Chapter 11 -Timby's -Lecture on Admission, Discharge, Transfer, and Referrals
Admission, Discharge, Transfer, and Referrals
Chapter 11 Timby
Learning Objectives
Upon completion of the lecture, students will be able to:
List the major steps involved in the admission process.
Identify common physiological responses when clients are admitted to health agencies.
List the steps involved in the discharge process.
Give examples of the use of transfers in client care.
Describe the levels of care that nursing homes provide.
Discuss the purpose of Minimum Data Set (MDS).
Explain the difference between transferring clients and referring clients.
Identify the contributing factors to the increased demand for home health care.
1. Major Steps in the Admission Process
Authorization from a physician.
Collection of billing information.
Completion of the agency’s admission database.
Documentation of medical history and physical examination findings.
Development of an initial nursing care plan.
Issuance of initial medical orders for treatment.
2. Common Responses to Admission
Clinical responses often include:
Anxiety
Fear
Decisional Conflict
Situational Low Self-Esteem
Powerlessness
Social Isolation
Ineffective Self-Health Management.
3. Steps in the Discharge Process
Discharge planning (starting at admission).
Obtaining physician authorization for medical discharge.
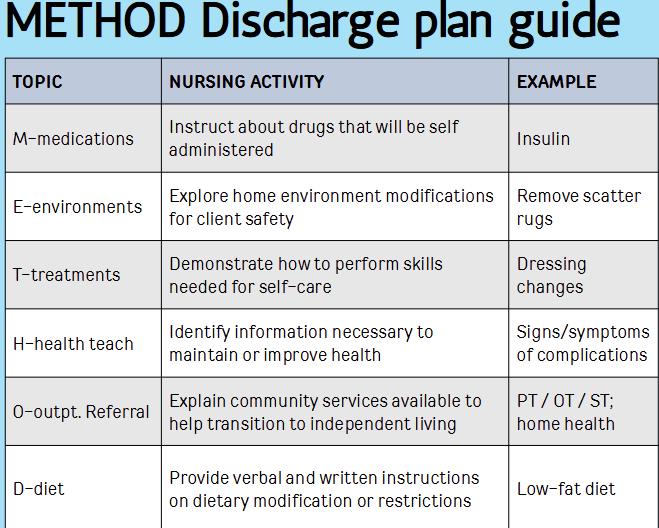
Completing discharge instructions (often using the METHOD acronym).
Notifying the business office to finalize financial records.
Assisting the client in leaving the agency.
Writing a summary of the client's condition at discharge.
Requesting room cleaning.
4. Examples of Transfers in Client Care
Moving a client to an intensive care unit for specialized care during a life-threatening situation.
Moving a client to a step-down or progressive care unit to reduce specialized healthcare costs.
Transferring a client to a general medical-surgical ward when they no longer require intensive observation.
5. Levels of Care in Nursing Homes
Skilled Nursing Facility (SNF): Provides high-level, 24-hour nursing care under a Registered Nurse (RN).
Intermediate Care Facility: Provides support for those requiring nursing care but not the intensive levels of an SNF.
Basic Care Facility: Provides assistance with activities of daily living (ADLs) for relatively independent individuals
6. Purpose of Minimum Data Set (MDS)
The MDS is a standardized screening and assessment tool used in nursing homes to identify resident problems.
It is updated every 3 months or when conditions change, and the results are integrated into the nursing care plan to ensure appropriate levels of care and screening
7. Transfer vs. Referral
Transfer: Discharging a client from one unit or agency and admitting them directly to another (e.g., from hospital to a nursing home) without the client going home in between.
Referral: Sending a client to another person or agency (usually private practitioners or community agencies) to receive specific specialized services
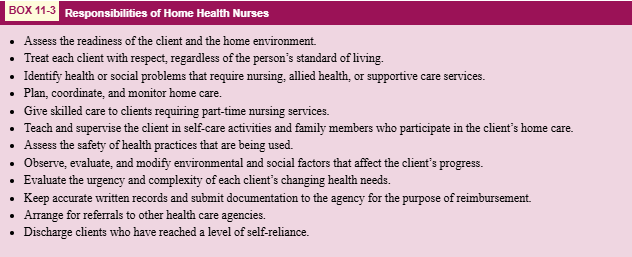
8. Factors for Increased Home Health Care Demand
Limitations by Medicare and insurance companies on the number of reimbursable hospital and nursing home days.
The growing number of chronically ill older adults who require continued assistance and nursing supervision.
Student Learning Outcomes (SLO's):
Safety
Patient-centered care
Professional behavior
Nursing judgment
Words To Know
Acute rehabilitation facility: A healthcare facility that provides intensive physical, occupational, and speech therapy for patients recovering from serious injury or illness.
Admission: Entering a health care agency for nursing care and medical or surgical treatment.
Basic care facility: An agency that provides individuals with assistance with activities of daily living (ADLs) while they remain relatively independent.
Clinical résumé: A concise summary of the client's hospital stay, including the reason for admission, significant findings, treatments provided, and the condition at the time of discharge.
Continuity of care: Uninterrupted client care despite changes in the caregivers or the setting.
Discharge: The termination of care from a health care agency.
Discharge planning: The process of identifying and anticipating a client's needs after discharge, starting at the time of admission.
Extended care facility: A health care agency that provides long-term care for individuals who require assistance over a prolonged period.
Home health care: Health care provided at home by an employee of a home health agency.
Intermediate care facility: A health agency that provides 24-hour nursing care and assistance to residents who do not require the intensive care of a hospital or skilled nursing facility.
Long-term care facility: A facility that provides nursing and medical care over an extended period for individuals who cannot care for themselves.
Medication reconciliation: The process of comparing a patient's medication orders to all of the medications that the patient has been taking to avoid errors.
Orientation: Helping a patient become familiar with a new environment and its routines.
Progressive care units: Specialized hospital units for patients who are stable enough to leave the ICU but still require close observation and monitoring.
Referral: Sending someone to another person or agency for specialized services.
Skilled nursing facility: A facility that provides 24-hour nursing care under the direction of a registered nurse for people who require high-level nursing intervention.
Step-down units: Similar to progressive care units, these bridge the gap between critical care and general medical-surgical wards.
Transfer: Discharging a client from one unit or agency and admitting them to another without going home in between.
Transfer summary: A written review of the client's current status and care needs at the time of transfer.
Transitional care units: Units designed to bridge the gap between acute care and the client's return to home or to a long-term care facility.
The Admission Process
Admission Definition
Admission refers to entering a health care agency for nursing care and medical or surgical treatment.
Major Steps Involved in the Admission Process
Authorization:
Obtaining authorization from a physician that the person requires specialized care and treatment.
Billing Information:
Collection of billing information by the admitting department of the health care agency.
Admission Database:
Completion of the agency’s admission database by nursing personnel.
Medical History:
Documentation of the client’s medical history and findings from physical examination.
Nursing Care Plan:
Development of an initial nursing care plan.
Initial Medical Orders:
Issuance of initial medical orders for treatment.
Types of Admissions
Type | Explanation | Example |
|---|---|---|
Inpatient | Length of stay generally more than 24 hrs | Acute Pneumonia |
Planned (nonurgent) | Scheduled in advance | Elective or required major surgery (e.g., bladder suspension) |
Emergency | Unplanned; stabilized in ED and transfers to nursing care unit | Unrelieved chest pain, major trauma, stroke |
Direct admission | Unplanned; emergency department is bypassed | Acute prolonged vomiting or diarrhea; major wound infection |
Outpatient | Length of stay less than 24 hrs | Minor surgery, cancer therapy, physical therapy |
Observational | Monitoring required; need for inpatient admission determined within 23 hrs | Head injury, unstable vital signs; premature or early labor |
Pharmacologic Considerations: Nonadherence to medication regimens accounts for more than 10% of older adult hospital admissions, nearly one fourth of nursing home admissions, and 20% of preventable adverse drug events among older persons in an ambulatory setting.
Admission Process Continued
Medical Authorization Details
Most patients will see their Primary Care Physician (PCP) or Emergency Department (ED) Medical Doctor (MD) just before admission.
MD Responsibilities:
Determine required procedures.
Advise patients and staff on how to proceed.
Admitting Department Responsibilities
Preliminary data collected.
Identification bracelet is issued.
Escort non-emergent patients to next place of care.
Clients who are extremely unstable or in severe discomfort may bypass the admitting department and go directly to the nursing unit.
Nursing Admission Activities
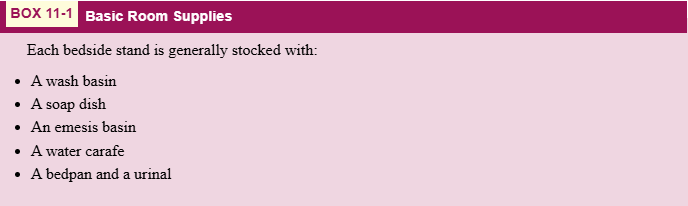
Preparing the Client’s Room
Ensure the room is ready for the incoming client.
Welcoming the Client
Greet the client warmly to ease anxiety.
Orienting the Client
Purpose: Facilitates comfort and adaptation by helping the client become familiar with the new environment.
Key Orientation Components:
Unit Features: The nurse describes the location of the nursing station, toilet, shower/bathing area, and lounges available to the client and visitors.
Storage: Instruction on where to store clothing and personal items.
Equipment Usage: How to call for nursing assistance from the bed and bathroom, adjust the hospital bed, and regulate room lights.
Utility Services: How to use the telephone (including night policies regarding diverted calls) and operate the television.
Daily Routine: Information on mealtimes, food ordering procedures, and expected times for doctor visits, surgeries, or laboratory/diagnostic tests.
Instructional Aids: While hospital booklets may provide extra details (gift shop, chapel), they must never replace a nurse's individualized explanations.
Safeguarding Valuables and Clothing
General Protocol: Nurses should give items such as prescription and nonprescription medications, jewelry, and large sums of money to family members to take home whenever possible.
Agency Policy and Storage: If family cannot take items, the nurse must follow agency policies:
Lockers: May be provided for clients expected to stay less than 24 hours.
Hospital Safe: Valuables may be stored here temporarily.
Documentation: Record the type of valuables and where they are safeguarded in the medical record.
Specificity: Be as descriptive as possible; for example, describe the type of metal and specific stones in a ring rather than simply recording ‘a ring.’
Legal Protections: To avoid legal implications or lawsuits regarding lost or stolen property:
Ensure a second nurse, supervisor, or security officer signs the envelope containing secured valuables.
Inventory Form: Use an inventory signed by both the nurse and client. Provide one copy to the client and keep another in the chart.
Updates: Revise the inventory and obtain new client signatures whenever items are added or returned to prevent discrepancies.
Helping the Client Undress
Purpose: Facilitate a physical examination.
Procedures for Assistance: If the client cannot undress independently, the nurse should:
Provide Privacy: Ensure the patient's dignity is maintained during the process.
Positioning: Have the client sit on the edge of the bed after it has been lowered.
Footwear and Stockings: Remove the client’s shoes and gather each stocking, sliding it down the leg and over the foot.
Rest: Help the client lie down if they feel weak or tired.
Clothing Removal: Release fasteners such as zippers and buttons. Remove items in a way that is most comfortable and least disturbing; for example, gather or fold a garment and work it up and over the body.
Facilitating Movement: Ask the client to lift their hips to slide clothes up or down, and lift the client’s head to guide garments over it.
Front/Back Fastening Items: Roll the client from side to side to remove clothes that fasten in the front or back.
Post-Undressing Care: Cover the client with a bath blanket or provide a hospital gown, explicitly explaining that hospital gowns fasten in the back.
Compiling the Nursing Database
Collect necessary clinical data and assessments.
Reconciling Medications
Verify current medications with patient.
Patient Belongings Form
Filled out and signed by nurse and patient.
One copy for the patient, one for the chart.
Similar policy for items the patient wishes to store in the safe with security.
Common Responses to Admission
Each admission is unique; responses may vary.
Common reactions/nursing diagnoses include:
Anxiety
Fear
Decisional Conflict
Situational Low Self-Esteem
Powerlessness
Social Isolation
Ineffective Self-Health Management
Nursing Intervention Strategies
Always evaluate the results and identify if the “expected outcomes” have been met
Interventions | Rationales |
|---|---|
Encourage use of previous methods to reduce anxiety | Known interventions with beneficial outcomes can increase potential effectiveness in current situations. |
Reduce external stimuli | Numerous stimuli escalate anxiety, interfering with attention and concentration, and taxing the client’s energy. |
Maintain a calm manner | A calm nurse can model a controlled state, promoting similar responses in the client. |
Establish trust | Knowing they can depend on the nurse helps relieve client insecurity. |
Stay with client during severe anxiety | Nurse presence can help the client regain control or return to comfort. |
Always evaluate outcomes | Identifying whether the expected outcomes have been met is crucial for effective care. |
The Discharge Process
Definition of Discharge
Discharge refers to the termination of care from a health care agency.
Discharge Planning Initiatives
Begins at admission or shortly thereafter.
Involves special considerations to ensure a smooth transition.
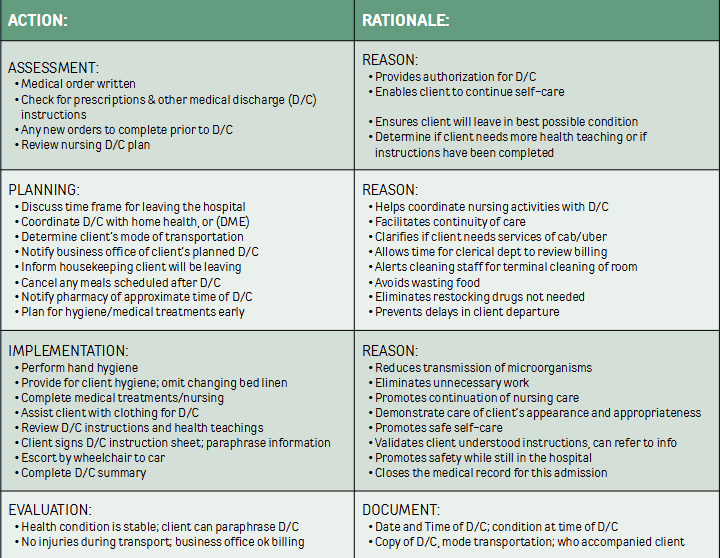
Steps in the Discharge Process
Discharge Planning
Obtaining Authorization for Medical Discharge
The physician determines when the client is well enough for discharge, usually after examining the client.
Before leaving, the physician writes the discharge order, provides written prescriptions, and indicates follow-up appointment details.
Leaving Against Medical Advice (AMA):
Occurs when a client leaves before physician authorization, often due to dissatisfaction with care.
Nursing Actions: Inform the physician and supervisor; attempt to negotiate a compromise or persuade the client to stay.
Documentation: Ask the client to sign a special AMA form to release the physician and agency from future responsibility. If the client refuses to sign, personnel cannot prevent them from leaving but must note the refusal in the medical record.
Insurance Considerations: It is a myth that insurance providers will refuse to pay for care following an AMA discharge.
Completing Discharge Instructions
Identification of Needs: The nurse establishes the anticipated knowledge, skills, and community resources the client requires for safe self-care at home.
METHOD Acronym: A planning technique used to identify specific discharge requirements (refer to Table 11.2).
Periodic Teaching: Education is provided incrementally during the hospital stay and documented accordingly.
Final Steps Prior to Departure:
Review previously provided teaching.
Hand over prescriptions to be filled.
Advise on the specific date and location for follow-up appointments as mandated by the physician.
Written Summary: The nurse provides a written copy of all discharge instructions. The client signs this document, keeping the original, while the nurse attaches the signed copy to the medical record.
Notifying the Business Office
Purpose: Ensures all financial and administrative records are finalized before the client departs.
Clerical Verification: Personnel verify insurance completeness and verify that a signed consent form exists for releasing medical information to insurance carriers.
Financial Arrangements: If records are incomplete or health insurance is missing, the client may be asked to arrange future payment plans before discharge.
Helping the Client Leave the Agency
Writing a Summary of the Client’s Condition at Discharge
Requesting Room Cleaning
Discharge Plan Guide Method
Discharge Process Implementation Steps
ACTION:
Medical order written
Check for prescriptions and other medical discharge instructions.
Planning for Discharge:
Collaborate for home health or durable medical equipment (DME).
Implementation:
Ensure hand hygiene and assist with patient's discharge.
Evaluation:
Review the client's health condition at discharge for stability.
DOCUMENTATION:
Log date, time, condition at discharge, mode of transportation, and who accompanied the client.
The Transfer Process
Definition of Transfer
Transfer refers to discharging a client from one unit or agency and admitting them to another without going home in between.
Reasons for Transfers
Facilitate more specialized care in life-threatening situations.
Reduce health care costs.
Provide less intensive nursing care.
Steps Involved in Transfer
Informing client and family about the transfer.
Completing a transfer summary.
Speaking with a nurse on the transfer unit to coordinate.
Transporting the client along with belongings, medications, nursing supplies, and charts to the new unit.
Extended Care Facilities
Definition: An extended care facility or long-term care facility (LTC) provides care for individuals who do not meet the criteria for acute hospitalization but still require assistance. While this description includes assisted living, adult day care, and hospice, extended care is most commonly associated with nursing homes.
Classification of Nursing Homes:
Skilled Nursing Facilities (SNF): Provide high-level, 24-hour nursing care under the direction of a Registered Nurse (RN).
Intermediate Care Facilities: Provide assistance for those requiring some nursing care but not the intensive levels provided in an SNF.
Basic Care Facilities: Provide help with activities of daily living (ADLs) for relatively independent individuals.
Types of Senior Living Options (2022)
Independent Living Options:
Aging in Place: Remaining in one's current home instead of moving to a facility.
55+ Retirement Communities: Age-restricted housing limited to seniors.
Senior Cohousing Communities (SCCs): A group of seniors design or purchase a complex with private rooms and shared common areas.
Senior Home Sharing: Older adults share living spaces to reduce costs or exchange help with tasks for reduced rent.
Options with Assistance:
Nursing Homes: Clinical environments offering high-level medical care, medication management, and 2424-hour supervision.
Respite Care: Short-term care provided by assisted living or nursing homes for those needing temporary help.
Continuing-Care Retirement Communities (CCRCs): Properties including apartments, assisted living, and nursing homes on one site; residents move between areas as needs change.
Assisted Living: Provides help with instrumental activities of daily living (IADLs), such as cooking and bathing, with limited medical assistance.
Memory Care Facilities: Specialized nursing or assisted living units for individuals with dementia, featuring larger staff-to-patient ratios.
Hospice: Care focused on pain management and comfort for those with terminal illnesses, provided at home or in facilities.
Skilled Nursing and Acute Rehabilitation Facilities
Qualification Criteria: To qualify for skilled care, a client must be referred by a physician and require daily skilled nursing care or intensive physical therapy (PT).
Multidisciplinary Team: Includes nurses, PT, occupational therapists (OT), pharmacists, dietary services, and dental services (often on a contract basis).
Common Procedures Qualifying for Skilled Care:
Care for pressure ulcers.
Enteral feedings or intravenous (IV) fluids.
Bowel or bladder retraining.
Injectable medications.
Sterile dressing changes.
Tracheostomy care.
Recovery from significant illness, stroke, surgery, or accidents.
Financial and Insurance Considerations
Medicare Part A Benefits for Skilled Care:
Requirement: The client must have been hospitalized for 3 days or more within 30 days prior to admission for skilled care.
Days 1 to 60: Full assistance for eligible clients.
Days 61 to 90: The client must pay co-insurance.
Day 101: Medicare Part A benefits are exhausted; the client is responsible for 100% of costs.
Medicaid: Once a client's financial resources (and those of a spouse) are exhausted, they may apply for state Medicaid to cover continued long-term care costs.
Determining the Level of Care
Minimum Data Set (MDS)
MDS Defined:
A standard form for nursing home resident assessment and care screening developed by the Health Care Financing Association.
Requires updates every three months or whenever a client's condition changes.
The problems identified on the MDS are integrated into the nursing care plan.
MDS Factors for Evaluation
Cognitive patterns, communication/hearing patterns, vision patterns.
Physical functioning and structural problems.
Continence patterns in the last 14 days.
Psychosocial well-being, mood & behavior patterns.
Activity patterns, disease diagnoses, and health conditions.
Oral, nutritional and dental status; skin conditions; medication use; special treatments or procedures.
The Referral Process
Definition of Referral
Referral involves sending someone to another person or agency for specialized services.
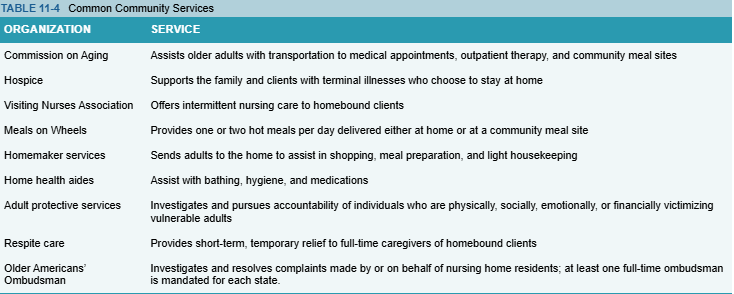
Generally made to private practitioners or community agencies.
Early planning is essential to ensure continuity of care.
Home Health Care
Definition: Health care provided at home by an employee of a home health agency.
Helps shorten recovery time in hospital, prevents admissions to extended care facilities, and reduces readmissions to acute care settings.
Contributing Factors to Increased Demand for Home Health Care
Limitations imposed by Medicare and insurance companies on the number of reimbursable hospital and nursing home days.
Growing number of chronically ill older adults needing assistance.
General Gerontologic Considerations
Older adults may minimize their symptoms and require consideration for smooth transitions during admissions, discharges, or transfers.
Pets can serve as important social support systems.
Early discharge planning with appropriate community resources can facilitate a successful return to home.
Barriers to Community-Based Services
Financial limitations or distrust in service providers.
Reluctance to admit need for services.
Lack of time, energy, or ability to find suitable services.
KEY POINTS
Admission Overview
Definition: Entering a health care agency for nursing care and medical/surgical treatment.
Inpatient Care: Longer than 24 hours; includes planned, emergency, and direct admissions.
Outpatient Care: Shorter than 24 hours; often used for observation.
Nursing Responsibilities for Admission
Setting up the room
Welcoming the client
Orienting the client
Safeguarding valuables and clothing
Helping the client undress
Compiling the nursing database
Reconciling medications
Initial nursing care plan
Medical admission responsibilities
Discharge Planning and Implementation
Process: Improves outcomes by predetermining needs and coordinating community resources; starts at admission.
Major Steps:
Obtaining medical authorization.
Providing detailed discharge instructions via the METHOD acronym.
Notifying the business office for financial closure.
Documenting the discharge summary, including transportation and client condition.
Referrals and Level of Care
Level of Care Determination: Assessed prior to or at admission using the Minimum Data Set (MDS) for nursing home assessment.
MDS Schedule: Repeated every 3 months or when the client's condition changes significantly.
Home Health Care
Services: A wide range of healthcare services provided in the home for illness or injury.
Benefits: Usually less expensive, more convenient, and provides a continuum of care comparable to facility-based settings.
CRITICAL THINKING EXERCISES
Discuss how the admission of a child might differ from that of an adult.
Compare and contrast admission to a hospital and to a nursing home.
Describe the criteria you would use when selecting a nursing home for a relative.
If it becomes apparent that a relative cannot continue to live independently, what options would you pursue?
NEXT-GENERATION NCLEX-STYLE REVIEW QUESTIONS
Which nursing action is essential for complying with federal regulations that ensure the client’s right to privacy?
a. Addressing clients only by their first names
b. Obtaining consent for releasing information
c. Referring to the client as the person in Room 201201
d. Using a code number rather than a name in the medical record
Test-Taking Strategy: Although all the options may protect the client’s privacy, select the best option from among those provided.
Which information is essential for the nurse to obtain at the time of a client’s admission to a health care agency?
a. Social security number
b. Medicare status
c. Advance directive
d. Health insurance policy
Test-Taking Strategy: Eliminate options that identify information that is unnecessary or may be obtained by personnel in the business office. Select the option that correlates with information that is important to the nursing care of clients.
Which nursing observation is most suggestive that a newly admitted client is anxious?
a. The client is unusually quiet and withdrawn.
b. The client is restless and awakens frequently.
c. The client eats little food at each meal.
d. The client misses their spouse and children.
Test-Taking Strategy: Select the option that is most representative of manifestations associated with stimulation of the sympathetic nervous system.
If the nurse suspects that an older adult in the community is the target of abuse, what agency would be appropriate to contact?
a. Commission on Aging
b. Visiting Nurse Association
c. Older Americans’ Ombudsman
d. Adult Protective Services
Test-Taking Strategy: Use the process of elimination to select the agency whose mandate is to ensure the safety of vulnerable adults.
Which type of extended care facility referral would be most appropriate for the nurse to recommend for an older adult who needs further rehabilitation for mobility at the time of discharge from an acute care facility?
a. Skilled care facility
b. Intermediate care facility
c. Basic care facility
d. Assisted living facility
Test-Taking Strategy: Eliminate options that fail to correlate with the client’s level of care