Dysrhythmia & EKGs (Critical Care)
Dysrhythmia Fundamentals
Abnormal cardiac rhythms = dysrhythmias.
Prompt assessment of BOTH the rhythm and the patient’s clinical response is critical.
Cardiac Conduction Pathway
SA Node → AV Node → Bundle of His → R/L Bundle Branches → Purkinje Fibers
Autonomic Nervous System Effects
Parasympathetic (Vagus Nerve): ↓ SA node automaticity, ↓ AV conduction, ↓ HR, ↓ contractility.
Sympathetic: ↑ SA node automaticity, ↑ AV conduction, ↑ HR, ↑ contractility.
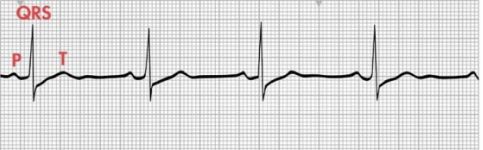
ECG Waveforms & Normal Intervals
Depolarization: Triggers contraction of the heart.
Repolarization: Cells return to resting polarized state
Component
Description
Normal Range
P Wave
Atrial depolarization (contraction)
0.06–0.12 sec
PR Interval
SA → AV → His → Purkinje
0.12–0.20 sec
QRS
Ventricular depolarization (contraction)
< 0.12 sec
(Anything more may indicate a PVC)
ST Segment
Early ventricular repolarization (isoelectric → net charge of zero from being at rest)
~0.12 sec
T Wave
Ventricular repolarization
~0.16 sec
QT Interval
Full depolarization + repolarization
0.34–0.43 sec
ECG Recording Basics
12-lead ECG = Gold standard
6 frontal-plane leads (I, II, III, aVR, aVL, aVF) → measure different angles of the heart in the vertical/frontal plane.
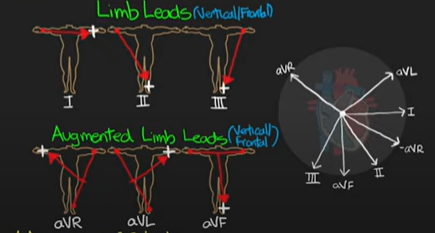
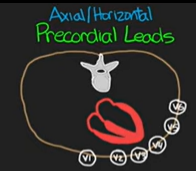
6 precordial leads (V1-V6) → goes around the heart and measures in the horizontal/transverse plane.
Single or multiple-lead monitoring for continuous rhythm strips. Measures electrical signal from patient.
Lead Placement (bedside)
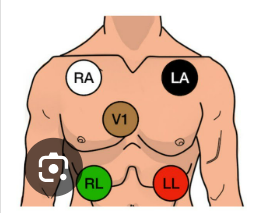
3-lead (MCL): RA, LA, LL with chest lead.
5/6-lead: RA, LA, RL, LL + V1 or V6 chest lead (exact precordial landmarks given) → most common in an acute care setting.
Telemetry Monitoring
Centralized system (tech monitors multiple patients) OR bedside computerized alarms for dysrhythmia/ischemia/infarction.
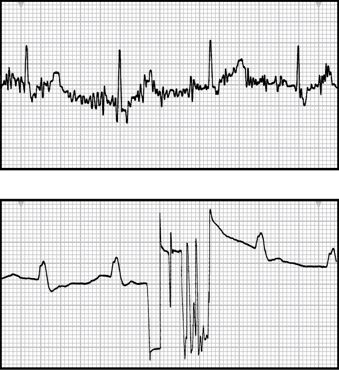
Artifact & Electrode Preparation
Artifact distorts interpretation; verify cable connections and placement FIRST, replace dried electrodes, keep patient warm and still, HOB 30 degrees.
Anything that’s not the actual heart rhythm
poor prep ↑ artifact.
Prep: Clip hair, clean skin (alcohol/gauze) and use skin prep, dry thoroughly.
Monitoring: Leads must be changed.
Rhythm Interpretation Steps
Regular or Irregular? (equal R-R distances = regular).
Atrial & Ventricular rate?
Are there any P waves? – What do they look like (morphology)? No P waves narrows down the rhythm.
Is there 1 P wave for every QRS complex (1:1 Ratio) or is there more?
Are the PR and QRS within normal limits? If not, this narrows down the rhythm.
ST segment isoelectric (having no net charge)?
Elevated may indicate STEMI
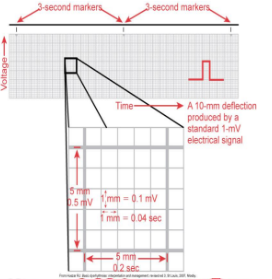
Heart-Rate Calculation Tricks
Count QRS in 1 min (full strip) – most accurate.
Count R-R intervals in 6 seconds and multiply by 10.
**Each small box within a big box is 0.04 seconds.
**The large box is equal to 0.20 seconds.
30 big boxes = 6 seconds
SINUS NODE (SA) RHYTHMS
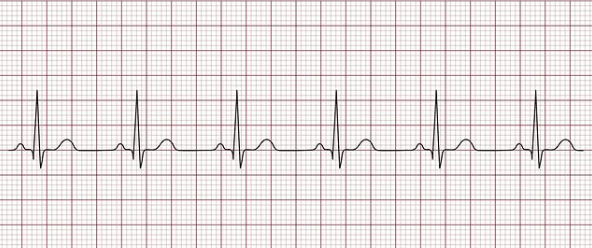
Normal Sinus Rhythm (NSR): SA fires 60-100 bpm; normal conduction.
Sinus Bradycardia: <60 bpm; normal conduction. Increased space between complexes.
Can be a normal rhythm in very healthy pts or athletes.
General Treatment: Stop causative drugs (ex. beta blockers) or reduce dose
Treatment (if symptomatic/unexpected):
Atropine (first-line)
Dopamine and epinephrine infusions in ICU (increases contractility, HR, and CO)
Pacing (if nothing else works)
Symptomatic S/S: Hypotension, pale/cool skin, dizziness/syncope, confusion, tachypnea.
Sinus Tachycardia: 100-180 bpm; normal conduction; often compensatory (ex. fever, pain, hypovolemia, etc). Closer R-R intervals.
Treatment → #1 Identify & treat underlying cause (ex. Potassium)
#2 Vagal maneuvers (stimulate the Vagus nerve to slow a fast HR / have patient “bear down” or blow into an empty syringe).
#3 Beta-blockers or CCBs
Long-standing tachycardia causes decreased CO due to poor perfusion (heart unable to fill completely).
ATRIAL-ORIGIN RHYTHMS
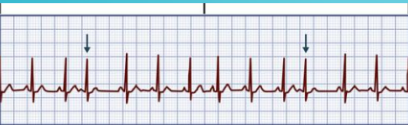
Premature Atrial Complexes (PACs)
Characteristics: Early heart beats. All waves present but altered. Often triggers PSVT.
Causes: Emotional stress, fatigue, tobacco/alcohol/caffeine (stimulates sympathetic nervous system), cardiac diseases (HF, CAD).
Treatment: Monitor until symptomatic, reduce stimulation, treat underlying conditions (ex. HF), B-blockers.
Supraventricular Tachycardia (SVT) - Gradual or Sudden
Includes a-fib, a-flutter, PSVT, sinus tachycardia.
Conduction abnormality; HR >150 bpm and narrow QRS complex tachycardia.
SVT Sustained: Dangerous because HR is too fast and can’t fill with enough blood to perfuse the rest of the body. Requires intervention. Same treatment as PSVT. Regular rhythm.
Prolonged: Less blood in = less blood out.
Leads to decreased CO → hypotension, dyspnea, angina, palpitations, HF.
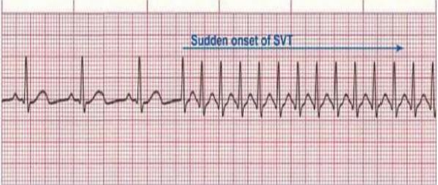
Paroxysmal Supraventricular Tachycardia (PSVT) - Sudden
Characteristics: Ectopic focus above Bundle of His; usually sudden onset/offset (paroxysmal).
String of repeated premature beats often triggered by PAC.
HR can be 151-220 bpm (narrow QRS).

Causes:
In a Normal Heart:
Emotional stress
fatigue
tobacco/alcohol/caffeine/Adderall (stimulants)
Digoxin toxicity, CAD, cor-pulmonale (right-side HF).
Digoxin toxicity slows the AV node conduction, increases contractility, and increases irritability of cardiac cells.
Prolonged PSVT (HR >180 bpm):
Palpitations or complaints of a “racing heart”
Hypotension
Dyspnea
Angina
Treatment Hierarchy:
• #1 Vagal maneuvers “bear down” (Valsalva/breathing into syringe, coughing) → first-line.
• #2 IV adenosine (drug of choice if vagal fails).
• #3 β-blockers or CCBs (diltiazem).
• #4 Synchronized cardioversion if unstable (last option).
Atrial Flutter “Sawtooth”
Characteristics: Single atrial focus → saw-tooth F waves. Single ectopic focus in atria. NO P WAVES.
HR 250-350 bpm and ventricular rates may vary.
Ex. 4 F waves for every 1 QRS complex (4:1 ratio).
Causes:
CAD/HF
HTN (uncontrolled)
mitral valve disorders
PE (right-sided strain on heart, “cor pulmonale”)
COPD
hyperthyroidism
cardiomyopathy
Drugs: Digoxin and epi (long-term use of epi).
Risks: ↓ CO from rapid beat and loss of atrial kick (pushes the rest of the blood into the ventricle).
Stroke from atrial thrombus (blood isn’t fully expelled from atria)
HF
Angina
Treatment: Goal is to slow the ventricular rate
Drugs:
B-blockers → Slows HR.
IV CCBs & Amiodarone → Converts to sinus rhythm (Antidysrhythmias).
Anticoagulants
Common Complication: Blood clots (atria not fully contracting → blood pools in atria).
Warfarin (Coumadin) → prevent clot formation.
Synchronized cardioversion if unstable
Dronedarone (Multaq) given beforehand.
Procedures (last option):
Radio-frequency ablation (curative for chronic a-flutter)
Looks for ectopic beat by entering through femoral artery to see where in atria the tissue is firing from → cauterize tissue.


Atrial Fibrillation - “Irregularly Irregular” or “chaotic twitching”
Characteristics: Chaotic atrial activity; NO P WAVES.
Atrial: 400-600 bpm (too fast to be counted)
Ventricular rate varies:
Slow (<60 bpm)
Controlled ventricular: 60-100 bpm
Rapid >100 bpm (A-fib with RVR)
Most common dysrhythmia; Prevalence ↑ with age or post-op.
Clinical Manifestations: Hypotension, palpitations, dyspnea, angina.
Causes:
Mainly underlying heart disease: Rheumatic HD, CAD, cardiomyopathy, HF, pericarditis,
Acutely: Alcohol (especially withdrawing), caffeine, post-cardiac surgery, electrolyte disturbances, thyrotoxicosis (hyperthyroidism).
Consequences: ↓CO (loss of atrial kick) + risk of embolic stroke
Treatment: Goal is to decrease ventricular rate and prevent embolic stroke
Drugs:
Anticoagulants (#1 to prevent stroke) → Warfarin
B-blockers & IV CCBs (#1 to slow HR)
Antidysrhythmias (#1 for rhythm control) → Amiodarone
Aspirin if low risk for embolic stroke
Procedures:
Synchronized Cardioversion
If pt has A-Fib >48 hours → start anticoagulation (Warfarin/Coumadin) minimum 3-4 weeks before cardioversion and 4-6 weeks after.
Radio-frequency ablation
Maze procedure (curative)
Procedure stops a-fib by interrupting ectopic signals with creation of scar tissues via incision in atria.
ATRIOVENTRICULAR (AV) BLOCKS
First-Degree
Consistent PR >0.20\,\text{s}; usually benign/asymptomatic.
Ex. Pt can have NSR and may present with a first-degree AV block without symptoms.
Occurs with: CAD, rheumatic heart disease, vagal stimulation, inferior MI.
Drugs: Digoxin (with and without toxicity), B-blockers, CCBs.
Treatments: Check medications FIRST and monitor for worsening symptoms.
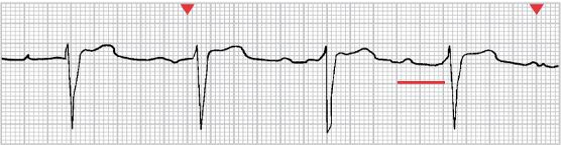
Second-Degree Type I (Wenckebach) → Usually Asymptomatic
“Longer… longer… longer… DROP! This is when you have a Wenckebach”
Gradual lengthening of the PR interval (time between P wave and QRS) until a P wave is not followed by a QRS (dropped beat) → usually in AV node or His-Purkinje system.
Occurs With: Drugs (B-clockers or digoxin), CAD, myocarditis, and electrolyte imbalances such as hyperkalemia.
Result of inferior MI or myocardial ischemia (transient and well-tolerated).
Acute MI patients → may be warning sign of complete heart block.
Symptomatic → atropine or temporary pacemaker
Asymptomatic → observe (TCP on standby).
Bradycardia is likely to become symptomatic when hypotension, HF, or shock is already present.
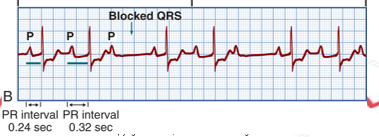
Second-Degree Type II (Mobitz II) → “Lethal Rhythm”
P waves are randomly dropped, but the PR interval stays the same.
Often progresses to complete heart block (3rd degree).
Occurs With: Anterior MI, CAD, and drug toxicity
Results in ↓CO with hypotension and myocardial ischemia
Treatment: Permanent pacemaker
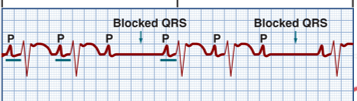
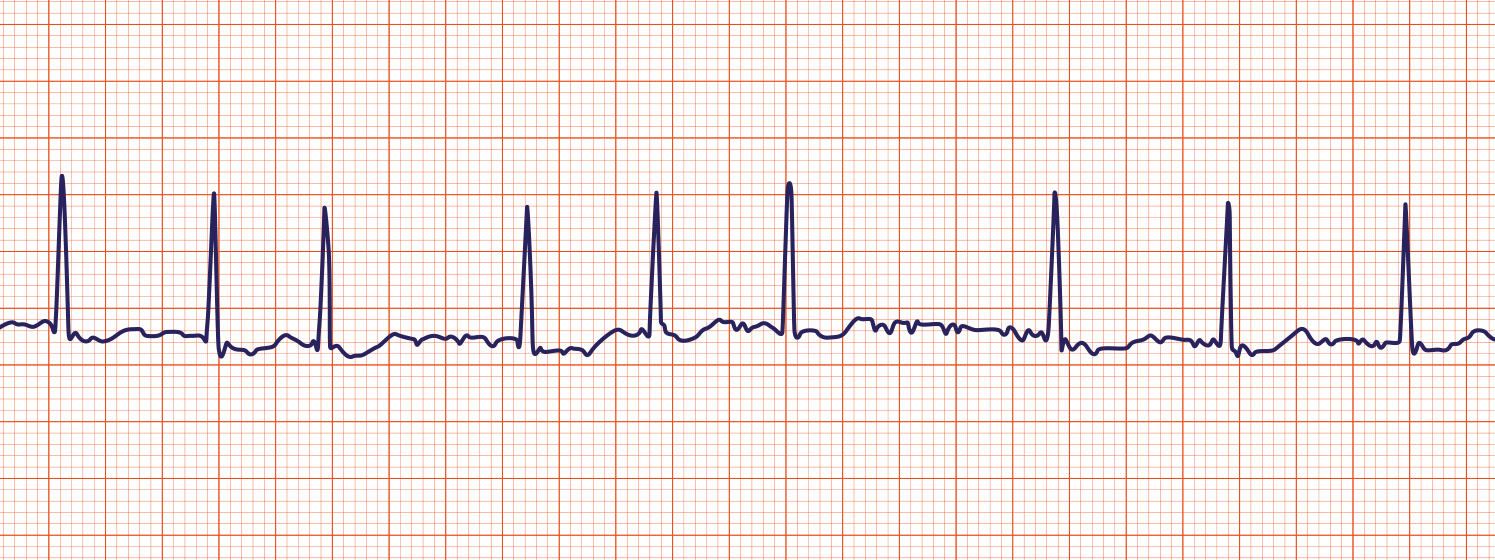
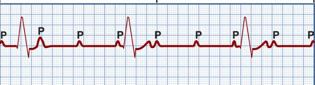
Third-Degree (Complete) AV Block → “Lethal Rhythm”
No atrial impulses reach ventricles (AV dissociation); Atria and ventricles beat independently.
Ventricular escape 20-40 bpm (slow) → depends on site of block.
P waves and QRS complexes are present with QRS frequently missing beats (PR intervals are inconsistent).
Occurs With: Severe heart disease (CAD, MI, cardiomyopathy, myocarditis, scleroderma), and digoxin/b-blockers/CCBs.
Results in ↓CO with ischemia, HF, shock, and syncope from severe bradycardia or asystole.
Treatment: Immediate transvenous pacing (TCP) + permanent pacemaker.
Drugs: Dopamine and epi drips for BP and HR support; atropine ineffective.
VENTRICULAR RHYTHMS
Premature Ventricular Contractions (PVCs)
Abnormal early occurrence of a wide and distorted QRS (>0.12\,\text{s}); ectopic focus of the ventricles. Contains P wave, QRS, and T wave.
Unifocal (arising from or occurring in a single direction or location) or multifocal (arising in different directions like up and down).
Causes: Emotional stress, stimulants, digoxin, hypoxia, electrolyte imbalances (hyperkalemia), disease states (MI, MVP, HF, fever).
Usually benign in healthy hearts; in diseased hearts may ↓CO, trigger angina/HF.
Don’t count PVCs → watch on monitor and feel a pulse that correlates with the heart rhythm.
Treatment: Treat cause (O₂, replete K⁺/Mg²⁺)
Drugs: β-blocker, amiodarone, lidocaine.

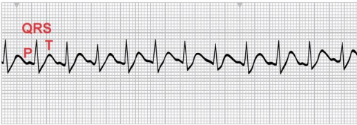
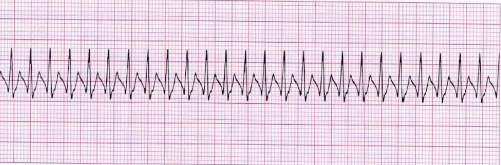
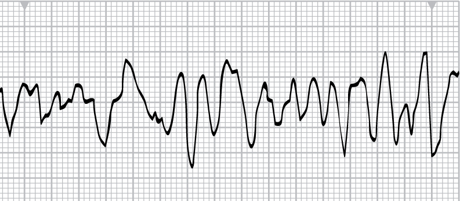
Ventricular Tachycardia (VT) → !!!!!Lethal Rhythm!!!!!!!
≥3 consecutive PVCs with HR >100 bpm, can be as high as 300 bpm.

Comes in multiple forms:
Monomorphic VT: All beats look the same (shockable).
Polymorphic VT (e.g., torsades de pointes): Beats look different; rhythm varies.
Nonsustained VT: Brief episodes of VT that last less than 30 seconds.
Sustained VT: When the ventricular tachycardia lasts longer than 30 seconds and causes severe decrease in CO. Can be life—threatening.
Life-threatening – may deteriorate to VF from decreased CO.
Causes: MI, CAD, cardiomyopathy, electrolyte issues (K or Mg), drug toxicity (digoxin), CNS disorders, long QT.
Treatment (based on pulse):
Monomorphic VT with Pulse:
Stable→ IV amiodarone/lidocaine
Unstable → IV amiodarone/lidocaine followed by synchronized cardioversion.
Pulseless Monomorphic VT (life-threatening)
(Cardiac Arrest) → CPR + rapid defibrillation (unsynchronized shock)
Epinephrine if shock fails.
Polymorphic VT w/ prolonged QT (torsades) → NOT SHOCKABLE
IV magnesium
Isoproterenol (speed up heart)
Lidocaine
Stop QT-prolonging meds ASAP (ex. antipsychotics)
Cardioversion considered if rhythm not converted.
**May reoccur in patients if prophylactic treatment isnt initiated
Ventricular Fibrillation (VF) - !!Lethal Rhythm!!
Multiple ventricular foci firing → chaotic quivering; no CO → START CPR IMMEDIATELY.
Patient is unresponsive, pulseless, apneic – death without immediate action.
Types of V-Fib:
Fine
Coarse
Causes: Acute MI, CAD, reperfusion, trauma (ex. car accident), pacing/cath lab, electric shock, hyperkalemia, acidosis.
Treatment:
CPR + rapid defibrillation
Drug therapy.
LETHAL RHYTHMS
Ventricular Fibrillation (fine/coarse) – shockable.
Ventricular Tachycardia (monomorphic) – shockable.
Torsades de Pointes (polymorphic VT) - NOT shockable.
Second-degree AV block Type II - NOT shockable.
Third-degree AV block - NOT shockable.
Asystole / Pulseless Electrical Activity - NOT shockable.
Torsades de Pointes (polymorphic VT) → “Arctic Monkeys” (Not Shockable)
Polymorphic VT twisting around baseline; long QT predisposition.
Risks: TCA overdose, hypomagnesemia, hypokalemia, congenital long QT, cardiac disease.
S/S: palpitations, light-headedness, syncope → arrest.
Therapy: correct electrolytes (Mg²⁺), antiarrhythmics, pacemaker, ICD.
Pulseless Electrical Activity (PEA)
Electrical rhythm present, no pulse (no mechanical activity).
Must search for cause – “Hs & Ts”:
Hypovolemia (loss of blood/low blood volume→ must replace blood lost)
Hypoxia (consider intubation)
Hydrogen ions (acidosis)
Hypo/hyperkalemia (flat/peaked T waves→ if hyperkalemia, give calcium gluconate)
Hypothermia (give warm fluids or bear hugger)
Toxins,
Tamponade,
Tension pneumothorax,
Thrombus (MI/PE).
Treatment: CPR + epinephrine, intubation, correct underlying cause.
Asystole “Flat-line” → NOT SHOCKABLE
Total absence of ventricular electrical activity; no CO; poor prognosis.
Causes: End-stage HF, severe conduction disease, advanced CAD.
Treatment: CPR, ACLS (epi, intubation, TCP). Defibrillation not indicated.
Synchronized Cardioversion vs. Defibrillation
Method | Use For | Notes |
|---|---|---|
Synchronized Cardioversion | Unstable VT (with pulse), SVT, A-Flutter, A-Fib | Sync with R wave, sedate if awake |
Defibrillation | VF, pulseless VT | Unsynchronized, performed ASAP (<2 min), biphasic preferred (energy delivered in two directions 120-200 J) |
Defibrillation: Depolarizes entire myocardium allowing SA node reset.
Pacemakers
Provide electrical stimuli when intrinsic path fails.
Components: programmable generator + pacing leads.
Ex. Can be programmed for 70 bpm and if heart doesn’t meet requirement then it’ll shock.
Pacer spike will be seen on EKG.
Temporary Pacing
Transvenous (bridge to permanent), Epicardial (during open-heart), Transcutaneous (emergency; painful – give analgesia/sedation if possible).
Permanent / Cardiac Resynchronization Therapy (CRT)
Goal to re-pace the heart
Biventricular pacing for HF to re-sync ventricles; may combine with ICD.
Complications: infection, hematoma, pneumothorax, lead displacement/perforation (ex. Heavy lifting).
If vegetation occurs around leads then it’ll be shut off temporarily until vegetation resolved.
Post-Procedure Care & Teaching
Monitor site; OOB once stable; limit arm/shoulder on pacer side.
Patient education:
• Attend follow-up checks.
• Incision care; report redness, swelling.
• Arm restrictions (no lifting above shoulder for specified time).
• Avoid direct blows nor contact spots; high-output generators (ex. No working with certain heavy machinery because it can interfere); strong magnets (unless MRI-safe), anti-theft devices
• Microwaves OK; airport security – show ID card.
• Carry Medic-Alert & ID card; learn to take pulse daily.
Implantable Cardioverter-Defibrillator (ICD)
Lead via subclavian → endocardium; generator subcutaneously.
Detects and shocks lethal rhythms, delivers ≤25 J.
Indications: survived SCD, sustained VT, syncope with inducible VT/VF, high-risk patients.
Functions: defibrillation + over-drive pacing for VT + back-up pacing for bradycardia.
Same peri-op care as pacemaker.
Psychosocial: body image, fear of shocks; encourage support group.
Teaching parallels pacemaker plus: what to do if ICD fires (sit/lie, call EMS if >1 shock), caregivers learn CPR.
Adult Cardiac Arrest (VF/pVT vs PEA/asystole)
Shockable (VF/pulseless VT):
Shock
CPR 2 min + Epinephrine q3–5 min
Re-shock + CPR → Amiodarone or Lidocaine
Non-Shockable (PEA/Asystole):
CPR + Epinephrine ASAP
Identify & treat Hs & Ts
Ethical & Practical Implications
Rapid recognition of lethal rhythms saves lives; nurses must master equipment setup, artifact reduction, and algorithms.
Anticoagulation decisions in AF involve risk-benefit, shared decision making.
Device therapy (pacemaker/ICD) impacts lifestyle & psychological well-being – holistic education & support needed.