Chapter 31
Coordinating Care for Patients With Vascular Disorders
The distribution of cardiac output to various tissues depends on the interplay of
The pressure differences that drive the flow of blood and
the resistance to blood flow through specific blood vessels
The primary causes of many vascular disorders are arteriosclerosis and atherosclerosis
Arteriosclerosis: thickening or hardening of the arterial wall, most often associated with aging.
cause stiffness and loss of elasticity
include 3 pathological processes
medial calcific sclerosis, occurs when calcium is deposited in the arterial wall.
A second process, arteriolar sclerosis, involves the thickening of the smaller arterioles.
The third process, atherosclerosis, occurs when low-density lipoprotein (LDL) particles build up in the arterial wall.
a patient with arteriosclerosis or hardened arteries may not have atherosclerosis or plaque, but a patient with atherosclerosis does have arteriosclerosis. Patients often have both conditions.
Risk factor
Elevated cholesterol levels
Elevated triglycerides
Elevated low-density lipoprotein cholesterol (LDL-C)
Low high-density lipoprotein cholesterol (HDLC)
Other risk factors include
hypertension, diabetes, smoking, family history, obesity, and a sedentary lifestyle.
Hypertension: acts synergistically with other risk factors in the development of atherosclerosis.
It causes a mechanical injury to the arterial walls that, over time, makes them harder and less elastic.
Diabetes is linked to atherosclerosis partially because of the increased LDLs and hyperglycemia associated with the disease.
Hyperglycemia is thought to damage the intimal layer of the arterial wall.
Tobacco smoke greatly worsens atherosclerosis and accelerates its growth in the coronary arteries, aorta, and arteries in the legs.
does not directly cause atherosclerosis, cigarette smoke and the by-products of tobacco cause vasoconstriction, hypertension, endothelial cell, and platelet dysfunction and increase circulating cholesterol.
Second-hand smoke has also been shown to manifest these harmful effects
Smoking increases the risk of coronary artery disease two to four times above normal levels.
Men have a higher incidence of atherosclerosis earlier in life than women; however, after menopause, the incidence of the disease is relatively equal in men and women.
There is an increased incidence of atherosclerosis among African Americans and Hispanics compared with Caucasians.
This is partially because of an increased prevalence of smoking, diabetes, and hypertension in these races as compared with Caucasian Americans.
Atherosclerosis comes from Greek words “athero,” meaning “gruel” or “paste,” and “sklerosis,” meaning “hardness.
atherosclerosis is a disease in which LDL-C particles build up in the arterial wall.
The lesions of atherosclerosis accumulate in large and medium-sized arteries.
After the vessel becomes inflamed, a fatty streak appears on the intimal surface, or inner lining, of the artery.
Depending on the artery involved, the coronary or carotid arteries, plaque formation and/or rupture can lead to myocardial infarction, unstable angina, sudden cardiac death, or stroke
atherosclerotic disease in the coronaries can result in chest pain or angina, shortness of breath, fatigue, and arrhythmias. As noted, it may also result in sudden cardiac death.
Manifestations of a stroke include sudden weakness (sometimes noted more on one side than the other), dizziness and loss of coordination, difficulty talking, facial droop, sudden vision problems, and sudden and severe headaches.
If blood supply to the arms or legs is reduced in a similar manner, it can cause significant pain and difficulty walking.
If blood supply is completely occluded peripherally to the affected body part, it can eventually lead to gangrene(death of tissues of the body)
most common site of gangrene is The most common sites include the toes, fingers, hands, and feet.
Medical management
the basic medical treatment is to identify and control the risk factor of developing atherosclerosis.
A decrease in serum LDL-C levels leads to a reduction in the risk of atherosclerotic cardiovascular disease.
antilipidemic is the primary treatment
anticoagulant is also used to decrease clot formation.
Other options include modification in dietary habits
smoking cessation,
lifestyle modifications: exercise and stress reduction plan. Proper management of diabetes is essential.
Surgical management
surgical intervention is reserved for irreverrsible cause of atherosclerosis such as chest pain or gangrene
chest pain caused by CAD require revascularization
gangrene caused by artheriosclerosis might require amputation
Nursing management
disease in the carotid arteries results in; chest pain, SOB, and fatigue.
critical disease in the carotid arteries might be a sign of stroke
Nursing dx
Risk for ineffective tissue perfusion;cerebral, r/t interuption of carotid blood flow
Pain r/t decreased blood flow
Nursing intervention
complete a pt hx with cardiovascular assessment
genetic and environmental link to cardiovascular disease
assess BP from both arms
palpate all pulse in the body; carotid 1 @ time, weak suggest poor flow to through the artery
Auscultation for bruit; heard blood passing through a narrow artery; Bruits often occur in the carotid, aortic, femoral, and popliteal arteries.
High LDL-C levels indicate an increased risk for atherosclerosis. target is less than 100mg/dL
low HDL indicate risk for artherosclerosis; target is less than 40mg/dL
Elevated triglycerides are marker of other lipoproteins; level of 150mg/dL indicate hypertriglyceridemia
High serum levels of homocysteine may block production of nitric oxide on the vascular endothelium, making the cell walls less elastic and permitting plaque to build up.
An HgbA1c of greater than 7% may indicate poor glycemic control.
Action-administer all medication such as antihypertensive and antilipidemia
Teaching- Bp management, lifestyle changes such as healthy diet, smoking cessation, exercise.
Hypertension
Risk factor: stroke, kidney failure, vision loss, dementia, circulation problems such as PAD, premature morbidity and mortality; increase with increase systolic and diastolic rises.
High Bp risk factor:
age: 65 or older
gender: before age 45 men are at risk but sfter 65 women at more risk
race: African American adults
socioeconomic status: low socioeconomic status
Essential or primary hypertension: no medical cause, silent killer, multifactorial, polygenic condition, predisposed factor is genetic and can increase when combined with unhealthy lifestyle such as smoking or poor diet.
4x common in african american than in Caucasian
90-95% of all cases of HTN
Major risk factor of developing HTN
Cigarette smoking
Obesity (body mass index ≥30 kg/m2)
Physical inactivity
Excessive Alcohol use (more than two drinks per day for men and more than one drink per day for women)
Diet
Stress
Dyslipidemia*
Diabetes mellitus- insulin resistance
Microalbuminuria or estimated glomerular filtration rate of less than 60 mL
Age (older than 55 years for men, 65 years for women)
Family history of premature cardiovascular disease (men younger than age 55 years, women younger than age 65 years)
pregnancy
sleep apnea
salt sensitivity
renin elevation- activation of the renin-angiotensin system
Vit D deficiency
cigarette smoking
Endothelial functions
Secondary hypertension: elevations in blood pressure due to a specific cause
Renal parenchymal disease affecting the renal medulla and renal cortex, where the “work” of the kidney is done, is the most common cause of secondary hypertension excluding obesity and alcohol abuse. e.g chronic glomerulonephritis or pyelonephritis, polycystic renal disease, connective tissue disorders and obstructive uropathy
Other causes of secondary hypertension include renovascular disease, pheochromocytoma, Cushing’s syndrome, primary aldosteronism, congenital adrenal hyperplasia, hyperthyroidism, myxedema, and coarctation of the aorta. Excessive alcohol intake and use of oral contraceptives are also common causes of secondary hypertension, as is the use of sympathomimetics, NSAIDs, corticosteroids, cocaine, or licorice.
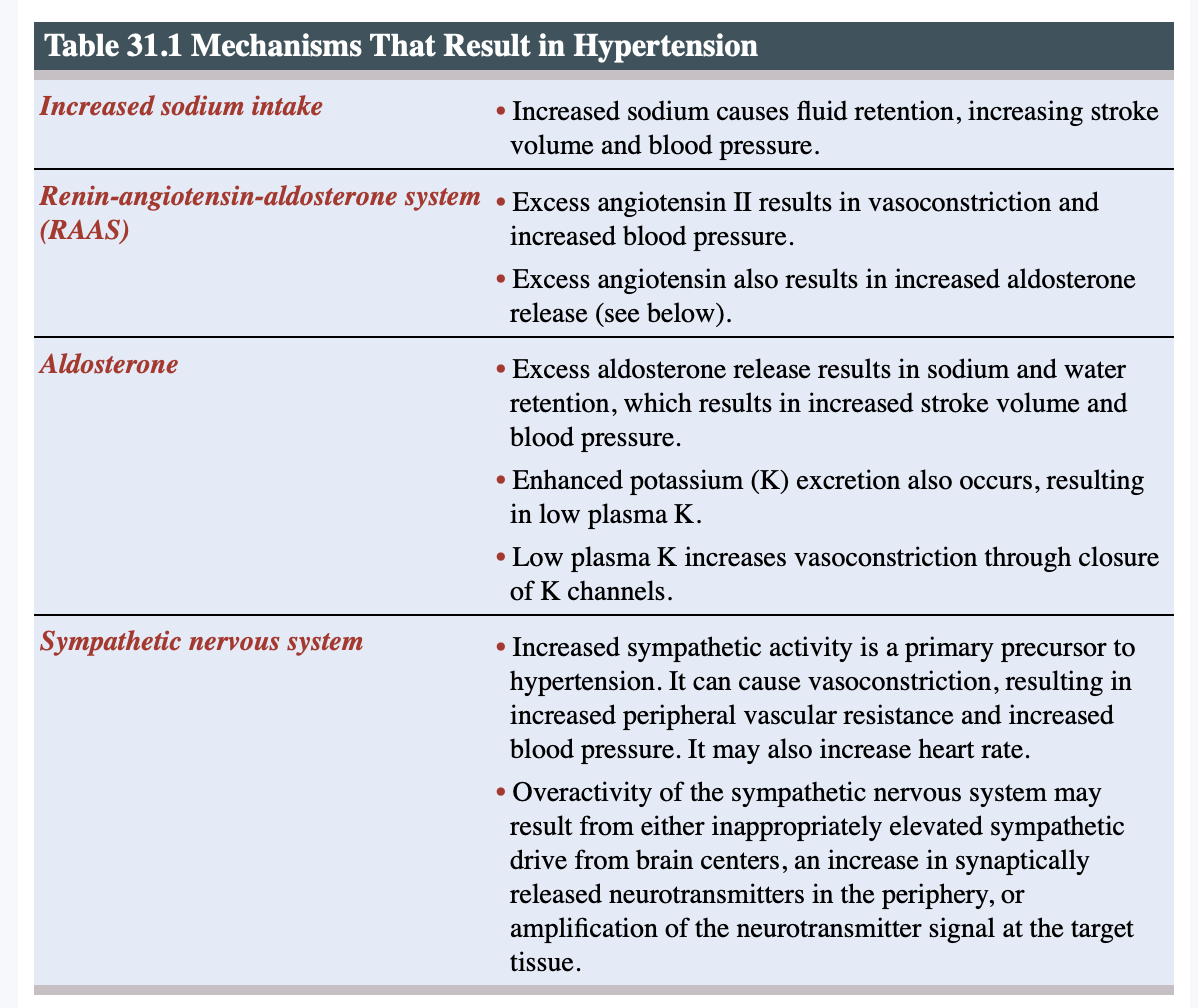
Pathophysiology
Bp is a result of CO* total peripheral vascular resistance (PVR)
pathogenic mechanism involve increase CO, increase PVR or both
Cardiac output= HR*SV
any factor that increases HR increases BP.
any factor that increase PVR increases BP
in early HTN or younger people CO is increased but PVR is normal.
 Clinical manifestation
Clinical manifestation
only result after a long-term increase BP result in target organ damage (TOD)
symptom of chronic uncontrolled HTN: headaches, fatigue, SOB, chest pain, vision changes, renal dysfunction, dizziness, fatigue or nosebled.
clinical manifestations of secondary HTN are result of disease process cause by HTN.
Management
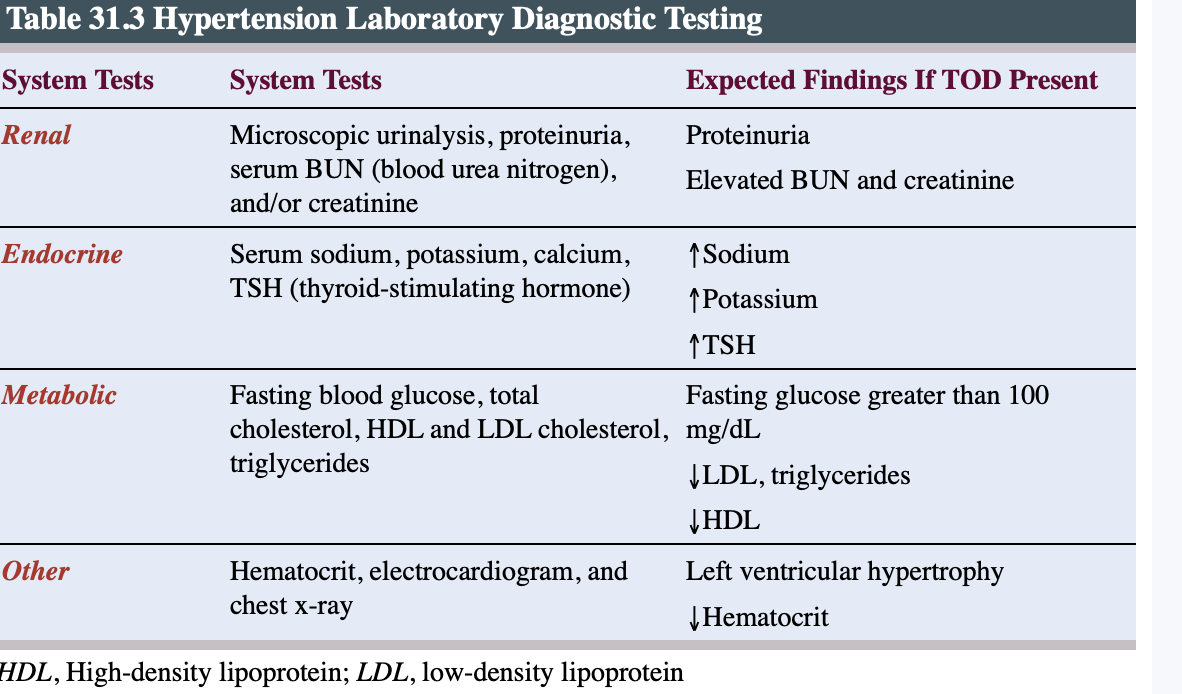
2 or more of properly measured BP reading. dx HTN
identify the undelying cause
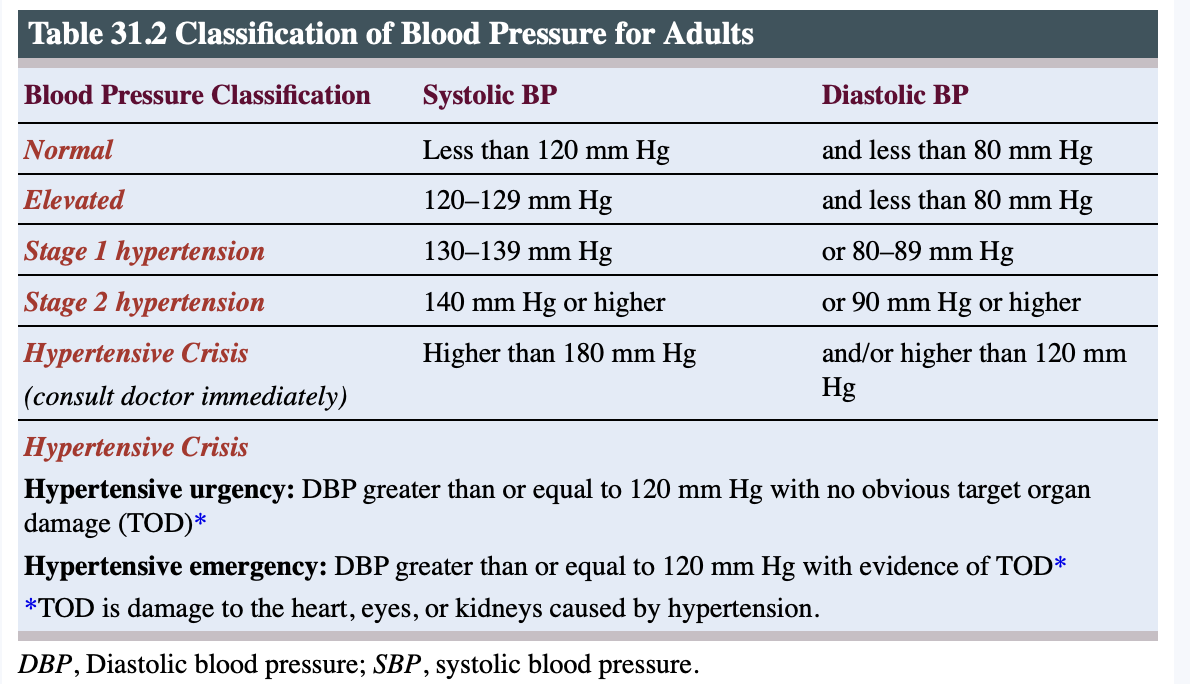
Target organ damage (TOD) is strongly recommended because it allows a better stratification of cardiovascular risk- cause damage to heart, eyes, kidney, lungs.
lower BP
Treatment
To bring high blood pressure down to a healthy level
treatment guidelines recommend healthy lifestyle changes
medication, or both
if a pt Bp is mildly elevated with a BP of 120-129/80mmhg lifestyle changes may be the only option.
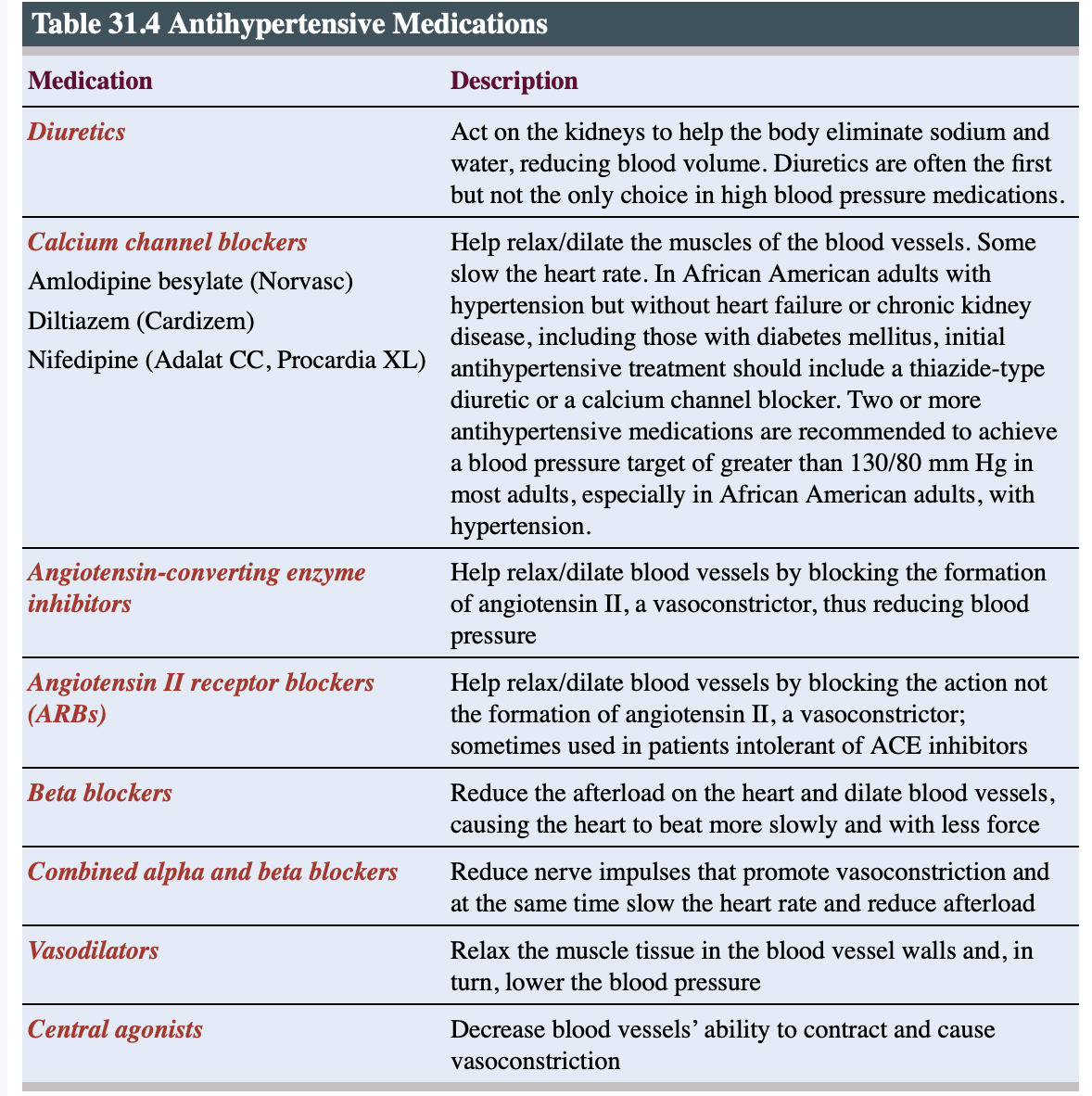
Medication
Recommended of medication @ the beginning of stage 1 if pt had a hx of stroke based on age or DM, chronic kidney disease or calculation of atherosclerotic risk.
lifestyle changes include weight control, diet modification- salt intake, lowering alcohol use and regular exercise and relaxation.
excess weight- esp abd weight raise Bp and blood volume
recommended BMI is 25% and a waist circumference less than 102 in men and 88cm in women.
Diet: high salt is common in pt with. resistant HTN
salt causes fluild retention which boost blood volume and tighten small blood vessels.
more common in older adult, afican american and pt with chronic kidney disease.
if salt is reduce the sys BP can be reduced at least 5-10mm Hg and diastolic 2-6mm Hg
Other dietary considerations include the minerals calcium, magnesium and potassium (found in low-fat and fat-free dairy products, such as milk and yogurt, as well as in produce and dried beans).
They help the body regulate blood pressure; too little can raise blood pressure.
Saturated fat (found in meat, cheese, butter, full-fat dairy products and many processed foods) may also raise blood pressure.
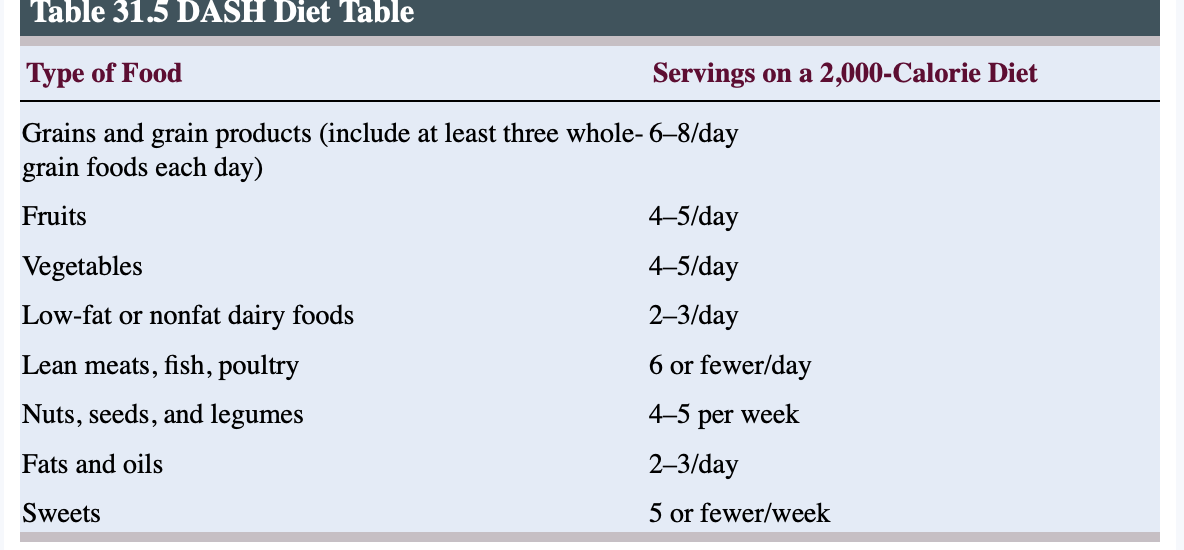
A DASH (Dietary Approaches to Stop Hypertension) diet high in fruits, vegetables, and low-fat dairy products has been shown to lower elevated pressures.
Alcohol consumption patients who quit heavy alcohol drinking reduce their systolic by 7.2 mm Hg and diastolic BP by 6.6 mm Hg. their prevalence can decrease from 42% to 12%. Men are advised not to have more than 2 a day while 1 a day for women.
Exercise- becoming more active can lower systolic BP by an average of 5 to 10 mm Hg,
which is as good as some BP medications.
The ACC/AHA guidelines recommend at least 90 to 150 minutes per week of aerobic activity
Stress management- regularly practicing stress-soothing techniques such as breathing exercises, progressive relaxation, and fitness activities helps the recipient feel better, finding it easier to make other healthy changes.
Complication
silent killer
cause damage to the heart, brain, and kidney(target organ
heart is the most common organ affected; when arterial pressure is high, the heart uses more energy to pump against the increased afterload caused by the elevated pressure in the aorta.
Kidney-principal site of damage is in the arterioles leading to the renal system.
continuous high Bp exert force against the wall which causes it to thicken and narrow the lumen, blood supply is reduced and kidney secretes more renin and Bp is elevated and leads to death of kidney cells.
Stroke
prolonged increases in BP may cause vessel rupture, which leads to hemorrhage and a sudden loss of function, resulting from a disruption of the blood supply to a part of the brain.
It is the fourth-leading cause of death in the United States
aneurysm
An intracranial aneurysm is a dilation of the walls of the cerebral artery that develops as a result of weakness in the arterial wall. The
aneurysm presses on nearby cranial nerves or brain tissue causing damage or ruptures causing subarachnoid hemorrhage and stroke
Hypertensive crisis
acute, severe elevated BP
comprises of 2 conditions
Hypertensive urgency: severely elevated BP (diastolic BP ≥120 mm Hg) with no obvious, acute TOD.
Hypertensive emergency: evidence of TOD which include stroke, papilloedema, HF, aortic dissection.
most serious but least common
Higher in older adults, African Americans, and men
Nursing intervention
Assessment
assess for signs of TO and cerebrovascular disease that may lead to stroke and aneurysm.
early detection and treatment prevent TOD
increase PVR can lead to increased HR or increase SV to compensate for it.
HTN can damage the retinal and leads to retinal hemorrhage
auscultate carotid, abd, and femoral brut; created by blood flow through a stenosed or narrow vessel.
monitor doe abnormal level of renal lab such as serum creatine, BUN, eGFR.
Microalbuminuria is a significant marker of early cardiac, renal, and retinal structural and functional changes in essential hypertension.
Action
administer bp medication
provide pt with DASH diet for meals- 1600mg sodium