Exam 3
CHAPTER 10: STRESS
1. What role does the autonomic nervous system (ANS) play in the response to and effects of stress on the body? (p. 155-156 Varcarolis 9th ed.)
Fight-or-Flight Response:
Acute stress response
the body’s way of preparing for a situation an individual perceives as a threat. This response results in increased blood pressure, heart rate, respiration, and cardiac output.
General Adaptation Syndrome
Selye (1936) defined stress as “a nonspecific response of the body to any demand for change.” He incorporated Cannon’s fight-or-flight response into an expanded theory of stress known as the general adaptation syndrome (GAS). While Cannon focused on the sympathetic nervous system, Selye included the hypothalamus-pituitary-adrenal axis in his research.
GAS occurs in 3 stages
Alarm
Resistance
Exhaustion
Bad Stress Versus Good Stress?
individuals become energized by both negative and positive events.
Distress is a negative, draining energy that results in anxiety, depression, confusion, helplessness, hopelessness, and fatigue
Eustress normal physiological workings of an organism. It is a positive energy that motivates individuals and results in feelings of happiness, hopefulness, and purposeful movement.
2. How does acute stress and chronic stress effect the body? (p. 155-156 Varcarolis 9th ed.)]9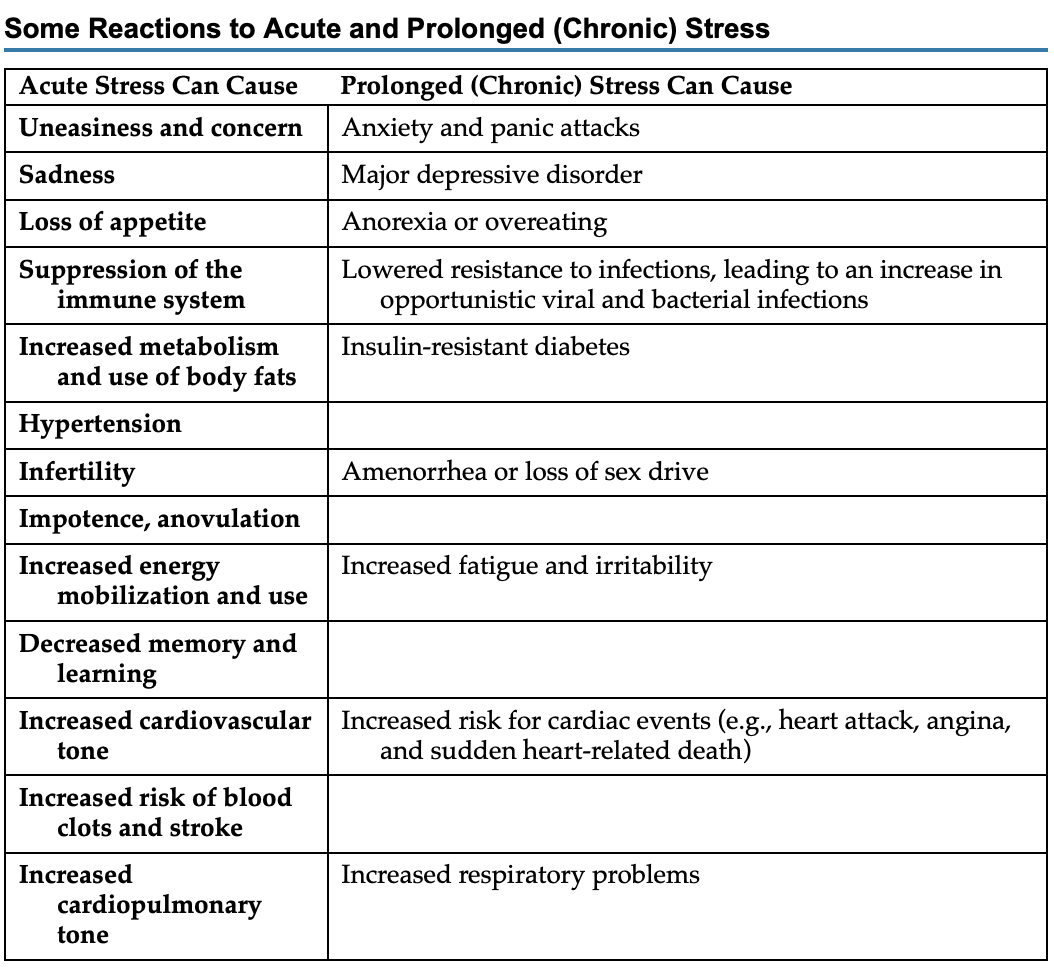
2. What are potential causes of stress and stressors? (pp. 157-159 Varcarolis 9th ed.)
Many situations, such as emotional arousal, fatigue, fear, humiliation, loss of blood, extreme happiness, or unexpected success, are capable of producing stress and triggering the stress response.
Stressors can be divided into two broad categories: physiological and psychological.
Physiological stressors include environmental conditions such as trauma and excessive cold or heat, and physical conditions such as infection, hemorrhage, hunger, and pain. Psychological stressors include such events as divorce, loss of a job, unmanageable debt, the death of a loved one, retirement, and fear of a terrorist attack. Psychological stressors also include changes we consider positive, such as marriage, the arrival of a new baby, or unexpected success.
3. What should the nurse assess for in the patient’s ability to manage stress? (pp. 157-159, 161 Varcarolis 9th ed.).
Health-sustaining habits (e.g., medical adherence, proper diet, relaxation, pacing one’s energy)
Life satisfaction (e.g., work, family, hobbies, humor, spiritual solace, arts, nature)
Social support
Effective and healthy responses to stress
4. What technique or treatment has the potential to immediately reduce stress levels? (pp. 161-162 Varcarolis 9th ed.; Chapter 10 Stress power point).
deep-breathing exercises: The first part focuses on abdominal breathing, while the second part helps patients interrupt trains of thought, thereby quieting mental noise. With increasing skill, breathing becomes a tool for dampening the cognitive processes likely to induce stress and anxiety reactions.
5. Understand how exercise, cognitive reframing, journaling, and humor help with relaxation. pp. 163-164 Varcarolis 9th ed.)
Physical Exercise: Physical exercise can lead to protection from the harmful effects of stress on both physical and mental states.Spending at least 3 hours a week participating in any activity, such as walking, running, or biking, reduces the risk for depression.
Cognitive Reframing: Goal of CR is to change an individual’s perceptions of stress by reassessing a situation and replacing irrational beliefs. For example, the thought “I can’t pass this course” is replaced with a more positive self-statement, “If I choose to study for this course, I will increase my chances of success.
Journaling: is an extremely useful and surprisingly simple method of identifying stressors. It is a technique that can ease worry and obsession, help identify hopes and fears, increase energy levels and confidence, and facilitate the grieving process. Keeping an informal diary of daily events and activities can reveal surprising information on sources of daily stress. Simply noting which activities put a strain on energy and time, which trigger anger or anxiety, and which precipitate a negative physical experience (e.g., headache, backache, fatigue) can be an important first step in stress reduction.
Humor: use of humor as a cognitive approach is a good example of how a stressful situation can be “turned upside down.
6. Be familiar with the stress managing relaxation techniques: biofeedback, deep-breathing, progressive, relaxation, meditation, and mindfulness. (pp. 161-163; p. 164 Box 10.5 Varcarolis 9th ed.).
Biofeedback: provides immediate and exact information regarding muscle activity, brain waves, skin temperature, heart rate, blood pressure, and other bodily functions. Indicators of the particular internal physiological process are detected and amplified by a sensitive recording device. An individual can achieve greater voluntary control over phenomena once considered to be exclusively involuntary by knowing whether a somatic activity is increasing or decreasing. example Exercise trackers and smartwatches
Deep-breathing exercises: quick fix to calm down. Breathing exercises are simple and easy to remember, even when anxiety begins to escalate. This technique involves focusing on taking slow, deep, and even breaths.
One breathing exercise that has proved helpful for many people coping with anxiety and anxiety disorders has two parts The first part focuses on abdominal breathing, while the second part helps patients interrupt trains of thought, thereby quieting mental noise.
Progressive relaxation: This technique can be done without any external gauges or feedback and can be practiced almost anywhere by anyone.
The premise behind progressive relaxation is that because anxiety results in tense muscles, one way to decrease anxiety is to relax muscle contraction. This is accomplished by deliberately tensing groups of muscles (beginning with feet and ending with face or vice versa) as tightly as possible for about 8 seconds and then releasing the tension you have created.
Meditation: Meditation is a discipline for training the mind to develop greater calm and then using that calm to bring penetrative insight into one’s experience. Meditation can be used to help people tap into their deep inner resources for healing, calm their minds, and help them operate more efficiently in the world. It can help people develop strategies to cope with stress, make sensible adaptive choices under pressure, and feel more engaged in life.
Meditation elicits a relaxation response by creating a hypometabolic state of quieting the sympathetic nervous system. Some people meditate using a visual object or a sound to help them focus. Others may find it useful to concentrate on their breathing while meditating.
Mindfulness: a centuries-old form of meditation that dates back to Buddhist tradition. Mindfulness is based on two ways our brains work. One is a default network that includes the medial prefrontal cortex and memory regions such as the hippocampus. In this state, we operate on a sort of mental autopilot or “mind wandering.” You are thinking about what to make for dinner or how your hair looks and are continually compiling the narrative of your life and the people you know. This type of thinking tends to be dominant.
The other network is the direct experience network which is the focus of mindfulness. Several areas of the brain are activated in this state. The insular cortex is active and makes us aware of bodily sensations and a sense of self. The anterior cingulate cortex is active and is central to attention and focuses us on what is happening around us. In this state, you are in tune with your environment, live in the moment, and take a break from planning, strategizing, and setting goals
CHAPTER 15: ANXIETY AND OCD
1. Be able to differentiate between mild, moderate, severe, and panic level anxiety. (pp. 269-270 (Table 15.1) Varcarolis 9th ed.; pp 119-120 Varcarolis Care manual 7th ed.)
Mild anxiety occurs in the normal experience of everyday living and allows an individual to perceive reality in sharp focus. A person experiencing a mild level of anxiety sees, hears, and grasps more information, and problem-solving becomes more effective. Physical symptoms may include slight discomfort, restlessness, irritability, or mild tension-relieving behaviors (e.g., nail-biting, foot or finger tapping, fidgeting).
Moderate Anxiety As anxiety increases, the perceptual field narrows, and some details are excluded from observation. The person experiencing moderate anxiety sees, hears, and grasps less information and may demonstrate selective inattention, where only certain things in the environment are seen or heard unless they are pointed out. The ability to think clearly is hampered, but learning and problem solving can still take place, though not at an optimal level. SNS symptoms kick in and individual may experience tension, a pounding heart, increased pulse and respiratory rates, perspiration, and mild somatic symptoms (e.g., gastric discomfort, headache, urinary urgency). Voice tremors and shaking may be noticed
Severe anxiety A person with severe anxiety may focus on one particular detail or on many scattered details and have difficulty noticing what is going on in the environment, even when another person points it out. Learning and problem solving are not possible at this level, and the person may be dazed and confused. Behavior is automatic and aimed at reducing or relieving anxiety. Somatic symptoms (e.g., headache, nausea, dizziness, insomnia) often increase. Trembling and a pounding heart are common, and the person may experience hyperventilation and a sense of impending doom or dread.
Panic: Panic is the most extreme level of anxiety and results in markedly dysregulated behavior. Someone in a state of panic is unable to process what is going on in the environment and may lose touch with reality. The behavior that results may be manifested as pacing, running, shouting, screaming, or withdrawal. Hallucinations, which are false sensory perceptions, such as seeing something that is not really there or hearing voices, may be experienced. Physical behavior may become erratic, uncoordinated, and impulsive. Automatic behaviors are used to reduce and relieve anxiety, although such efforts may be ineffective
2. Review patient assessment, interventions, and rationale for client experiencing moderate level anxiety. (pp. 278, 280 (Table 15.9 Varcarolis 9th ed; pp. 131-132 Varcarolis Care Planning Manual 7th ed).
A person experiencing a mild to moderate level of anxiety is still able to solve problems. However, the ability to concentrate decreases as anxiety increases. A patient can be helped to focus and solve problems when you use specific nursing communication techniques such as asking open-ended questions, giving broad openings, and exploring and seeking clarification.
Closing off topics of communication and bringing up irrelevant topics can increase a person’s anxiety, making the nurse, not the patient, feel better.
Reducing the patient’s anxiety level and preventing escalation to more distressing levels can be aided by providing a calm presence, recognizing the anxious person’s distress, and being willing to listen. Evaluation of effective past coping mechanisms is also useful. Often, you can help the patient consider alternatives to problem situations and offer activities that may temporarily relieve feelings of inner tension
3. Be familiar with the defense mechanisms: regression, undoing, and splitting. (p. 271 Table 15.2 Varcarolis 9th ed).
Regression is reverting to an earlier, more primitive and childlike pattern of behavior that may or may not have been exhibited previously.
adaptive: A 4-year-old boy with a new baby brother temporarily starts sucking his thumb and asking for a baby bottle.
maladaptive: A man who loses a promotion starts complaining to others, hands in sloppy work, misses appointments, and comes in late for meetings.
Undoing is when a person makes up for a regrettable act or communication.
Adaptive: After flirting with her male secretary, a woman brings her husband tickets to a concert he wants to see.
Maladaptive:A man with rigid, moralistic beliefs and repressed sexuality is driven to wa sh his hands to gain composure when he is around attractive women.
Splitting is the inability to integrate the positive and negative qualities of oneself or others into a cohesive image.
Maladaptive: A 26-year-old woman initially values her acquaintances yet invariably becomes disillusioned when they turn out to have flaws.
4. What is claustrophobia, germaphobia or mysophobia, monophobia, and agoraphobia? (p. 272 Table 15.4 Varcarolis 9th ed).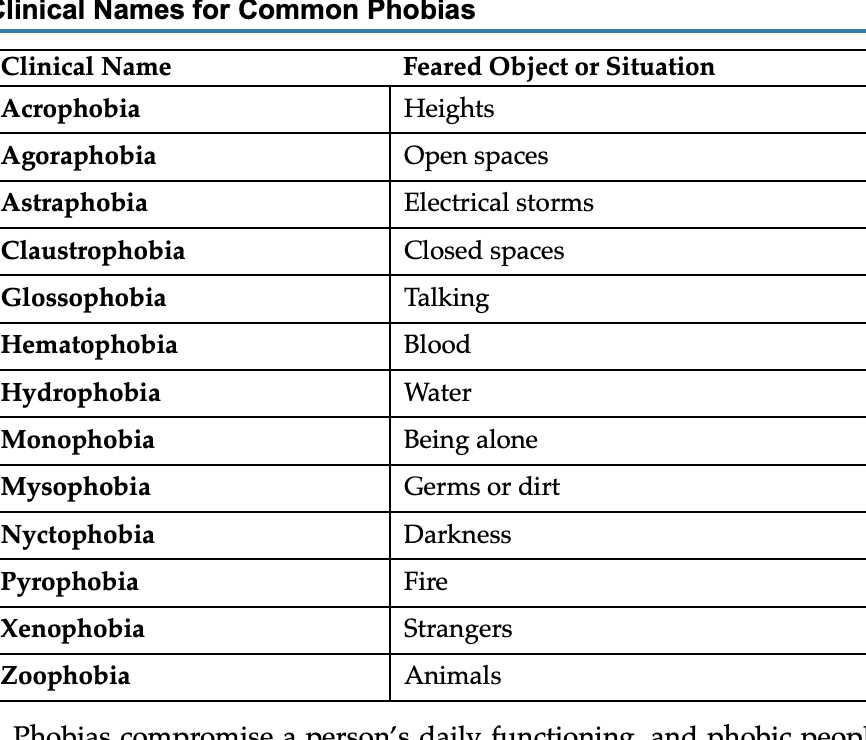
5. Care planning for clients with an anxiety disorder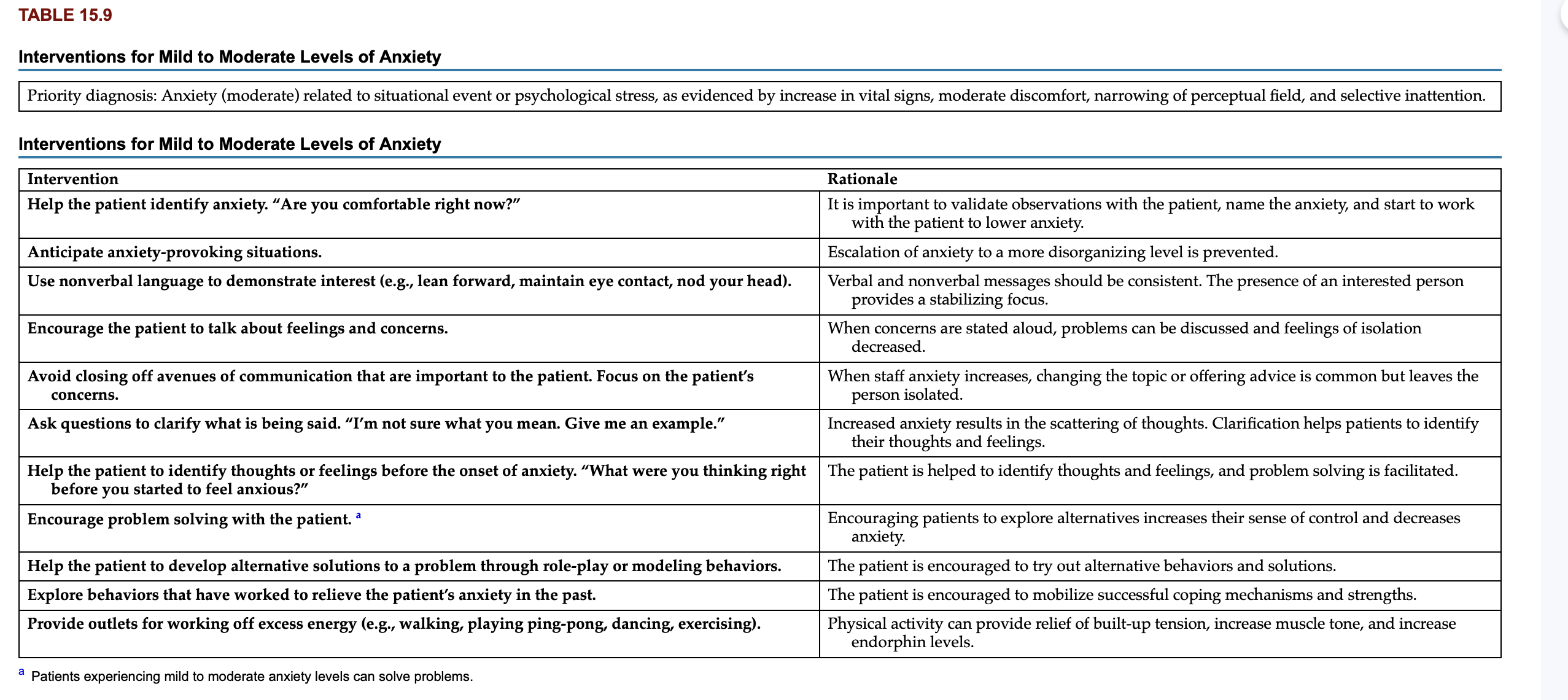
 6. Be familiar with generalized anxiety disorder.
6. Be familiar with generalized anxiety disorder.
excessive worrying, sleep disturbance is common, and fatigue is a noticeable side effect of this sleep deprivation.
Common worries in generalized anxiety disorder are inadequacy in interpersonal relationships, job responsibilities, finances, and health of family members. Because of this worry, huge amounts of time are spent in preparing for activities. Putting things off and avoidance are key symptoms and may result in lateness or absence from school or employment and overall social isolation. Family members and friends are overtaxed as the person with this disorder seeks continual reassurance and perseverates about meaningless details.
7. Indications for administering alprazolam (Xanax)?
generalized anxiety disorder and panic disorder
8. Peak action of benzodiazepines.
quick onset
9. What are the uses for alprazolam (Xanax).
10. What is gamma aminobutyric acid (GABA) role in anxiety.
GABA slows neuron activity which plays a role of lowering anxiety and also effects memory.
CHAPTER 16: TRAUMA AND DISSOCIATIVE DISORDERS
1. What is disinhibited social engagement disorder? (pp. 294-295 V9th ed.)
Children with this disorder demonstrate no normal fear of strangers. They seem to be unfazed in response to separation from a primary caregiver. Younger children may allow unfamiliar people to pick them up, feed them, or play with them. These children tend to be overly friendly and are usually willing, or even eager, to go with someone they do not know.
2. Nursing assessment for acute stress disorder?
A nursing assessment for acute stress disorder is similar to that of PTSD. One key difference is that individuals who have recently experienced trauma may have more difficulty sharing their symptoms. Furthermore, this population is more likely to experience derealization, which makes a person less secure in the environment. These problems result in a need for a non-rushed and reassuring approach to assessment.
3. What is dissociation? (pp. 295 V9th ed.)
occur after significant adverse experiences and traumas. The predominant response is a severe interruption of consciousness. Dissociation is an unconscious defense mechanism that protects the individual against overwhelming anxiety through an emotional separation. However, this separation results in disturbances in memory, consciousness, self-identity, and perception.
Dissociation may be protective in that it decreases the immediate distress of the trauma and also continues to protect the individual from full awareness of the disturbing event.
4. What are the signs and symptoms of PTSD in children, adolescents, and adults? (pp. 295-300 V9th ed.)
Essential assessment data include posttraumatic symptoms such as:
• Nightmares and night terrors
• Intrusive traumatic thoughts and memories
• Re-experiencing or flashbacks
• Numbing
• Avoidance of stimuli associated with the traumatic event
Another area of assessment includes the presence of self-injurious behaviors due to anxiety and negative emotional states. Children and adolescents may experience somatic symptoms such as headaches, stomachaches, or pain; memory problems include amnesia, forgetfulness, difficulty concentrating, or trance states. The child may disturbingly re-enact the trauma in play.
5. What is acute stress disorder? (p. 303 V9th ed.)
Acute stress disorder (ASD) may develop after exposure to a highly traumatic event, such as those listed in the prior section on PTSD. ASD is diagnosed 3 days to 1 month after the traumatic event. To be diagnosed with ASD, the individual must display 8 out of the following 14 symptoms either during or after the traumatic event:
• A subjective sense of numbing
• Derealization (a sense of unreality related to the environment)
• Inability to remember at least one important aspect of the event
• Intrusive distressing memories of the event
• Recurrent distressing dreams
• Feeling as if the event is recurring
• Intense prolonged distress or physiological reactivity
• Avoidance of thoughts or feelings about the event
• Sleep disturbances
• Hypervigilance
• Irritable, angry, or aggressive behavior
• Exaggerated startle response
• Agitation or restlessness
6. Be able to distinguish between depersonalization and derealization. (p. 306 V9th ed.)
Depersonalization is an extremely uncomfortable feeling of being an observer of one’s own body or mental processes. Feelings of unreality, detachment, or unfamiliarity with parts of self or the whole self are features of this disorder. A patient may feel detached from his entire self, aspects of himself, including feelings, thoughts, body parts, or sensations.
derealization, the focus is on the outside world. It is the recurring feeling that one’s surroundings are unreal or distant. The person may feel like she is walking around in a fog, bubble, or dream. It may feel like there is an invisible veil between her and the rest of the world. Visual distortions are manifested in blurriness, changes in the visual field (widened or narrowed), and altered size of objects. Auditory distortions include the muting or heightening of sound
7. DSM 5 diagnosis criteria for dissociative identity disorder (DID)? (pp. 306-307 V9th ed.)
For a diagnosis of dissociative identity disorder to be made, medical and neurological illnesses, substance use, and other psychiatric disorders are ruled out. The assessment should include objective data from physical examination, EEG, imaging studies, and specific questions to identify dissociative symptoms.
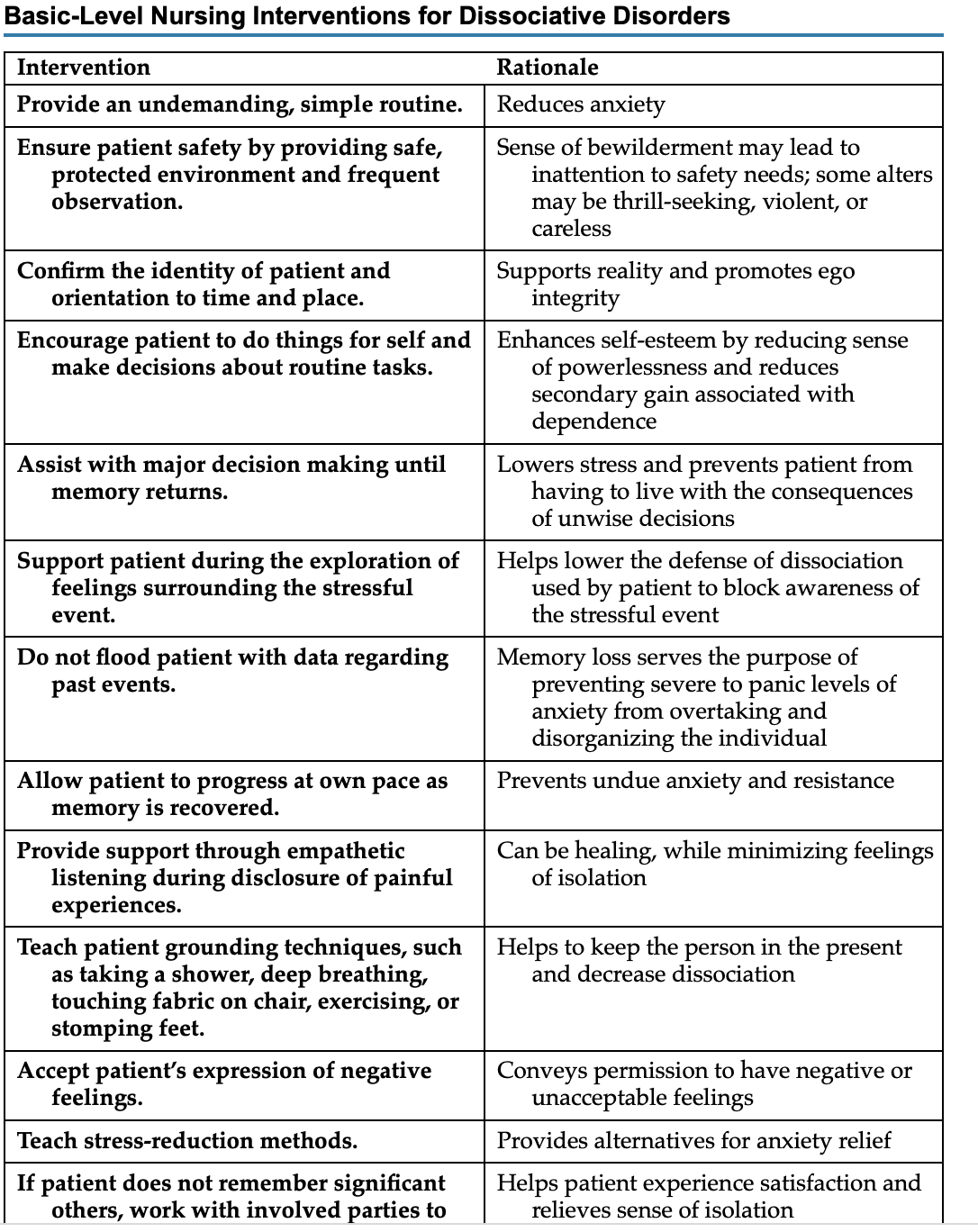
8. Nursing interventions for DID?
9. What is the primary and alter personalities in DID? (pp. 306-307 V9th ed.)
Dissociative identity disorder is characterized by at least two identity states: one is a state or personality that functions on a daily basis and blocks access and responses to traumatic memories. A second or more state, referred to as an alter state, is fixated on traumatic memories. These separate states are due to the activation of increased endogenous opioids that prevent high arousal states at times of severe threat . This response is mediated by the dorsal vagal parasympathetic response, such as occurs in mammals who freeze when threatened and play dead.
Chapter 22 Substance-Related and Addictive Disorders
1. DSM5 criteria for substance abuse?
The APA defines a substance use disorder as a pathological use of a substance that leads to a disorder of use. Symptoms fall into four major groups:
1. Impaired control
2. Social impairment
3. Risky use
4. Physical effects (i.e., intoxication, tolerance, and withdrawal)
2. Be able to distinguish between substance dependency, abuse, addiction, tolerance, withdrawal.
Substance dependency: physiological or psychological reliance on a substance in which the body os accustomed to its presence
Subtance abuse:excessive or improper use of substance which leads to negativie consequence
Addiction is a chronic medical condition with roots in the environment, neurotransmission, genetics, and life experiences
Tolerance occurs when a person no longer responds to the drug in the way that the person initially responded. It takes a higher dose of the drug to achieve the same level of response achieved initially.
Withdrawal is a set of physiological symptoms that occur when a person stops using a substance. Withdrawal is specific to the substance being used, and each substance will have its own characteristic syndrome.
1. What is the purpose of the Clinical Institute Withdrawal Assessment revised (CIWA-Ar)? (Chapter 22 power point)
it is used to quantify the severity of alcohol withdrawal syndrome
monitor and medicate pt going through withdrawal
Measures withdrawal symptom
score of 8 or fewer- mild withdrawal
score of 9-15 moderate
score greater than 15 severe withdrawal
2. What is the purpose of the Clinical Opiate Withdrawal Scale (COWS)? (Chapter 22 power point)
Assist in tailoring opiod treatment
determines the severity of the opiod withdrawal
inpt and outpt setting
monitor how symptoms change over time during treatment uses 11 common symptoms of opioid withdrawal and measures their severity
3. What medications are used for alcohol withdrawal? (p. 419 Varcarolis 9th ed)
Chlordiazepoxide (Librium) is useful for tremulousness and mild to moderate agitation.
Diazepam (Valium) given intravenously is a common treatment for withdrawal seizures
Oral diazepam (Valium) may be useful in the symptomatic relief of acute agitation, tremor, impending or acute DTs, and hallucinosis. Chlordiazepoxide (Librium) may keep your patient out of danger. However, once delirium appears, intravenous lorazepam (Ativan) is used to treat these severe symptoms. Seclusion may be necessary. Dehydration, often exacerbated by diaphoresis and fever, can be corrected with oral or intravenous fluids.
4. What is delirium tremens (DTs)? ((p. 419 Varcarolis 9th ed.)
Alcohol withdrawal delirium, also known as delirium tremens (DTs), is a medical emergency that can result in the death in 20% of untreated patients, usually as a result of medical problems such as pneumonia, renal disease, hepatic insufficiency, or heart failure.
Alcohol withdrawal delirium may happen anytime in the first 72 hours. Autonomic hyperactivity may result in tachycardia, diaphoresis, fever, anxiety, insomnia, and hypertension. Delusions and visual and tactile hallucinations are common in alcohol withdrawal delirium.
Symptoms associated with alcohol withdrawal.
tremulousness: shakes or jitters
agitation
lack of appetite
nausea
vomiting
insomnia
impaired cognition
mild perceptual changes
Both systolic and diastolic blood pressure increases
pulse and body temperature increases
5. Be familiar with Wernicke-Korsakoff Syndrome. (pp. 419-420 Varcarolis 9th ed; see Chapter 22 power point)
people who are heavy users of alcohol can suffer from short term of memory disturbance
One memory-reducing problem is Wernicke’s (alcoholic) encephalopathy, an acute and reversible condition. Another problem is Korsakoff’s syndrome, a chronic condition with a recovery rate of only about 20%. The pathophysiological connection between the two problems is a thiamine deficiency, which may be caused by poor nutrition associated with alcohol use or by the malabsorption of nutrients.
Wernicke’s encephalopathy is characterized by altered gait, vestibular dysfunction, confusion, and several ocular motility abnormalities (horizontal nystagmus, lateral orbital palsy, and gaze palsy). These eye-focused signs are bilateral but not necessarily symmetrical. Sluggish reaction to light and anisocoria (unequal pupil size) are also symptoms. Wernicke’s encephalopathy may clear up within a few weeks or may progress into Korsakoff’s syndrome, the more severe and chronic version of this problem.
Wernicke’s encephalopathy responds rapidly to large doses of intravenous thiamine two to three times daily for 1 to 2 weeks. Treatment of Korsakoff’s syndrome is also thiamine for 3 to 12 months. Most patients with Korsakoff’s syndrome never fully recover, although cognitive improvement may occur with thiamine and nutritional support
Treatment for Wernicke’s encephalopathy, Korsakoff’s syndrome, and Wernicke-Korsakoff Syndrome (pp. 419-420 Varcarolis 9th ed; see Chapter 22 power point)
Wernicke’s encephalopathy responds rapidly to large doses of intravenous thiamine two to three times daily for 1 to 2 weeks. Treatment of Korsakoff’s syndrome is also thiamine for 3 to 12 months. Most patients with Korsakoff’s syndrome never fully recover, although cognitive improvement may occur with thiamine and nutritional support.
6. What medication is used for opiate overdose? (p. 413 Varcarolis 9th ed)
Treatment for an overdose begins with promoting breathing by aspirating secretions, inserting an airway, and mechanical ventilation. Naloxone (Narcan), a specific opioid antagonist, has FDA approval for opioid overdose and can be given intranasally, intramuscularly, subcutaneously, or intravenously.
Symptoms of Wernicke’s encephalopathy, Korsakoff’s syndrome, and Wernicke-Korsakoff Syndrome (pp. 419-420 Varcarolis 9th ed; see Chapter 22 power point)
altered gait
vestibular dysfunction
confusion
several ocular motility abnormalities (horizontal nystagmus, lateral orbital palsy, and gaze palsy).
These eye-focused signs are bilateral but not necessarily symmetrical.
Sluggish reaction to light and anisocoria (unequal pupil size)
7. What is methadone (Dolophine, Methadone), clonidine (Catapres), and buprenorphine used to treat? (pp. 413-414 Varcarolis 9th ed)
Methadone (Dolophine, Methadose) is a synthetic narcotic opioid. It is used to decrease the painful symptoms of opiate withdrawal. It also blocks the euphoric effects of opiate drugs such as heroin, morphine, and codeine, as well as semisynthetic opioids like oxycodone and hydrocodone.
Clonidine (Catapres), an alpha agonist antihypertensive, is often used to reduce the symptoms of opioid withdrawal. By blocking neurotransmitters that trigger sympathetic nervous system activity, clonidine eases sweating, hot flashes, watery eyes, and restlessness. This drug also decreases anxiety and may even shorten the detox process.
Buprenorphine is also used to help people reduce or quit opiates. Buprenorphine is an opioid partial agonist. Like opioids, it produces effects such as euphoria or respiratory depression, but these effects are weaker than those of drugs such as heroin and methadone.
2. Signs and symptoms of opioid withdrawal?
mood dysphoria
nausea,
vomiting,
diarrhea,
muscle aches,
fever
insomnia.
Other classic symptoms of withdrawal are
lacrimation (watery eyes),
rhinorrhea (runny nose),
pupillary dilation
yawning.
The symptom of piloerection (bristling of hairs) or gooseflesh is the origin of the term cold turkey for the abstinence syndrome.
Males may experience sweating and spontaneous ejaculations while awake.
3. What is the purpose of Al-Anon.
Anyone with the desire to quit drinking or using substances is welcome to attend meetings. Individuals learn how to be sober through the support of other members and the 12 steps.
CHAPTER 24: PERSONALITY DISORDERS (ATI Chapter 16)
1. What are personality disorders? (pp. 451-452 Varcarolis 9th ed.)
People with these disorders have difficulty recognizing or owning that their difficulties are problems of their personalities. They may truly believe that the problems originate outside of themselves.
2. Be able to distinguish between the 10 personality disorders and 3 clusters. (pp. 452-458, 464 Varcarolis 9th ed.; Personality Disorder Power Point). KNOW SIGNS AND SYMPTOMS OF ALL 10 AND THE 3 CLUSTERS.
Cluster A: Behaviors described as odd or eccentric
Paranoid personality disorder
Schizoid personality disorder
Schizotypal personality disorder
Cluster B: Behaviors described as dramatic, emotional, or erratic
Borderline personality disorder
Narcissistic personality disorder
Histrionic personality disorder
Antisocial personality disorder
Cluster C: Behaviors described as anxious or fearful
Avoidant
Dependent
Obsessive-compulsive
3. How is splitting used by clients with borderline personality disorder (pp. 458 V9th ed.)
It involves an inability to view both positive and negative aspects of others as part of a whole, which results in viewing someone as either a wonderful person or a horrible person. This kind of dichotomous thinking and coping behavior is believed to be partly a result of the person’s failed experiences with adult personality integration. It is likely influenced by exposure to earlier psychological, sexual, or physical trauma. For example, individuals with borderline personality disorder may idealize other people (e.g., friends, lovers, healthcare professionals) at the start of new relationships, hoping that these people will meet all of their needs. However, at the first disappointment or frustration, the individual’s status quickly shifts to one of devaluation, and the other person is despised.
4. What medications are used to treat personality disorders?
CBT
Antidepressant-SSRI
antianxiety
antipsychotics
5. What is first line treatment for personality disorders?
Psychotherapy-CBT
CHAPTER 30: DEATH, DYING, AND GRIEVING
1. What are the 5 stages of grief and characteristics of each?
Kübler-Ross (1973) identified distinctive phases, or cycles, in people’s responses to terminal illness:
Denial and Isolation: Denial is typically a brief reaction, in which the patient is in disbelief or shock about the situation. This phase functions as a buffer after receiving shocking news and allows the patient to regroup. This phase can also result in “doctor shopping,” in which the patient will seek advice from other specialists in hopes that the diagnosis will indeed be a mistake. Examples of expressions in this phase include, “There has been a mix-up with my test results,” or “No, it can’t be true. That’s impossible.”
• Anger: This phase typically surfaces when patients are ready to acknowledge their illness, when they come to terms with the fact that they are, in fact, seriously ill. The patient becomes pessimistic and unhappy. An example of a question in this phase is, “Why me? Why not someone else?” This phase is particularly difficult for the family and medical personnel to deal with because the anger is often projected unpredictably on to others. The most important things the angry patient needs are respect, understanding, attention, and time.
• Bargaining: As the patient attempts to deal with overwhelming feelings of vulnerability and helplessness, the individual may secretly try to make deals with a higher power to prolong life. Examples of this include, “I’ll stop smoking if I can just stay alive long enough to attend my daughter’s wedding.”
• Depression: This phase arises when patients can no longer avoid a sense of great loss. They can feel guilty because of the strain they feel they’re putting on their family and a deep sadness for experiences they may miss out on. Kübler-Ross defines two phases of depression: preparatory and reactive. Preparatory refers to patients preparing themselves for their final separation from this world, while reactive encompasses the unrealistic guilt or shame patients feel about their illness. In this phase, it is imperative that patients are allowed to express their justified sadness.
• Acceptance: Although this phase should not be confused with happiness, it does warrant a quiet peacefulness in the end of life. It is a final time for resting, free of pain and struggle. The patient may wish for solitude and may not be as talkative. Times of silence during visits may be the most meaningful mode of communication for these patients. This phase can be notably difficult for loved ones of the patient, as they may not have accepted the impending loss and view the patient’s ambivalence with death as “giving up.”
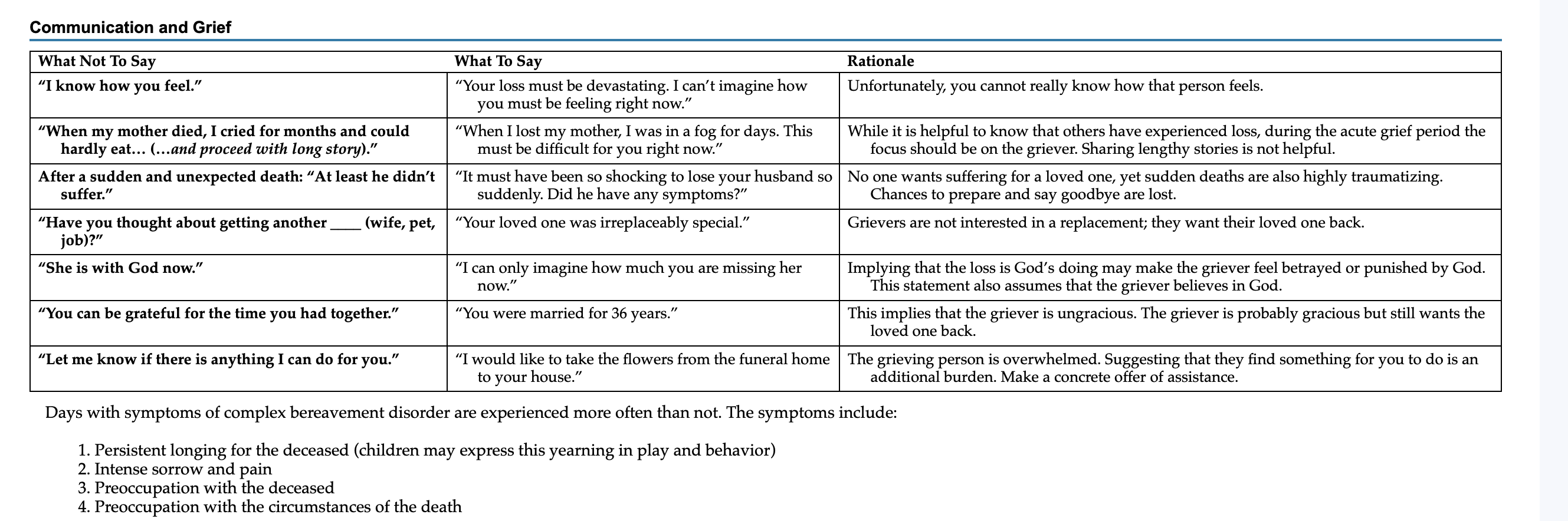
2. Therapeutic communication with the grieving client.
3. What is normal grief?
Grieving is a normal and complex process in response to loss. We grieve the commonplace losses in our lives—loss of a relationship (e.g., divorce, separation, death, abortion), health (e.g., a body function or part, mental or physical capacity), a friendship, status or prestige, security (e.g., occupational, financial, social, cultural), or a dream. Other normal losses include changes in circumstances such as retirement, promotion, marriage, and aging. These losses can promote growth through adaptation or may result in apathy, anger, and resentment.
4. What is complicated grief (bereavement)?
bereavement, derived from the Old English word berafian, meaning “to rob,” is the period of grieving after a death.
prolonged and intense form of grief characterized by persistent longing and difficulty accepting the loss, leading to significant impairment in daily functioning.
5. Nursing interventions for acute grief.
Eye contact, the suitable use of touch, and a posture of attentiveness express warmth and provide comfort.
Listening is the absolute best nursing intervention that a nurse can use
spiritual care is important to people with spiritual convictions and religious beliefs. Assess the role of faith in your patient’s life and the perspective of death that accompanies religious beliefs. Offer support and referrals to pastoral counseling (when available) or community resources.
6. What nursing cares are provided at the end of life? (Table 30.4 p. 558 Varcarolis 9th ed.)
CHAPTER 31: OLDER ADULTS
1. What mental illness(es) is/are prevalent in older adults?
MDD
suicide
GAD
dellirum
Alcohol use disorder
2. What contributes to mental illness in older adults?
3. Risk factors for alcohol abuse in older adults?
Risk factors for heavy drinking in older adults are being male and single, having less than a high school education, low income, and cigarette smoking. Additionally, depression often plays a role in increased alcohol consumption in the older adult.
4. Alcohol abuse in older adults can lead to what neurocognitive disorder?
Long-term excessive alcohol use can lead to alcohol-induced dementia.
5. What should nurses assess for when caring for older adults?
6. What factors may increase suicidal ideation (SI) in older adults?
• Diagnosable psychiatric illness (psychosis, anxiety, substance use, previous suicide attempts)
• Psychological alterations (personality, emotional reactivity, impulsiveness)
• Stressful life events
Other risk factors include access to weapons, access to large doses of medications, and chronic or terminal illness. Some protective factors include spiritual beliefs, being married, personal resilience, perception of social/family support, and having children.
7. Be able to distinguish between aphasia, apraxia, and agnosia in older adults.
aphasia (difficulty finding words)
apraxia (difficulty carrying out motor functions)
agnosia (failure to recognize objects), and disturbances in executive functioning (organizing, planning, abstracting, insight, judgment).