WEEK 8 - Lec 1.2 - Viral transmission and treatment
Introduction to Medical Virology - Lecture 1.2
Page 1: Overview of Virus Transmission and Classification
Introduction to the concepts of virus transmission, classification, and prevention/treatment.
Page 2: Modes of Viral Transmission
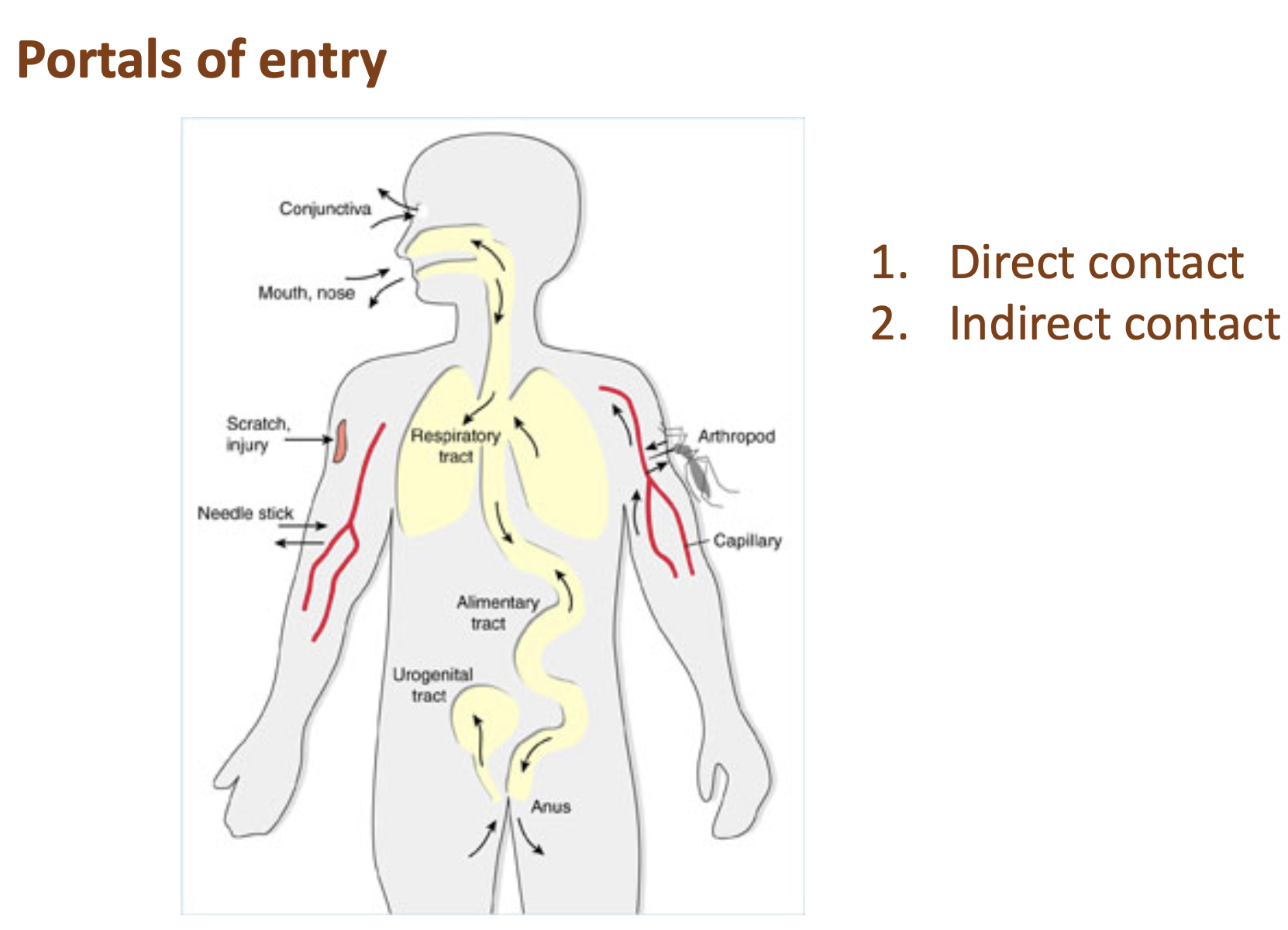
Portals of Entry:
Direct contact
Indirect contact
Page 3: Detailed Modes of Viral Transmission
Direct Transmission:
Person-to-person contact (most common)
Can occur via:
Respiratory tract
Urogenital tract
Skin
Viral particles found in:
Respiratory secretions
Stools
Blood
Indirect Transmission:
Common Vehicle:
Contaminated food or water (e.g., norovirus causing gastroenteritis)
Vector:
Mosquitoes (e.g., Dengue virus, Zika virus)
Fomites:
Inanimate objects (e.g., door handles, injecting equipment)
Page 4: Viral Transmission and Shedding
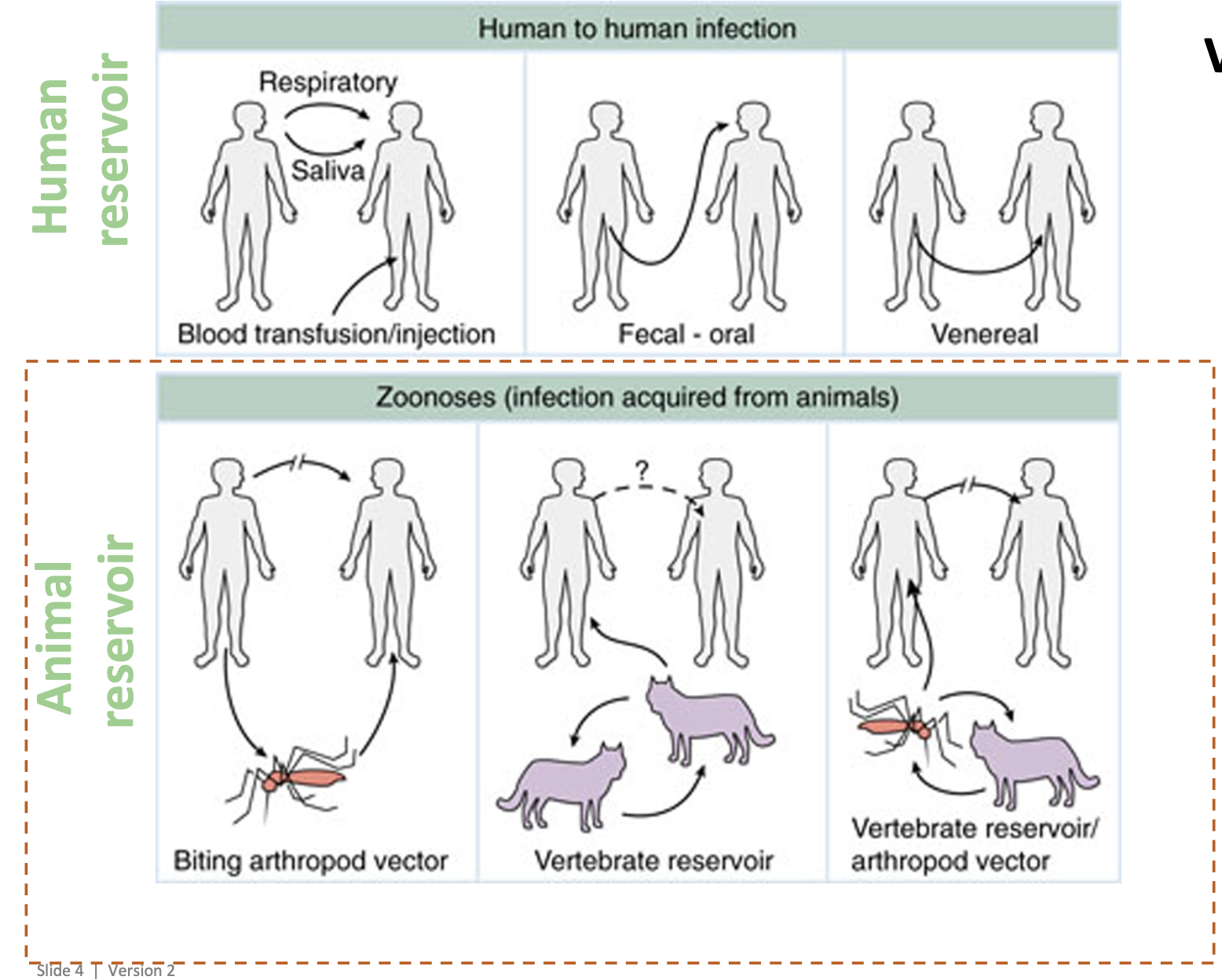
Reservoirs:
Human reservoir
Animal reservoir
Modes of Shedding:
Aerosols
Fecal-oral
Lesions
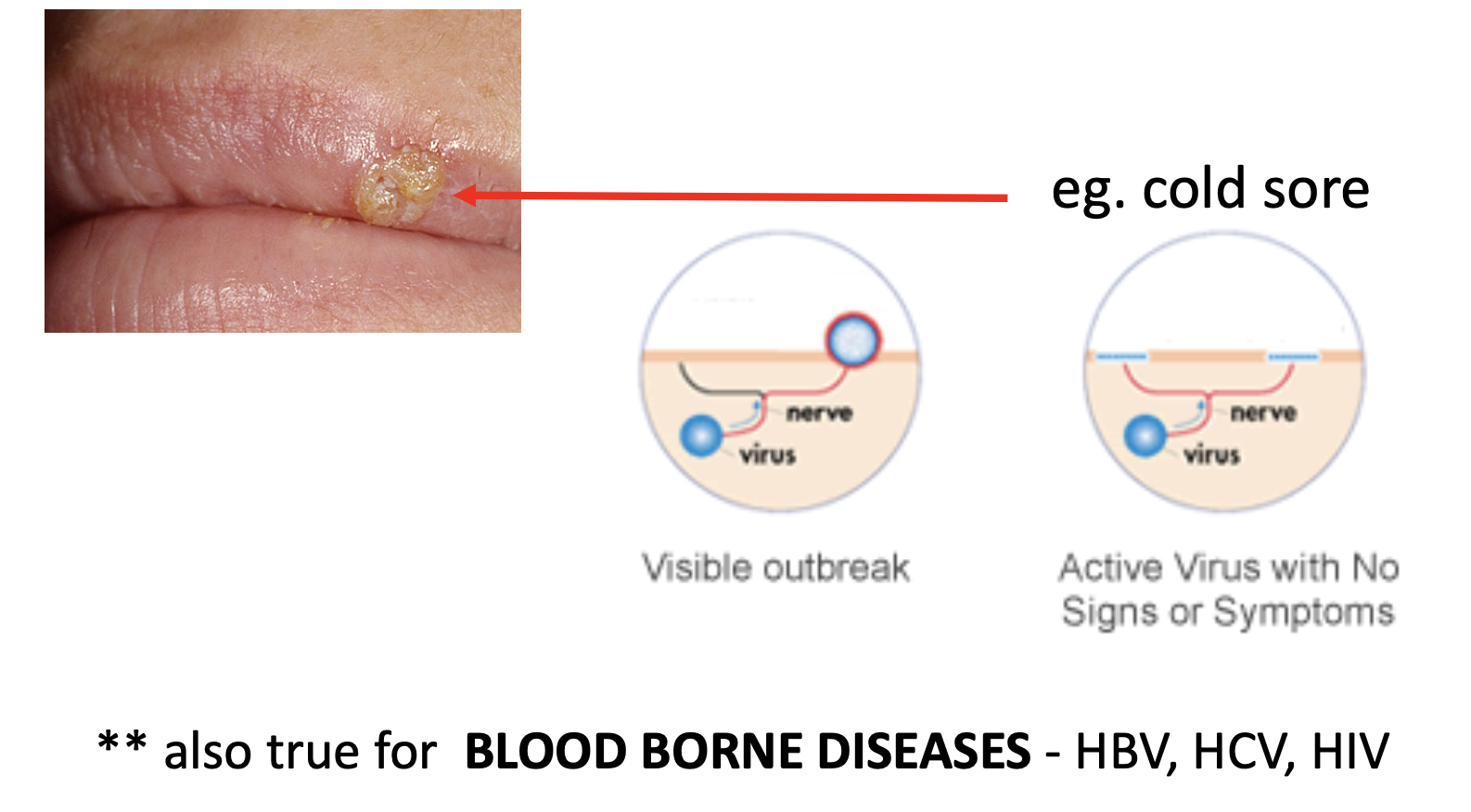
Page 5: Transmission via Lesions- Viral shedding
Example: Herpes virus
Can present as cold sores or genital herpes
Shed in lesions, allowing transmission to uninfected individuals
Blood-Borne Diseases:
Transmission also occurs via lesions for diseases like HBV, HCV, and HIV.
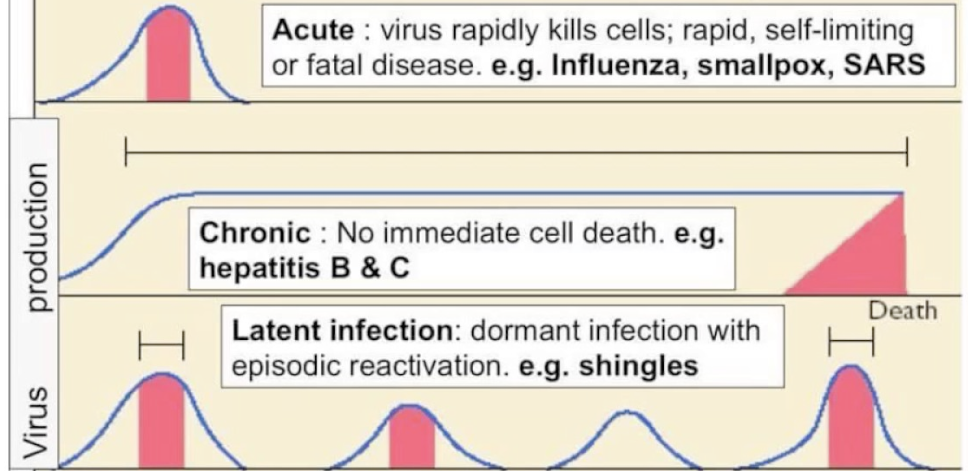
Page 6: Classification of Infectious Viral Diseases
By Duration:
Acute: Develops and runs its course quickly (e.g., Rhinovirus)
Chronic: Develops slowly and persistsfor a long, indefinite
period of time (e.g., HIV, Hepatitis B and C)
Latent: Periods of no symptoms between illness (e.g., Herpes virus)
By Location:
Local: Confined to a specific area (e.g., Hepatitis C in the liver, influenza in the respiratory tract)
Systemic: Generalized illness affecting most of the body- with pathogens distributed widely in tissues (e.g., HIV, Ebola, Rabies)
Herpes virus refers to a family of viruses that cause infections in humans, primarily recognized for causing herpes simplex virus (HSV) infections. There are two common types of herpes simplex virus: HSV-1, which typically causes oral herpes (cold sores), and HSV-2, which generally leads to genital herpes.
Function:
The primary function of the herpes virus is to infect and replicate within host cells. Once introduced into the body, the virus can evade the immune system and establish latency in nerve cells.
Causes:
Herpes virus infections are caused by direct contact with an infected individual or through contact with contaminated surfaces. The virus can be transmitted through kissed, sexual activity, or sharing items like lip balm or utensils with an infected person.
Symptoms:
Symptoms of a herpes infection may include:
Painful blisters or sores in the affected area (oral or genital)
Itching or burning sensations
Pain during urination and sexual intercourse (in genital herpes)
Flu-like symptoms during initial outbreak (fever, swollen lymph nodes)
Cures:
There is no cure for herpes virus infections. However, antiviral medications (such as Acyclovir or Valacyclovir) can help manage symptoms, reduce the frequency of outbreaks, and lower the risk of transmission to others.
Page 7: Prevention and Treatment of Viral Diseases
and Treated?
Good Hygiene Practices:
Avoid contact with contaminated food, water, fecal material, or body fluids.
Wash hands frequently.
Vaccines:
Stimulate natural defenses within the body.
Contain components of weakened or killed virus particles or synthetic portions of viral genomes.
Developed for many common illnesses (e.g., smallpox, polio, mumps, chicken pox).
Not available for all viruses.
Page 8: Antiviral Drugs
Anti-viral drugs (but not antibiotics)
Availability:
Only a few viruses have antiviral drugs available (not antibiotics).
Function:
Inhibit virus development and/or relieve symptoms.
Generally do not cure chronic viral infections (e.g., HIV, HBV).
Treatment Limitations:
Most viruses have no available treatment; focus is on comfort and survival.
Yes, viruses can be contagious. They are transmitted from one person to another primarily through direct contact (person-to-person), respiratory droplets, or contact with contaminated surfaces. Various viruses have different modes of transmission, making some more contagious than others. For instance, the flu virus spreads easily through airborne droplets, while viruses like norovirus can spread via contaminated food and water.
Page 9: Antiviral Agents
Viral Replication:
Depends on host cell metabolic functions and factors.
Effective Antiviral Agents:
Must inhibit virus-specific events without interfering with host metabolism to avoid toxicity.
Typically have a restricted spectrum of activity (e.g., HIV, HCV, HBV, HSV, Influenza virus).- have good viral treatment
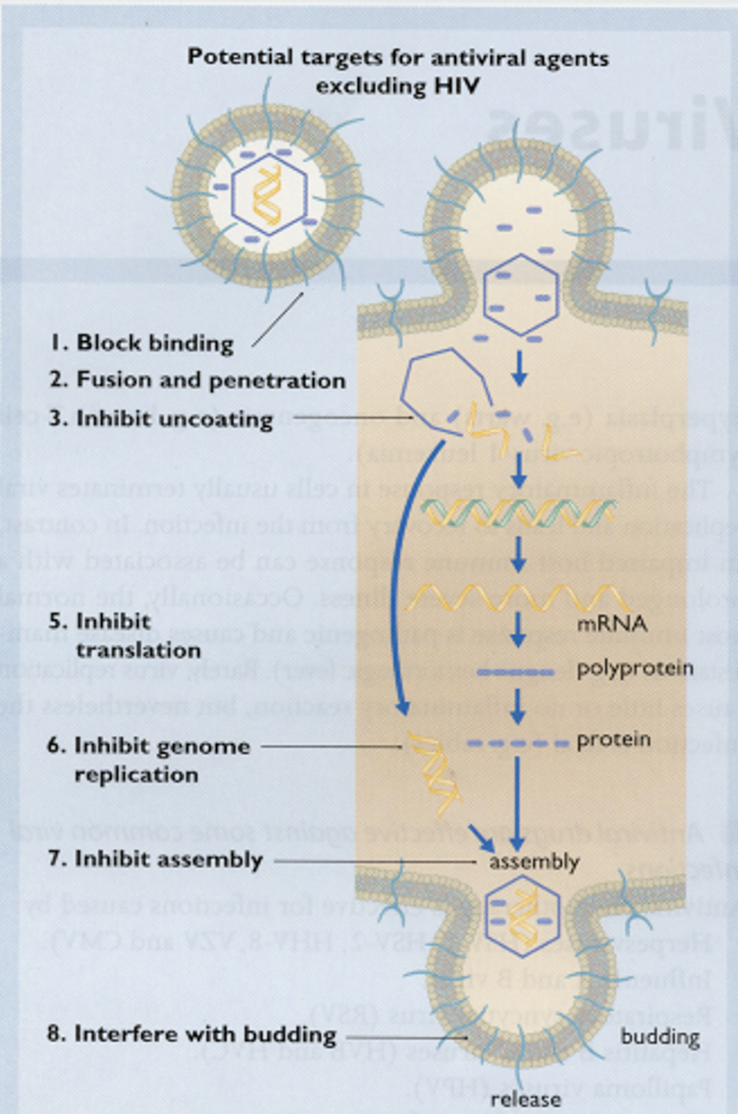
Antiviral drugs work by inhibiting the development and replication of viruses within host cells. They target specific viral processes or structures to prevent the virus from multiplying and spreading. Here are some key mechanisms:
Inhibition of Viral Replication: Antivirals block the ability of viruses to replicate their genetic material, which is essential for producing new viral particles.
Interference with Viral Entry: Some antivirals prevent viruses from entering host cells by blocking viral attachment to cell receptors or interfering with the viral fusion process.
Preventing Virus Release: Certain antiviral agents inhibit the release of newly formed viruses from infected cells, thereby limiting their spread to other cells.
Disrupting Viral Proteins: Antiviral drugs can target viral enzymes critical for the virus's life cycle, such as proteases and reverse transcriptases, rendering them ineffective.
It's important to note that antiviral medications cannot cure chronic viral infections (like HIV or HBV) but can help manage symptoms and reduce the severity of the disease.
Page 10: Learning Objectives
Understand how viruses are transmitted.
Viruses are transmitted through several primary routes:
Direct Contact: Touching infected individuals or surfaces.
Airborne Transmission: Inhalation of droplets from coughs or sneezes.
Vector-Borne: Transmission through insects (e.g., mosquitoes).
Fecal-Oral Route: Ingesting contaminated food or water.
Bloodborne: Contact with infected blood or bodily fluids.
Preventive measures include hand hygiene, vaccination, and avoiding close contact with infected individuals.
Classify viral diseases and explore management strategies with examples.
Classification of Viral Diseases
Acute Viral Infections
Examples: Influenza, Common Cold
Management: Symptomatic treatment, antiviral medications (e.g., Oseltamivir for influenza).
Chronic Viral Infections
Examples: HIV, Hepatitis B
Management: Antiretroviral therapy (ART) for HIV, antiviral drugs (e.g., Tenofovir for Hepatitis B).
Oncogenic Viral Infections
Examples: Human Papillomavirus (HPV), Hepatitis C
Management: Vaccination (e.g., HPV vaccine), antiviral therapy.
Zoonotic Viral Infections
Examples: Rabies, Ebola
Management: Vaccination (e.g., rabies vaccine), supportive care.
Management Strategies
Vaccination: Preventive measure for many viral diseases.
Antiviral Medications: Target specific viruses to reduce severity.
Supportive Care: Manage symptoms and complications.
Integrated learning will continue throughout the virology lecture series.
Antibiotics and antivirals are both types of medications, but they target different pathogens:
Antibiotics:
Used to treat bacterial infections.
Effective against bacteria, not viruses.
Examples: Penicillin, Amoxicillin.
Antivirals:
Used to treat viral infections.
Effective against viruses, not bacteria.
Examples: Oseltamivir (Tamiflu), Acyclovir.
In summary, antibiotics combat bacteria, while antivirals target viruses.
Here are some example exam questions related to medical virology:
Multiple Choice: What is the most common mode of direct viral transmission?
A) Contact with contaminated surfaces
B) Inhalation of droplets from coughs or sneezes
C) Consumption of contaminated food
D) Vector-borne transmission Answer: B) Inhalation of droplets from coughs or sneezes
True or False: Herpes simplex virus can present as cold sores and genital herpes, and it is transmissible even when lesions are not present. Answer: True
Short Answer: Describe the differences between acute, chronic, and latent viral infections, providing one example for each. Answer:
Acute: Develops quickly and lasts for a short time (e.g., Influenza).
Chronic: Develops slowly and persists for a long time (e.g., HIV).
Latent: Periods of no symptoms between episodes of illness (e.g., Herpes virus).
Essay: Discuss the role of vaccines in the prevention of viral diseases. Include the mechanisms by which vaccines work and any limitations they may have.
Fill-in-the-Blank: The primary function of the herpes virus is to infect and replicate within ____________ (host cells). Once introduced into the body, the virus can evade the immune system and establish ____________ in nerve cells. Answer: host cells, latency
These questions cover various aspects of virus transmission, classification, and prevention.
There is currently no vaccine or cure for the common cold primarily due to several factors:
Diversity of Viruses: The common cold is most often caused by a variety of different viruses, with the rhinovirus being the most common. There are over 200 different strains that can cause cold symptoms, making it difficult to create a single vaccine that would be effective against all of them.
Mutation Rates: Many of the viruses that cause colds can mutate rapidly, which can render a vaccine ineffective shortly after it is developed.
Lower Severity: The common cold is usually a mild illness, and the need for a vaccine is not seen as urgent. In contrast, the flu can lead to severe complications and has a higher mortality rate, which underscores the importance of vaccine development for flu viruses.
Existing Vaccines: There are vaccines available for flu because the influenza virus also has multiple strains, but scientists can predict which strains will be most prevalent in a given flu season and formulate a vaccine accordingly.
Overall, the combination of variability among cold viruses, their rapid mutation rates, and the generally mild nature of the illness contrast with the flu's more severe impact, leading to a focus on vaccinating against the flu rather than the common cold.