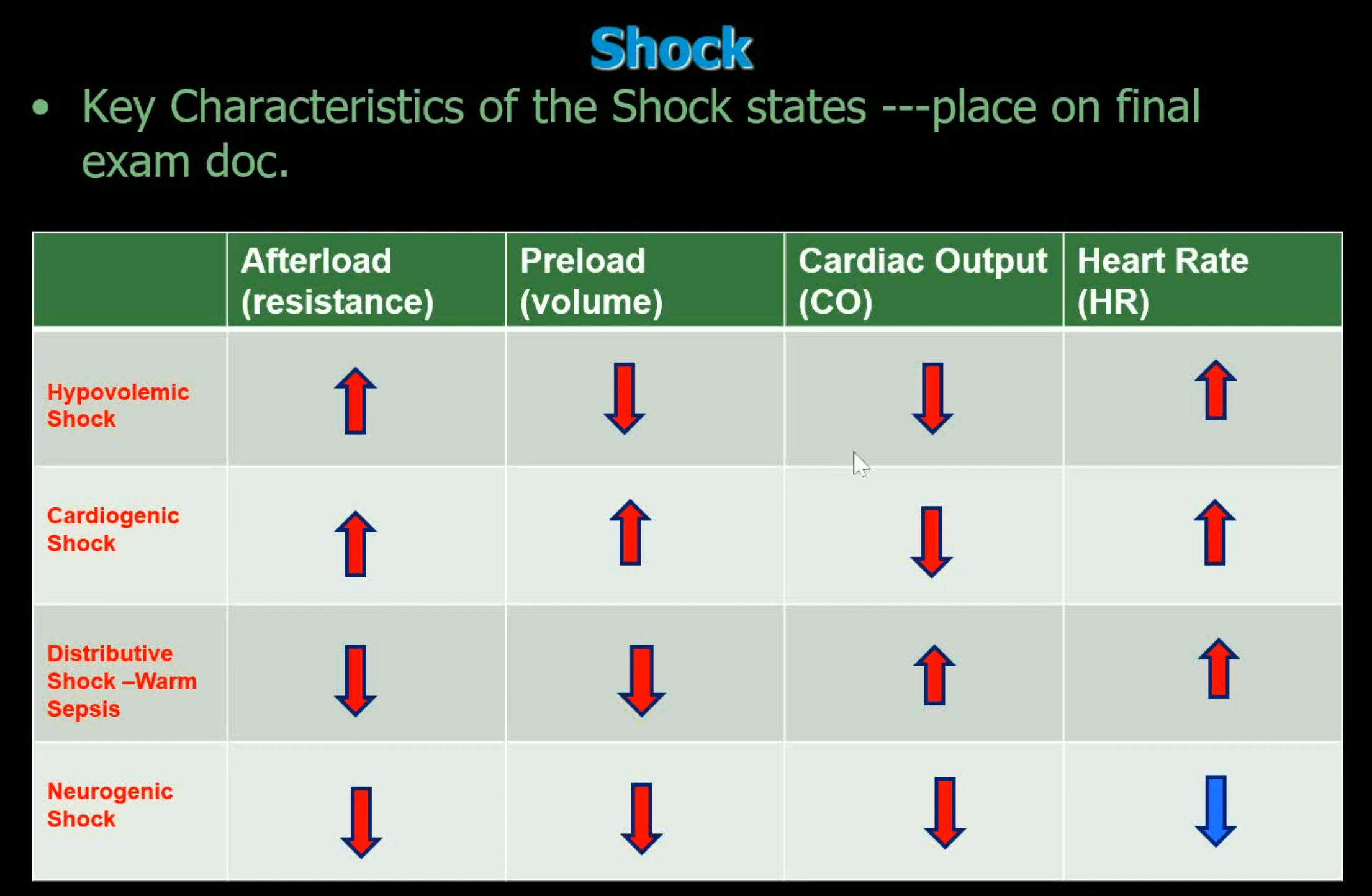
Neurogenic Shock: Massive vasodilation (a hallmark characteristic in ALL distributive shock states) → causes decreased SVR AND decreased HR bc of a loss of SNS → the SNS cannot compensate.
Treatment: ATROPINE IVP. The BP is low b/c the HR is low. Recall that massive vasodilation has occured. As the vascular “tank”/space is vasodilated → what was a 5L/tank now becomes a 7L tank. Bc the HR cannot increase → SNS compensation is GONE → the BP will go down. You texbook deems that cautious administration of fluid may be administered. Therefore a vasopressor is indicated:
Neosynephrine (phenylephrine), levophed (norepinephrine), dopamine, vasopressin.
Cardiogenic Shock: Heart's inability to pump effectively; requires stabilization of cardiac output and possibly surgical interventions.
Distributive Shock: Includes septic shock; characterized by vasodilation leading to hypotension and requires infection control and fluid resuscitation.
Causes: A systemic allergic reaction caused by drugs, pollen, bee stings, blood transfusion reactions, food allergies, etc.
Hallmark characteristics of anaphylactic shock? - Massive systemic vasodilation → decreased SVR, increased HR + S/S noted in the picture to your left. No hemodynamic data usually provided. Your clue is history.
Treatment: Airway management + epinephrine SQ or IV → epi causes vasoconstriction and bronchodilation + steroids to reduce swelling (in bronchials and periphery) caused by the inflamm mediators + antihistamines to counter further allergic hypersensitivity.
Septic Shock: Rapid identification and antibiotics critical; aggressive fluid resuscitation essential to restore perfusion.
Started as generalized inflammation (the inflammation that begin in the skin cells) → has now progressed to a non-focused SYSTEMIC inflammation → inflammation gone crazy and without a specific focus → inflammation without a TRUE focus will begin to damage healthy cells/tissues/organs
What is the big deal about SEPSIS? - Possibility of SEPTIC SHOCK → inflammation gone REALLY REALLY CRAZY that now causes HYPOTENSION
What is the big deal about SEPTIC SHOCK? - Carries a 35% mortality.
INFECTION + SIRS = SEPSIS + LOW BP = SEPTIC SHOCK
In ANY/EVERY patient that has a suspected infection → be on the watch for SIRS → sepsis!!!!!!
S/S of SIRS:
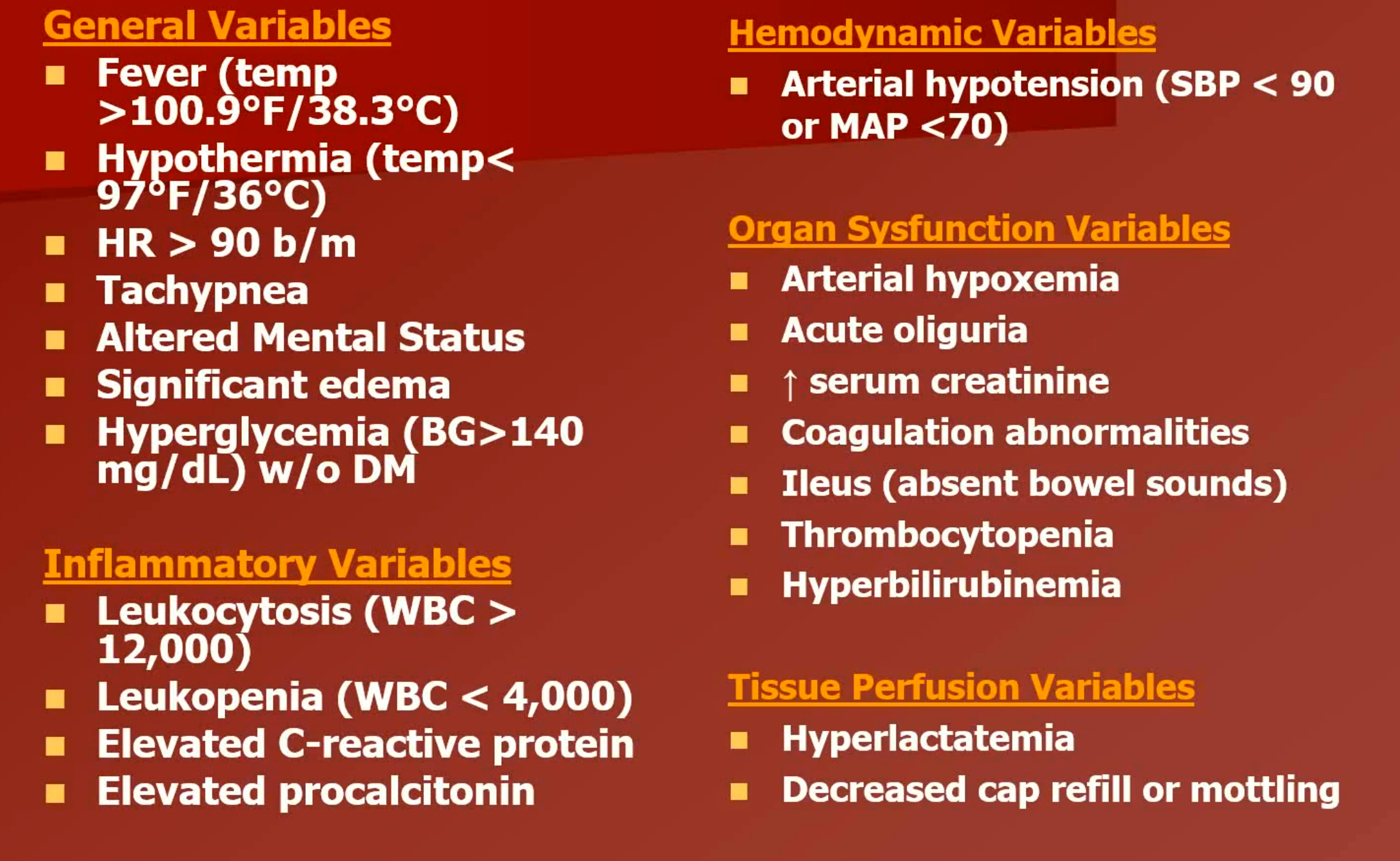
Causes: Any local inflammatory state (be it caused by a microbe, trauma, cancer cell, etc) that then initiates systemic inflammation → that then becomes crazy/wild/uncontrolled systemic inflammation (SIRS) + infection → sepsis.
Treatment: 3 L of IV fluids (systemic inflammatory mediators will cause vasodilation and/or the microbe of the microbe’s toxins will cause vasodilation), culture blood, sputum, urine, wound, etc. Initiate antibiotics within an hour or less of arrival to the health care facility → do NOT delay antibiotics if the person is unable to produce sputum or blood is tooo difficult to draw.
Rationale for the CO and the SVR values (Hallmarks): These values reflect the “warm” stage of septic shock. The inflammatory mediators/microbe toxins increase the force of myocardial contraction. The inflammatory mediators/microbe toxins are also responsible for vasodilation.
In the warm stage of septic shock → increased CO, decreased SVR and the urine output is good.
The septic shock is progressing to the cold stage - as myocardial contractility decreases, the CO decreases. The MAP is decreased - the fluid status is good AEB the CVP and PAWP value. The nurse would need to administer a vasopressor such as Norepinephrine (levophed), phenylephrine (neosynephrine), dopamine or vasopressor → since the “tank” is full it is now time to compress the vascular space to improve the BP. Use the MAP and SVR as a guide to drug titration.
Obstructive Shock:
Sample Question: The nurse should suspect cardiac tamponade → JVD, muffled heart tones AND a narrowed pulse pressure → known as Beck’s triad → indicates cardiac tamponade → a type of obstructive shock
BP was 100/80 → if the S-D = <30/40 mmHg → poor heart function
Causes & Hallmark Characteristics: With obstructive shock a physical obstruction impedes filling or outflow of blood to or from the heart → decreased CO. Characteristics will depend on the type → too varied to list → in all cases a decreased CO will occur → decreased perfusion to tissue → shock. Other major causes include;
tension pneumothorax
massive pulmonary embolus
Treatment: Fix the problem!
Shock; ANY S/S
WE HAVE IDENTIFIED SOME GENERAL CLINICAL MANIFESTATIONS - KNOW THAT CLINICAL MANIFESTATIONS ARE RELATED TO THE “STAGE” OF SHOCK THE PATIENT IS IN. The stages and associated S/S / expected VS are detailed in your shock study sheet:
Neuro: decreased LOC/altered mental status (AMS), dilated pupils (SNS)
CV: increased HR (SNS activation), diaphoretic BUT cool hands and feet, decreased pedal pulses, prolonged cap refill, narrowed pulse pressure (a smaller than normal difference between systolic and diastolic blood pressure readings)→ 110/88 (tricky S/S, so don’t pick BP as the first answer due to compensation)
GI: hypoactive bowel sounds r/t decreased gastric motility, increased gastric residual if on tube feeds.
GU: decreased UO → should be >/= 0.5-1.0 ml/kg/hr
Hemodynamic Principles
Conclusion
Overall Goal: Restore tissue perfusion and oxygenation while minimizing organ dysfunction through timely recognition and intervention.
Collaboration: Interdisciplinary approach required for optimal management and supportive care throughout shock states.