Cardiovascular Physiology - MSU PSL 310
Overview
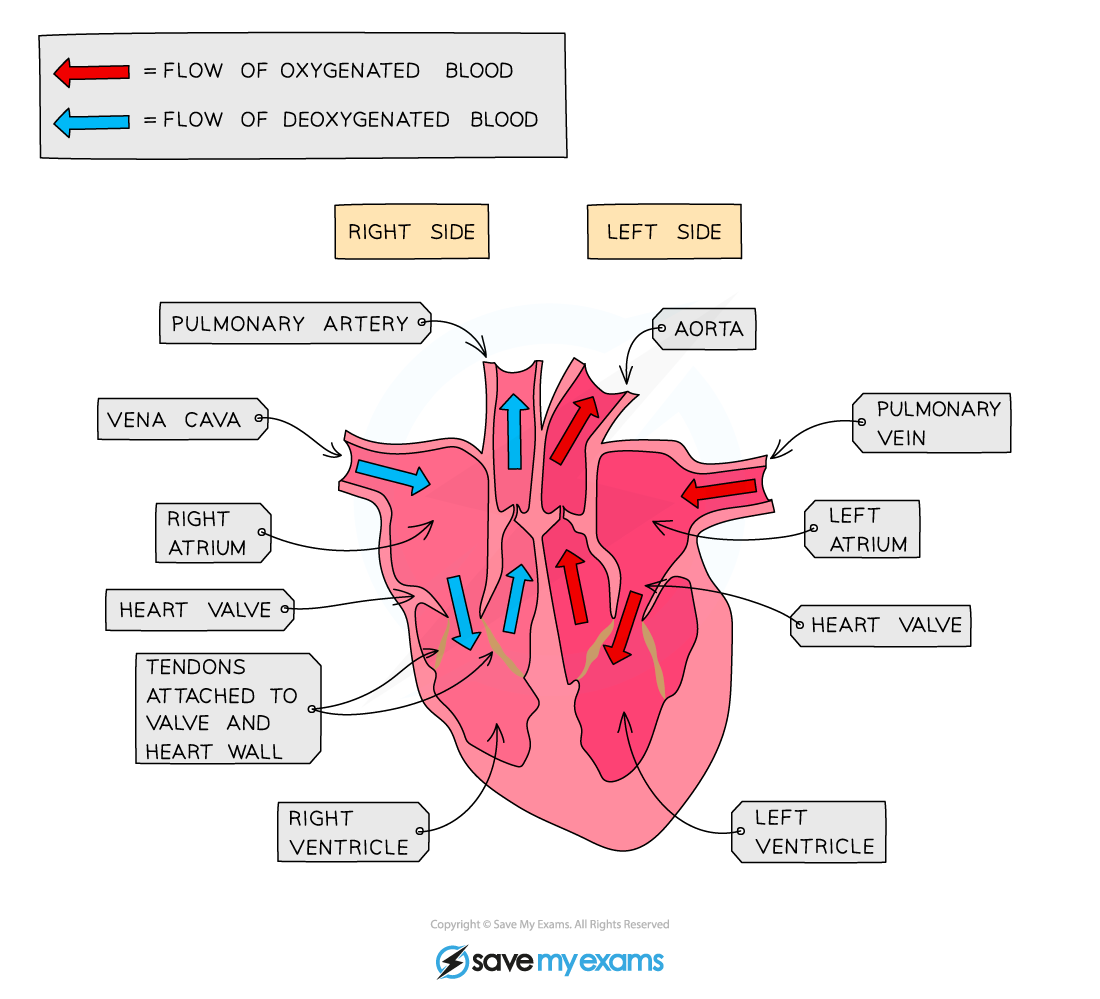
The heart has 2 separate pumps
Left pump
pumps oxygenated blood to the body (systemic circuit)
consists of the left atrium, bicuspid valve, left ventricle and left atrium
pathway of left pump:
pulmonary veins → left atrium → bicuspid (left AV or mitral) valve → left ventricle → aortic semilunar valve → aortic trunk (right and left carotid artery & left and right subclabical artery) → body
Systemic circuit
Arteries carry oxygenated blood
Veins carry deoxygenated blood
Right pump
pumps deoxygenated blood into the lungs (pulmonary circuit)
consist of the right atrium, tricuspid valve, right ventricle and right atrium
pathway of left pump:
superior & inferior vena cava → right atrium → tricuspid (right AV) valve → right ventricle → pulmonary semilunar valve → pulmonary trunk → pulmonary artery → lungs
Pulmonary circuit
Arteries carry deoxygenated blood
Veins carry oxygenated blood
Diagrams
Right and left pathways
Exterior anatomy
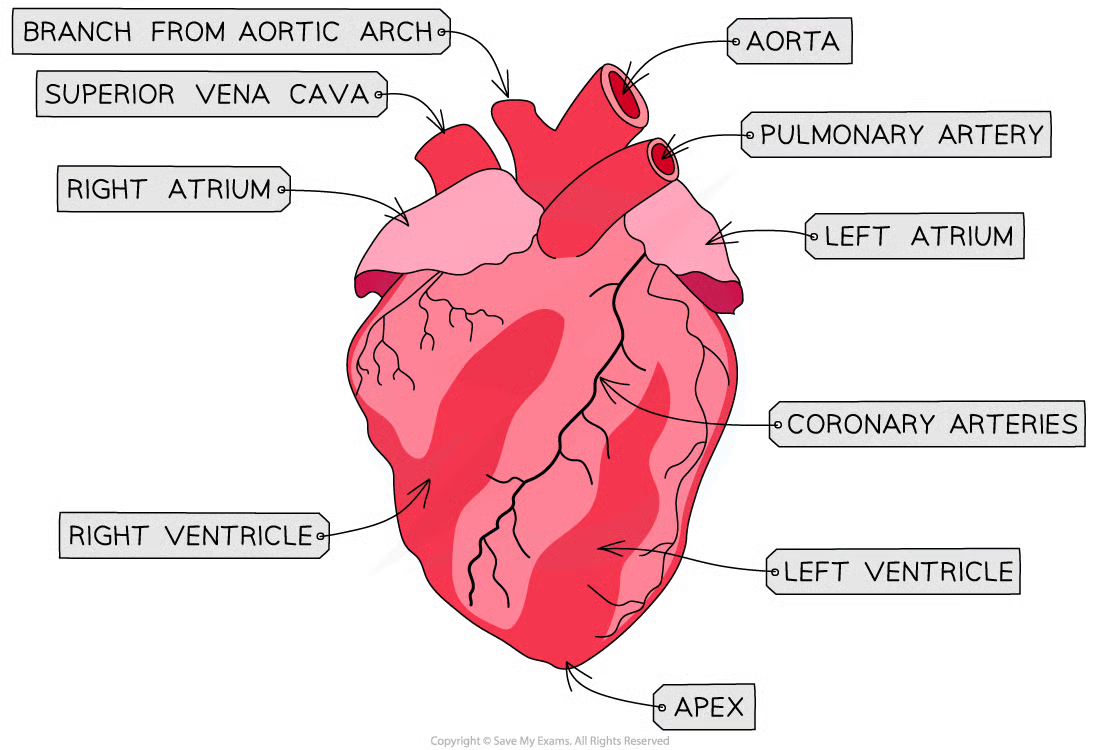
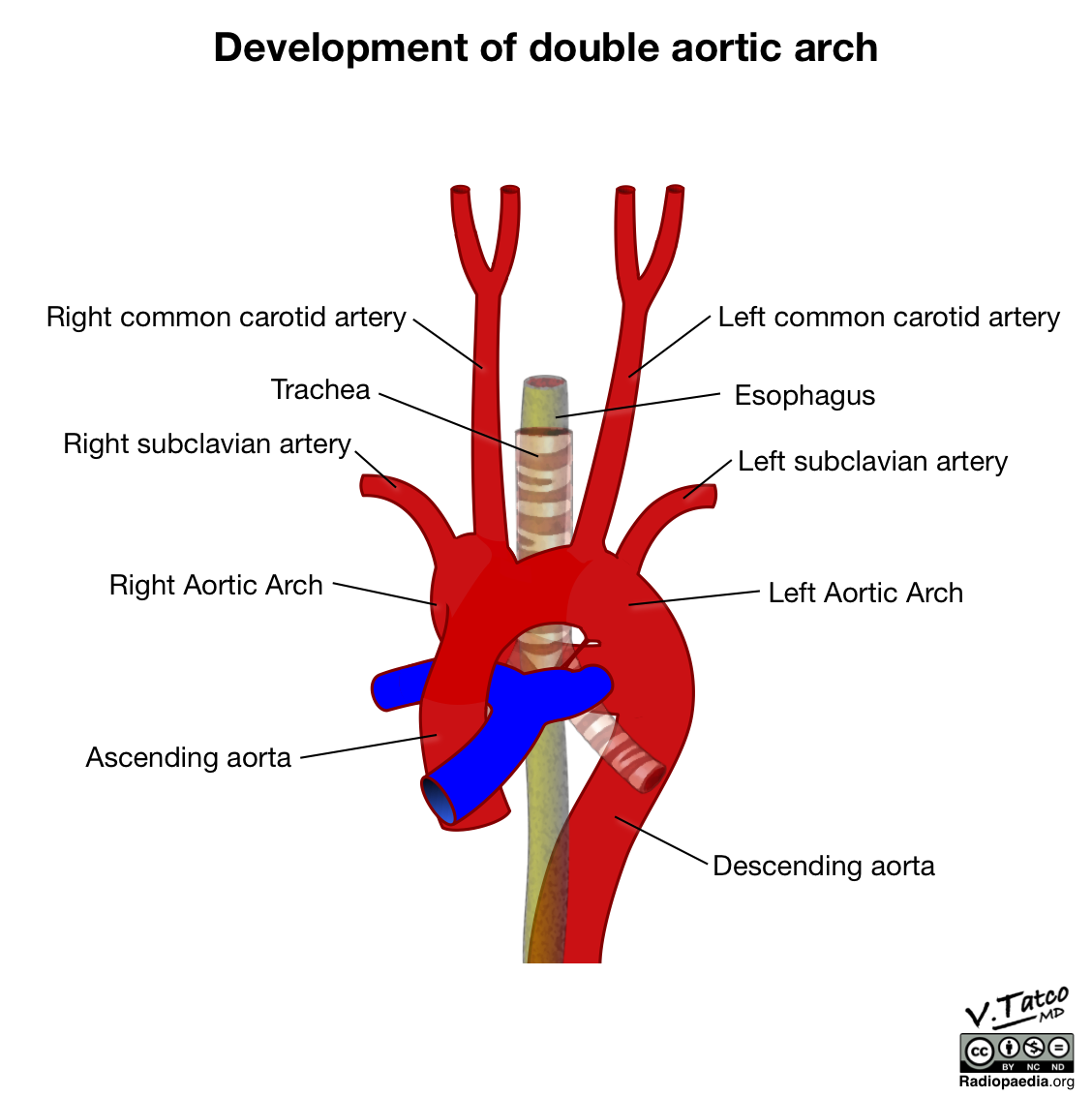
5 vessels that emerge from the aorta
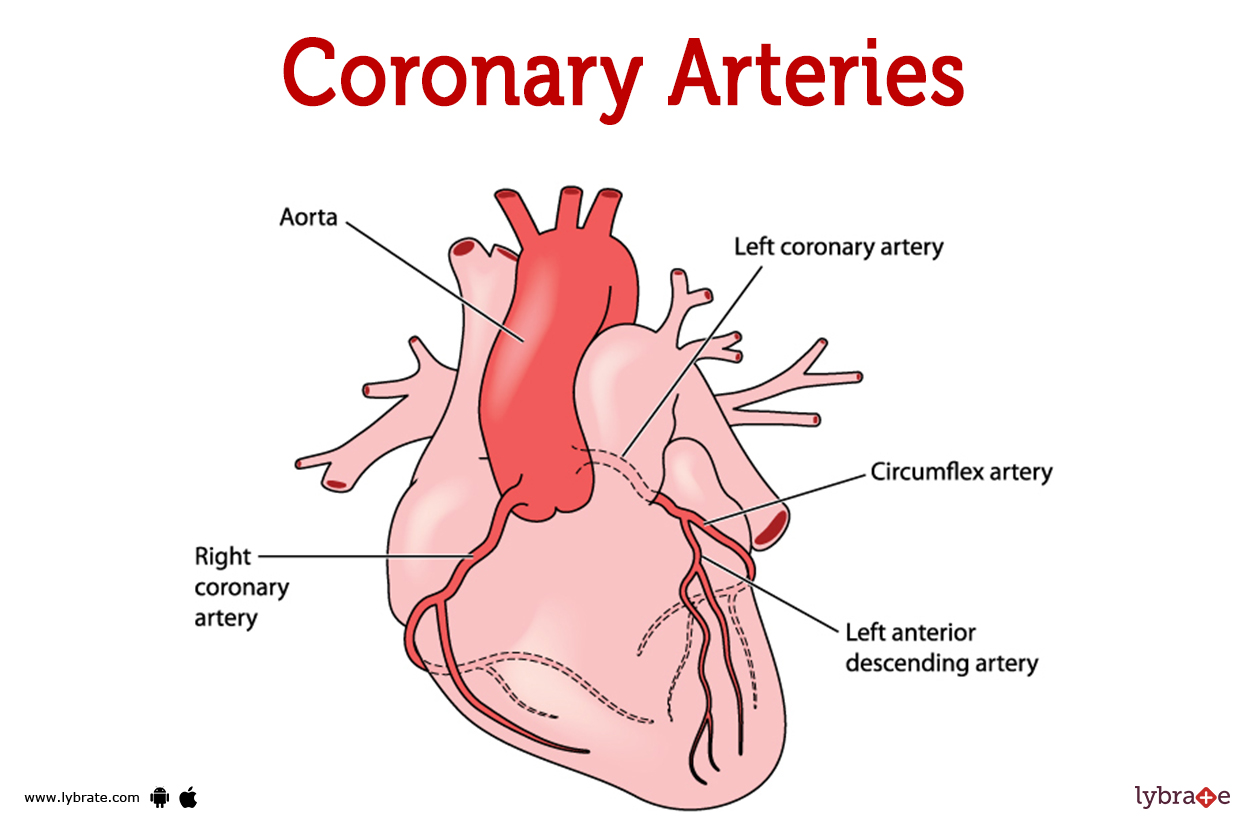
Coronary circulation
Left coronary artery → supply blood to the left side of the heart
Right coronary artery → supply blood to the right side of the heart
Left anterior decreasing (LAD) coronary artery → located in interventicular sulcus
supplies blood to the front side of the heart
Also referred to as “widow maker”
LAD supplies the heart with fresh blood,
if blocked it can lead to…
ischema → low O2
infart → cell death
Coronary Artery disease (CAD)
Atherosclerosis
arterial wall disease characterized by the development of an atheroma (or plaque) leading to arterial narrowing and impaired blood flow (perfusion)
atheroma → abnormal accumulation of macrophages, lipid, Ca2+, smooth muscle cell, and connective tissue in the tunica intima
LDL → cholesterol carrier
carries cholesterol to cell, too much is bad bc it carries cholesterol to parts we do not want (i.e. cell wall of veins/arteries)
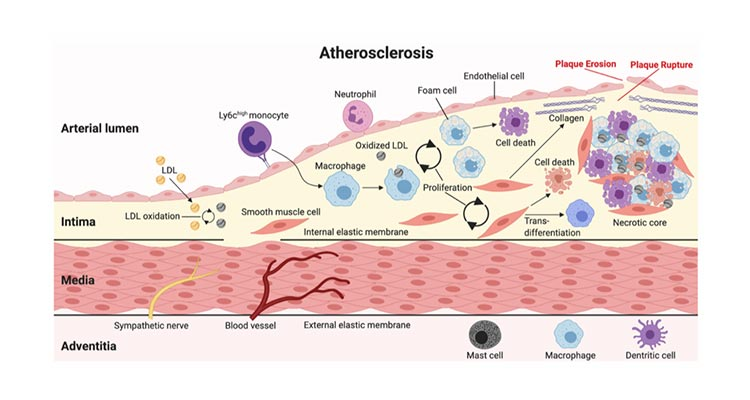
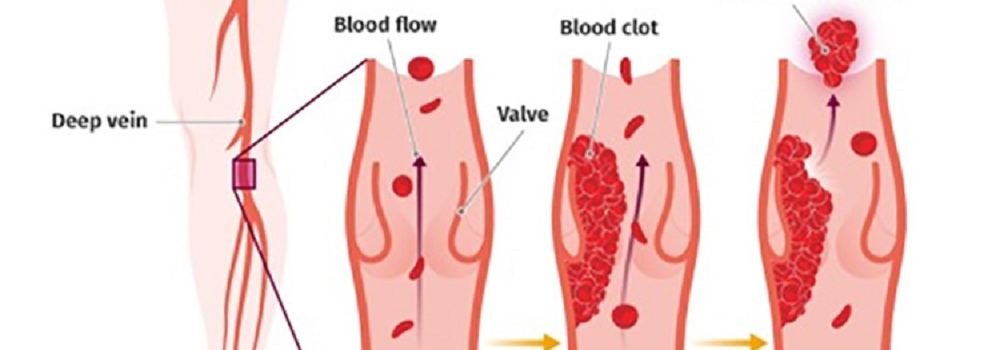
Thromboembolism
late stage atheromas can rupture and promote the formation of a thrombus (or blood clot) which exacerbates arterial narrowing, impaired perfusion and inschemia
embolus - free-floating thrombus broken loose from a vessel wall which can lodge in, and occlude, downstream, smaller vessels
major be the cause of…
(ischemic) stroke
potential cause of…
myocardial ischemia (cerebral infart)
myocardial infarction (heart attack)
CAD treatments
lifestyle changes → exercise, stress-reduction, and healthy eating
treatments →
thrombolytics
cloth busters
anticoagulants
aspirin (antiplaquet)
blood thinNers (NOACS/DOACS)
cholesterol medications
statins
negative inotropes
beta blockers
vasodialators (angina → chest pain)
nitroglycerine
PCSK9 inhibitors
erocumab
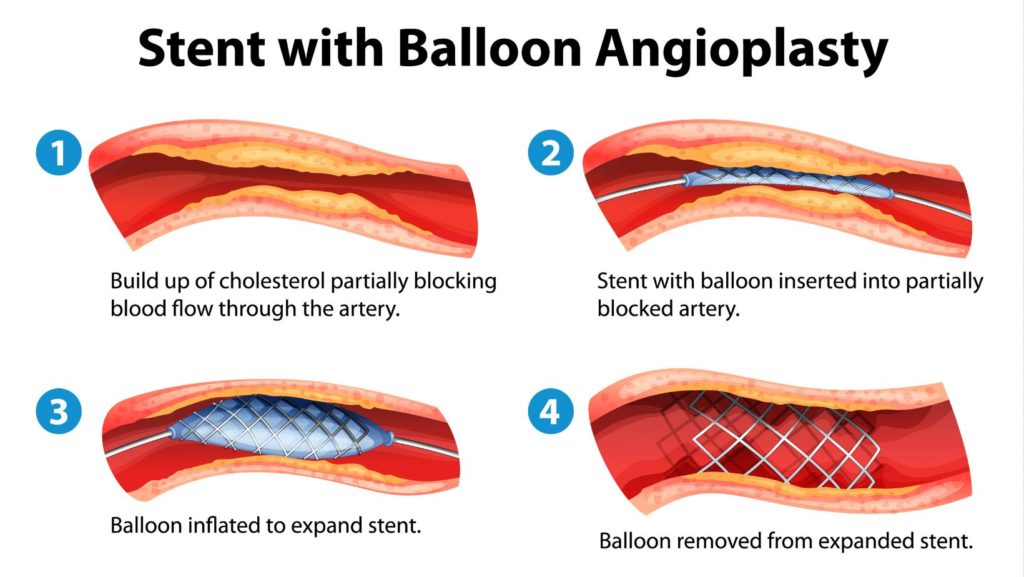
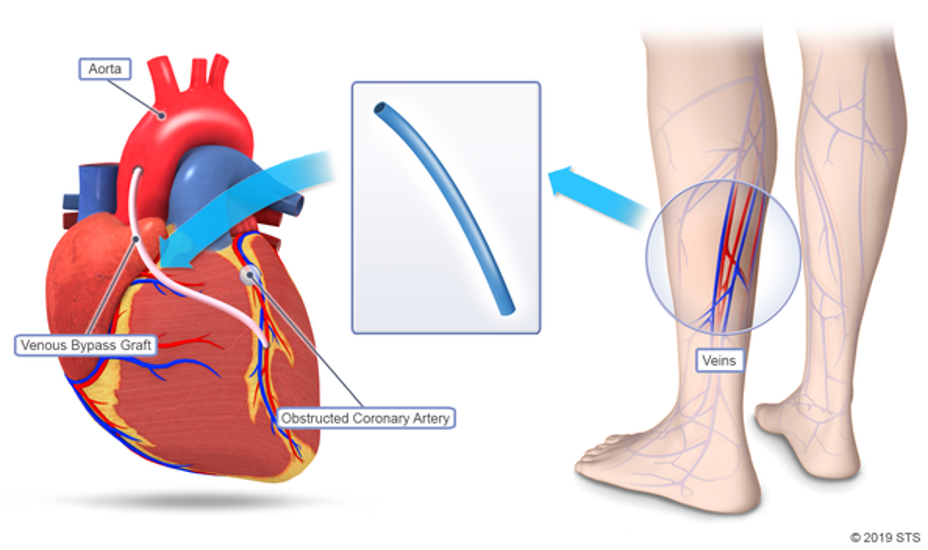
Corrective Procedures
ballon angioplasty
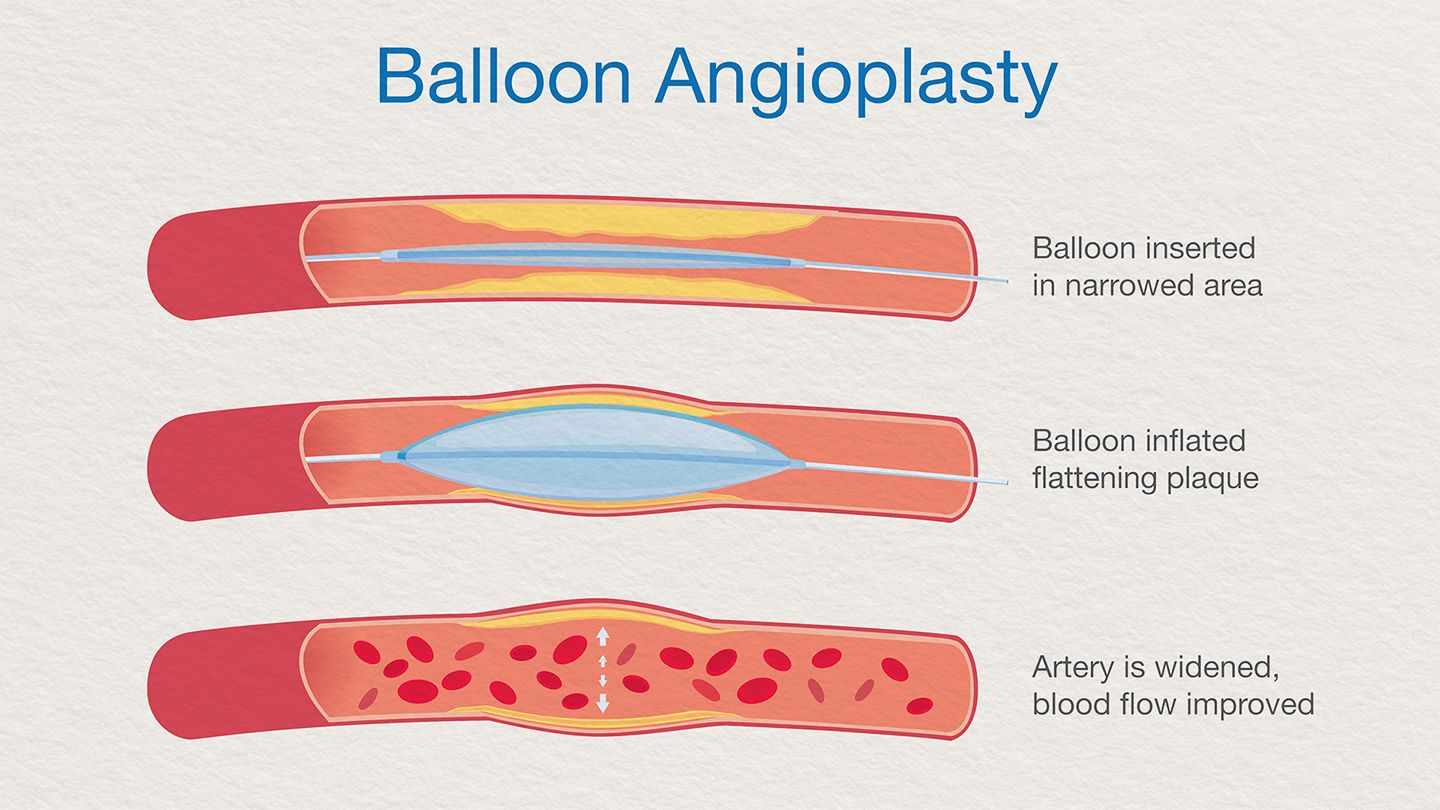
coronary stenting
coronary by-pass
take segment of vein in leg and stitch it to the heart
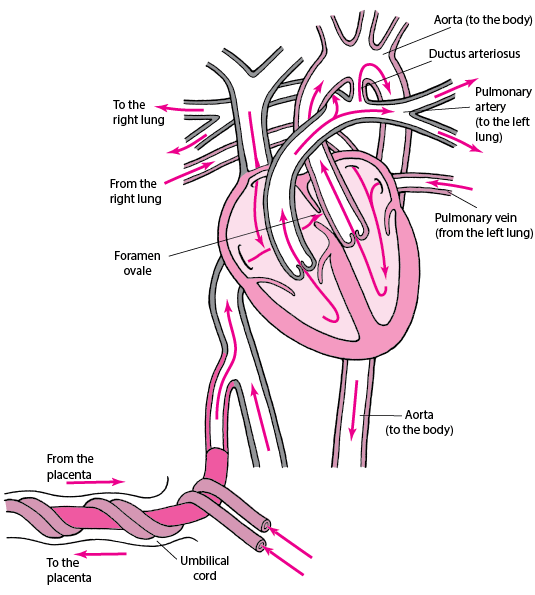
Fetal Circulation
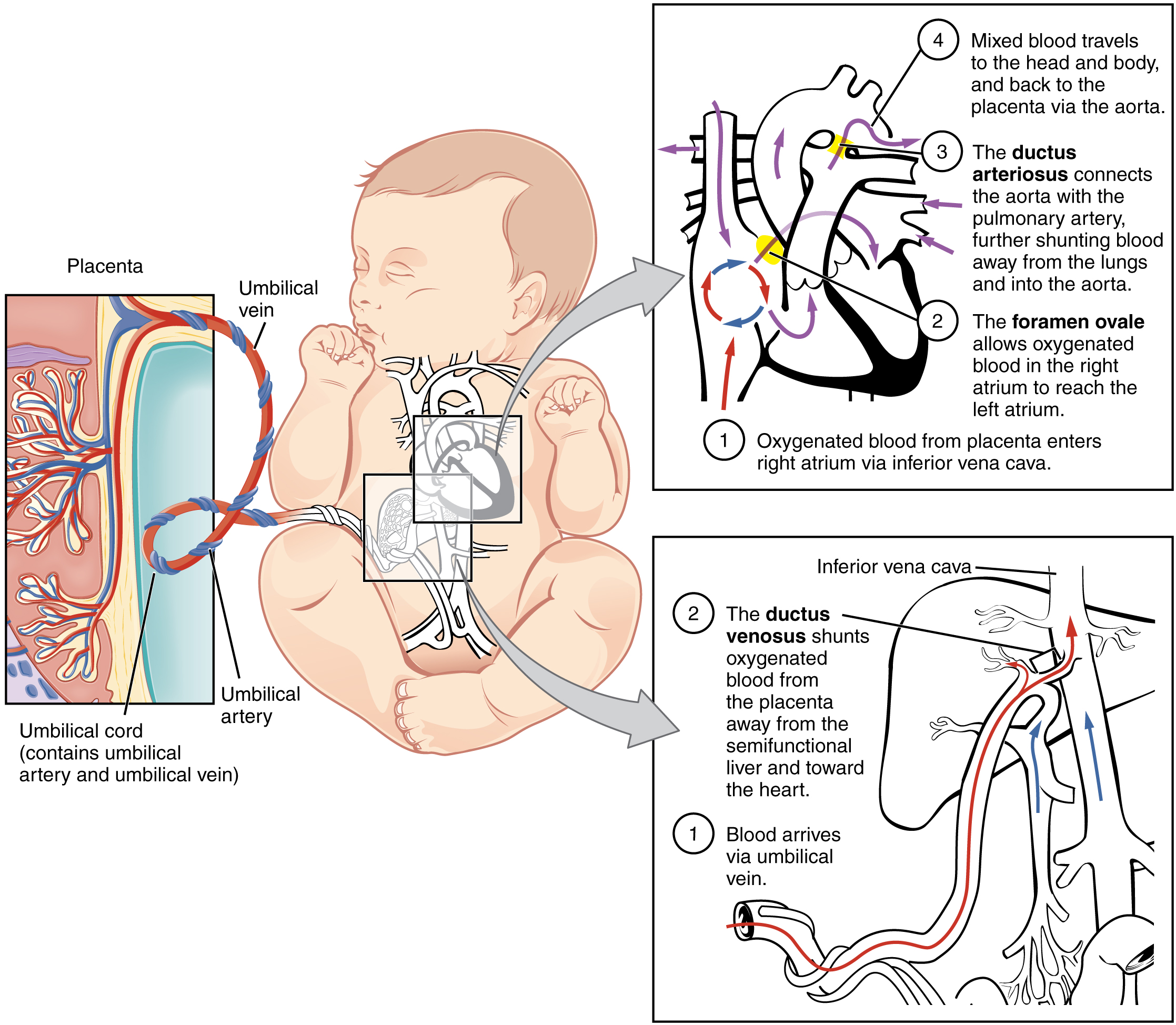
Special feature
Foramen Ovale → this hole closes and turns into the Fossa ovalis
Ductus arteriosus → closes and becomes ligamentum arteriosum
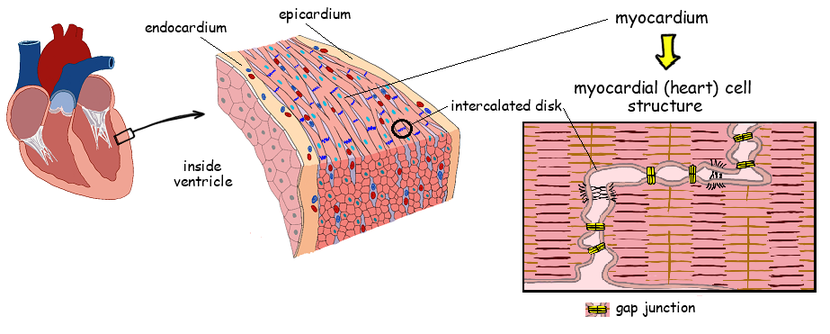
3 layers of the heart
Dense fibrous layer
Parietal pericardium
lose connective tissue
epithelium
Pericardial cavity
Epicardium
lose connective tissue
epithelium
Myocardium
thicker on the left ventricle than the right as it need to pump blood to the entire body thus needs to generate a great ammount of energy.
the right pump only pumps blood 6inches away to the lungs
Endocardium
lose connective tissue
endothelium
Cardiac Conduction system
Heart cells (2 types) →
contractile cells (99%)
authotithmic cells (1%)
subendocardial network of specialized authotithmic cardiomyocites cappable of generating and conducting APs
cardiac vs skeletal muscle
cardiac muscle cells only have one or two nuclei while muscle cells are multinucleate.
cardiac cells are involuntary controlled while skeletal are voluntarily controlled.
cardiac are interconeccted by gap junction while skeletal are long and fused
in cardiac cell DHPR (voltage-gatted Ca2+ channel) is used for depolarization while in cardiac its L-type Ca2+ channel
Cardiac Conduction Anatomy
![]()
![]()
Sinoatral node (SA node)
its a small body of specialized muscle tissue that acts as as pacemaker by spontaneously producing a contractile signals (prepotential signals) that establishes heart beat
located in the upper wall of the right atrium
AP frequency → 70mph
Internodal pathway (fibers)
cardiac conductive cells that emanate from the SA node and innervate the atrial myocardium and terminate at the atrioventricular (AV) node.
they conduct the prepotential signal from the SA node to the myocardial cells of the atria and the AV node
located in right atrium
Atrioventricular (AV) node
Electrically connects the right atrium and ventricle, it generated and conduces APs, also delays SA signal.
delays the SA signal for about ~100ms
located in the floor of the right atrium
AP frequency → 50mph
Purkinje fibers
in charge to send the contraction signal to the the ventricular myocardium
AP frequency → 30mph
Intercalated discs
regions in cardiac tissue which contain a high density of gap junctions
Function syncytium
cardiomiocytes are interconnected by gap junctions, once a AP signal is sent it travels through the gap junctions spreading through the cells making them contract in unison
Cardiac Conduction signal process
Step by step
SA is depolarized and produces the AP signal
AP signal travels through the intermodal fivers to the AV node
AV node delays the signal (~100ms)
signal travels through the bundle of His
the bundle of his splits into the right and left branches of His
the signal travels through the branches
the signal is directed through the moderator band which stimulates the papillary muscle in the ventricles and then propagated up the Purkinje fibers
What if there is a derailment?
if one cell derails the next one with the highest rate of prepotentials takes over '
(condition): derails → takes over
Sick Sinus Syndrome: SA node (70mph) → AV node (50mph)
low heartbeat
can live but in some casses migh require the need of a pacemaker
Complete Heart Block: AV node (50mph) → Purkinje fibers (30mph)
Due to AV node being derrailed the SA derrails as well making the Purkinje fibers be the peacemakes.
may cause the person to faint with injury, low blood pressure, and damage to other internal organs, and cardiac arrest
treatment → pacemaker
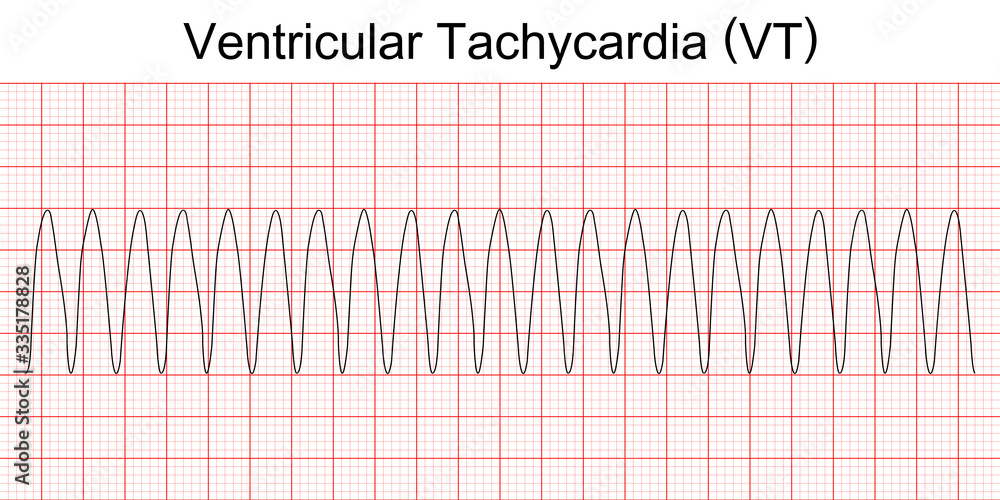
Ventricular Tachycardia: non-cardiac cells send signals to the Purkinje fibers making them rapidly fire signals
heart beats too fast to pump well and the body doesn't receive enough oxygenated blood
may lead to fainting
can be caused by things such as caffeine (stimulants)
Autorythmic ( cardiomyocites
Slow cell AP (SA & AV nodes)
the pacemaker cells (SA & AV nodes) are auto-rhythmic (self-exitatory)
in other words they can spontaneously generate APs (in this case they are referred as pre-potentials) without innervation
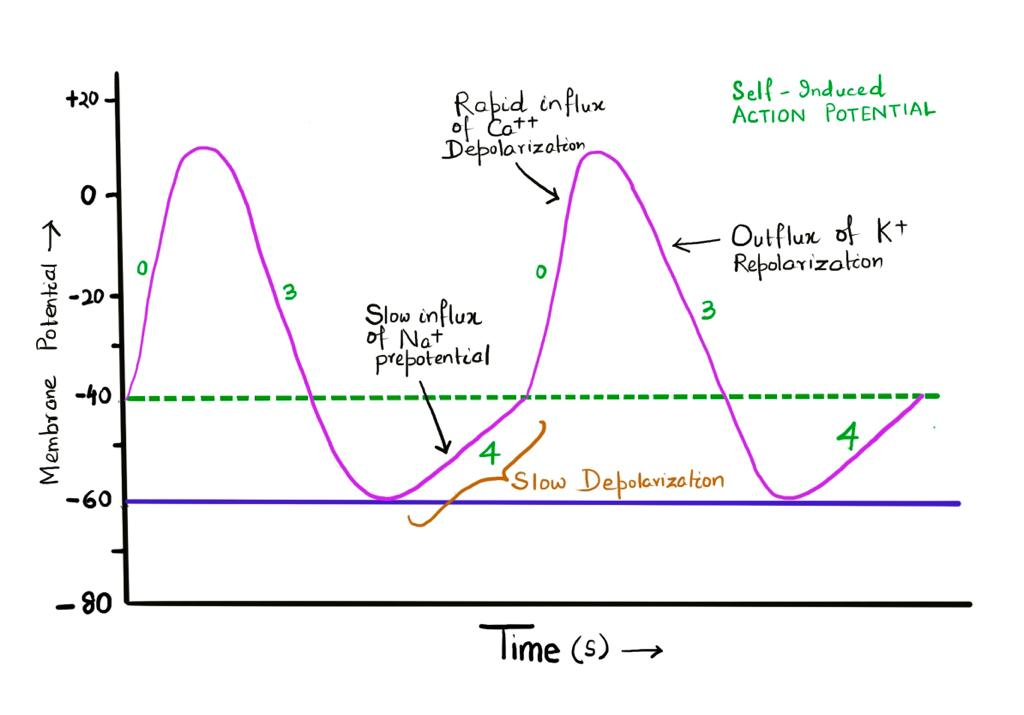
Resting membrane potential (RMP)→ -60mV
Threshold Potential (TP) → -40mV
Phase 0 → depolarization phase
beguins after threshold potential is reached
At around -40 mV, L-type (iCa+,(L)) calcium channels open up and allow the steady flow of calcium into the cell
this influx of calcium depolarizes the cell
Phase 3 → repolarization phase
at +30 mV voltage-gated potassium channels (iK1) open creating a outflow of K+ from the cell through them
potassium current
At some point during the end of the phase, when the depolarization reaches -40mV iK1 close and the funny channels open
Phase 4 → pre-potential phase
funny channels open allowing Na+ in making the cell repolarize back to RMP and subsequently TP to go into phase 0 again
Contractile cardiomyocites
Fast cell AP (Ventricular Cardiomyocyte)
any other cardiac cell that is not the AV or the SA
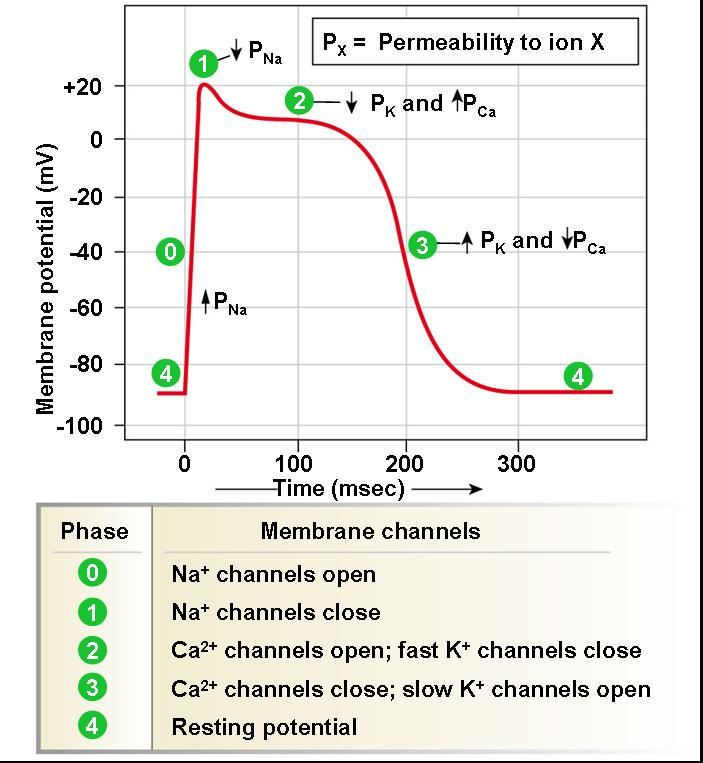
Resting membrane potential (RMP)→ -90mV
Threshold Potential (TP) → -70mV
Phase 0
constant leaking of K+ from iK channels maintains the cell at RMP
makes it be at equillibrium potential with K+
the depolarization of an adjacent cells make voltage-gated sodium channels (iNa+) open allowing Na+ to go into the cell
the cell depolarizes FAST as Na+ comes in
Phase 1
at +30 mV voltage-gated potassium channels (iK) making potassim leak out the cell
Slightly depolarizes the cell
Phase 2
at -55mV iCa+,(L) channels open, allowing Ca+ in
this influx of Ca+ balancess the Na+ with the K+ leaking out
influx → Ca+
efflux → K+
this creates the plateau
Phase 3
eventually the first iK+ channels close and other iK+ channels open allowing K+ to fully leave the cell making it repolarize
Excitation-contraction coupling
Cardiac vs skeletal
In cardiac muscle the contraction is triggered by electrical
signals from neighboring cells. The ANS modulates the response.
Excitation-contraction coupling is mediated by a phenomenon referred to
as calcium-induced calcium release
What is calcium-induced calcium release?
Calcium-induced calcium release is when calcium is able to
enter the sarcoplasm via DHPR to bind to and activate RyR and cause
calcium release into the sarcoplasm.
what are funny channels?
The funny channels are activated by repolarization and cAMP.
Sympathetic innervation increases cAMP, which binds to funny channels and increases the probability that they are open.
Parasympathetic innervation decreases cAMP, which is now unbound to funny channels and therefore decreases the probability that they are open.
Atrial and Ventricular Cardiomyocytes
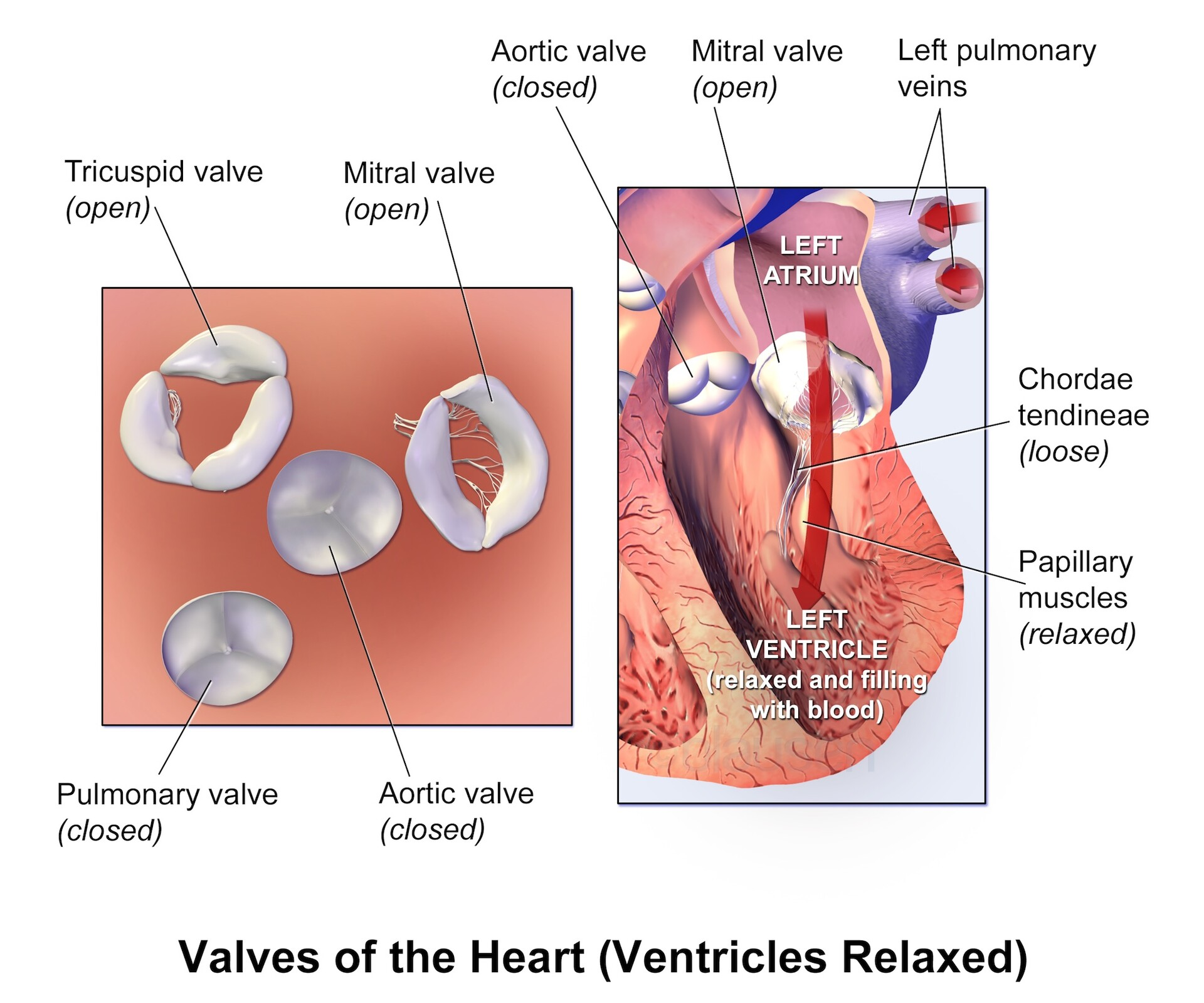
Semilunar valves
Semilunar valves are inherently one-way valves meaning they
only open in one direction, without the assistance of papillary muscles and
chordae tendineae.
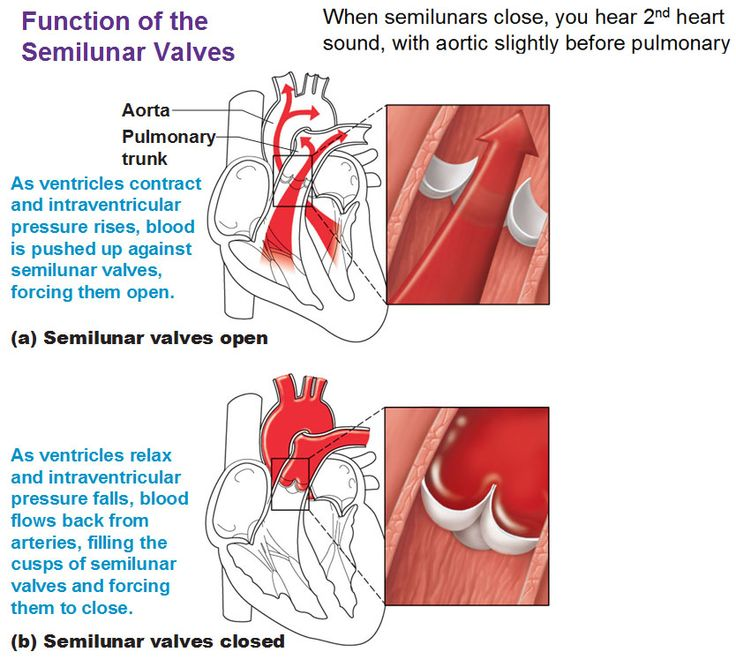
Atrioventricular (AV) velves
AV valves are not inherently one-way valves because they
require papillary muscles and chordae tendineae to function properly.Wow do they work together?
Papillary muscles contract prior to the ventricles contracting to
reduce the travel of the AV valves so that they properly shut. The papillary muscles are attached to chordae tendineae, which are also attached to the flaps of the AV valves.when the ventricles are relaxed the AV valves are open allowing blood to pool into the ventricle
passive ventricular fill
What if the chordae tendineae were severed?
If chordae tendineae were severed the AV valve would prolapse
and potentially lead to atrial regurgitation.
Top hat Q: papillary muscless contract to…
…prevent the AV valves from opening into the atria
Mitrial (bicuspid) valve
Cardiac Electrophysiology
The Electrocardiogram (ECG)
what is it?
body surface recodring of the heart’s electrical events occurring within the heart
correlated with the mechanical events of the heart
ECG waveform
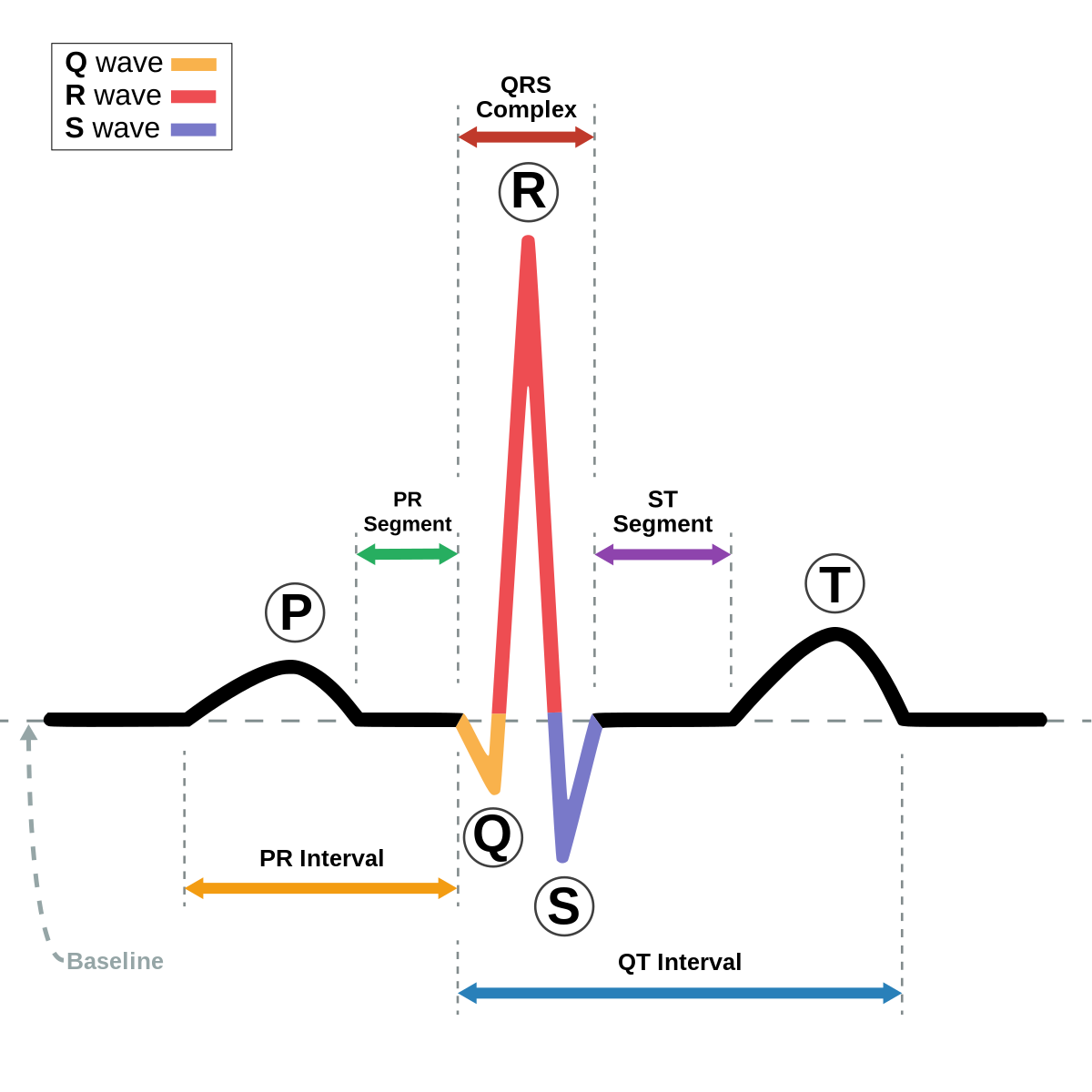
Components
P-wave → atrial depolarization
PR segment → atrial contraction (systole)
AV node delay
QRS complex → simultaneous atrial repolarization and ventricular depolarization
ST segment → ventricular contraction (systole)
time during which ventricles are contracting and emptying
T-wave → ventricular repolarization
TP interval → time during which ventricles undergo passive ventricular fill
RR interval → heart rate
Cardiac Arrythmias
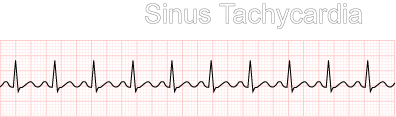
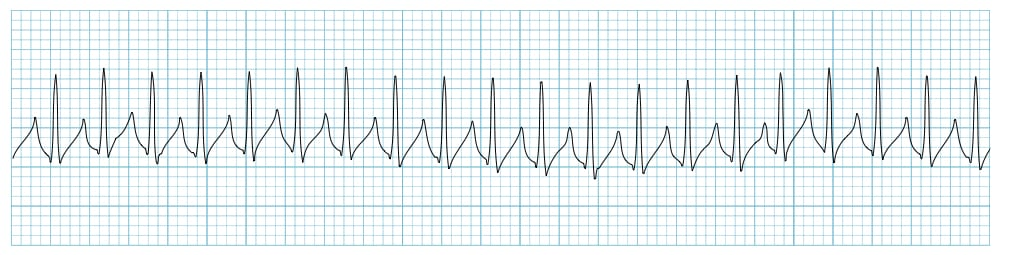
Tachycardia
A heart rate of more than 100 hpm
During tachycardia, the RR interval decreases in length
Sinus Tachycardia
Ventricular Tachycardia (VT, Vtach
Supraventricular Tachycardia
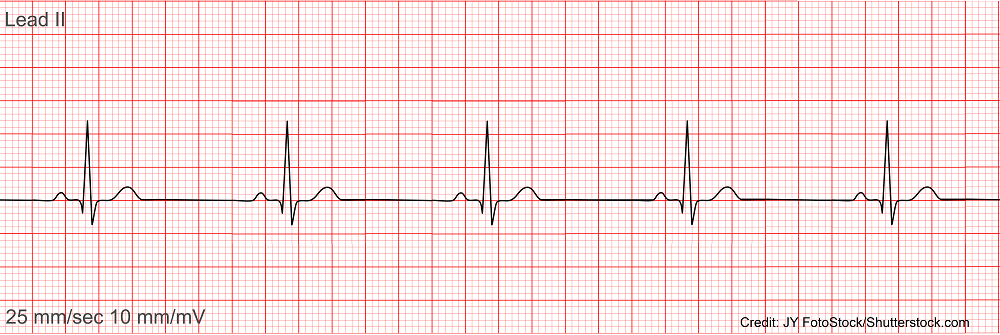
Bradycardia
a heart rate that is equal or less than 60 hpm
During bradycardia, the RR interval increases in length
Can someone be clinically bradycardic and still considered to have a normal heart rate?
Yes, you can be clinically bradycardic and be considered to have
a normal heart rate. A slow heart rate does not cause any problems.Bradycardia can be a sign of being very fit.
Healthy young adults and athletes often have heart rates of less than 60 beats per minute.
Sinus Bradycardia
Premature Contraction
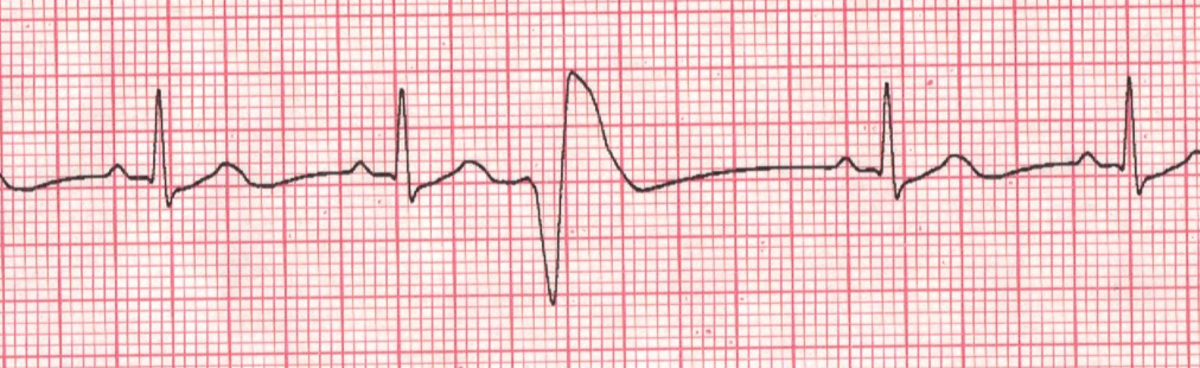
Premature Ventricular Contraction (PVC)
During a PVC, the ventricles contract before the ST segment, making the QRS complex abnormal.
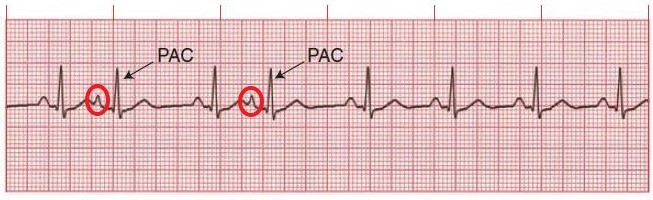
Premature Atrial Contraction (PAC)
During a PAC, the TP segment is shorter because the P wave is occurring prematurely.
Fibrillation
ventricular fibrillation
During ventricular fibrillation, the QRS complex decreases in size
and the signal is noisy.
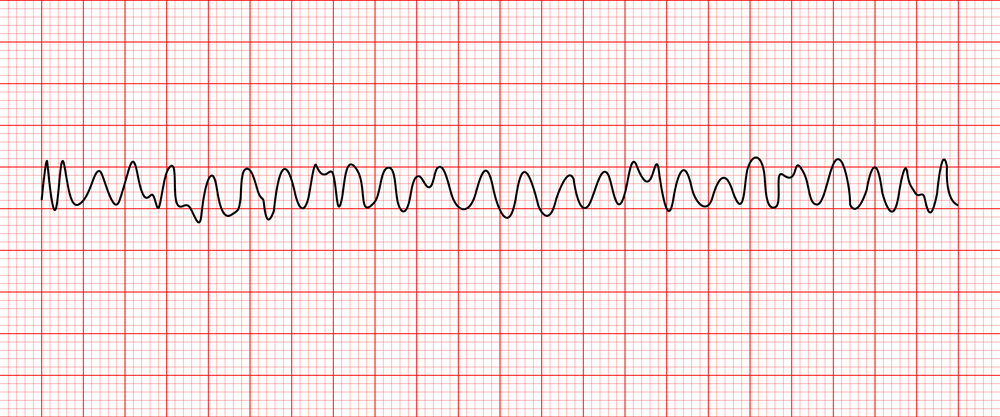
atrial fibrillation
During atrial fibrillation, the P waves in the ECG are absent and the signal is noisy

Complete Heart Block
In complete heart block, QRS complexes may be missing and
the signal is conducting slowly due to a blockage
![]()
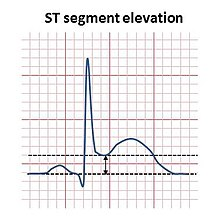
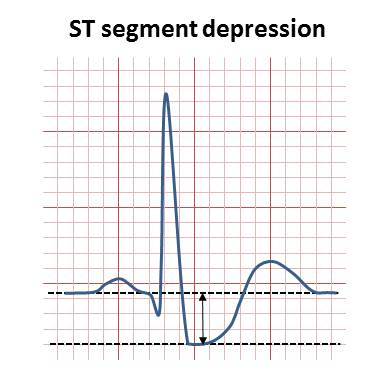
ST segment
ST segment elevation
An ST segment elevation is transmural, or full thickness, ischemia and indicative of a myocardial infarction
ST segment depression
An ST segment depression results from subendothelial partial thickness ischemia
indicative of coronary artery disease
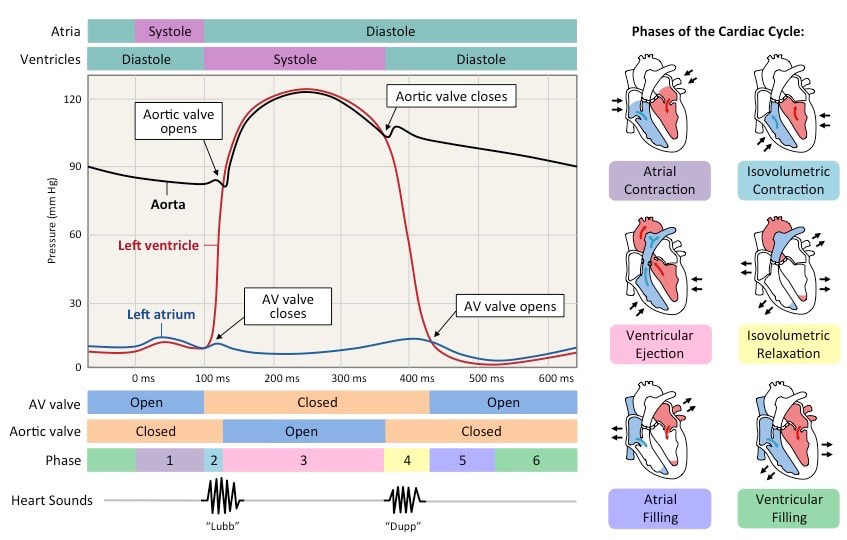
Cardiac Cycle
period of mechanical events of the heart between the start of one heartbeat and the start of the next
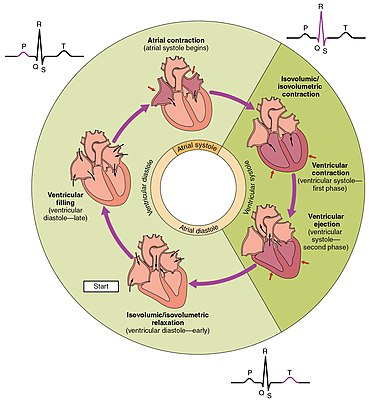
Phases:
Systole → contraction phase
Diastole → relaxation phase
Does the heart spend more time during systole or diastole?
The heart spends more time in diastole (specifically, the heart
spends 2/3 of the cardiac cycle in diastole)
Events:
atrial systole → atrial contraction
atria contracts and and fill the relaxed ventricles with an additiona ammount of blood
they are already 75% filled with blood
atrial diastole → atrial relaxation
ventricular systole →
early → isovolumetric ventricular contraction
the ventricles contract isovolumetrically or in other words while they are contracting the, pressure within the ventricle is not great enough to open the semilunar valve
this contractions push the AV valves close
AV → closed
Semilunar → closed
late → rapid ejection
pressure keeps rising untill it is creater than the pressure in the arteries, opening the semiluner valves and rapidly ejecting blood
AV → closed
Semilunar → open
ventricular diastole
early → isovolumetric ventricular relaxation
pressure in ventricle drops; blood passively flow into the atria and against the cusps of semilunar valves forcing them shut
AV → closed
Semilunar → closed
late → passive ventricular filling
all chambers of the heart are relaxed allowing blood to passibly fill the ventricles
this is where the 75% already full comes from
AV → open
Semilunar → closed
Mechanical (M) & electrical (E) events of the heart
Start
E: pre-P-wave → SA node depolarization
E: P-wave → atrial depolarixation/AV nde depolarization
PR segment →
M: atrial systole
E: AVN delay (100ms)
E: His/Purkinje depolarization
QRS complex→
E: atrial repolarization
M: Atrial diastole
E: ventricular depolarization
M: ST-segment → early ventricular systole (IVC)
ST-segment →
M: late ventricular systole (rapid ejection)
T-wave →
E: ventricular repolarization
M: TP-interval → early ventricular diastole (IVR)
TP-interval →
E: no activity
M: late ventricular diastole (passive ventricular filling)
Wiggers diagram
shows the pressure changes within the heart during the cardiac circle
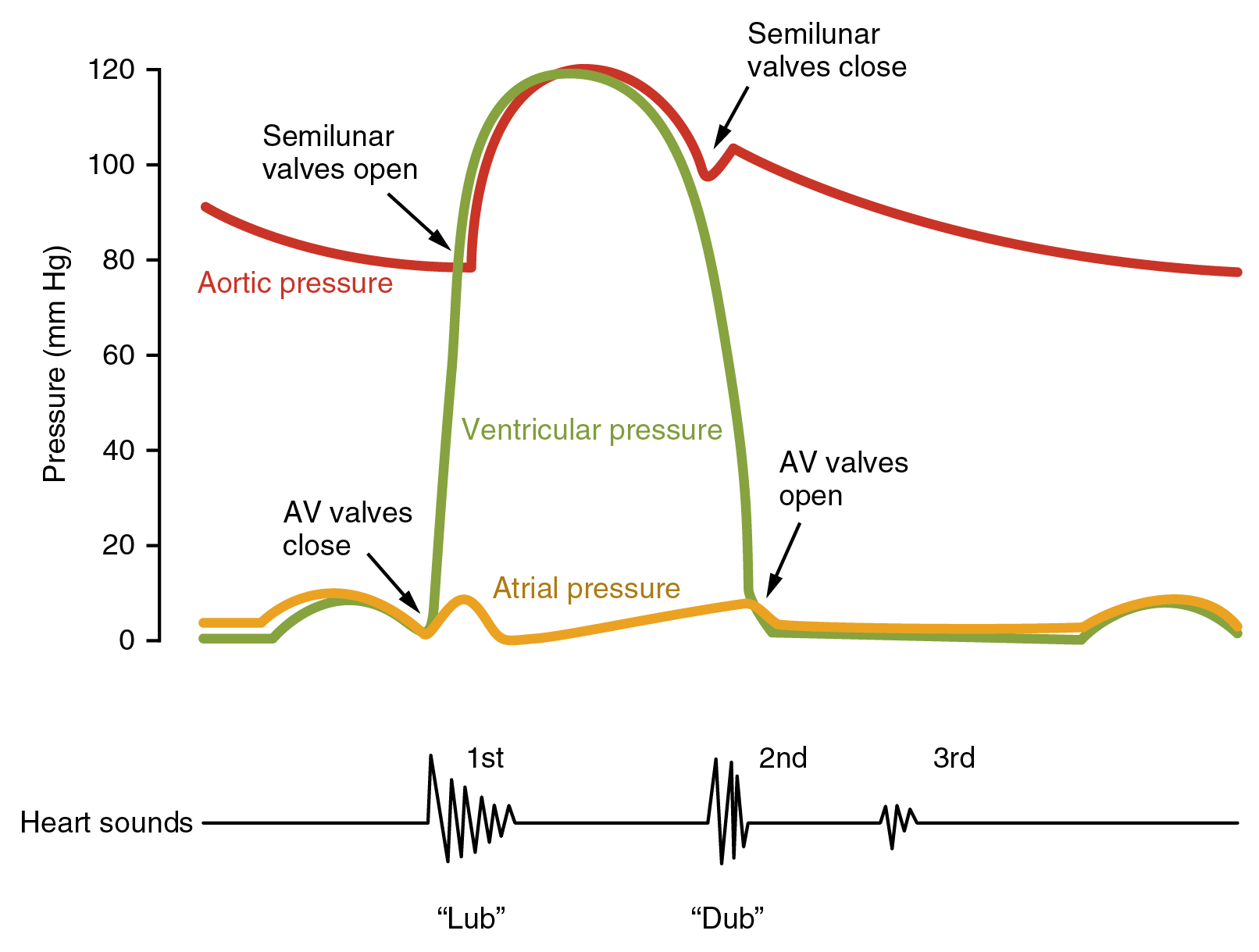
How does this diagram differ between the left and right sides?
in the right ventricle there is not that much pressure generated, since blood is pumped to the lungs so the pressure loop is shorted than that of the left ventricle which pumps blood to the entire body.
Sounds of the heart
“lubb” → closure of AV valves
occurs at 3
“dubb” → closure of semilunar valves
occurs at 6
Cardiac Hemodynamics
Cardiac Hemodynamic Parameters
Cardiac output (CO)
the volume of blood pumped by each ventricle of the heart per minute
the heart pumps 5L of blood to the body per minute
can increase during exercise to 20-40 L/min
ANS (autonomic nervous system) control of CO
cardiac output = heart rate * stroke volume (CO=HR*SV)
cardiac output is dependent on HR and SV
Heart Rate (HR)
how many time a heart beats per minute (bpm)
~70 bpm
Ranges:
Normal → 60-100 bpm
Bradycardia → <60bpm
Tachicardia → >100 bpm
Intrinsic rate → 100-110bpm
upper limit → ~220 bpm
ANS controll of HR
heart is innervated by both arms of the ANS
Sympathetic (SNS)
primary innervate the SA and AV nodes, and contractile cardiocytes
increases HR (increase chronotropy) and dromortopy
during exersise, increases HR due to an initial rapid withdrawal of PNS activity
SNS acctivity → NE → Beta 1 → increase AC → increase cCamp → increase iF (funny current) → increase phase 4 slope → increase HR
SNS activity → EPI
Parasympathetic (PNS)
The ANS modulates the heart rate by the sympathetic and parasympathetic branches. Stimulation of the sympathetic branch increases heart rate, and stimulation of the parasympathetic branch decreases heart rate
primary innervate the SA and AV nodes
at rest PNS activity dominares SNS (Vagal tone)
during exersise HR increases due to an initial and rapid withdrawal of PNS (a release of the vagal break) and subsequen increase in SNS activity
PNS acctivity → Ach → M2 → decrease AC → decrease cCamp → decrease iF → decrease phase 4 slope → decrease HR
There is a “vagal brake” on the heart. What does this mean and how does the brake work?
The SA node is innervated by the vagus nerve. It drips acetylcholine onto the pacemaker, slowing heart rate. When vagal tone to the heart’s pacemaker is high, a baseline or resting heart rate is produced.
In other words, the vagus nerve acts as a restraint, or brake, limiting heart rate
more ACth = slower HR
What is a funny channel?
The funny channels are activated by repolarization and cAMP.
Sympathetic innervation increases cAMP, which binds to funny channels and increases the probability that they are open.
Parasympathetic innervation decreases cAMP, which is now unbound to funny channels and therefore decreases the probability that they are open.
Stroke volume (SV)
volume of blood pump out of each ventricle of the heart during each beat
~70ml
can increase during exercise to 120-180ml
Contractility in how hard and fast myocardial cells are contracting.
Increases in contractility increase stroke volume.
An increase in contractility will decrease end systolic volume and increase stroke volume.
What controlls it?
SNS control of SV
extrinsic control
increase SNS → increase in β1-adrenergic activation → increase cardiac contractile force
Contractility in how hard and fast myocardial cells are contracting.
Increases in contractility increase stroke volume
intrinsic
ncrease SNS → increase cardiomiocyte relaxation rate (lustriopy) → increase venous return to beart (Frank–Starling law of the heart)
calculations
SV = EDV – ESV
end-diastolic volume (EDV) is the volume of blood in the ventricles at the end of passive ventricular filling.
This is approximately 120 mL
end-systolic volume (ESV) is the volume of blood in the ventricles at the end rapid ejection.
This is approximately 50 mL
Frank-Starling effect
The Frank–Starling law of the heart states that the stroke volume
increases in response to an increase in the volume of blood filling the
heart. Increases in preload will increase stroke volume
ejection fraction (EF)
EF is the fraction of blood ejected from a ventricle of the heart
with each heartbeat.A normal ejection fraction value is approximately 55%.
Below that indicates heart failure.
calculations
EF = SV / EDV
SV → stroke volume
EDV → end-diastolic volume
normal → 55-75%
absnormal → <40%
Heart Failure
Heart failure with a reduced ejection fraction (HFrEF) → occurs when the ejection fraction is below 40%.
The heart is too weak to pump properly
Heart failure with a preserved ejection fraction (HFpEF) → occurs when the heart is too stiff to pump properly. The ejection fraction, in this case, is normal
preload and afterload
preload
the blood return venously to the heart
How do changes in preload affect EDV, ESV, and SV?
An increase in preload will increase EDV, decrease ESV, and
increase SV.
afterload
the blood within the arteries that blood being pumped from the heart has to push against
How do changes in afterload affect EDV, ESV, and SV?
An increase in afterload will decrease SV and increase ESV
Circulation
anatomy
Veins
![]()
Veins have 3 layers, valves and are more superficial in the subcutaneous tissue.
Artery
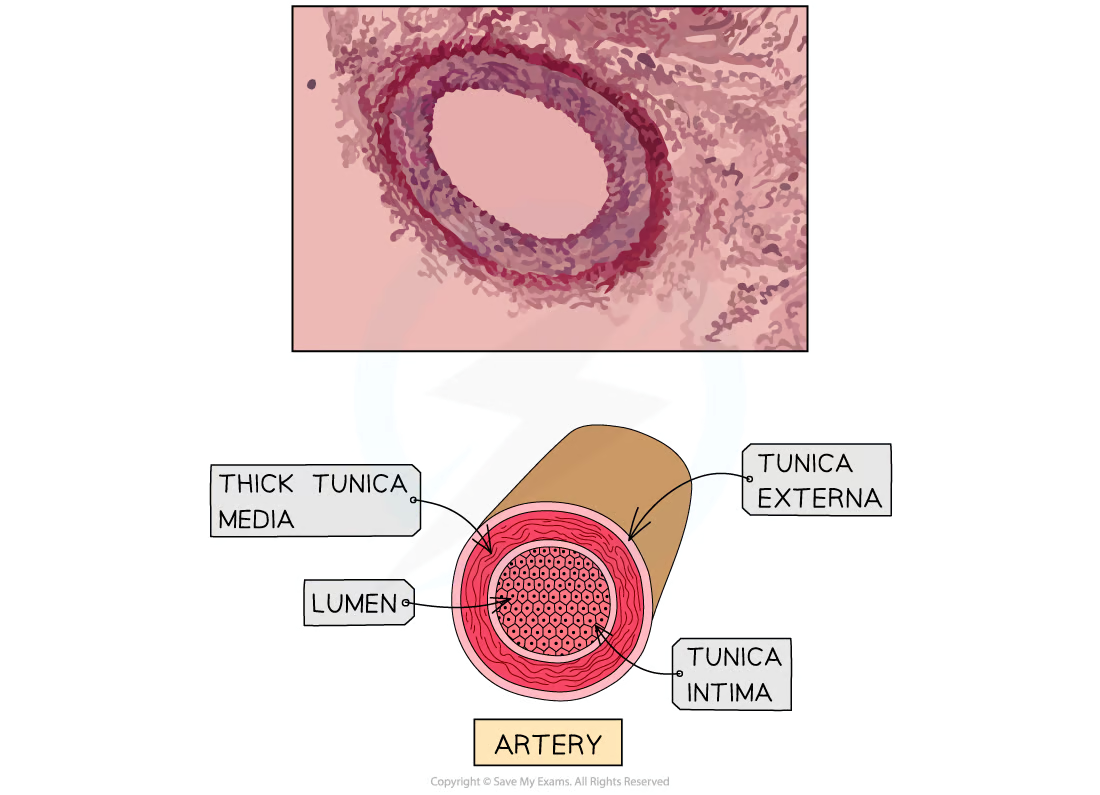
Arteries have 3 layers, prominent smooth muscle, no valves and
are deeper in the subcutaneous tissue.
Microcirculation
It is the part of the vascular system and consists of the small
vessels called arterioles, capillaries, and venules.
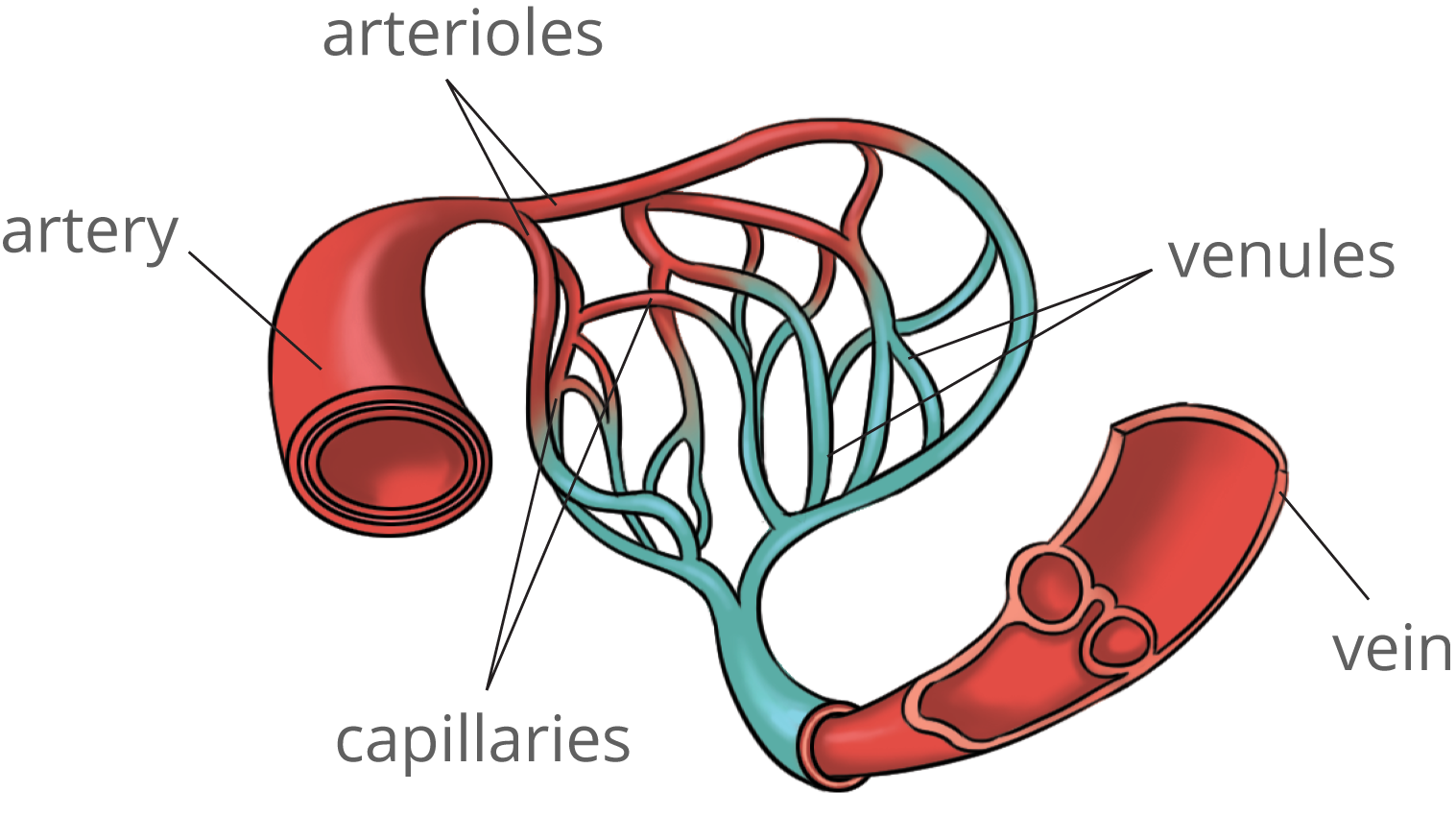
Functions
arterioles → resistance
control your blood pressure and blood flow throughout your body, using their muscles to change their diameter.
link to capillaries to exchange oxygen, nutrients and waste
venules → capacitance
smallest veins and receive blood from capillaries.
Also play a role in the exchange of oxygen and nutrients for water products
capillaries → exchange
have thin walls to facilitate exchange
Oxygen and nutrients from the blood can move through the walls and get into organs and tissues.
also take waste products away from your tissues.
Measuring blood pressure
When blood pressure is taken, it is reported as a “top number” and a “bottom number.” What do these numbers represent?
The top number represents the systolic blood pressure
The bottom number represents the diastolic blood pressure
normal blood pressure value → 120/80
Mean arterial BP (MAP) = [(2*DBP)+SBP]/3
How to measurre BP using a sphygmomanometer and a stethoscope
The cuff is inflated above 120 mmHg to stop arterial blood flow.
As the cuff is deflated, Korotkoff sounds are generated by turbulent blood flow through the brachial artery.The first instance of these sounds is systolic blood pressure.
What are the Korotkoff sounds?
Korotkoff sounds are the sound of blood flowing turbulently through the artery.
Korotkoff sounds are absent when the brachial artery is fully patent, and flow is laminar.
When the Korotkoff sounds cease, that is diastolic blood pressure.
How is pulse pressure calculated?
difference between the systolic and diastolic pressure
How is pulse measured and what is a typical value?
Pulse is typically measured by placing the tips of your index and middle finger on the radial artery at the wrist.
A typical value of a pulse is 60-100 beats per minute
Chronic hypertension
Antihypertensive medications
beta 1 blockers → metoprolol-Lopressor
alpha 1 blockers →