Session: 7 Endocrine System & Pituitary Gland Notes
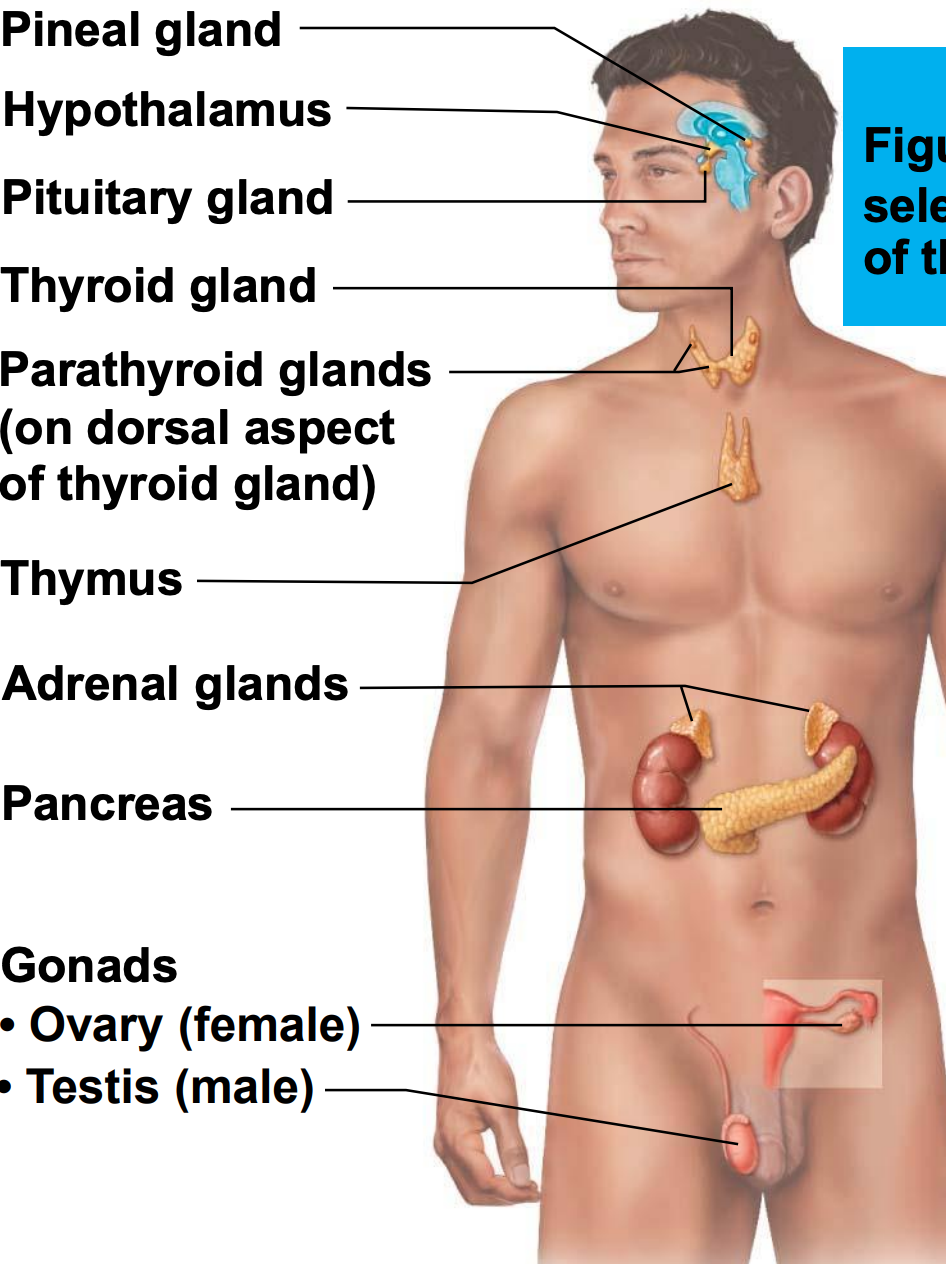
Endocrine System Overview
Exocrine glands:
Produce non-hormonal substances (e.g., sweat, saliva).
Have ducts to carry secretions to the membrane surface.
Endocrine glands:
Produce hormones.
Lack ducts.
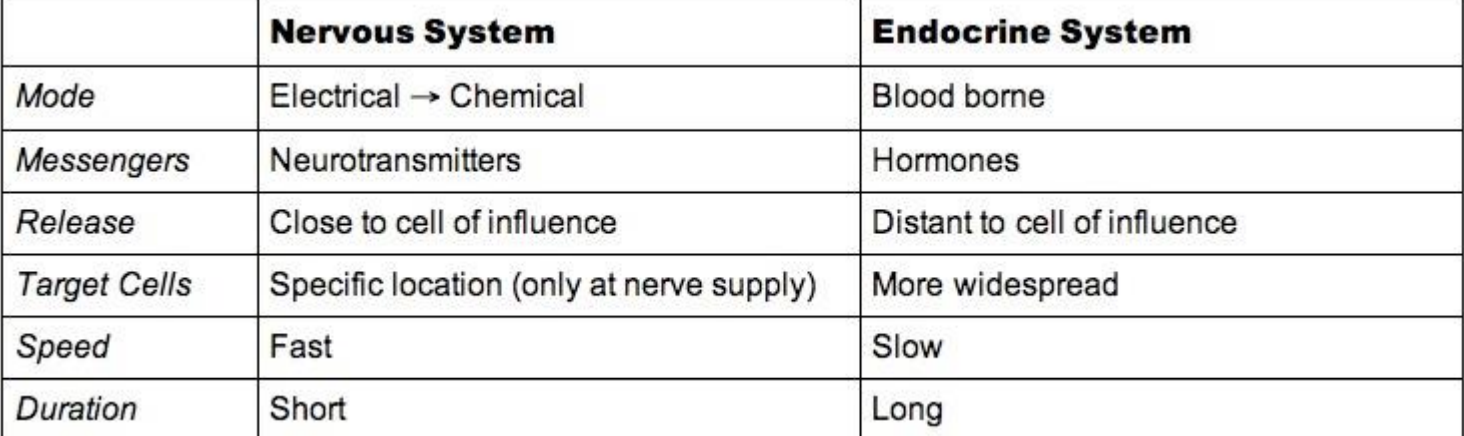
The endocrine system works with the nervous system to coordinate and integrate the activity of body cells.
It influences metabolic activities via hormones transported in the blood.
Responses are slower but longer-lasting than nervous system responses.
Endocrinology is the study of hormones and endocrine organs.
Endocrine System Function
The endocrine system controls and integrates:
Reproduction.
Growth and development.
Maintenance of electrolyte, water, and nutrient balance of blood.
Regulation of cellular metabolism and energy balance.
Mobilization of body defenses.
Action of Hormones
Hormones circulate systemically, but only cells with receptors for that hormone are affected.
Target cells are tissues with receptors for a specific hormone.
Hormones alter target cell activity.
TSH (Thyroid-stimulating hormone) binds and acts on the thyroid gland cells.
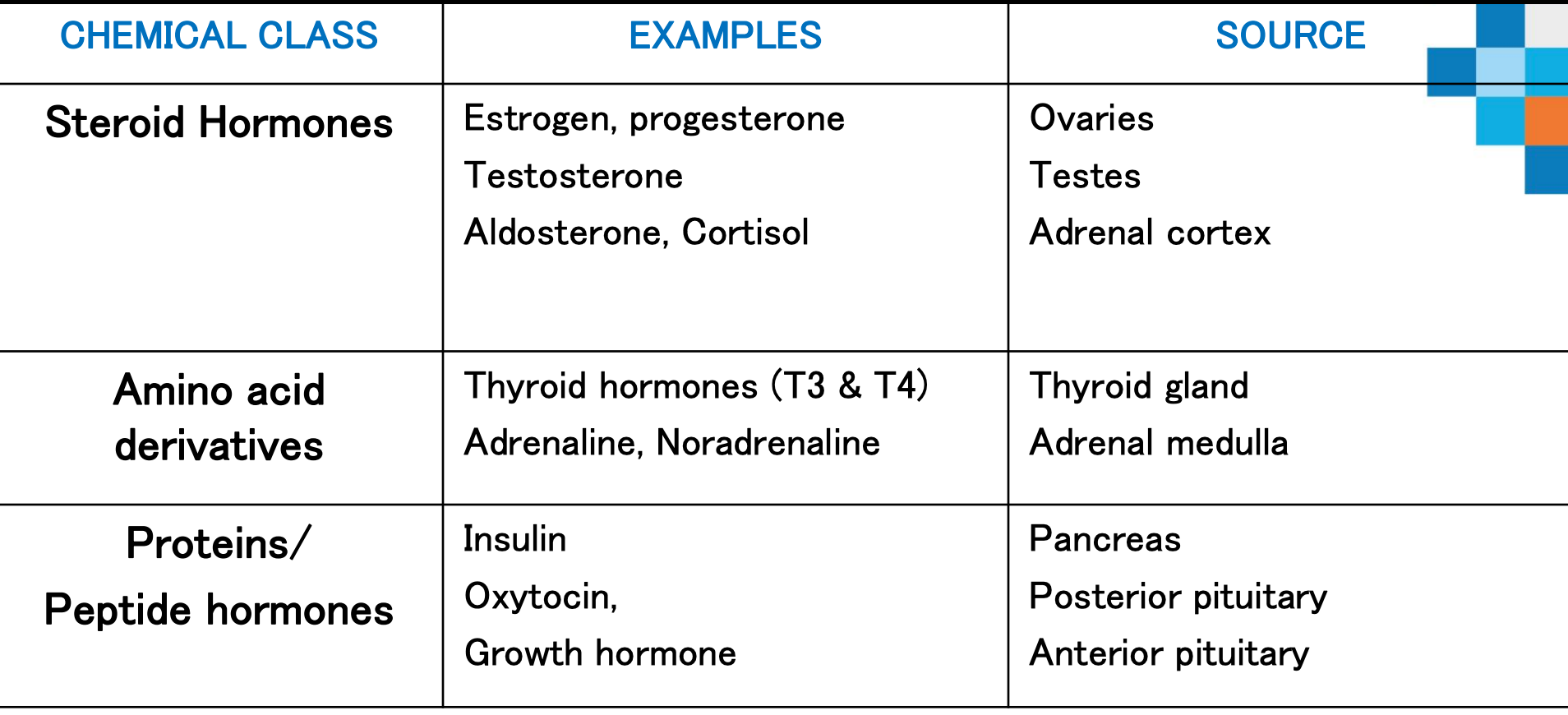
Hormone Chemical Structure
Two main classes of hormones:
Amino acid–based hormones
Amino acid derivatives, peptides, and proteins.
Steroids
Synthesized from cholesterol.
Gonadal (testosterone, estrogen, progesterone) and adrenocortical hormones (aldosterone, cortisol, androgens).
Chemical Structure of Hormones most common elements
Element | Symbol | Role & Why It's Common |
|---|---|---|
Carbon | C | Backbone of all organic molecules, forms stable chains and rings essential for hormone structure (e.g., steroids, peptides) |
Hydrogen | H | Bonds with carbon to complete structures, forms functional groups (–CH₃, –OH) critical for shape and function |
Oxygen | O | Found in hydroxyl (–OH), carbonyl (C=O), carboxyl (–COOH) groups; important for polarity, solubility, and hydrogen bonding |
Nitrogen | N | Present in amino groups (–NH₂) of peptide and amine hormones; key for forming proteins and neurotransmitters |
Sulfur | S | Present in some peptide hormones (like insulin) via disulfide bonds, which stabilize 3D structure |
Iodine | I | Unique to thyroid hormones (T3, T4); essential for their synthesis and function |
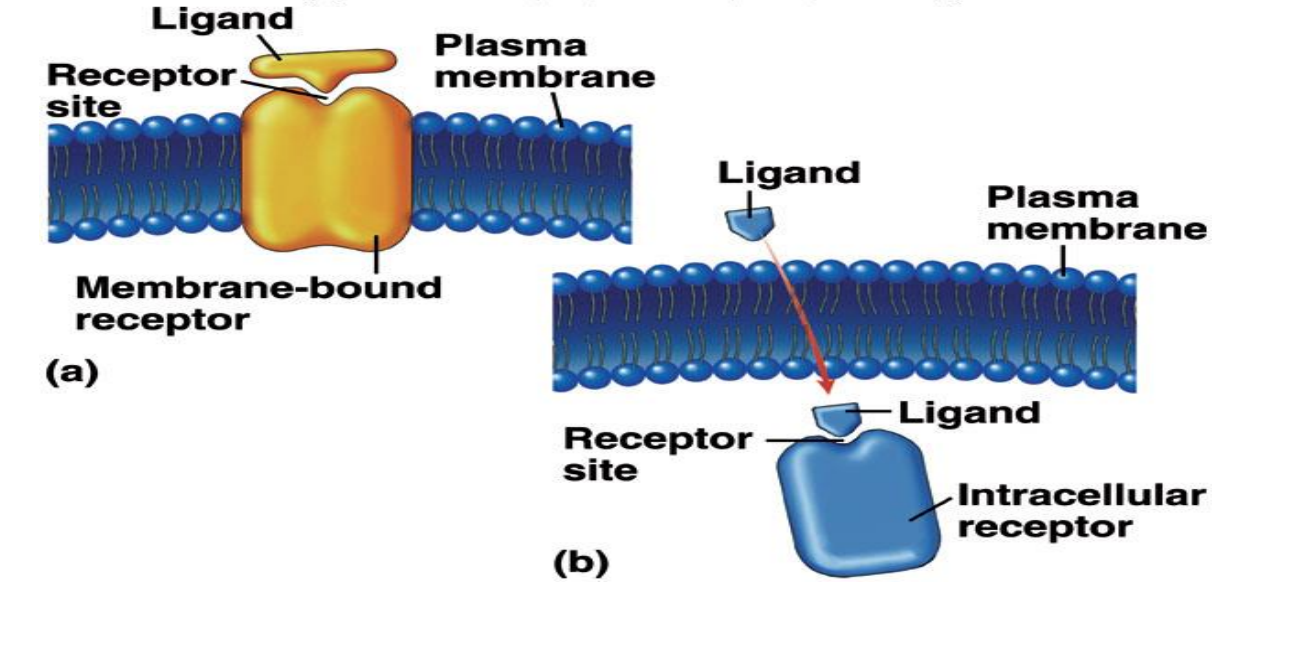
Action of Hormones (Mechanism)
Hormones act in one of two ways, depending on their chemical nature and receptor location:
Water-soluble hormones (all amino acid–based hormones except thyroid hormone):
Act on plasma membrane receptors.
Act via G protein second messengers.
Cannot enter the cell.
Lipid-soluble hormones (steroid and thyroid hormones):
Act on intracellular receptors that directly activate genes.
Can enter the cell.
Classes of Hormone Receptors
Membrane-bound receptors bind to water-soluble or large-molecular-weight hormones.
Intracellular receptors bind to lipid-soluble hormones.
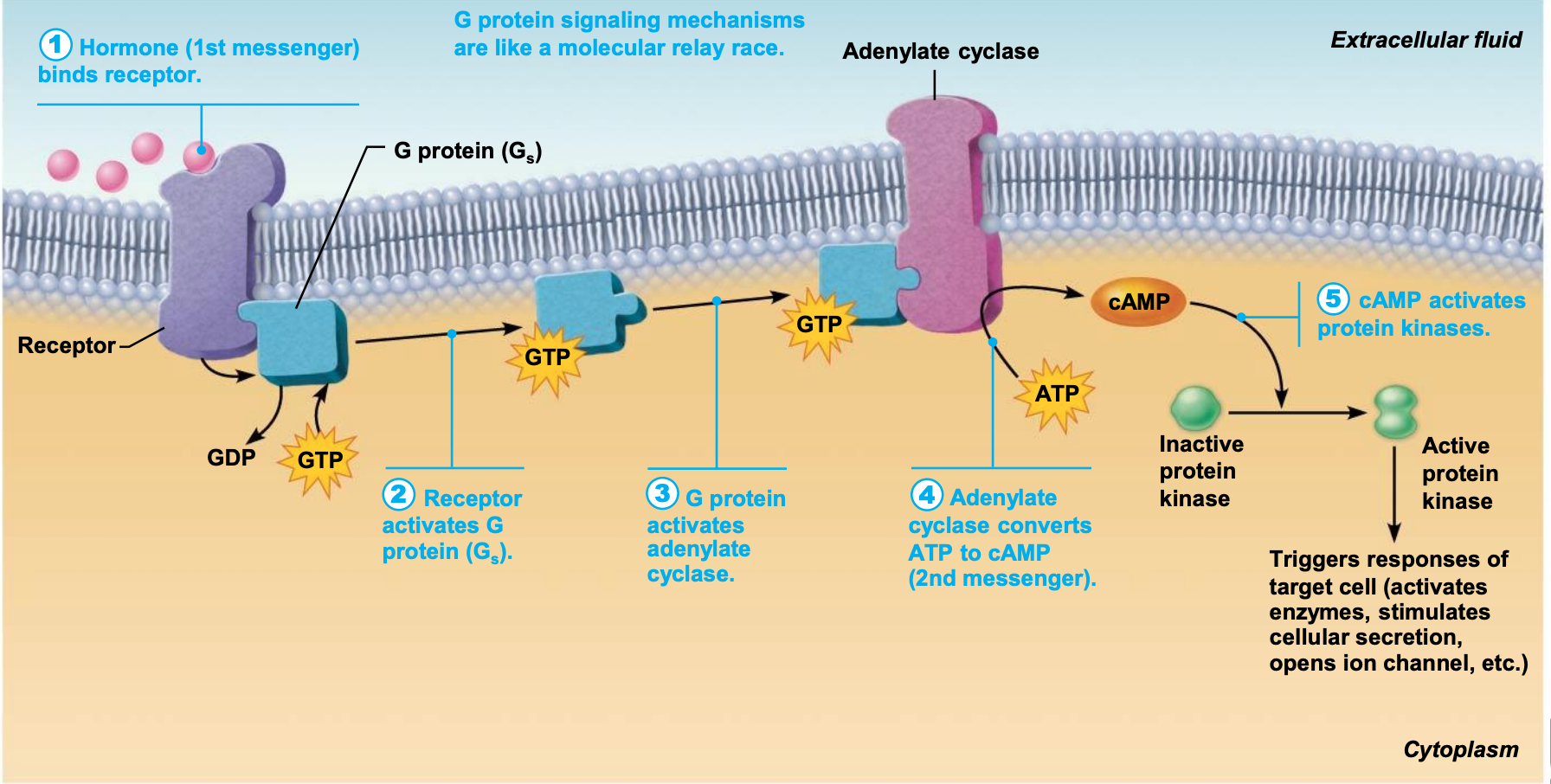
Plasma Membrane Receptors and Second-Messenger Systems
Amino acid–based hormones, except thyroid hormone, exert effects through second-messenger systems.
signal sent from outside the cell to the inside
Two main second-messenger systems:
Cyclic AMP.
PIP2 -calcium (this won’t be discussed).
Cyclic AMP (cAMP) signaling mechanism:
Hormone (first messenger) binds to receptor.
Receptor activates a G protein.
G protein activates or inhibits effector enzyme adenylate cyclase(converts ATP into cAMP)
Adenylate cyclase then converts ATP to cAMP (second messenger).
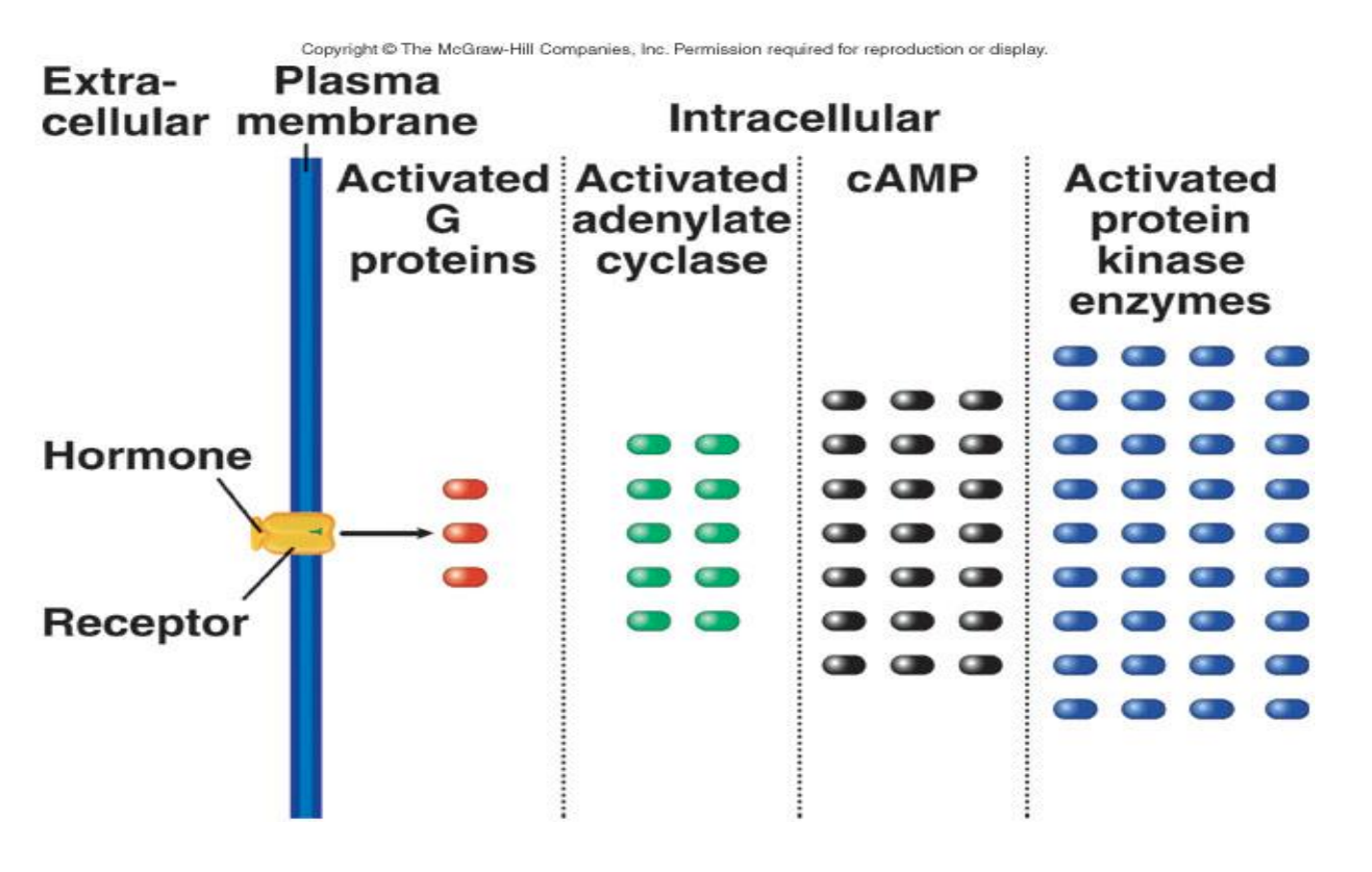
cAMP activates protein kinases that phosphorylate (add a phosphate) other proteins (this can change shape/ function op protein)
Phosphorylated proteins are then either activated or inactivated.
cAMP is rapidly degraded (broken down) by enzyme phosphodiesterase, stopping cascade.
Cascades have huge amplification effect.
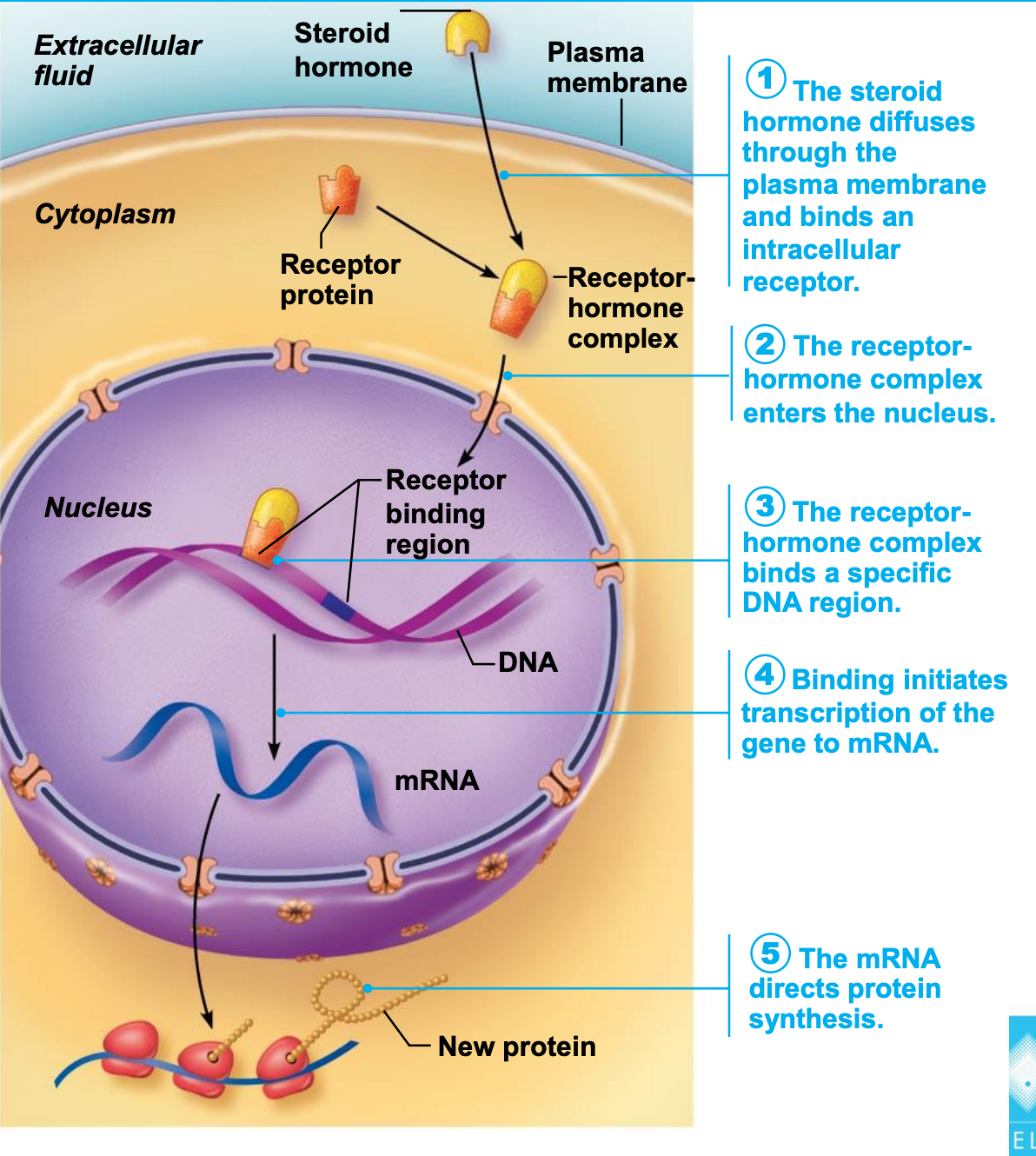
Steroid & Thyroid Hormones: Intracellular Receptors and Direct Gene Activation
Lipid-soluble steroid hormones and thyroid hormone can diffuse into target cells and bind with intracellular receptors.
Receptor-hormone complex enters the nucleus and binds to a specific region of DNA.
Helps initiate DNA transcription to produce mRNA.
mRNA is then translated into a specific protein.
Proteins synthesized have various functions:
Examples: metabolic activities, structural purposes, or exported from the cell.
Hormone Release
Blood levels of hormones are controlled by negative feedback systems.
Increased hormone effects on target organs can inhibit further hormone release.
Levels vary only within a narrow, desirable range.
Hormone release is triggered by:
Humoral stimuli (changes in blood levels of non-hormone chemicals)
Neural stimuli (stimulation of cells, tissues, or glands by the nervous system)
Hormonal stimuli.
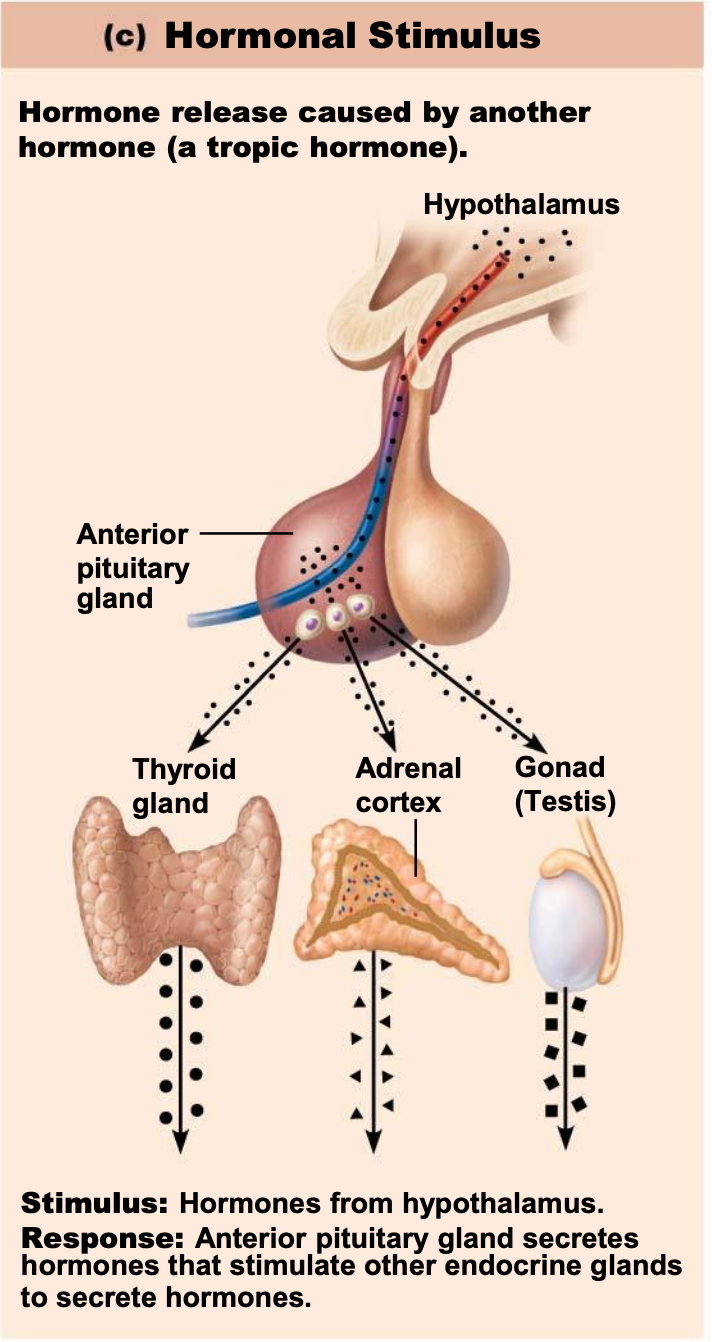
Hormonal Stimulus
Hormone release is caused by another hormone (a tropic hormone).
Stimulus: Hormones from the hypothalamus.
Response: The anterior pituitary gland secretes hormones that stimulate other endocrine glands to secrete hormones.
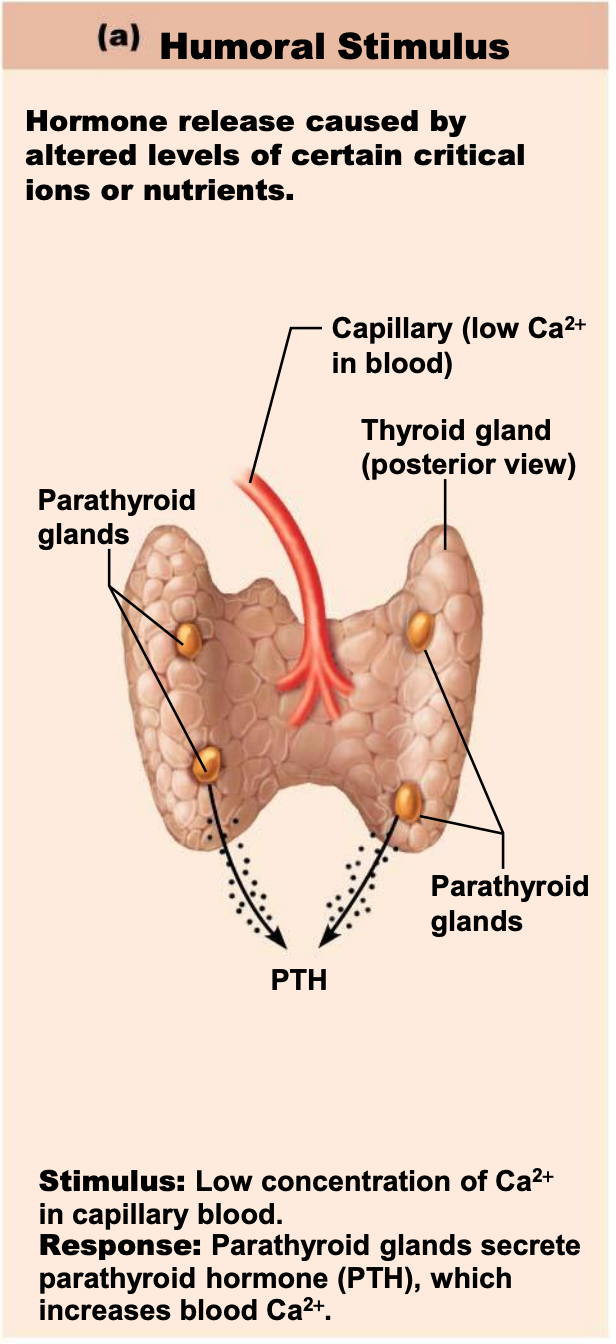
Humoral Stimulus
Hormone release is caused by altered levels of certain critical ions or nutrients.
Stimulus: Low concentration of Ca^{2+} in capillary blood.
Response: Parathyroid glands secrete parathyroid hormone (PTH), which increases blood Ca^{2+}.
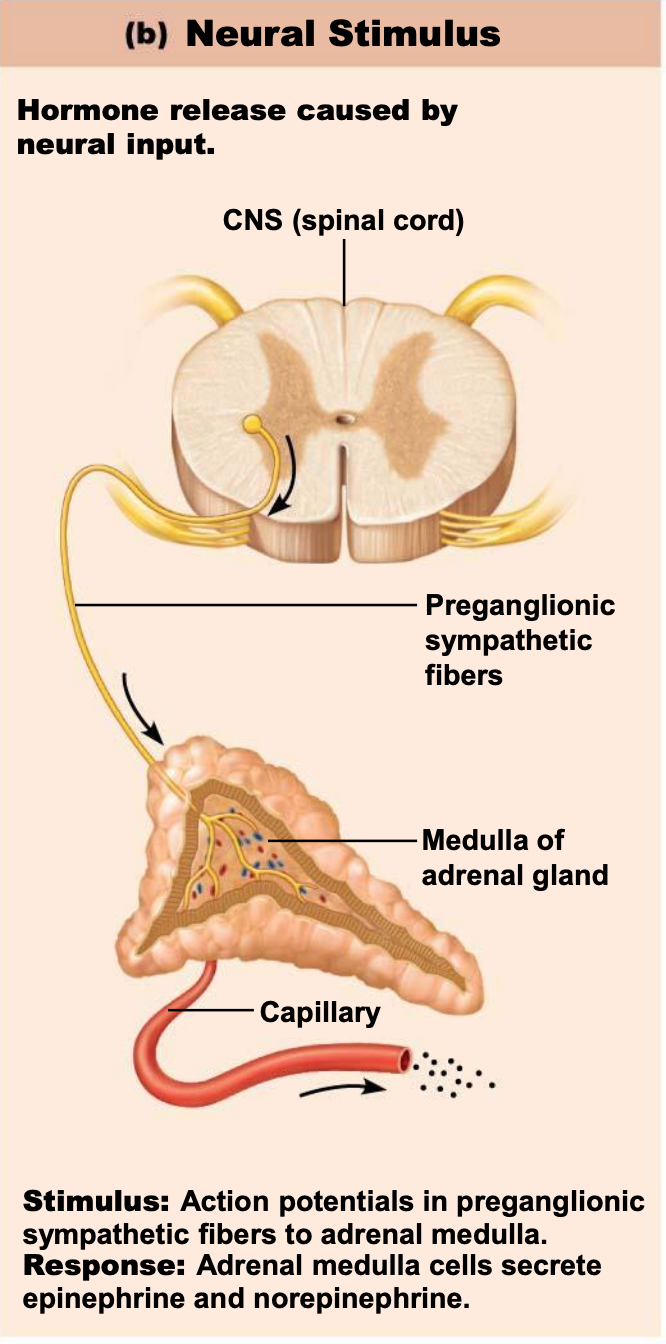
Neural Stimulus
Hormone release is caused by neural input.
Stimulus: Action potentials in preganglionic sympathetic fibers to adrenal medulla.
Response: Adrenal medulla cells secrete epinephrine and norepinephrine.
Onset and Duration of Hormone Activity
Onset (initial production) and duration of hormone activity are dependent on whether the hormone is water or lipid-soluble.
Hormones have different response times:
Some responses are immediate.
Some, especially steroid hormones, can take hours to days.
Some are inactive until they enter target cells.
The duration of response is usually limited, ranging from 10 seconds to several hours.
Effects may disappear rapidly as blood levels drop, but some may persist for hours at low blood levels.
Hormones - Blood Transport
Hormones circulate in the blood either free or bound.
Steroids and thyroid hormones are attached to plasma proteins.
All other hormones circulate without carriers.
Transport and Distribution
Some hormones are transported freely in the blood.
As concentration of free hormone increases in the blood, more hormone molecules diffuse from capillaries into interstitial spaces (fluid-filled areas between cells and organs) to bind to target cells.
Effects are short-lived, as free hormone is rapidly eliminated from the blood by the liver and kidneys.
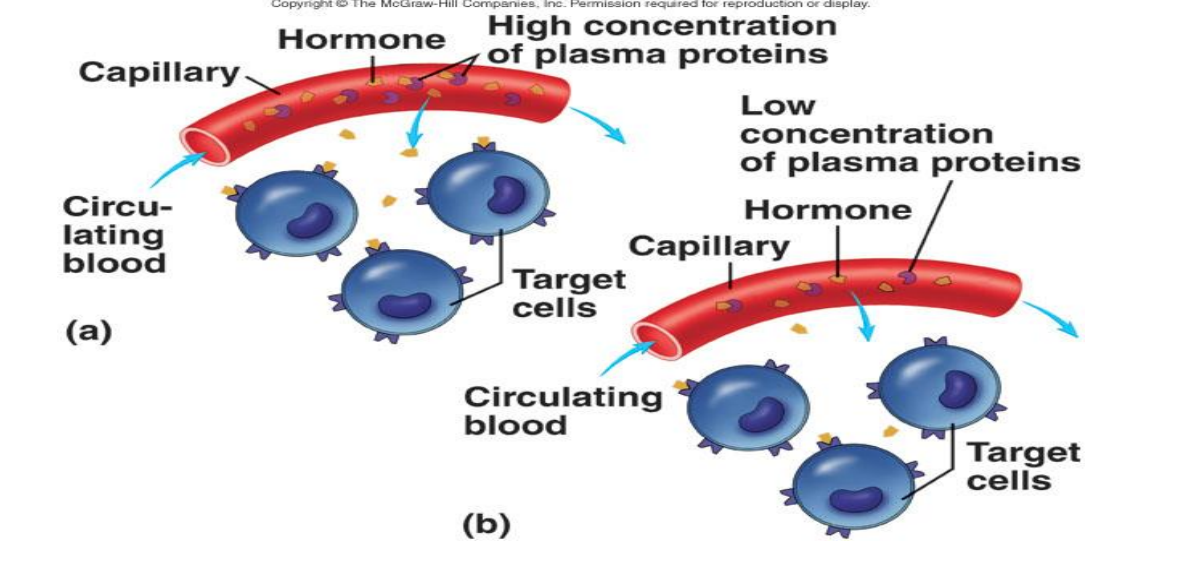
Lipid-soluble hormones and thyroid hormone circulate bound to plasma proteins.
An equilibrium is established between free hormone and hormone bound to plasma proteins.
Only free hormones can diffuse through capillaries to target cells.
A decrease in plasma protein concentration leads to an increase in the concentration of free hormone in circulation which in turn lead to rapid elimination ⟶ less available to bind to target cells.
Plasma protein binding decreases the rate of elimination and increases the half-life of the hormone.
Half-Life & Duration of Hormone Activity
The concentration of circulating hormone reflects:
Rate of release
Speed at which it is inactivated and removed from the body
Hormones can be removed from the blood by:
Degrading enzymes
Kidneys
Liver
Half-life: the time required for the level of hormone in the blood to decrease by half.
Varies anywhere from a fraction of a minute to a week, depending on the hormone.
Target Cell Specificity
Target cells must have specific receptors to which a hormone binds.
Example: ACTH receptors are found only on certain cells of the adrenal cortex, but thyroxin receptors are found on nearly all cells of the body.
Target cell activation depends on three factors:
Blood levels of hormone
Relative number of receptors on/in target cell
Affinity (strength) of binding between receptor and hormone
Comparison Between Lipid- and Water-Soluble Hormones
Feature | Lipid-Soluble Hormones | Water-Soluble Hormones | |
|---|---|---|---|
Examples | All steroid hormones and thyroid hormone | All amino acid-based hormones except thyroid hormone | |
Sources | Adrenal cortex, gonads, and thyroid gland | All other endocrine glands | |
Storage in secretory vesicles | No | Yes | |
Transport in blood | Bound to plasma proteins | Usually free in plasma | |
Half-life in blood | Long (most need to be metabolized by the liver) | Short (most can be removed by kidneys) | |
Location of receptors | Usually inside the cell | On the plasma membrane | |
Mechanism of action | Activate genes, causing synthesis of new proteins | Usually act through second-messenger systems |
The Endocrine System 2 Part A – Pituitary Gland
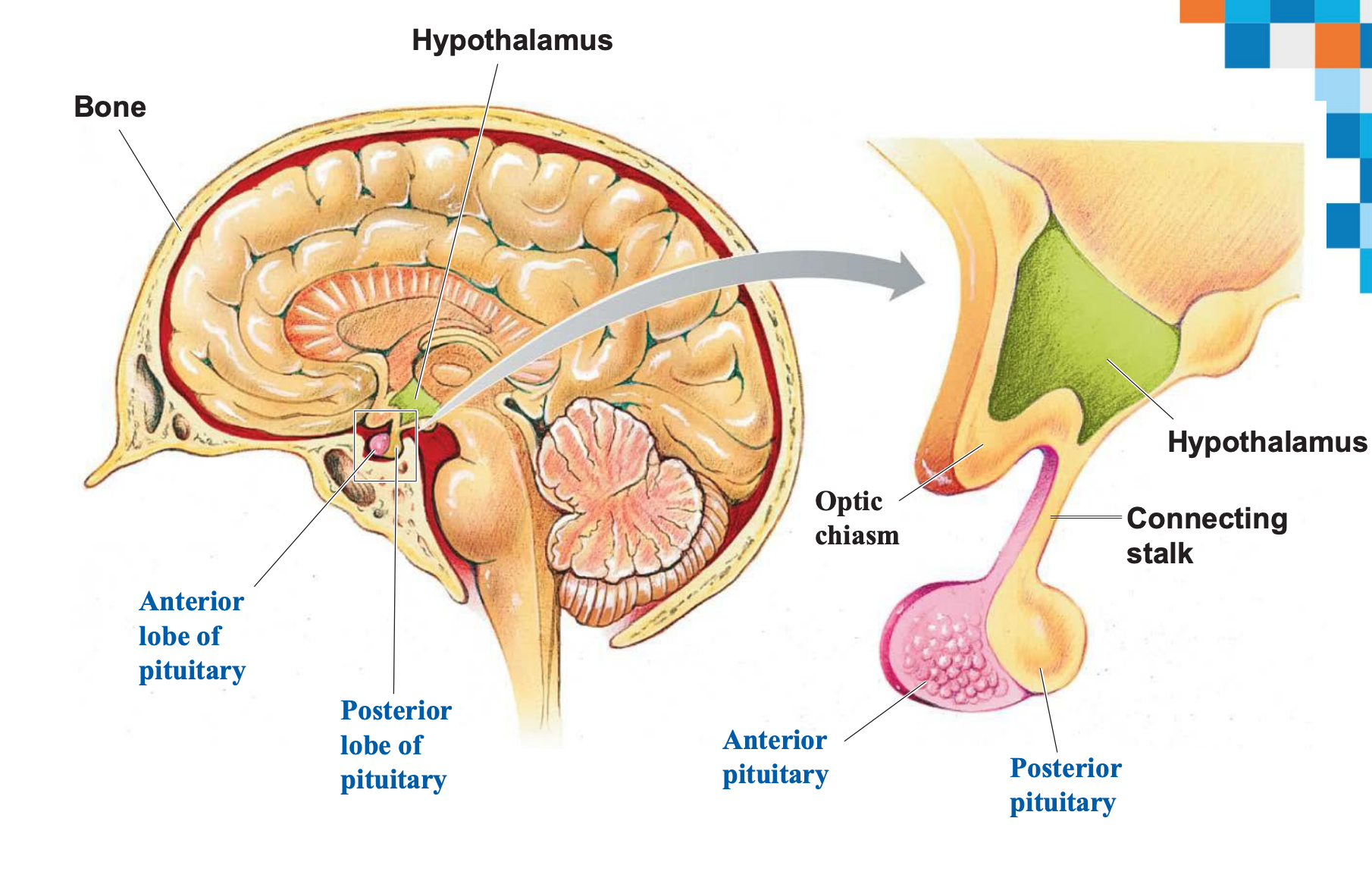
The Hypothalamus
The hypothalamus is connected to the pituitary gland (hypophysis) via a stalk called the infundibulum.
It has 2 parts:
Nerve tissues (axons) expanding into the neurohypophysis (posterior pituitary).
The hypophyseal portal system (blood vessels).
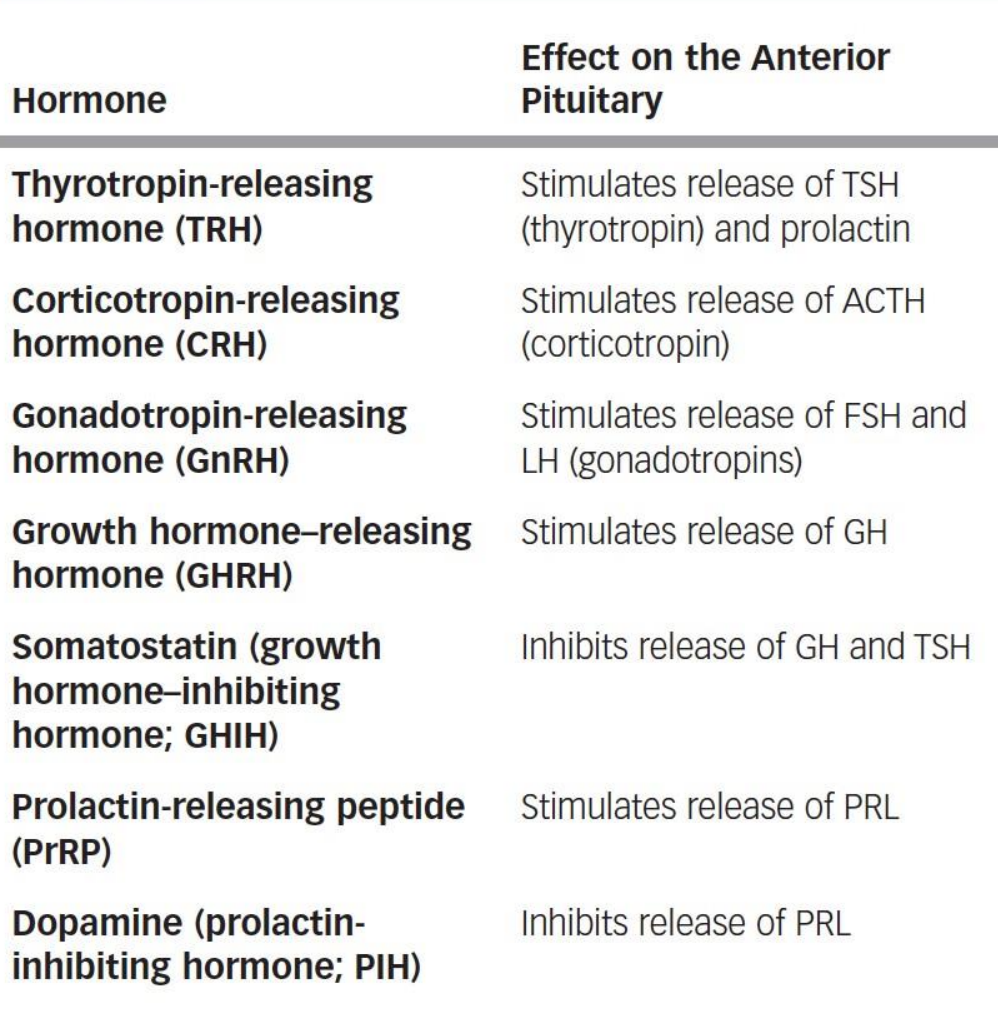
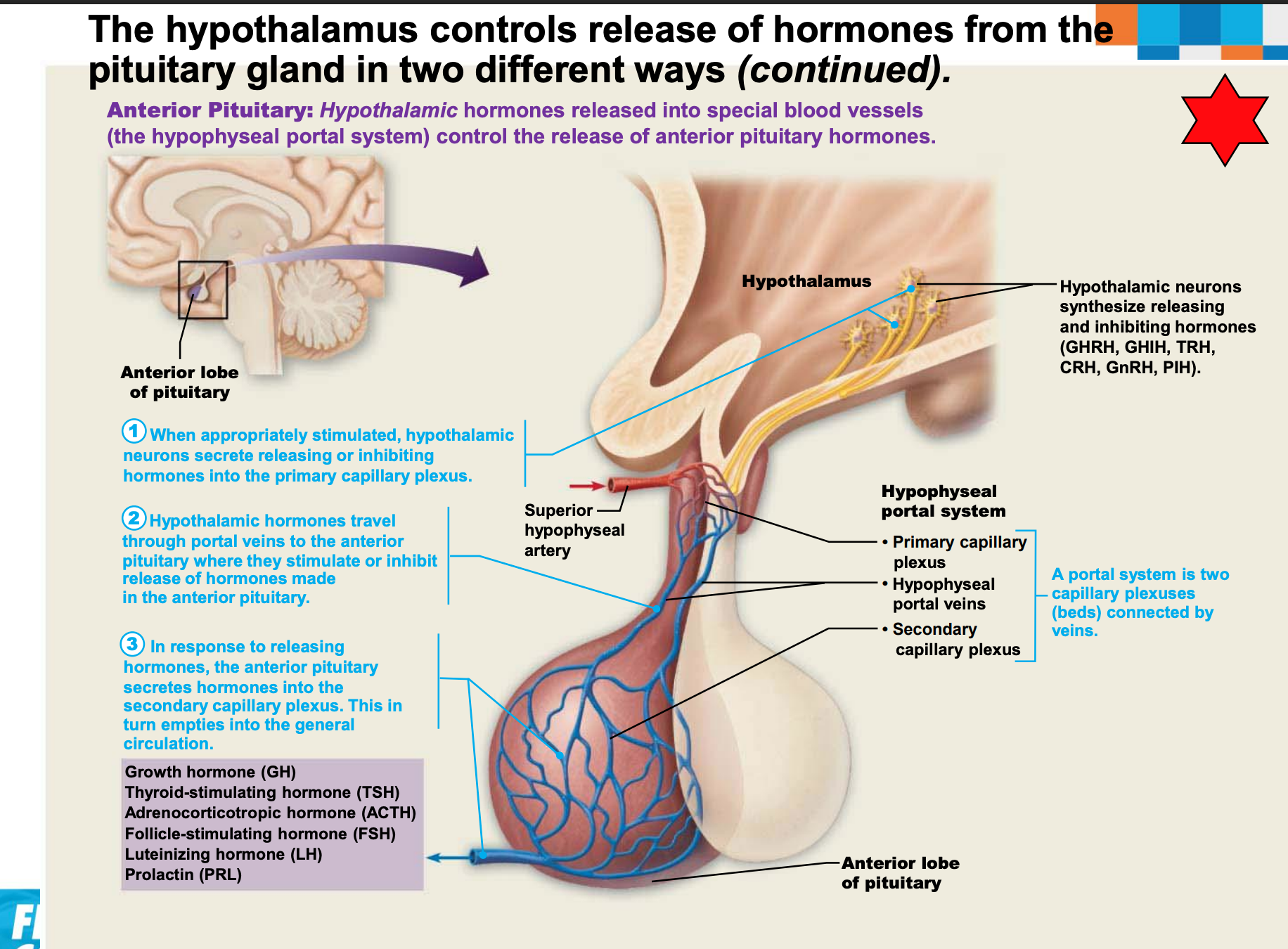
Hypothalamic hormones released into special blood vessels (the hypophyseal portal system) control the release of anterior pituitary hormones.
The Pituitary Gland
The pituitary secretes at least eight major hormones.
It has two major lobes:
Posterior pituitary: composed of neural tissue that secretes neurohormones.
The posterior lobe, along with the infundibulum, makes up the neurohypophysis.
Anterior pituitary (adenohypophysis): consists of glandular tissue.
Posterior Pituitary
The posterior lobe is neural tissue derived from a down-growth of the brain.
Secretes two hormones - oxytocin and ADH.
Hormones are made in neurons in the hypothalamus, transported and stored in axon terminals in the posterior pituitary, and are released into the blood when neurons fire.
Each is composed of nine amino acids.
Almost identical but differ in two amino acids.
Oxytocin
Strong stimulant of uterine contractions released during childbirth.
Also acts as a hormonal trigger for milk ejection.
Both are positive feedback mechanisms.
Antidiuretic Hormone (ADH) (also called Vasopressin)
The hypothalamus contains osmoreceptors that monitor solute concentrations.
If the concentration is too high, the posterior pituitary is triggered to secrete ADH.
Targets kidney tubules to reabsorb more water to inhibit or prevent urine formation.
Release is also triggered by low blood pressure.
Inhibited by alcohol and diuretics.
High concentrations cause vasoconstriction, so it's also called vasopressin.
Anterior Pituitary
The hypothalamus controls the release of hormones from the pituitary gland in two different ways:
Hypothalamic hormones released into special blood vessels (the hypophyseal portal system) control the release of anterior pituitary hormones.
Anterior Pituitary Hormones
Growth hormone (GH)
Thyroid-stimulating hormone (TSH)
Adrenocorticotropic hormone (ACTH)
Follicle-stimulating hormone (FSH)
Luteinizing hormone (LH)
Prolactin (PRL)
Pituitary-Hypothalamic Relationships
The anterior lobe is glandular tissue derived from an out-pocketing of oral mucosa.
Vascularly connected to the hypothalamus via the hypophyseal portal system consisting of:
Primary capillary plexus
Hypophyseal portal veins
Secondary capillary plexus
The hypothalamus secretes releasing and inhibiting hormones to the anterior pituitary to regulate hormone secretion.
Anterior Pituitary Hormones
All six hormones are peptide hormones.
All but growth hormone (GH) activate target cells via the cAMP second-messenger system.
All but two are tropic hormones (tropins) that regulate the secretion of other hormones:
Prolactin (PRL)
Growth hormone (GH)
Thyroid-stimulating hormone (TSH) (tropic)
Adrenocorticotropic hormone (ACTH) (tropic)
Follicle-stimulating hormone (FSH) (tropic)
Luteinizing hormone (LH) (tropic)
Prolactin (PRL)
Stimulates milk production in females; the role in males is not well understood.
Regulation is primarily controlled by prolactin-inhibiting hormone (PIH), which is dopamine.
PIH prevents the release of PRL until needed (lactation).
Increased estrogen levels stimulate PRL.
The reason behind breast swelling and tenderness during the menstrual cycle.
Blood levels rise toward the end of pregnancy.
Suckling stimulates PRL release and promotes continued milk production.
Growth Hormone (GH)
Is produced by the anterior pituitary.
Has direct actions on metabolism and indirect growth-promoting actions.
Direct actions on metabolism:
Glucose-sparing actions decrease the rate of cellular glucose uptake and metabolism (spares glucose for the brain).
Triggers the liver to break down glycogen into glucose.
Increases blood levels of fatty acids for use as fuel.
Encourages cellular protein synthesis.
Indirect actions on growth:
GH triggers the liver, skeletal muscle, and bone to produce insulin-like growth factors (IGFs).
IGFs then stimulate:
Cellular uptake of nutrients used to synthesize DNA and proteins needed for cell division.
Formation of cartilage and deposition of bone matrix.
GH stimulates most cells to enlarge and divide, but major targets are bone and skeletal muscle.
Regulation of secretion:
GH release or inhibition is chiefly regulated by hypothalamic hormones.
Growth hormone–releasing hormone (GHRH) stimulates GH release.
Triggered by low blood GH or glucose, or high amino acid levels.
Growth hormone–inhibiting hormone (GHIH) (somatostatin) inhibits release.
Triggered by an increase in GH and IGF levels.
Ghrelin (hunger hormone) also stimulates GH release.
Thyroid-Stimulating Hormone (TSH)
Stimulates the normal development and secretory activity of the thyroid gland.
Release is triggered by thyrotropin-releasing hormone from the hypothalamus.
Inhibited by rising blood levels of thyroid hormones that act on both the pituitary and the hypothalamus = negative feedback.
Adrenocorticotropic Hormone (ACTH)
ACTH stimulates the adrenal cortex to release corticosteroids.
Regulation of ACTH release:
Triggered by hypothalamic corticotropin-releasing hormone (CRH) in a daily rhythm.
Highest levels are in the morning.
Internal and external factors that alter the release of CRH include fever, hypoglycemia, and stressors.
Gonadotropins (FSH and LH)
Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) are secreted by the anterior pituitary.
FSH stimulates the production of gametes (egg or sperm).
LH promotes the production of gonadal hormones.
In females, LH helps mature follicles of the egg, triggers ovulation, and releases estrogen and progesterone.
In males, LH stimulates the production of testosterone.
LH and FSH are both absent from the blood in prepubertal boys and girls.
Regulation of gonadotropin release:
Triggered by gonadotropin-releasing hormone (GnRH) during and after puberty.
Suppressed by gonadal hormones (feedback).
Hormone Summary
Hormone | Secreted From | Targets | Action(s) at Target Site |
|---|---|---|---|
GH | anterior pituitary | bone, muscle, fat | growth of tissues, protein synthesis, lipolysis, increase blood glucose |
PRL | anterior pituitary | mammary glands | Stimulate milk production after birth |
TSH | anterior pituitary | thyroid | Stimulates secretion of thyroid hormones |
ACTH | anterior pituitary | adrenal cortex | Stimulates secretion of cortisol and androgens |
LH | anterior pituitary | males: testes; females: ovaries | males: testosterone secretion females: ovulation |
FSH | anterior pituitary | males: testes; females: ovaries | males: sperm production females: follicle and ovum maturation |
ADH | posterior pituitary | kidney | reabsorption of water |
Oxytocin | posterior pituitary | uterine smooth muscle | contraction during labor |