Session 8: Endocrine System Part 2 - Detailed Notes
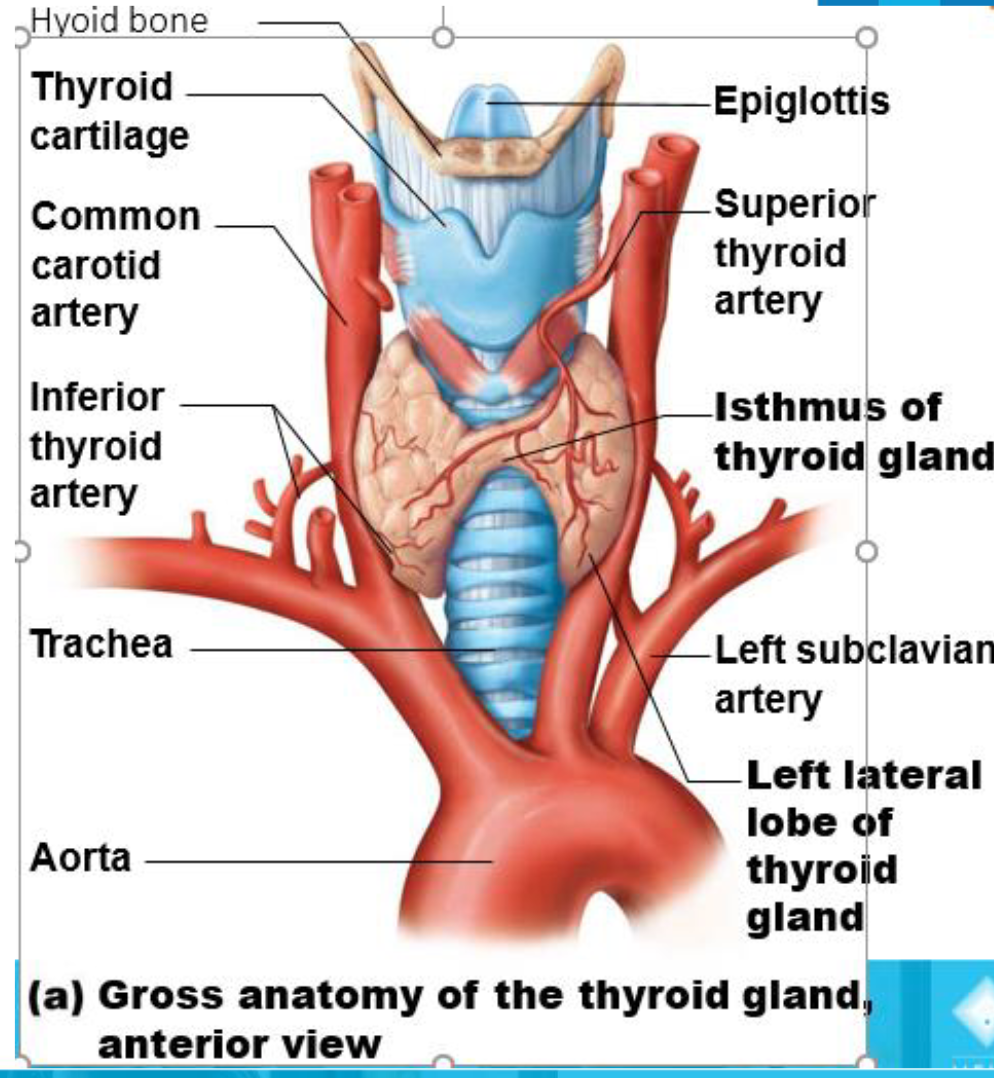
Thyroid Gland
Butterfly-shaped gland in the anterior neck on the trachea, just inferior to the larynx.
Consists of:
Isthmus: median mass connecting two lateral lobes.
Follicular cells secrete thyroid hormone.
Parafollicular cells secrete calcitonin.
Colloid-filled follicles contain precursors to thyroid hormone.
Thyroid Hormone (TH)
Body’s major metabolic hormone.
Found in two forms:
T4 (thyroxine): major form with two tyrosine molecules and four bound iodine atoms.
T3 (triiodothyronine): form with two tyrosines with three bound iodine atoms.
Must be converted to T3 at the tissue level.
Both are iodine-containing amine hormones.
Act like steroid hormones on target cells by binding to an intracellular receptor and moving to the nucleus.
Transport and Regulation
T4 and T3 are transported by thyroxine-binding globulins (TBGs) - protein carrier
T3 is 10 times more active than T4.
Peripheral tissues have an enzyme to convert T4 to T3 (removes one iodine).
TH release is regulated by negative feedback:
Falling TH levels stimulate the release of thyroid-stimulating hormone (TSH).
Rising TH levels provide negative feedback inhibition on TSH.
Major Functions
Affects virtually every cell in the body.
Enters target cell and binds to intracellular receptors within the nucleus, triggering the transcription of various metabolic genes.
Increases basal metabolic rate and heat production (calorigenic effect).
Regulates tissue growth and development.
Critical for normal skeletal and nervous system development and reproductive capabilities.
In adults, regulates nervous system reactivity.
Increases blood pressure.
Major Effects of Thyroid Hormone (T4 and T3)
Increases basal metabolic rate and heat production
• Referred to as calorigenic effectRegulates tissue growth and development
Critical for normal skeletal and nervous system development and reproductive capabilities
In the adult regulates nervous system reactivity
Increases bloodpressure

Calcitonin
Produced by parafollicular (C) cells in the thyroid gland in response to high Ca^{2+} levels.
Antagonist to parathyroid hormone (PTH).
Actions:
Inhibits osteoclast activity and prevents the release of Ca^{2+} from bone.
Stimulates Ca^{2+} uptake and incorporation into bone.
Parathyroid Gland
Four to eight tiny yellow-brown glands embedded in the posterior aspect of the thyroid.
Contain parathyroid cells that secrete parathyroid hormone (PTH).
PTH is the most important hormone in Ca^{2+} homeostasis.
Secreted in response to low blood levels of Ca^{2+}.
Inhibited by rising levels of Ca^{2+}.
Target organs are the skeleton, kidneys, and intestine.
Functions of Parathyroid Gland
Stimulates osteoclasts to digest bone and release Ca^{2+} to the blood.
Enhances reabsorption of Ca^{2+} by the kidneys.
Promotes activation of vitamin D by kidneys, which leads to increased absorption of Ca^{2+} by intestinal mucosa.
Adrenal Glands
Paired, pyramid-shaped organs atop the kidneys (suprarenal glands).
Structurally and functionally, two glands in one:
Adrenal cortex: three layers of glandular tissue that synthesize and secrete several different hormones.
Adrenal medulla: nervous tissue that is part of the sympathetic nervous system.
Mineralocorticoids
Regulate electrolyte concentrations (primarily Na^{+} and K^{+}) in ECF.
Importance of Na^{+}: affects ECF volume, blood volume, and blood pressure.
Importance of K^{+}: sets resting membrane potential of cells.
Aldosterone
Most potent mineralocorticoid.
Stimulates Na^{+} reabsorption by kidneys.
Stimulates K^{+} elimination by kidneys.
Primary factors that regulate aldosterone secretion:
Renin-angiotensin-aldosterone mechanism.
Plasma concentration of K^{+}.
Regulation of Aldosterone Release
Renin-angiotensin-aldosterone mechanism: Initiates cascade that produces angiotensin II.
Angiotensin II: Targets kidney tubules to increase the absorption of Na^{+} and increase secretion of aldosterone.
Absorption of Na^{+} and water causes increased K^{+} excretion, thereby increase blood volume and/or blood pressure.
Plasma concentration of K^{+}: A direct stimulating effect on the Adrenal cortex (zona glomerulosa).
Other Factors:
Adrenocorticotropic hormone (ACTH)
Atrial natriuretic peptide (ANP)
Glucocorticoids
Influence the metabolism of most cells and help resist stressors.
Keep blood glucose levels relatively constant.
Maintain blood pressure by increasing the action of vasoconstrictors.
Include:
Cortisol (hydrocortisone): the only glucocorticoid in significant amounts in humans.
Cortisone
Corticosterone
Cortisol - Regulation
Cortisol is released in response to ACTH.
ACTH is released in response to corticotropin-releasing hormone (CRH).
CRH is released in response to low cortisol levels.
Increased cortisol levels inhibit ACTH and CRH through negative feedback.
Secretion cycles are governed by patterns of eating and activity.
Acute stress (infection, physical or emotional trauma) interrupts cortisol rhythm.
Cortisol – Actions
Causes an increase in blood levels of glucose, fatty acids, and amino acids.
The prime metabolic effect is gluconeogenesis: the formation of glucose from fats and proteins by the liver.
Encourages cells to use fatty acids for fuel, so glucose is “saved” for the brain.
Enhances vasoconstriction, causing a rise in blood pressure.
Glucocorticoids – Actions (Prolonged High Levels)
Depress cartilage and bone formation (in kids).
Inhibit inflammation by decreasing the release of inflammatory chemicals.
Depress the immune system.
Disrupt normal cardiovascular, neural, and gastrointestinal functions.
Glucocorticoid drugs can control symptoms of many inflammatory diseases (arthritis, allergies) but can also cause undesirable effects.
Gonadocorticoids
Weak androgens (male sex hormones) converted to testosterone in tissue cells.
Examples: androstenedione and dehydroepiandrosterone (DHEA).
May contribute to:
Onset of puberty and appearance of secondary sex characteristics.
Sex drive in women.
Pubic & axillary hair growth.
Source of estrogens in postmenopausal women.
Adrenal Medulla
Medullary chromaffin cells synthesize catecholamines:
Adrenaline (epinephrine) (80%).
Noradrenaline (norepinephrine) (20%).
Effects of catecholamines:
Vasoconstriction.
Increased heart rate.
Increased blood glucose levels.
Blood diverted to the brain, heart, and skeletal muscle.
Adrenaline (Epinephrine) vs. Noradrenaline (Norepinephrine)
Both hormones have basically the same effects, but:
Adrenaline (epinephrine) is more of a stimulator of metabolic activities.
Example: bronchial dilation and increased blood flow to skeletal muscles and the heart.
Noradrenaline has more of an influence on peripheral vasoconstriction and blood pressure.
Responses to stressors are brief, unlike adrenal cortical hormones.
Short-Term Stress Response (Adrenal Medulla)
Heart rate increases
Blood pressure increases
Bronchioles dilate
The liver converts glycogen to glucose and releases glucose to the blood
Blood flow changes, reducing digestive system activity and urine output
Metabolic rate increases
Long-Term Stress Response (Adrenal Cortex)
Kidneys retain sodium and water
Blood volume and blood pressure rise
Proteins and fats converted to glucose or broken down for energy
Blood glucose increases
Immune system suppressed
Summary of Adrenal Gland Hormones
Mineralocorticoids (chiefly aldosterone)
Regulation of release: Stimulated by renin-angiotensin-aldosterone mechanism (activated by decreasing blood volume or blood pressure), elevated blood K^{+} levels, and ACTH (minor influence); inhibited by increased blood volume and pressure, and decreased blood K^{+} levels.
Target organ and effects: Kidneys: increase blood levels of Na^{+} and decrease blood levels of K^{+}; since water reabsorption usually accompanies sodium retention, blood volume and blood pressure rise.
Glucocorticoids (chiefly cortisol)
Regulation of release: Stimulated by ACTH; inhibited by feedback inhibition exerted by cortisol.
Target organ and effects: Body cells: promote gluconeogenesis and hyperglycemia; mobilize fats for energy metabolism; stimulate protein catabolism; assist the body to resist stressors; depress inflammatory and immune responses.
Gonadocorticoids (chiefly androgens, converted to testosterone or estrogens after release)
Regulation of release: Stimulated by ACTH; the mechanism of inhibition incompletely understood, but feedback inhibition not seen.
Target organ and effects: Insignificant effects in males; contributes to female libido; development of pubic and axillary hair in females; the source of estrogens after menopause.
Catecholamines (epinephrine and norepinephrine)
Regulation of release: Stimulated by preganglionic fibers of the sympathetic nervous system.
Target organ and effects: Mimic sympathetic nervous system activation; increase heart rate and metabolic rate; increase blood pressure by promoting vasoconstriction.
Pancreas
Triangular gland located partially behind the stomach.
Has both exocrine and endocrine cells.
Acinar cells (exocrine) produce enzyme-rich juice for digestion.
Pancreatic islets (islets of Langerhans) contain endocrine cells:
Alpha (\alpha) cells produce glucagon (hyperglycemic hormone).
Beta (\beta) cells produce insulin (hypoglycemic hormone).
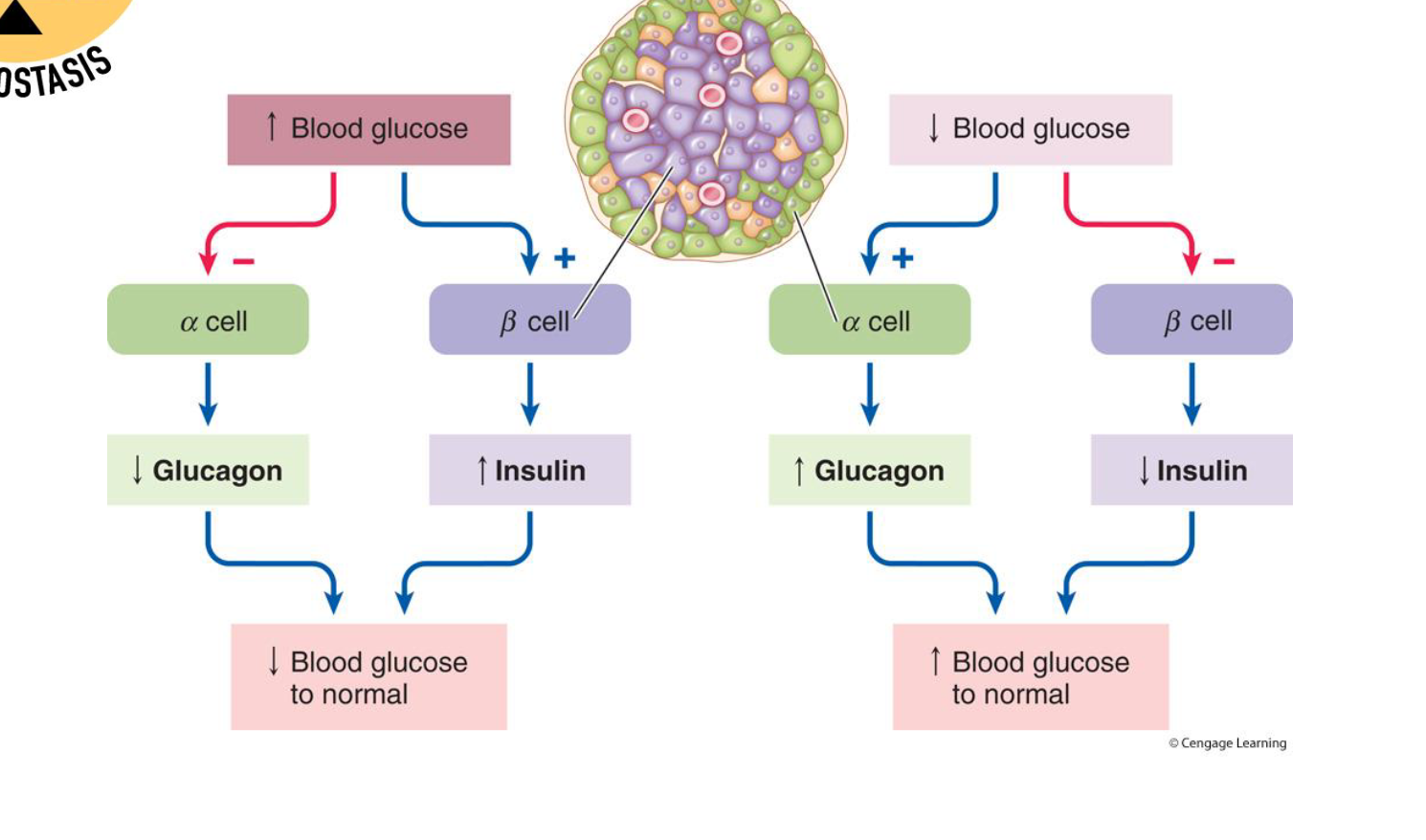
Pancreas - Insulin
Secreted when blood glucose levels increase.
Lowers blood glucose levels by:
Facilitating glucose uptake into cells.
Storing glucose as glycogen in the liver & skeletal muscle (glycogenesis).
Storing excess glucose and fatty acids as triglycerides in adipose tissue.
Inhibits breakdown of glycogen to glucose (glycogenolysis).
Storing amino acids as proteins in muscle.
Inhibits conversion of amino acids or fats to glucose (gluconeogenesis).
Regulation of Insulin Secretion
Food intake and increased blood glucose concentration are the major controls.
Increased Gastrointestinal hormones (incretins)
Increased Blood amino acid concentration
Parasympathetic stimulation
All Factors increase Islet Beta cells to increase insulin secretion, to decrease blood glucose, blood fatty acids, blood amino acids.
Protein synthesis.
Fuel storage
Sympathetic stimulation (and epinephrine)
Pancreas – Glucagon
Extremely potent hyperglycemic agent.
Triggered by decreased blood glucose levels, rising amino acid levels, or sympathetic nervous system.
Raises blood glucose levels by targeting the liver to:
Break down glycogen into glucose – Glycogenolysis.
Synthesize glucose from lactic acid and other non-carbohydrates – Gluconeogenesis.
Release glucose into the blood.
Insulin and Glucagon Regulation
Insulin:
From Tissue cells, insulin stimulates glucose uptake by cells
Stimulates glycogen formation in the liver
Stimulus: Blood glucose level rises to normal range
Glucagon:
Stimulates glycogen breakdown in the liver
Stimulus: Blood glucose level falls to normal range
Factors that Increase Blood Glucose
Glucose absorption from the digestive tract.
Hepatic glucose production:
Through glycogenolysis of stored glycogen.
Through gluconeogenesis.
Factors that Decrease Blood Glucose
Transport of glucose into cells:
For utilization for energy production.
For storage.
As glycogen through glycogenesis.
As triglycerides.
Urinary excretion of glucose (occurs only abnormally when the blood glucose level becomes so high it exceeds the reabsorptive capacity of kidney tubules during urine formation).
Gonads
Produce the same steroid sex hormones as those of the adrenal cortex, just in lesser amounts.
Ovaries
Produce estrogens and progesterone.
Estrogen
Maturation of reproductive organs.
Menstrual cycle.
Appearance of secondary sexual characteristics.
With progesterone, causes breast development and cyclic changes in the uterine mucosa.
Testes
Produce testosterone.
Initiates maturation of male reproductive organs.
Causes the appearance of male secondary sexual characteristics and sex drive.
Necessary for normal sperm production.
Maintains reproductive organs in a functional state.
Hormone Secretion by Other Organs
Heart
Atrial natriuretic peptide (ANP) decreases blood Na^{+} concentration, therefore blood pressure and blood volume.
Kidneys
Erythropoietin signals the production of red blood cells.
Renin initiates the renin-angiotensin-aldosterone mechanism.
Actions at Target Site by Gland/Organ/ Tissue
HORMONE | TARGETS GLAND/ORGAN/ TISSUE? | ACTION(S) AT TARGETSITE |
|---|---|---|
GH | anterior pituitary bone, muscle, fat | growth of tissues, protein synthesis, lipolysis, increase blood glucose |
PRL | anterior pituitary mammary glands | Stimulate milk production after birth |
TSH | anterior pituitary thyroid | Stimulates secretion of thyroid hormones |
ACTH | anterior pituitary adrenal cortex | Stimulates secretion of cortisol and androgens |
LH | anterior pituitary In males:testes in females:ovaries | males: testosterone secretion females: ovulation |
FSH | anterior pituitary males: testes; females: ovaries | males: sperm production females: follicle and ovum maturation |
ADH | posterior pituitary kidney | reabsorption of water |
Oxytocin | posterior pituitary uterine smooth muscle | contraction during labor |