Postpartum Care Notes
Postpartum Care: Physiologic Changes
Postpartum Period:
From birth to the return of reproductive organs to a non-pregnant state.
Also known as the "Fourth Trimester" or Puerperium.
Typically lasts from delivery of the placenta to 6 weeks postpartum.
Recovery period is defined as the first 2 hours after birth.
Greatest risks during this time include postpartum hemorrhage (PPH), shock, and infection.
Assessments are done every 15 minutes for the first hour, then every 30 minutes for the next 2 hours.
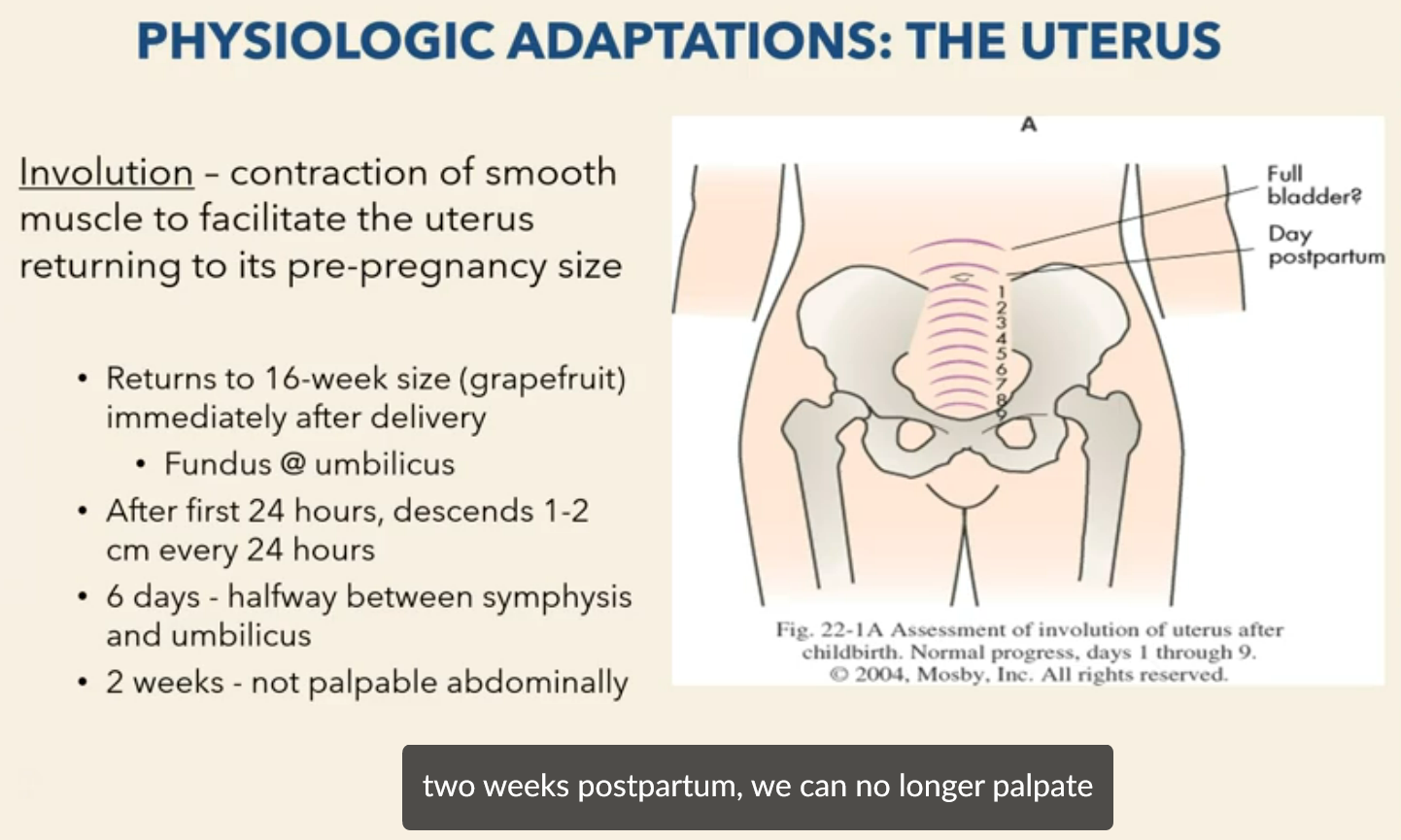
Physiologic Adaptations: The Uterus
Involution: Contraction of smooth muscle to facilitate the uterus returning to its pre-pregnancy size.
Immediately after delivery, the uterus returns to the size of a 16-week pregnancy (grapefruit).
Fundus is located at the umbilicus.
After the first 24 hours, the fundus descends 1-2 cm every 24 hours.
By 6 days postpartum, the fundus is halfway between the symphysis pubis and the umbilicus.
By 2 weeks postpartum, the uterus is typically not palpable abdominally.
Involution & "Afterpains"
Recovery period is a critical phase.
What happens during involution:
Contraction of muscle fibers.
Catabolism: shrinking of myometrial cells.
Regeneration of uterine epithelium.
This is the primary mechanism to prevent postpartum hemorrhage.
Endogenous oxytocin release is stimulated by nipple stimulation.
Exogenous oxytocin (IV administration) reduces PPH by half.
Afterpains are more intense in multiparas and with breastfeeding.
Nursing Actions:
Assess for pain frequently and identify the source.
Comfort measures: relaxation, heat, cold, sitz baths, witch hazel pads, peri bottles.
Medications: NSAIDs, narcotics.
Organize nursing care to allow for rest/naps, especially when the infant is sleeping.
Uterine Assessment
Fundal height: location in relation to the umbilicus.
Placement: midline or deviated.
Consistency: firm or boggy.
Ideally, the patient should void before the assessment.
Subinvolution: the uterus does not return to the normal non-pregnant state.
Factors that slow or cause abnormal involution process:
Over distended uterus.
Long labors.
Retained placenta.
C-sections.
Infection.
Overdistended uterus (twins, triplets, polyhydramnios).
Nursing Actions to facilitate uterine involution:
Administer Oxytocin after placenta.
Encourage early breastfeeding.
Facilitate emptying bladder.
Massage and frequent assessment.
FF @ U refers to fundus firm at umbilicus; FF @ U-1 refers to fundus firm one fingerbreadth below the umbilicus.
Pelvic Floor/Muscle Tone Support
May take 6 months to regain tone.
May be injured during birth, leading to future gynecologic problems.
Most women still look pregnant for a bit after delivery.
Abdominal wall is relaxed for approximately 6 weeks.
Diastasis recti may occur.
Interventions:
Kegels.
Early ambulation.
Body mechanics, posture.
No abdominal exercises after C-section until provider follow up.
Endocrine System
Delivery of the placenta leads to rapid clearance of placental hormones, reversing diabetogenic effects and significantly lowering blood sugar levels in the immediate puerperium.
Estrogen & Progesterone drop immediately after placenta separates and delivers.
Lowest levels at about 1 week postpartum.
Helps with lactation and diuresis of excess extracellular fluid.
Return of Menses:
Nonlactating patients: 4-10 weeks.
Lactating patients: 6+ months.
Urinary System
Kidney function returns to normal within a month; urinary tract structures return to normal within 2-8 weeks.
Diuresis and diaphoresis (especially at night) result in a weight loss of about 5 pounds.
Causes:
Decreased estrogen.
Decrease aldosterone= loose NA and water.
Can be 2500cc/day.
Trauma to urethra and bladder can make voiding difficult (and uncomfortable/painful).
Decreased urge or inability to void.
Full bladder = uterine atony = ^ bleeding.
Urinary System Assessment
Sensation.
Ability to void.
Output.
May be excessive 2-3 days PP.
Amount < 150 = consider urinary retention.
Signs/Symptoms of distended bladder:
Fundal height above umbilicus.
Displaced uterus.
Bladder bulge.
Tenderness or pressure when palpated bladder area.
Excessive lochia.
Interventions:
Frequently empty bladder.
Measure 1st 2-3 voids.
Increase PO fluids.
Consider catheterization.
I&O cath or Foley.
If bladder distended and patient unable to void.
Ambulation Safety
Check blood pressure first.
Assess motor function and sensation after epidural/spinal.
Elevate HOB prior to ambulating.
Dangle at side of bed.
Help client stand and test strength of legs and assess for signs/symptoms dizziness, lightheadedness.
Stay with the patient for their first ambulation.
GI System
Feed Mom!
Bowel tone may be reduced, but bowel function readily returns to normal.
Obstetric trauma can lead to incontinence.
Most have orders for stool softener – offer it!
NOTHING in the rectum for patients with 3rd or 4th degree laceration.
Nursing Interventions:
Water 8 glasses/day.
Ambulate.
Fiber.
Goal is to have BM by day 3 PP.
Assess bowels sounds.
Increased risk for ileus with c/s moms- passing gas to advance diet.
Consider interventions for gas pain.
Cardiovascular System
Average blood loss:
300-500 ml SVD.
700-1500 C/S.
Postpartum diaphoresis and diuresis 2-5 days PP due to elimination of excess fluid.
Stroke volume increases for at least 48 hours due to autotransfusion (may decrease HR to 50).
Cardiac output: remains high in recovery period, returns to pre-labor values at 24-48 hours then gradually returns to normal by 6-8 weeks.
Physiologic flow murmur may be present.
Labs:
HCT: decreases then returns to normal by 8 weeks PP.
HGB: decreases slightly and then rises slowly for 2 weeks PP.
Postpartum leukocytosis:
WBCs - Can rise to 20,000-25,000.
This allows healing and infection prevention.
Coagulation factors - remain hypercoagulable (remains elevated 2-3 weeks PP).
Vital Signs
Temperature may rise to 100.4F/38C due to dehydrating effects of labor; within 24 hours, it should be back to normal. Remember – this is not a fever!!!
Elevation of temp after 24 hours OR that persists >2 days = consider infection.
Respirations should decrease to within the woman's normal pre- pregnancy range within 6-8 weeks.
Pulse returns to nonpregnant levels within a few short days (may be as low as 50 first day pp).
Blood pressure is altered slightly, if at all.
Orthostatic hypotension due to blood redistribution.
Assess:
Compare VS to baseline.
Assess pedal pulse, skin turgor, edema.
Assess for signs/symptoms of DVT.
Interventions:
Fluids – PO.
Early ambulation.
SCDs.
Lovenox if high risk.
Physical Assessment
Standard adult assessment with a few pieces added - or Holistic assessment: labs, immunizations status, admission hx , L&D data, cultural considerations.
Every 15 minutes in recovery, on admission to postpartum, every 4 hours or every shift (if stable).
BUBBLEE:
B - breasts.
U - uterus.
B - bowel.
B - bladder.
L – lochia.
E – episiotomy, laceration or incision.
E – extremities (edema).
E – epidural.
E- emotional status.
Breasts
Sudden decrease in progesterone causes onset of milk production.
Prolactin produces the breastmilk; sustained and effective sucking releases adequate amounts of prolactin.
Oxytocin stimulates milk ejection (letdown); high levels of oxytocin in the first hours after delivery.
Assessment:
Soft, filling, engorged.
Stage of milk development - colostrum or true milk.
Nipple structure, pain, damage.
TEACH: Breast care, supportive bra, no soap to nipples.
Breastmilk
Colostrum- lactogenesis I (2-4 days): High protein (stabilizes infant glucose levels), high antibodies (immune protection; igA, igG), laxative (helps get rid of bilirubin).
Transitional Milk: Starts around the 3rd day, high in fat, calories, lactose.
Mature milk- lactogenesis II: More volume= lower fat, greater volume in early morning hours.
Foremilk- 90% water, low fat, low calories- satisfied thirst= wet diapers.
Hindmilk- creamier, thick, high fat- satisfied hunger= poopy diapers.
Breast Anatomy
External Structure:
Areola: darker area, 2-3 inches diameter, most sensitive part.
Montgomery Glands: bumpy places on the Areola, functions to lubricate skin, lower pH of skin, odor and dark color draw baby to the nipple, may stimulate infant oral cavity.
Nipples: 4-10 openings appear on the surface.
Internal Structure:
Ducts: Transports milk from alveoli to nipple openings.
Lobes: Groups of alveoli, 7-10 in each breast.
Alveoli: Cluster of alveolus, resembles a cluster of grapes.
Breastfeeding Education
Initiate 1st feed within 1-2 hours of birth.
Nurse the baby, not the clock.
Latch q2-3hours 20-40mins ***8-12 times in 24 hours.
Breastfeeding burns 500cal/day.
Drink adequate fluids & EAT.
Assessing for bonding.
Assess latch: no dimples, no smacking, deep latch with good tissue in NB mouth.
Wear well-fitted bra (avoid underwire).
Breastfeeding Holds
Football hold.
Side lying.
Cross cradle.
Cradle hold.
Layed back.
Benefits:
Promotes brain growth.
Fatty acids for brain and CNS development.
Passive antibodies.
Bonding.
Financial.
Engorgement and Mastitis
MASTITIS:
Affects about 1% of women; almost always unilateral.
Develops after milk flow established
Signs/Symptoms: chills, fever, malaise, and local breast tenderness. Pain, swelling, redness and axillary adenopathy may occur.
Most commonly caused by S. Aureus.
Antibiotics are prescribed; maintain lactation by emptying breast q 2-4 hours.
ENGORGEMENT:
Signs/Symptoms: appears tight and full, tender, warm, breast congestion and/or obstruction of the ducts.
Normal occurrence on day 3-5 postpartum.
Hand express first so baby can latch, warm packs before latch, ice after.
Frequent feeds, Tylenol/ibuprofen PRN.
Non-Nursing Mothers
Who shouldn’t breastfeed?
HIV.
Chemo/radiation.
TB.
HSV lesions on breast (can feed on unaffected side).
Teach about lactation suppression:
Tight-fitting, supportive bra 24/7.
No breast/nipple stimulation.
Ice pack (15 on, 45 off, repeat) or cabbage leaves.
Mild analgesics, anti-inflammatory meds.
Postpartum Assessment: BUBBLE-EE
B - breasts.
U - uterus: Fundus – firm, firm with massage, or boggy; Vertical position in relation to umbilicus; Midline or shifted to right or left; TEACH: how to palpate for self, massage.
B - bowel: Bowel sounds (Remember to do this before you assess uterus); Abdomen soft, distended-soft, distended- firm; Tympany; Flatus/BMs; TEACH: fiber/fluids/ambulation, peribottle for cleansing.
B - bladder: Is it full? (consider fundal assessment); Palpable?; Emptying? Measure first 3 voids 150cc or more; Urine quantity, color, clarity; Dysuria; TEACH: Diuresis, peribottle (for cleansing and to stimulate stream).
L – lochia: Post birth uterine discharge; Assess color, amount, odor consistency; Amount: Scant, Light, Moderate: <Heavy- saturating a pad in 1hr, Excessive- saturating pad in 15 mins; Clots- smaller than silver dollar; Odor - fleshy (similar to menstrual blood); TEACH: change pad every couple of hours, at least every time to bathroom, peribottle, change over time, amt for concern.
E – episiotomy, laceration or incision: Roll Mom to her side and separate the buttocks to visualize the perineum; Check for REEDA (Redness, Edema, Ecchymosis, Discharge, Approximation); Check for hemorrhoids; Check for hematomas; If applicable, assess cesarean incision; TEACH: Peribottle, changing pad & wiping front to back, wipe gently, Sitz bath, dermaplast.
E – extremities (edema).
E – epidural.
E- emotional status.
Lochia
Post birth uterine discharge.
Assess color, amount, odor consistency.
Amount:
Scant.
Light.
Moderate.
<Heavy- saturating a pad in 1hr.
Excessive- saturating pad in 15 mins.
Clots- smaller than silver dollar.
Odor - fleshy (similar to menstrual blood).
TEACH: change pad every couple of hours, at least every time to the bathroom, peribottle, change over time, amt for concern.
Lochia Types
Rubra - appears red & bloody, birth to 3-4 days – may have small clots.
Serosa - becomes pink or brown, begins day 3-4 and may last up to 22-27 days.
Alba – (primarily of leukocytes )may drain 6 weeks or longer; average is 10-14 days.
TEACH:
Change pad every couple of hours.
Perform hand hygiene when doing perineal care.
Use peri-bottle.
Wipe/blot front to back.
Nothing in the vagina for 6 weeks.
Multips have heavier bleeding than primips.
Bleeding may be lighter in cesarean sections vs vaginal delivery.
Episiotomy and Lacerations
Roll Mom to her side and separate the buttocks to visualize the perineum.
Check for REEDA.
Check for hemorrhoids; Check for hematomas.
If applicable, assess cesarean incision.
TEACH: Peribottle, changing pad & wiping front to back, wipe gently, Sitz bath, dermaplast.
LACERATION:
1st Degree - extends through the skin and structures superficial to the muscles.
2nd Degree - extends through muscles.
3rd Degree - continues through anal sphincter muscle (NO rectal suppositories).
4th Degree - extends through anterior rectal wall (NO rectal suppositories).
Other types:
Vaginal sidewall lacerations.
Periurethral lacerations, Abrasion “skid mark”, clitoral.
Laceration risk factors: macrosomia, rapid delivery, operative delivery, nulliparity, congenital abnormalities of maternal soft parts; contracted pelvis, skill level of delivery attendant; Requires Surgical repair.
Ice to perineum for 24 hours, Sitz bath after 24 hours (20 min BID), Analgesics only if needed (PO vs Topical).
Extremities, Edema & Epidural Site
Assessment of extremities (edema) and epidural site.
VTE Prevention
Venous thromboembolism (VTE); Most likely cause = DVT.
Risk factors:
Pregnancy.
Prolonged immobility (bedrest, c-section).
Obesity, Smoking, Multiple gestation, Age, Hx of thromboembolism.
Assess:
Leg pain, Warmth, redness, edema, Calf enlargement and pain, heaving aching
Infant Security
Inform parents of infant security plan.
Instruct not to give baby to anyone without proper identification.
Always match bands.
Postpartum Hemorrhage (PPH)
Accounts for 25% of maternal deaths.
Cumulative blood loss of >1000ml with signs/symptoms of hypovolemia.
Saturating a perineal pad in 15 or less and collection of blood under patient.
EBL (estimated blood loss) vs QBL (quantified blood loss).
Late PPH:
Occurs 24 hours to 6 weeks after delivery; may cause rapid onset of shock.
Causes - retained placental fragments, subinvolution, infection, lacerations.
The 4 T's of PPH:
Tone: (atony).
Trauma: (lacerations, expanding hematoma or uterine rupture).
Tissue: (retained placental tissue).
Thrombin (coags).
Traction: pulling on the umbilical cord>uterine inversion.
Prevention of Excessive Bleeding
Uterine atony is the leading cause of early PPH.
Uterine massage - gentle massage to firm uterus and expel clots – MASSAGE 1ST BEFORE you attempt to express clots!
Prevent bladder distention - assist to the bathroom, teach mother importance of emptying the bladder catheterize if necessary.
Soft boggy uterus accounts for > 90% of PP hemorrhage.
2/3 of PP hemorrhages occur without any predisposing factors.
Risk factors for uterine atony:
Overdistended uterus – macrosomia, multifetal pregnancy, polyhydramnios.
Anesthesia and analgesia, H/O uterine atony.
High parity, Prolonged labor; oxytocin induction.
Trauma during labor and birth – operative abdominal or vaginal delivery.
Managing Trauma
Suspect a pelvic hematoma if a woman reports a persistent perineal or rectal pain or a feeling of vaginal pressure: Bleeding into the tissues of the reproductive tract.
Increasing perineal or pelvic pain, Perineal, pelvic, or rectal pressure, Difficulty voiding.
Bulging, bluish swelling painful to palpate; Suspect laceration with steady bright red bleeding and firm fundus.
Where is the Bleeding Coming From?
Uterus: Fundus boggy, Lochia dark, Diminishes with massage or oxytocic's.
Laceration: Fundus firm, Frank, bright red bleeding.
PPH Interventions
Massage, Empty bladder, VS q5min, O2, EKG; IV x2 at least an 18g, Oxytocin.
Labs- type and cross, CBC, Pt/PTT/Fibrinogen, Balloon tamponade.
Massive blood transfusion protocol: Whole blood, PRBC, PLT’s, Fresh Frozen Plasma, Cryoprecipitate.
PPH Management
Massage, Breastfeeding, Bimanual Massage; Compression.
Medications:
Oxytocin (Syntocinon® Pitocin®) first line.
Methylergonovine (Methergine®) don’t give with HTN.
Prostaglandin F2alpha – (Hemabate®) don’t give with asthmatic.
Misoprostol – (Cytotec®)– off-label use.
Tranexamic Acid (TXA)- stops the breakdown of fibrinogen and fibrin clots. Given with trauma.
Last resort – Hysterectomy.
Infection Prevention
Standard precautions and handwashing - for all staff, parents, visitors.
Teach mother perineal care (peri bottle).
Teach mother to change pads with each trip to the bathroom and to remove and replace pad front to back.
Signs/Symptoms:
Maternal temp >100.4 on two successive PP days, not including the 24 hours after delivery.
Fever, localized pain, redness, swelling, purulent discharge, dysuria.
Risk factors: vaginal exams and procedures, trauma, hemorrhage.
Pathogens – numerous streptococci and anaerobic organisms most common.
Reproductive Tract Infections
Chorioamnionitis- a disorder characterized by acute inflammation of the membranes and fetal portion (chorion) of the placenta, typically due to polymicrobial bacterial infection in patients whose membranes have ruptured.
Endometritis - infection of uterine lining, fever, chills, flu-like symptoms, prolonged afterpains, uterine tenderness, foul lochia.
Parametritis - pelvic cellulitis, infection into the broad ligaments, usually unilateral, may progress to pelvic abscess.
Peritonitis - infection of the peritoneum, may lead to ileus.
Risk factors:
Cesarean Section – most significant risk.
PROM, Multiple vaginal exams, Compromised health status, Internal monitors, Trauma.
Chorioamnionitis, vaginal infections, Operative vaginal delivery, Manual extraction of placenta.
Wound Infection Signs and Symptoms
Wound warmth, Erythema, Tenderness, Pain, Edema, Seropurulent drainage.
Wound dehiscence, Evisceration, Temp >100.4 X 2 consec days.
Family Adaptation
Attachment: formation of a relationship between a parent and a newborn through physical and emotional interactions.
Taking in- mom is focused on herself, lasts 2 days (birth – 48 hours), reviews birth experience, dependent and passive.
Taking hold- concerned about her care and infants care, often feels vulnerable, mood swings, begins day 2-3 but last 10 days (up to several weeks).
Letting go- reestablishes relations with others (partner, children), confidence grows, focus on family unit.
Nursing Actions to Facilitate Bonding
Engrossment: a time of intense absorption, preoccupation, and interest in the newborn as a partner develops a bond.
Skin to skin; can be done with partner as well; Newborn facing position - observe similarities in features; Rooming in.
Quiet and private environment, Teach about newborn care, Encourage cuddling, bathing, feeding, diapering, swaddling, talking, singing, reading, etc.
Provide praise, support, and reassurance; Allow parents to express their feelings.
Postpartum Mood Disorders
Mood and anxiety disorders likely to start in or present itself in the post-partum time frame.
Can impact how the mother and family adapt to the newborn.
Baby Blues
Up to 85% of women experience “The Blues”; Does not interfere with caring for self or newborn.
Usually peaks day 2-3 and lasts up to 3 weeks; Typically resolves in 10 days without intervention.
Signs/Symptoms:
Feelings of sadness, Lack of appetite, Sleep pattern disturbances; Feeling of inadequacies.
Crying easily for no apparent reason; Restlessness, insomnia, fatigue, Headache, Anxiety, anger, sadness.
Letdown feeling, irritability.
Postpartum Depression (PPD)
Definition: Depression occurring within 12 months of childbirth lasting longer than postpartum blues; can interfere with the ADL’s and caring for the infant.
Occurs in approx 10-20% of postpartum women (up to 60% in adolescent mothers); May be influenced by estrogen fluctuations.
NEED TO look for post-partum patients who are agitated, overactive, confused, complaining, or suspicious.
Treatment:
Psychotherapy, antidepressants, or antianxiety medications.
Encourage her to ask for help from friends, family, SO (remember the lack of support system is a factor in developing PPD), Sleep, exercise, and nutrition.
Signs and Symptoms:
Feelings of guilt and inadequacies, Irritability, Anxiety, Fatigue persisting beyond a reasonable amount of time, Feeling of loss, Lack of appetite.
Persistent feelings of sadness, Intense mood swings, Sleep pattern disturbances, Thoughts of harming self or newborn.
PPD Risk Factors
Primip, Hx of PPD, History of depression, including prenatal depression, Low self-esteem, Traumatic delivery.
Lack of social support, Unresolved feelings about the pregnancy, Single with multiple life stressors.
Fatigue from delivery and change in sleep patterns, May be caused by biological, psychologic, situational, or multifactorial.
Frequently have had prior major depressive disorder or personal and family history of psychiatric disorders.
Postpartum Psychosis
Medical Emergency!!!. With Psychotic Features: 0.1-0.2% of pp women; Usually presents itself in the first 2 weeks pp.
Includes auditory or visual hallucinations, elements of delirium, poor impulse control and judgment, delusions.
Increased risk of suicide &/or homicide, May have auditory hallucinations related to injuring or killing infant.
Hospitalization required, Tends to reoccur.
Discharge Teaching
Rubella vaccination - requires maternal consent; avoid pregnancy for at least 1 month (some recommend 2-3 months).
Varicella vaccination before d/c and at 1st PP visit, TDAP vaccine, Signs/Symptoms infection, excessive bleeding, pain, swelling of one leg.
Follow up appointments for mom and baby; May be reluctant to bring it up – resuming sexual intimacy (contraception, fear, pain, decreased vaginal moisture).
Self-care and signs of complications; Sexual activity - pelvic rest for 6 weeks, Contraception - consider lactation.
Prescribed medications and continue prenatal vitamins (*iron); Check-ups and follow-ups
Resources - telephone follow-up, warm lines, support groups, community resources.
Birth Control Review of Types
Abstinence, Male or Female condom, Diaphragm or cervical cap.
Oral birth control pills – variety of strengths with varying amounts of a combination of hormones(estrogen/progestin) – requires prescription, taken daily.
Progestin only- fewer side effects- can take while breastfeeding or w/ hx of DVT/high BP, Injectables – typically every 12 weeks – when started? (5 days after delivery/menstrual period).
Implantable (Implanon: left in to approx. 4 years, When started?, IUDs – good for 5-10 years, may be with or without hormones.
Surgical- Bilateral tubal / bilateral salpingectomy- decreases risk for ovarian cancer by 50%.
Risk of adverse effects with hormonal contraceptives: thromboembolism; doesn’t prevent STI.
Essential Discharge Teaching
Focus teaching based on patient’s education level, health literacy, and language.
INCLUDE Teaching on:
Pain and discomfort, Immunizations, Nutrition, Activity and exercise.
Infant Care, Lactation, Sex and contraception, Follow up.
-
Postpartum Assessment (BUBBLES)
B - Breasts: Soft, filling, engorged; colostrum or true milk; nipple structure, pain, damage. Action: Teach breast care, supportive bra, avoid soap on nipples.
U - Uterus: Fundus – firm, firm with massage, or boggy; Vertical position in relation to umbilicus; Midline or shifted to right or left. Action: Teach self-palpation and massage.
B - Bowel: Bowel sounds; Abdomen soft, distended-soft, distended-firm; Tympany; Flatus/BMs. Action: Teach fiber/fluids/ambulation, peribottle for cleansing.
B - Bladder: Is it full? Palpable? Emptying? Measure first 3 voids >150cc; Urine quantity, color, clarity; Dysuria. Action: Teach diuresis, peribottle.
L - Lochia: Color, amount, odor consistency; Scant, Light, Moderate, Heavy, Excessive; Clots; Odor. Action: Teach pad changes, peribottle, amount for concern.
E - Episiotomy/Laceration/Incision: REEDA, hemorrhoids, hematomas, cesarean incision. Action: Teach Peribottle, changing pad, Sitz bath, dermaplast.
E - Extremities: Edema, DVT signs.
E - Emotional Status: Assess mood, bonding.
Anatomic and Physiologic Changes
Uterus: Involution (contraction), fundus descends 1-2 cm every 24 hours, returns to pre-pregnancy size by 6 weeks.
Involution - contraction of smooth muscle to facilitate the uterus returning to its pre-pregnancy size
Returns to 16- week size (grapefruit) immediately after delivery
Fundus @ umbilicus
After first 24 hours, descends 1-2 cm every 24 hours
6 days - halfway between symphysis and umbilicus
2 weeks - not palpable abdominally
Lochia: Rubra, serosa, alba.
Endocrine: Estrogen and progesterone drop, prolactin increases with breastfeeding.
Urinary: Diuresis, diaphoresis.
Cardiovascular: Blood volume decreases, cardiac output returns to normal by 6-8 weeks.
GI: Bowel tone reduced.
Normal vs. Abnormal Findings
Uterine Involution:
Normal: Firm fundus, descends daily.
Abnormal: Boggy uterus, subinvolution (caused by retained placenta, infection, overdistention).
Lochia Flow:
Normal: Rubra (3-4 days), serosa (up to 27 days), alba (10-14 days).
Abnormal: Heavy bleeding (saturating pad in 1 hour), large clots, foul odor.
Voiding/Stooling:
Normal: Diuresis, spontaneous bowel movement by day 2-3.
Abnormal: Urinary retention, constipation.
Vital Signs:
Normal: Temp up to 100.4F in first 24 hours, HR returns to pre-pregnant levels.
Abnormal: Fever after 24 hours, elevated BP, signs of DVT.
Laceration Degrees
1st Degree: Skin and superficial structures.
2nd Degree: Through muscles of the perineal body.
3rd Degree: Through anal sphincter muscle.
4th Degree: Through anterior rectal wall.
Systematic Assessment Sequence
Vital signs.
Breasts.
Uterus (fundal height, placement, consistency).
Bowel.
Bladder.
Lochia.
Episiotomy/laceration/incision (REEDA).
Extremities.
Emotional status.
Key Teaching Opportunities
Self-Care: Perineal care, hygiene, nutrition, rest.
Newborn Care: Feeding, diapering, cord care, safe sleep.
Complications: Signs of infection, PPH, DVT, mood disorders.
Follow-Up: Appointments for mom and baby.
Maternal, Paternal, and Sibling Adaptation
Maternal:
Taking-in: Focused on self, reviewing birth experience.
Taking-hold: Concerned about self and infant care, mood swings.
Letting-go: Reestablishes relationships, focuses on family unit.
Paternal: Engrossment (intense interest in the newborn).
Sibling: Adjustment to new family member.
Factors Affecting Attachment
Parent: Emotional well-being, support system, previous experiences.
Infant: Temperament, health status.
Interventions: Skin-to-skin, rooming-in, teaching newborn care.
Contraception
Risks: Thromboembolism (hormonal methods), infection (IUD).
Benefits: Prevents unwanted pregnancy, spacing births.
Teaching: Proper use, side effects, contraindications.
Postpartum Complications
Causes of Deviations
Vaginal Delivery: Lacerations, hematomas, infection.
C-Section: Infection, hemorrhage, thromboembolism.
Common Complications
PPH: Risk factors (uterine atony, lacerations), assessment (fundal height, lochia), prevention (uterine massage, oxytocin), management (medications, transfusion).
Infection: Risk factors (C-section, PROM), assessment (fever, wound assessment), prevention (hand hygiene, perineal care), management (antibiotics).
Thromboembolic Disorders: Risk factors (immobility, hypercoagulability), assessment (leg pain, edema), prevention (ambulation, SCDs), management (anticoagulants).
Postpartum Hemorrhage
Early PPH: Uterine atony, lacerations, retained placental fragments.
Late PPH: Subinvolution, infection.
Uterine Atony: Boggy uterus, massage and oxytocics.
Bleeding Lacerations: Firm fundus, bright red bleeding, surgical repair.
Immediate/Urgent Actions for PPH
Massage uterus.
Empty bladder.
Administer oxygen.
Establish IV access.
Administer medications (oxytocin, misoprostol, etc.).
Call for help.
Pharmacologic Agents
Oxytocin: First-line, contracts uterus.
Methylergonovine: Contraindicated in HTN.
Misoprostol: Off-label use, contracts uterus.
Tranexamic Acid (TXA): stops the breakdown of fibrinogen and fibrin clots. Given with trauma.
Postpartum Infections
Assessment: Fever, wound assessment, lochia assessment.
Laboratory Data: Elevated WBCs.
Treatment: Antibiotics.
Thromboembolic Disorders
Risk Factors: Hypercoagulability, immobility, C-section.
Treatment: Anticoagulants, compression stockings.
Postpartum Mood Disorders
Baby Blues: Transient sadness, resolves within 2 weeks.
Postpartum Depression: Persistent sadness, anxiety, interferes with ADLs, treat with therapy and/or medication.
Postpartum Psychosis: Hallucinations, delusions, risk of harm to self or infant, requires hospitalization.