EEG
Las pruebas neurofisiológicas complementan el examen neurológico y las imágenes convencionales (p. ej., tomografía computarizada, resonancia magnética) al evaluar la función nerviosa, muscular y/o cerebral.
La prueba neurofisiológica más utilizada es la electroencefalografía (EEG), que mide la fluctuación del potencial eléctrico en diferentes regiones de la corteza. El EEG se utiliza a menudo para evaluar la epilepsia y los trastornos del sueño.
Los potenciales evocados (PE) son fluctuaciones de microvoltios del SNC en respuesta a la estimulación de órganos sensoriales o de un nervio periférico. Estas fluctuaciones pueden registrarse mediante un EEG y pueden usarse para detectar desmielinización de la sustancia blanca (p. ej., esclerosis múltiple).
Los estudios de conducción nerviosa (NCS) evalúan la conducción de los impulsos nerviosos a través de los nervios periféricos y se utilizan para especificar el tipo de daño nervioso (desmielinización, compresión o sección de un nervio).
La electromiografía (EMG) mide la actividad eléctrica de los músculos en reposo y durante la contracción. La EMG es útil para diferenciar las neuropatías de las miopatías.
Electroencephalography (EEG)
Definition: a recording that shows the fluctuation of net electrical potential at different points on the cerebral cortex
Principle: Every neuron generates an electrical potential irrespective of the degree of neuronal firing. EEG electrodes add up these electrical potentials at different points, which allows visualization of neuronal activity of different areas of the cortex. The entire EEG recording is then examined for physiological or pathological patterns of electrical activity.
Procedure
6–19 electrodes are symmetrically placed on the scalp and the electrical activity is measured
6 electrodes are used during polysomnography, while 19 are required for neurological diagnostics. The 19 electrodes are placed evenly across the scalp according to the 10–20 system. Each electrode is denoted by an alphabet and a numeral. The alphabets are: O → occipital,T → temporal,F → frontal,P → parietal,Fp → frontal pole. Odd numbers are used for the left hemisphere and even numbers for the right hemisphere. E.g., O1 represents the left-occipital electrode.
The potential difference between two electrodes is measured and represented as line tracing.
E.g., The tracing O1P3 represents the potential difference between the left-occipital and left-parietal electrodes.
Indications
Epilepsy diagnostics: for first seizures with unclear cause, insufficient classification, or treatment-refractory seizures (see “Epileptic syndromes” and “Seizure disorders”)
The absence of characteristic epilepsy findings cannot, however, rule out epilepsy.
To determine the level of consciousness (bispectral index to determine the depth of anesthesia; diagnosis of brain death)
As a part of polysomnography (to identify the different phases of sleep)
Interpretation: The following steps should be followed when interpreting an EEG:
Define the background electrical activity of the brain. This baseline EEG serves as a control.
Sleeping patients have slower electrical activity. Also, different EEG patterns may overlap.
Look for physiological or pathological patterns of electrical activity (see “EEG patterns”).
Localize the pathology by identifying the EEG tracing associated with abnormal electrical activity.
Physiological EEG waveforms | ||
|---|---|---|
Wave type | Frequency | Stage of onset |
Alpha waves | 8–12 Hz |
|
Beta waves | 13–30 Hz |
|
Gamma waves | > 30 Hz |
|
Delta waves (EEG) | 0.1–4 Hz |
|
Theta waves | 4–8 Hz |
|
EEG patterns
Physiological EEG patterns | ||
|---|---|---|
Patterns | Characteristics | Occurrence |
Vertex waves (V waves) |
|
|
Sleep spindles |
|
|
K complex |
|
|
POSTS (positive occipital sharp transients of sleep) |
|
|
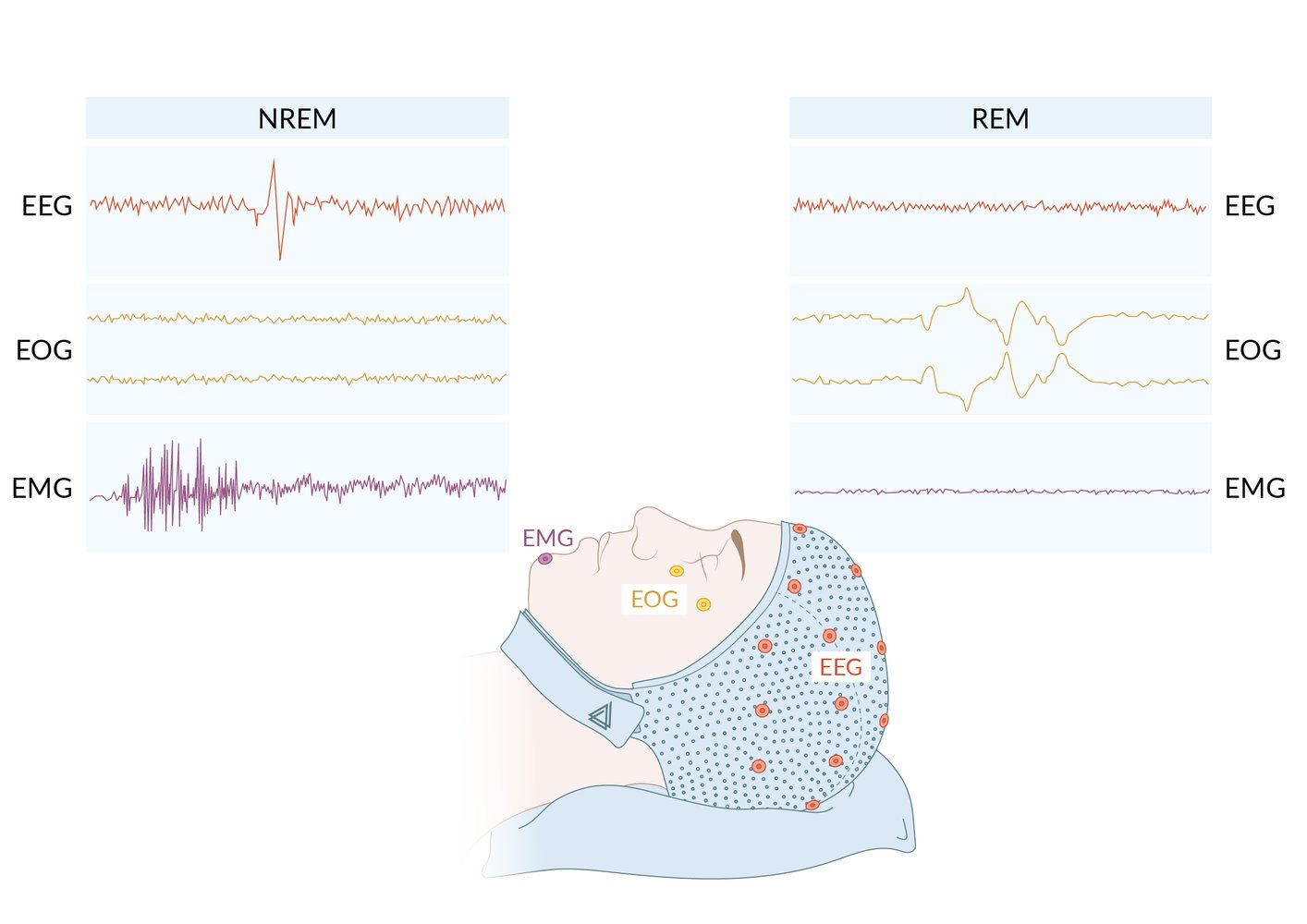 Description: NREM and REM
Description: NREM and REM
NREM sleep: EEG tracings show relatively slow (0-7 Hz, depending on which stage of NREM sleep), medium-amplitude waves with periodic high amplitude, diphasic (negative waveform followed by positive waveform) waves (K-complexes, seen in fronto-central head regions), and sleep spindles (not shown). EOG shows a relatively low amplitude and even pattern, indicating no eye movements. EMG shows fast waves, with some areas of high amplitude.
REM sleep: EEG tracings show faster (typically >13 Hz) waves of low amplitude. EOG shows jagged, irregular peaks and valleys (each curve mirrors the other, with each line representing one eye) consistent with eye movement. EMG is near-flatline, consistent with maximum muscle relaxation during REM sleep.
EEG = Electroencephalography
EOG = Electrooculography
EMG = Electromyography
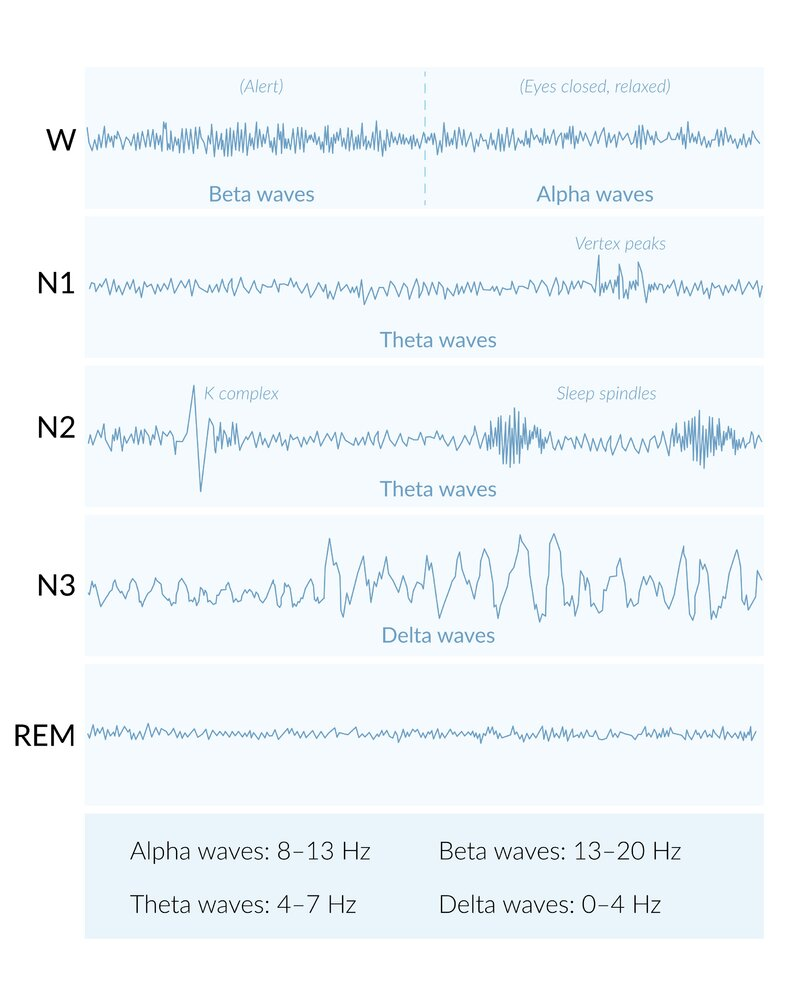 Description: W (beta and alpha waves): relaxed stage of wakefulness
Description: W (beta and alpha waves): relaxed stage of wakefulness
N1 (alpha and theta waves): transitional stage between wakeful and sleep
N2 (theta waves): beginning of sleep phase
N3 (delta waves): transitional stage between light and deep sleep
REM: deep or dreamstate sleep
Note: REM sleep has its own phase and waveforms not illustrated here
Pathological EEG patterns | |||
|---|---|---|---|
Patterns | Characteristics | Occurrence | |
Slow activity |
|
| |
Paroxysmal discharge |
|
| |
Sharp wave |
|
| |
Spike (EEG) |
|
| |
Spike-and-wave activity |
|
|
|
|
| ||
Polyspike and polyspike-wave complex |
|
| |
Periodic sharp wave complex |
|
| |
Hypsarrhythmia |
|
| |
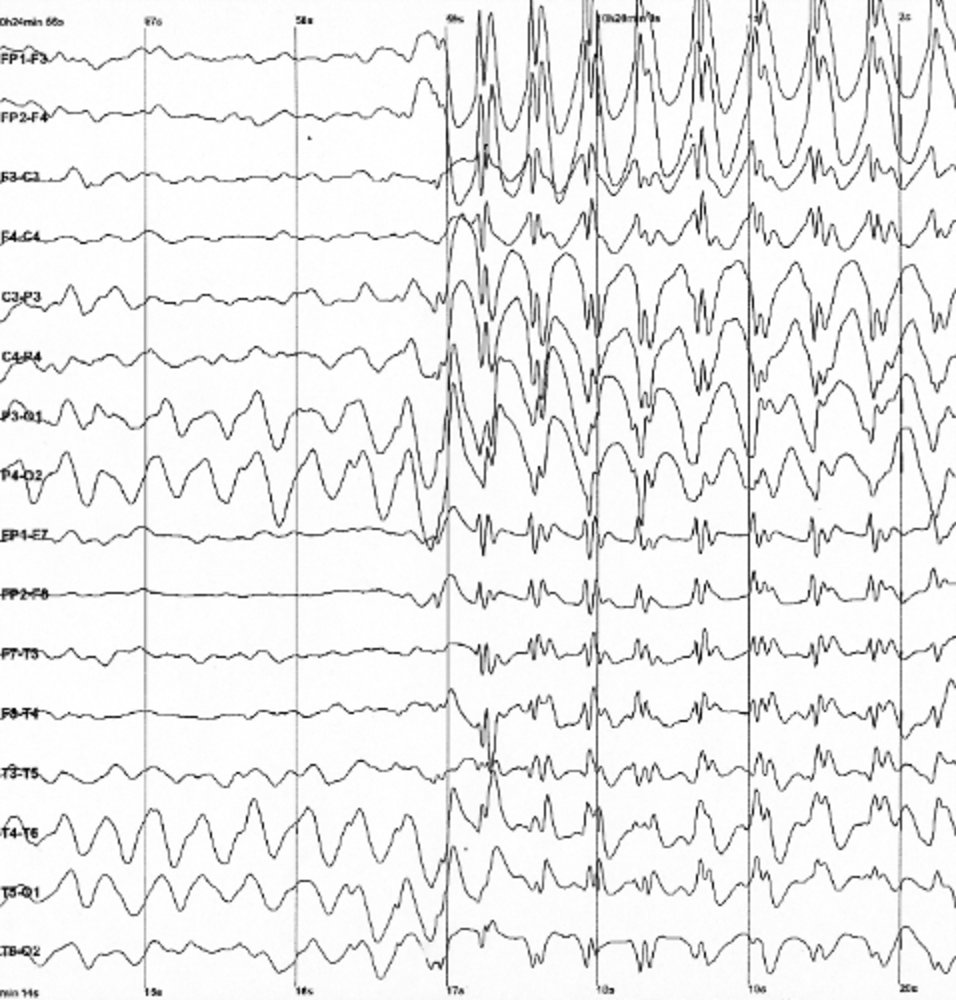 Image description: EEG with a frequency of 3/s spike waves in a child with absence seizures
Image description: EEG with a frequency of 3/s spike waves in a child with absence seizures
 Image description: EEG findings in absence seizures
Image description: EEG findings in absence seizures
Characteristic 3 Hz spikes and waves. The steep rise is the spike and the flat increase the wave. This complex usually occurs with a frequency of 3 per second (hence its name). This finding most commonly occurs during a seizure in absence epilepsy; it can also be seen in a seizure-free interval (interictal).
Evoked potentials
Definition: the electrical response of the CNS (as measured by an EEG) to stimulation of sensory organs or a peripheral nerve.
Based on the type of stimulus, evoked potentials may be visual, auditory, somatosensory, or motor.
Interpretation: Neurological diseases increase the latency and/or decrease the amplitude of the EP.
Types of evoked potential | Stimulus | Indication |
|---|---|---|
Visual evoked potential (VEP) |
|
|
Brainstem auditory evoked potential (AEP) |
|
|
Somatosensory evoked potential (SEP) |
|
|
Motor evoked potential (MEP) |
|
|
Nerve conduction study (NCS)
A direct electrical stimulus is applied to a motor nerve (motor nerve conduction study) and/or sensory nerve (sensory nerve conduction study) via surface electrodes at two or more points, and various parameters related to compound action potentials (CMAPs) are measured.
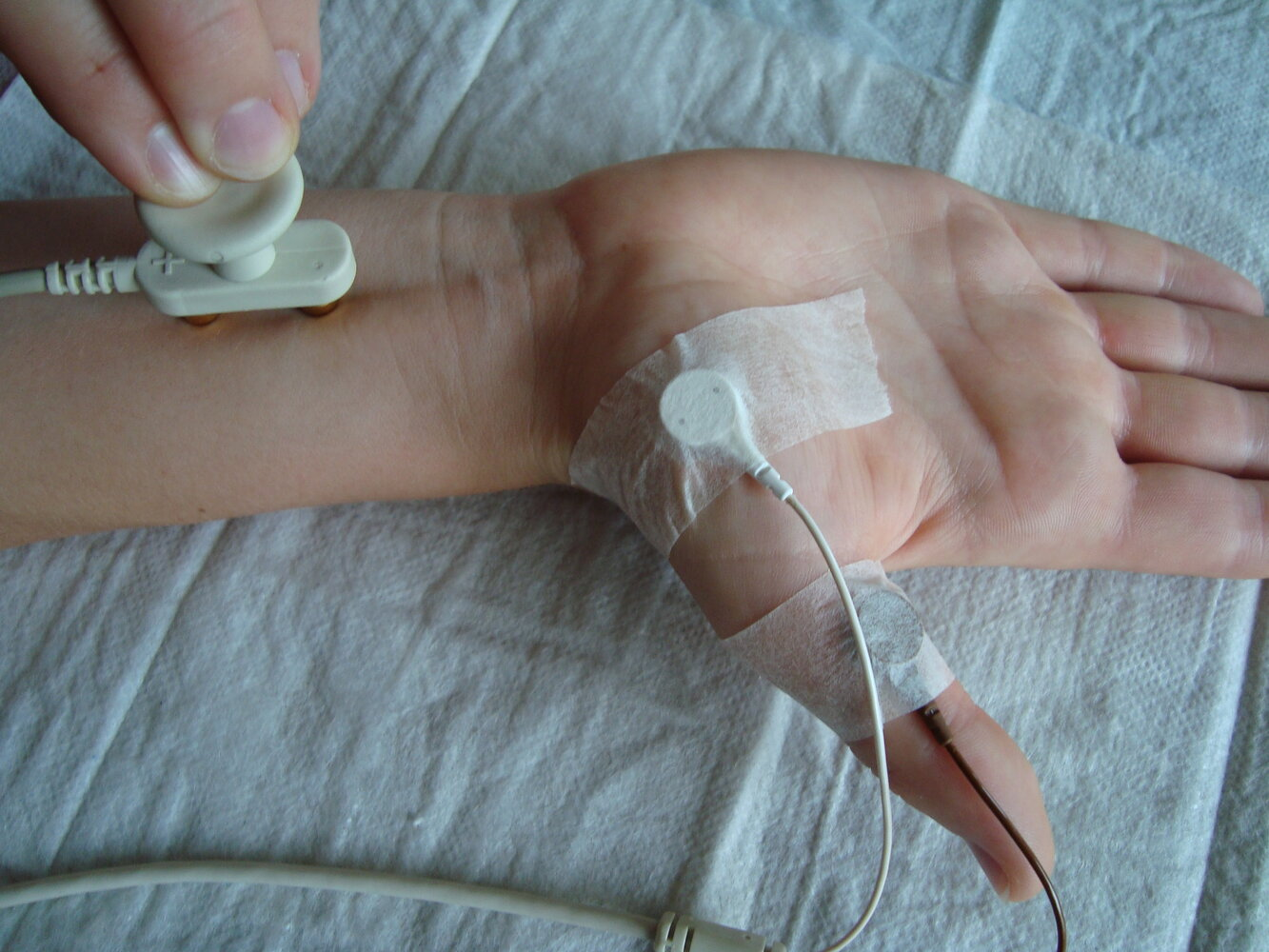 Description: Nerve conduction study
Description: Nerve conduction study
The right forearm and hand of a patient undergoing a median motor nerve conduction study
The recording electrodes have been placed over the abductor pollicis brevis muscle on the thenar eminence (white electrode) and further distal on the thumb (brown electrode). The stimulating electrodes (anode and cathode) have been placed a set distance away from the recording electrodes over the median nerve on the forearm. A mild electrical impulse is discharged from the stimulating electrodes and the activity is registered by the recording electrodes.
Sensory nerve conduction study
Definition: recording of a purely sensory portion of a nerve in response to electrical nerve stimulation
Indication: to determine whether sensory symptoms arise proximal or distal to the dorsal root ganglia
Sensory nerve conduction studies are normal in the case of a pathology proximal to the dorsal root ganglia.
Motor nerve conduction studies
Definition: Recording of a muscle's compound action potentials (CMAP) after stimulation of its innervating motor nerve.
Measured parameters
Nerve conduction velocity: ↓ nerve conduction velocity indicates nerve demyelination and/or nerve compression (e.g., carpal tunnel syndrome - median nerve compressed in flexor retinaculum)
The two factors that affect the velocity of a nerve impulse are axonal thickness and myelination (myelination allows faster saltatory conduction). Therefore, demyelination decreases nerve conduction velocity. Axonal lesions (except complete nerve transection) have little or no effect on nerve conduction velocity.
Amplitude of the CMAPs
Indirectly represents the area under the curve of the CMAP, which represents the summation of all axons of the motor nerve that was stimulated.
↓ CMAP amplitude → axonopathy or temporal dispersion due to axonal injury
Distal motor latency: time period from stimulation of the motor nerve to action potential
F-wave latency: a second action potential generated by the antidromic (proximal) conduction of the nerve that was stimulated
While physiological nerve conduction is unidirectional, external stimulation of a peripheral motor nerve generates an impulse that travels bidirectionally: towards the muscle (orthodromic conduction) and towards the spinal cord (antidromic conduction). The latter impulse stimulates the anterior horn cells, which generate a secondary impulse that travels antidromically and elicits a secondary muscle response. Damage to the anterior horns cells (e.g., Guillain-Barré syndrome) may increase F-wave latency.
Electromyography (EMG)
Definition: A diagnostic test that measures the activity of muscles in response to neural stimulation, in order to detect dysfunction at the level of the neuromuscular junction, the muscle, or the corresponding nerve.
Indications
Differentiate neuropathic from myopathic muscle weakness
Neuropathy: e.g., carpal tunnel syndrome, Guillain-Barré syndrome
Myopathy: e.g., polymyositis, muscular dystrophy
Determine the prognosis after nerve damage
Estimate the age of a nerve lesion
Diagnose sub-clinical myopathies
Localize neurological injury
Motor neurons in the brain or spinal cord: e.g., ALS, poliomyelitis
Nerve root: e.g., herniated disk
Peripheral nerves: e.g., carpal tunnel syndrome, Guillain-Barré syndrome, other polyneuropathies
Neuromuscular junction: e.g., myasthenia gravis, Lambert-Eaton myasthenic syndrome, botulism
Muscle: e.g., inflammatory myopathies, myotonic syndromes, muscular dystrophies
Procedure:
Needle electrodes are inserted into a muscle.
The electrical activity of the muscle is measured during rest (tonic activity) and during movements (phasic muscle activity).
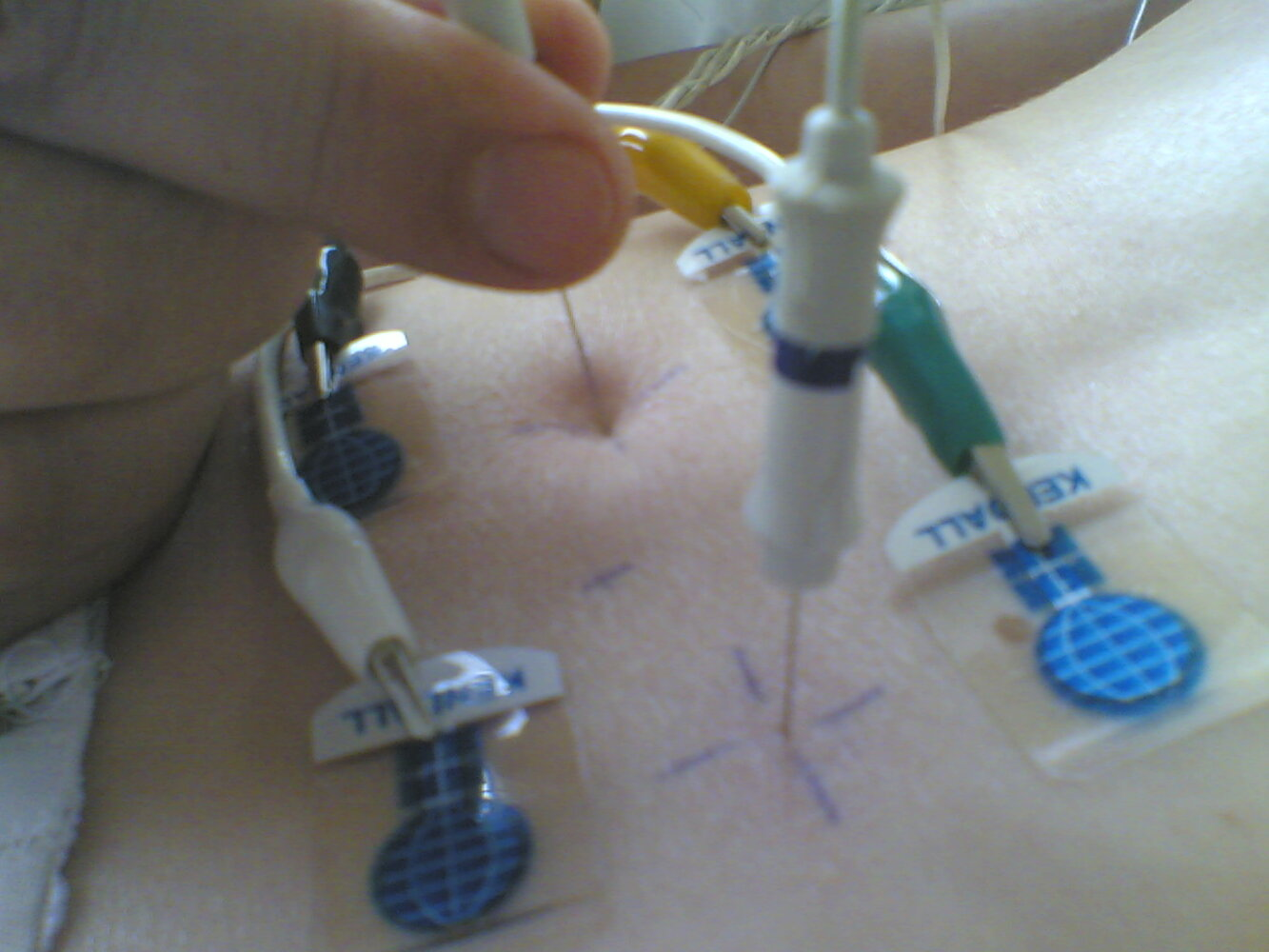 Description: Needle (intramuscular) electromyography (EMG)
Description: Needle (intramuscular) electromyography (EMG)Two needle electrodes have been inserted directly into the paravertebral muscles to record their electrical activity. Adjacent to these, four surface electrodes have been attached to the skin to act as reference electrodes.
Interpretation
EMG findings of neuropathy vs. myopathy | ||
|---|---|---|
Findings | Neuropathy | Myopathy |
Electrical activity at rest | Increased activity with needle insertion and pathological spontaneous discharge with fibrillations and fasciculations | Little or no spontaneous electrical activity |
Motor unit potential (nota 1) | Large-amplitude, polyphasic, and prolonged motor unit potential | Low-amplitude, polyphasic, and shortened motor unit potentials |
Interference pattern (nota 2) | Reduced interference pattern: muscle discharges have a low frequency but a large amplitude (nota 3) | Full interference pattern: muscle discharges have a high frequency but a small amplitude |
Nota 1) una unidad motora hace referencia a un grupo de células inervadas por la misma neurona.
Nota 2)Un patrón de interferencia es el patrón de actividad eléctrica que se observa durante una contracción fuerte cuando varias unidades motoras se activan simultáneamente.
Nota 3) Las neuropatías provocan una reorganización de las unidades motoras. Cuando una neurona concreta resulta dañada por una enfermedad neuropática, la unidad motora correspondiente recibe inervación de las neuronas vecinas. Este cambio disminuye el número de unidades motoras pero aumenta el área inervada por cada neurona. Como resultado, se observan menos descargas eléctricas pero más grandes durante la contracción muscular voluntaria.