Notes: Ch.5 Tissues
Course Information
Overview
Instructor: Dr. Nusrat Sajid
Course Title: Bio25 Anatomy and Physiology
Institution: Carrington College
Chapter: HORD
Outline of Key Topics
5.1 Epithelial Tissue
A comprehensive study of epithelial tissue types, focusing on their structural characteristics, classification, and functions in protection, secretion, and absorption.
Emphasis on the role of epithelial tissue in forming barriers and glandular structures in the body.
5.2 Connective Tissue
In-depth examination of various types of connective tissues, their composition, structural diversity, and functional roles in supporting, binding, and protecting different organs and systems.
Discussion on specialized connective tissues: blood, bone, and cartilage.
5.3 Muscle Tissue
Detailed insights into muscle tissue types including skeletal, cardiac, and smooth muscle, addressing their histological features, mechanisms of contraction, and physiological roles in movement and tissue support.
Description of the unique properties that differentiate each muscle type, including voluntary versus involuntary control.
5.4 Nervous Tissue
Overview of the structure and function of nervous tissue, focusing on neurons and glial cells, and their roles in signal transmission and neurological support.
Examination of the diverse types of glial cells and their functions in maintaining homeostasis and supporting neuronal health.
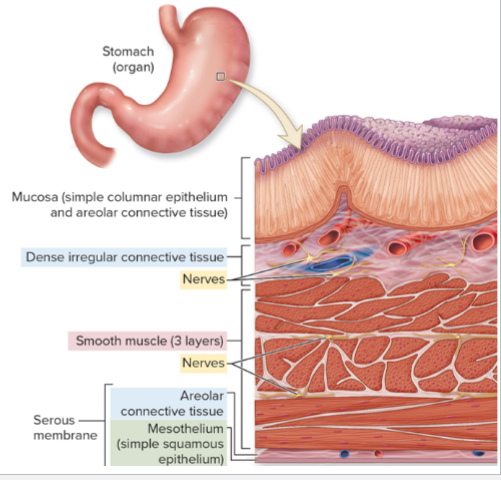
5.5 Tissue Integration: Organs and Membranes
Exploration of how various tissue types combine to form organs, illustrating the interdependence of epithelial, connective, muscle, and nervous tissues.
Highlighting examples of organs and their specific tissue compositions that contribute to their function.
5.6 Development, Change, Aging, and Death
Analysis of tissue development, including differentiation and specialization during embryonic growth.
Investigation of how tissues adapt to changes over time, the effects of aging on tissue function, and the processes leading to tissue degeneration and death.
Introduction to Histology
Definition
Histology is the microscopic study of tissues, essential for understanding their organization, functions, and interactions within the body.Tissues
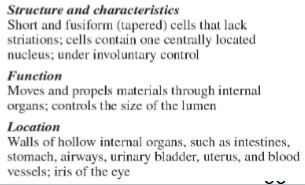
Tissues are groups of similar cells and extracellular matrix that work together to perform specific functions. Four main types of tissues are recognized:
Epithelial Tissue: Serves as barriers and facilitates absorption and secretion in various body surfaces and cavities.
Connective Tissue: The most diverse tissue type, provides structural support, stores energy, and participates in immune responses.
Muscle Tissue: Responsible for movement, composed of contractile fibers enabling body motion and function.
Nervous Tissue: Involves neurons for signal transmission, helping coordinate body responses to internal and external stimuli.
Composition and Functions of Tissues
Summary of Tissues
Composition
Epithelial Tissue: Composed of tightly packed cells with minimal extracellular matrix, essential for protective barriers and exchange surfaces.
Connective Tissue: Consists of fibrous protein structures, ground substance, and cells (both resident and wandering) that provide support and protection.
Muscle Tissue: Characterized by elongated cells (myocytes) organized into bundles allowing contraction and movement.
Nervous Tissue: Made of neurons that transmit impulses and supporting glial cells that protect and maintain neuronal function.
Function
Epithelial Tissue: Functions include protection against the external environment, absorption of nutrients, secretion of mucus and enzymes, and sensation.
Connective Tissue: Provides binding and support, stores fat, transports gases and nutrients, and plays a role in healing and immunity.
Muscle Tissue: Enables voluntary and involuntary movements as well as critical functions such as circulation and digestion.
Nervous Tissue: Essential for signal transmission and processing, integrating physiological responses to stimuli.
Subtypes
Epithelial Subtypes: Simple (squamous, cuboidal, columnar), stratified, and transitional types based on structure and function.
Muscle Types: Divided into skeletal (attached to bones), cardiac (heart), and smooth (walls of organs) muscle types based on structural and functional attributes.
Epithelial Tissue
Characteristics
Epithelial tissue consists of closely packed cells with minimal extracellular matrix. It serves multiple functions:
Protective Barrier: Covers and lines body surfaces and cavities.
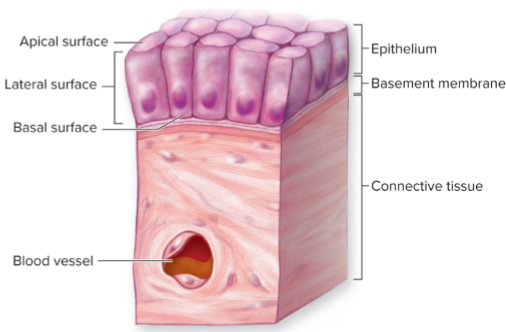
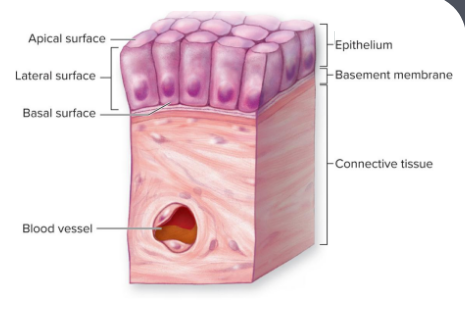
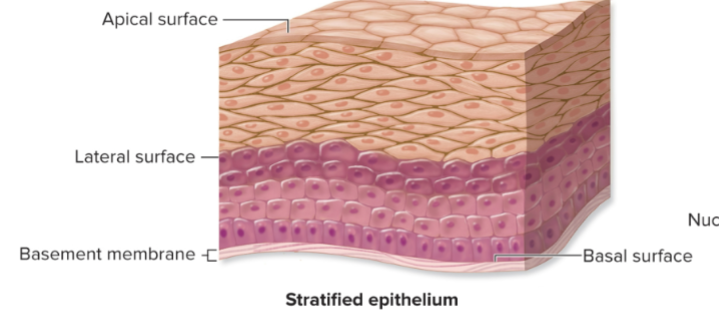
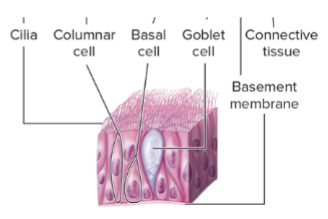
Polarity: Contains an apical surface that is exposed to the body fluids or external environment, lateral surfaces that connect with neighboring cells, and a basal surface anchored to the underlying connective tissue.
Avascular: Lacks direct blood supply but nourished through diffusion of substances from underlying tissues.
High Regenerative Capacity: Rapidly replaces damaged or lost cells to maintain tissue integrity.
Functions of Epithelial Tissue
Key Functions
Protection: Shields underlying tissues from mechanical and chemical injury, pathogens, and dehydration.
Absorption: Facilitates the uptake of nutrients and water in specialized regions like the intestines.
Selective Permeability: Manages the passage of materials into and out of tissues, vital for homeostasis.
Secretion: Specialized cells secrete products like hormones, enzymes, and mucus.
Sensation: Contains sensory receptors that increase body awareness of external stimuli and facilitate reflexes.
Classification of Epithelial Tissue
Ways to Classify
By Number of Cell Layers
Simple Epithelium: One layer facilitating absorption and secretion; ideal for filtration processes.
Stratified Epithelium: Multiple layers providing robust protection in high-friction areas.
Pseudostratified Epithelium: Appears layered due to varying cell heights while all cells connect with the basement membrane.
Classification by Cell Shape
Squamous Cells: Flat cells that allow for efficient diffusion of gases and nutrients.
Cuboidal Cells: As tall as wide; suited for secretion and absorption, found in glands.
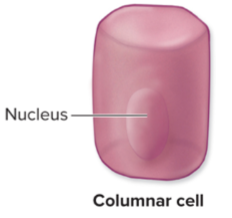
Columnar Cells: Taller than wide; involved in absorption, secretion, and sometimes possess cilia or microvilli for increased surface area.
Transitional Cells: Specialized to stretch, adapting shape based on the bladder's fullness.
Epithelium Illustrated
Visual Classification
Apical Surface: The exposed part of epithelial cells that interacts with the environment or internal spaces of organs.
Lateral Surface: Communicates and bonds with adjoining cells through specialized junctions.
Basal Surface: Anchors epithelial tissue to the underlying connective tissue via the basement membrane.
Types by Layers
Simple Epithelium: Includes simple squamous, simple cuboidal, and simple columnar epithelium. Each type has specific functions based on location and structure.
Stratified Epithelium: Includes stratified squamous, stratified cuboidal, and stratified columnar epithelium, providing protective functions in various organs where friction occurs.
Organization of Epithelia Types
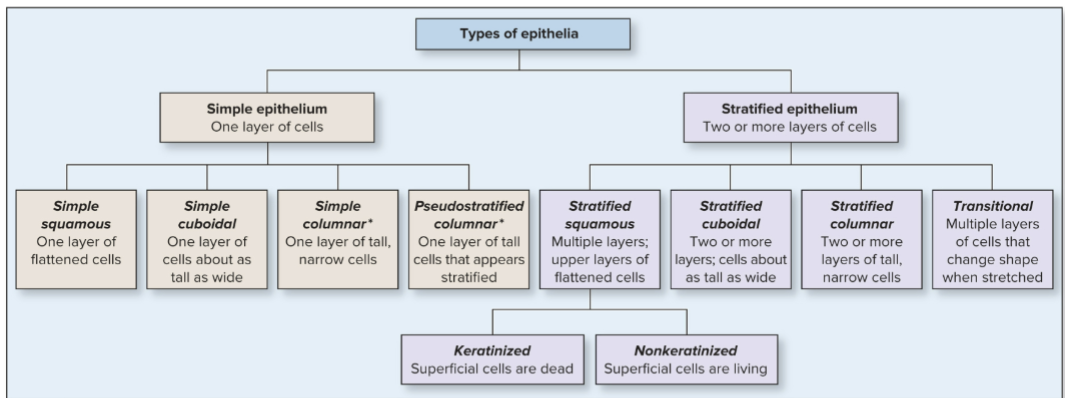
Simple Epithelia
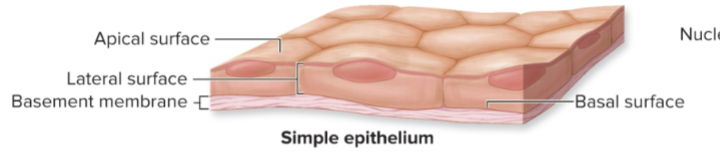
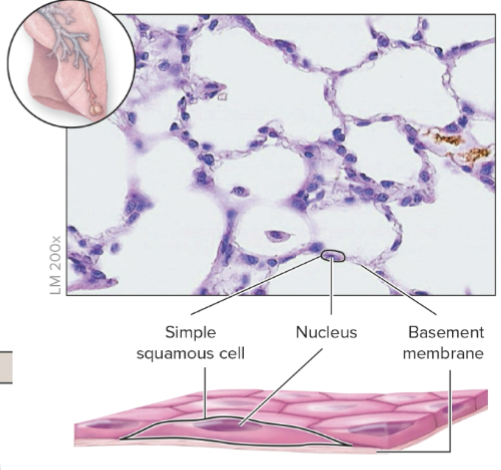
Simple Squamous: One layer of flattened cells; found in areas of diffusion such as blood vessels.
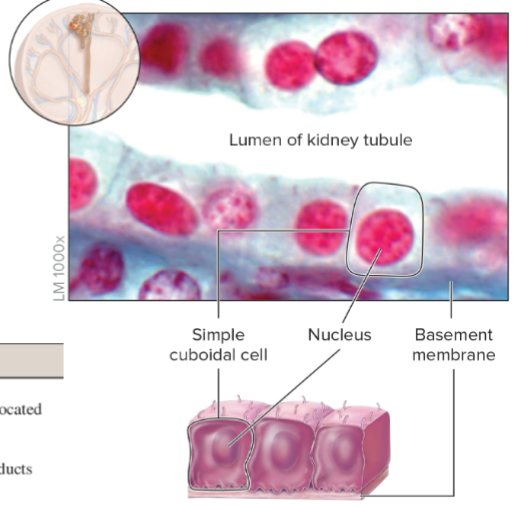
Simple Cuboidal: One layer of cube-shaped cells; involved in secretion in glands and kidney tubules.
Simple Columnar: One layer of long, column-like cells; involved in absorption in digestion and secretion of mucus.
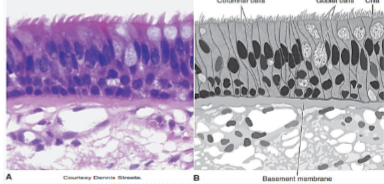
Pseudostratified Columnar: Appears stratified but is a single layer of irregularly shaped cells; often ciliated and found in the respiratory tract.
Stratified Epithelia
Stratified Squamous: Composed of multiple layers providing protection against wear and tear, found in skin, mouth, and esophagus.
Stratified Cuboidal: Rare type found in ducts of sweat glands; provides protection and secretion.
Stratified Columnar: Rare epithelial type with multiple layers; found in large ducts of glands.
Transitional: Composed of multiple layers thought to stretch and change shape, found in the urinary bladder.
Simple Squamous Epithelium
Description
A delicate layer with a thin structure to facilitate rapid movement of gases and liquids.
Location
Found lining the air sacs of the lungs (alveoli), blood vessel walls (endothelium), and serous membranes (mesothelium) in the body.
Simple Cuboidal Epithelium
Description
Structured for efficient absorption and secretion processes.
Structure
Consists of a single layer of cuboidal cells with a centrally located nucleus.
Location
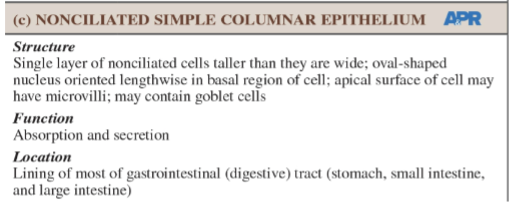
Typically located in the lining of kidney tubules, thyroid glands, the surface of ovaries, and ducts of exocrine glands. Nonciliated Simple Columnar Epithelium
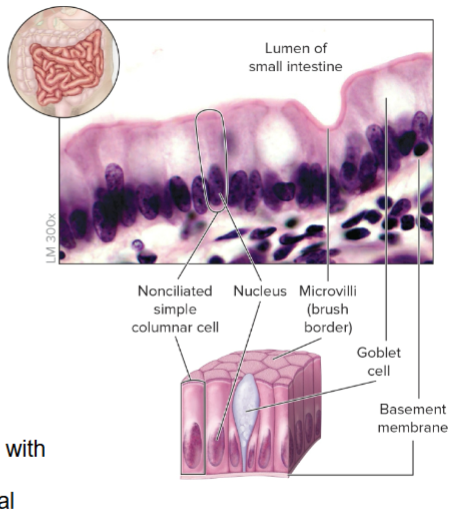
Description
Highly adapted for secretion and absorption, containing microvilli that increase surface area, and goblet cells that secrete mucus.
Location
Lines most of the digestive tract from the stomach to the anal canal, aiding in nutrient absorption and waste excretion.
Ciliated Simple Columnar Epithelium
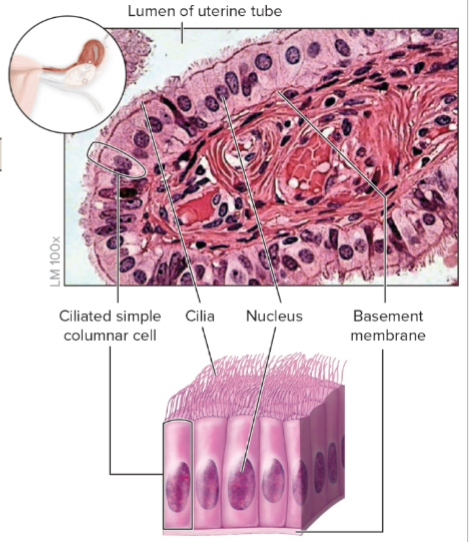
Description
Aberrant for secretion and absorption, featuring cilia that help in moving substances across the epithelial surface.
Location
Lines bronchioles in lungs and uterine tubes, where cilia facilitate the movement of mucus and oocytes.
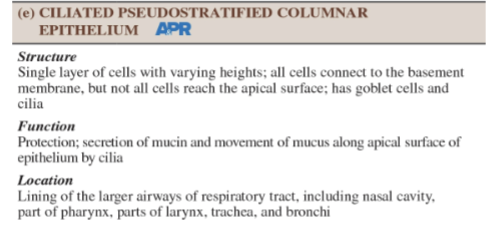
Ciliated Pseudostratified Columnar Epithelium
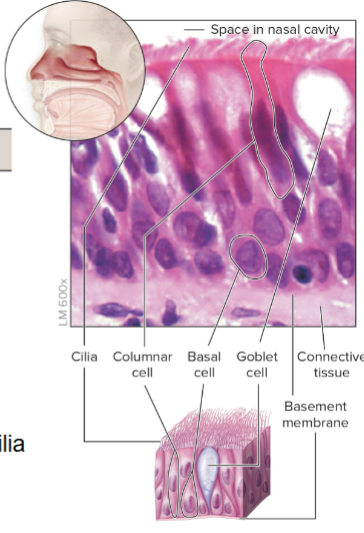
Description
Contains cilia and goblet cells for protective functions and mucous secretion.
Location
Found in the respiratory system's large passageways, providing respiratory surface protection and mucosal moistening.
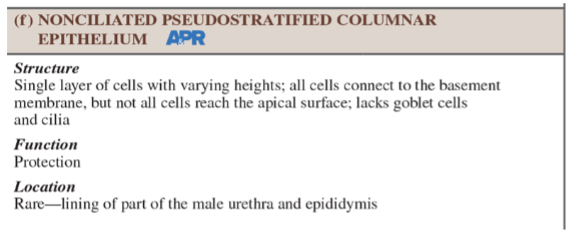
Nonciliated Pseudostratified Columnar Epithelium
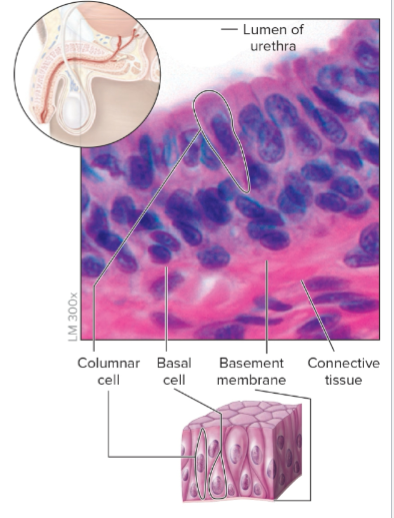
Description
A less common form without cilia or goblet cells, mainly serving a protective function.
Location
Present in the male urethra and epididymis, where it supports protective and reproductive functions.
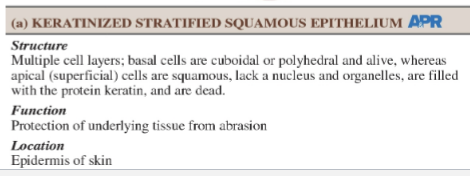
Keratinized Stratified Squamous Epithelium
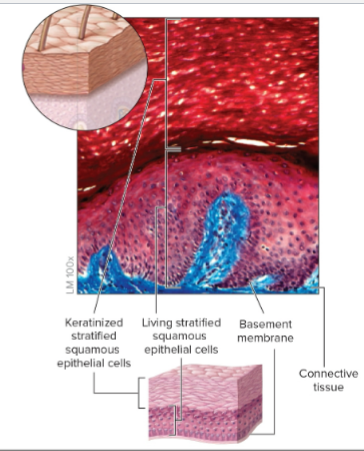
Description
Protective layer that has dead, keratin-filled cells at the surface, mitigating abrasion and desiccation.
Location
Found in the epidermis of the skin, providing a resilient barrier against environmental exposures.
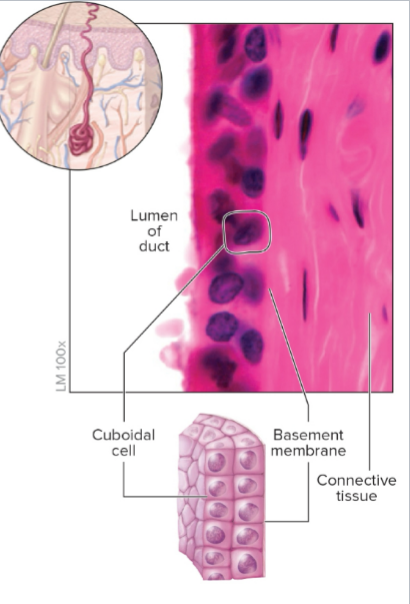
Nonkeratinized Stratified Squamous Epithelium
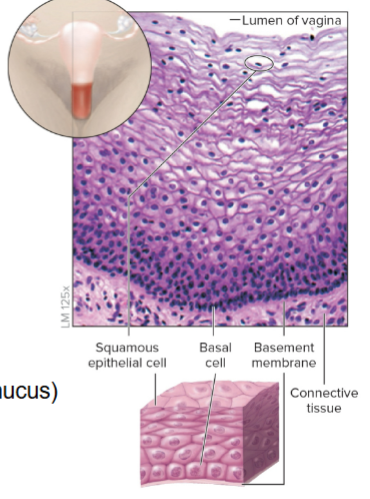
Description
Living cell layers that remain moist; suited for protection in areas subject to friction.
Location
Lining the oral cavity, pharynx, esophagus, vagina, and anus, where moisture retention and protective functions are essential.
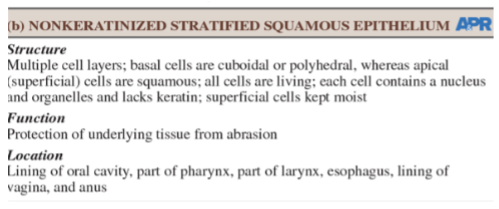
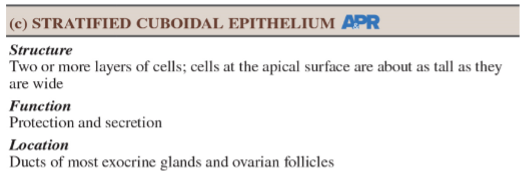
Stratified Cuboidal Epithelium
Description
Typically two or more layers providing protective and secretory capabilities.
Location
Found in the walls of ducts in exocrine glands, such as sweat glands, and parts of the male urethra.
Stratified Columnar Epithelium
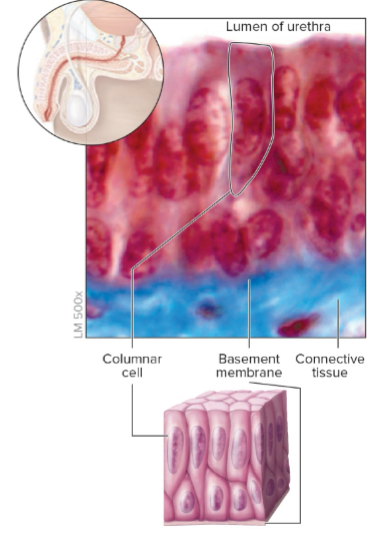
Description
Characterized by columnar cells on the surface layer; rare but serves critical secretory roles.
Location
Present in large ducts of salivary glands and parts of the male urethra.
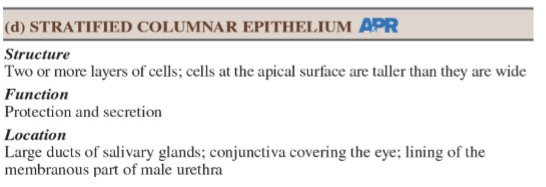
Transitional Epithelium
Description
Allows for stretching and recoiling as the bladder fills; the structure varies based on the degree of distension.
Location
Limited to the urinary tract, allowing it to accommodate fluctuating volumes of urine.
Glands in Epithelial Tissue
Definition
Glands are specialized organs formed primarily of epithelial tissue that produce and secrete substances.
Classification
Endocrine Glands: Release hormones directly into the bloodstream without ducts, influencing metabolic processes in target organs.
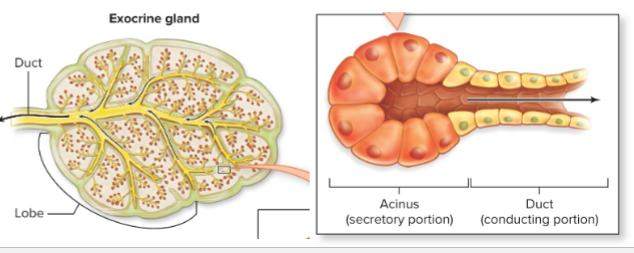
Exocrine Glands: Release their secretions through ducts to external spaces (e.g., sweat glands, mammary glands, and digestive glands).
Exocrine Gland Cellularity
Types
Unicellular Exocrine Glands: Comprise individual cells like goblet cells that secrete mucus directly onto epithelial surfaces.
Multicellular Exocrine Glands: Composed of clusters of cells forming complex structures, often encapsulated by fibrous tissue that organizes their secretory mechanism.
Anatomical Classification of Exocrine Glands
Forms
Simple Glands: Feature a single, unbranched duct for secretion.
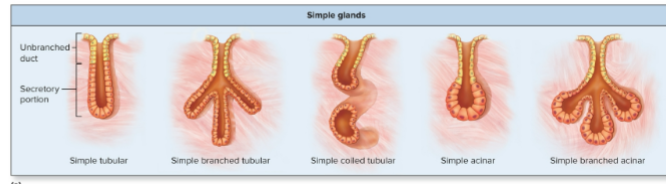
Compound Glands: Have branched ducts for more complex secretory functions.
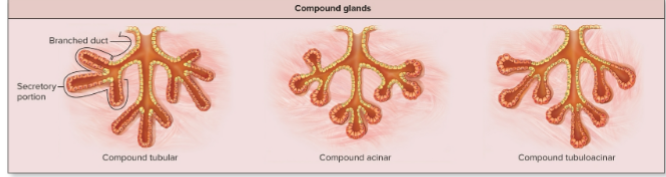
Tubular Glands: Characterized by a consistent diameter in the duct and secretory portions.
Acinar Glands: Have a balloon-like expansion at the secretory portion.
Tubuloacinar Glands: Combine features of both tubular and acinar forms.
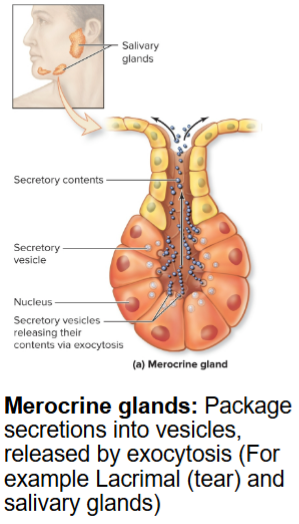
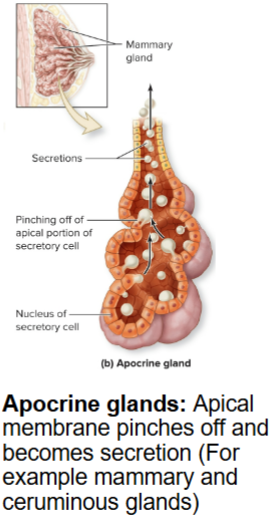
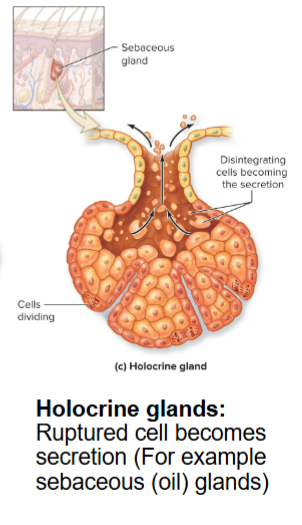
Method of Secretion in Glands
Types
Merocrine Glands: Release secretions via exocytosis without damaging the glandular cell (e.g., salivary glands).
Apocrine Glands: Release products by pinching off a portion of the cell's apical surface (e.g., mammary glands).
Holocrine Glands: Release their secretions through the rupture of gland cells, releasing the entire cell contents (e.g., sebaceous glands of skin).
Learning Review on Epithelial Tissue
Questions
Discuss the significance of high regenerative capacity in epithelial tissue.
Explain the importance of selective permeability in epithelial layers.
Describe the differences between simple and stratified epithelial tissues.
Identify various types of epithelial tissues found lining the air sacs of the lungs.
Compare transitional and keratinized stratified squamous epithelium properties.
Discuss the structure and function of multicellular exocrine glands.
Differentiate between holocrine and merocrine gland functions.
Connective Tissue Overview
Definition
Connective Tissue (CT) is the most diverse and abundant tissue type in the body, providing structure, support, and various protection functions. Originates from embryonic mesenchyme and exhibits variable vascularity among its subtypes.
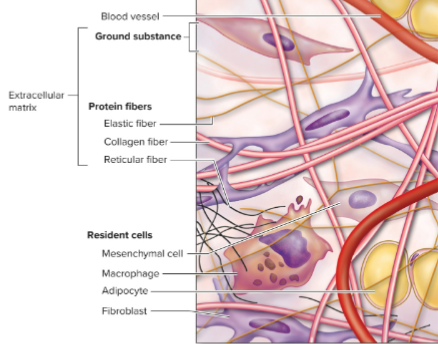
Cells in Connective Tissue
Types of Cells
Resident Cells: Stationary cells responsible for maintaining the extracellular matrix, including
fibroblasts (produce fibers)
adipocytes (store fat)
macrophages (immune defense)
mesenchymal cells (provide structural support and contribute to the formation of connective tissue)

Wandering Cells: Mobile cells playing crucial roles in the immune response, including
leukocytes (white blood cells) that can migrate to sites of inflammation or infection.
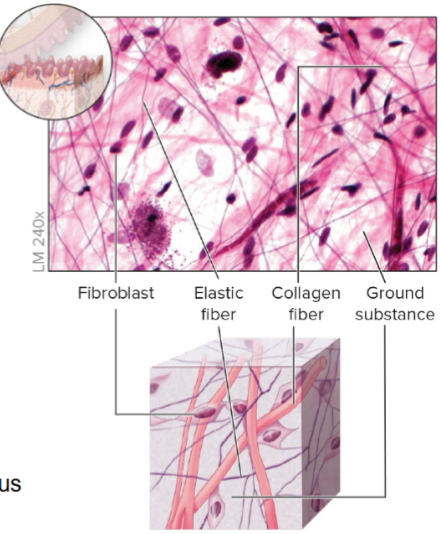
Extracellular Matrix in Connective Tissue
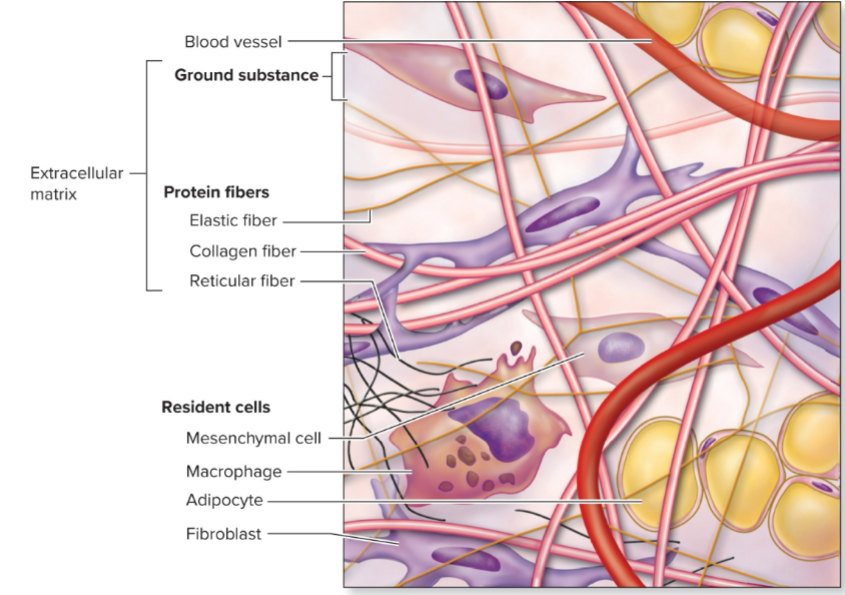
Components
Protein Fibers:
Collagen Fibers: Strong, cable-like structures providing tensile strength; found in tendons and ligaments.
Reticular Fibers: Thinner fibers forming supportive networks (framework) in organs like the liver and lymph nodes.
Elastic Fibers: Flexible fibers allowing tissues to stretch and recoil; mainly found in the skin and arterial walls.
Ground Substance: A gel-like fluid composed of glycoproteins and proteoglycans, providing hydration and biochemical support for cell and fiber arrangements.
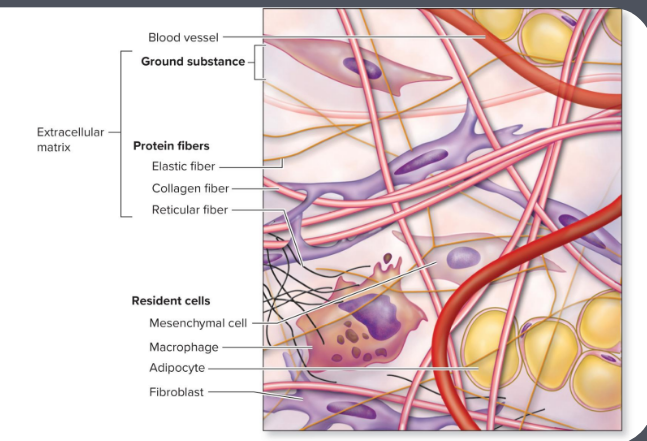
Structure of Connective Tissue
Overview
The structure showcases relationships between resident cells and the extracellular matrix, emphasizing fiber arrangement and types of ground substance, which together contribute to the functional diversity among connective tissues.
Clinical View: Scurvy
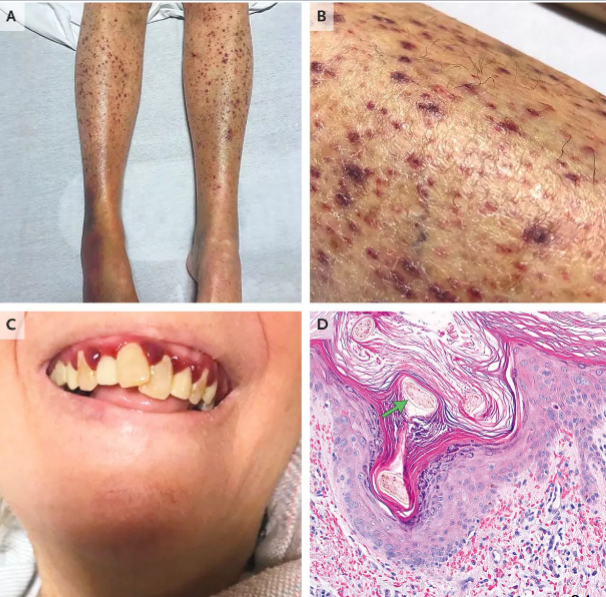
Description
A condition resulting from vitamin C deficiency, leading to weakened collagen fiber integrity, crucial for connective tissue health.
Symptoms
Manifestations include general weakness, bleeding gums, bruising, and complications with bone growth and repair.
Treatment
Managed through dietary changes to include vitamin C-rich foods (like citrus fruits) or supplements to restore collagen health.
Clinical View: Marfan Syndrome
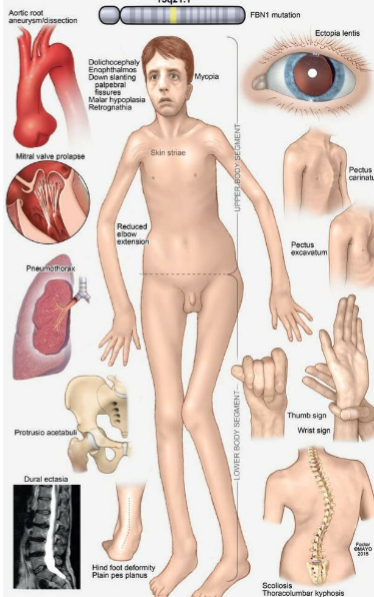
Definition
A rare and serious genetic condition impacting connective tissue, primarily resulting from mutations in the gene responsible for encoding fibrillin-1 on chromosome 15.
Symptoms
Individuals may present with disproportionately long limbs and digits, cardiovascular conditions, joint dislocations, and significant structural deficiencies.
Management
Requires early intervention through medical surveillance, ensuring cardiovascular health, and management strategies to enhance quality and length of life.
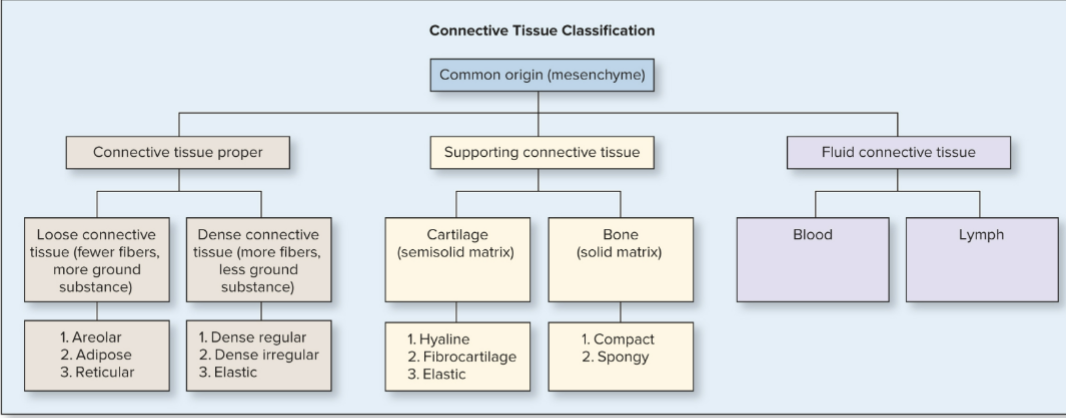
Nervous Tissue Overview
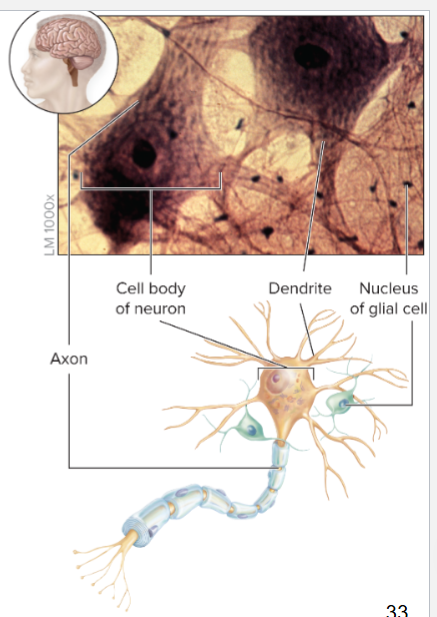
Definition
Nervous tissue comprises neurons tasked with receiving and transmitting nerve impulses, integral to processing sensory data, and initiating responses. Found in the brain, spinal cord, and nerves throughout the body.
Glial Cells
Supportive glial cells fulfill various roles including insulation, nutrient supply, and maintenance of the neuronal environment, crucial for efficient signal transmission.
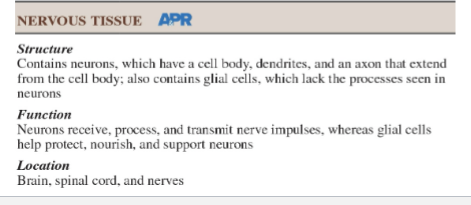
Parts of a Neuron
Neuron Structure
Cell Body: Contains the nucleus and organelles vital for cellular function and maintenance.
Dendrites: Short, branched processes that receive signals from other neurons and transmit them to the cell body.
Axon: An elongated process transmitting signals away from the cell body toward other neurons or target tissues.
Note
Neurons represent some of the longest cells in the human body, allowing for rapid communication over significant distances within the nervous system.
Learning Review on Nervous Tissue
Key Question
Assess and differentiate between the roles of neurons and glial cells in the nervous system, emphasizing their contributions to overall neural function.
Functions of Connective Tissue
General Functions
Connective tissue serves several critical roles in the body such as:
Physical Protection: Shielding organs from injuries.
Support: Providing frameworks for organ structure and function.
Binding Structures Together: Connecting different body structures, including organs and tissues.
Storage: Serving as energy reserves and mineral storage.
Transport: Facilitating the movement of materials like blood through vessels.
Immune Protection: Engaging in inflammatory and immune responses through various cell types.
Embryonic Connective Tissue
Types
Mesenchyme: The precursor tissue from which all connective tissues develop, consisting of unspecialized cells. (immature cells)
All cells in connective tissues!! are derived from mesenchyme, which plays a crucial role in the formation of various tissue types as they differentiate and mature.

Mucous Connective Tissue: Present in the umbilical cord, providing flexible support during fetal development.

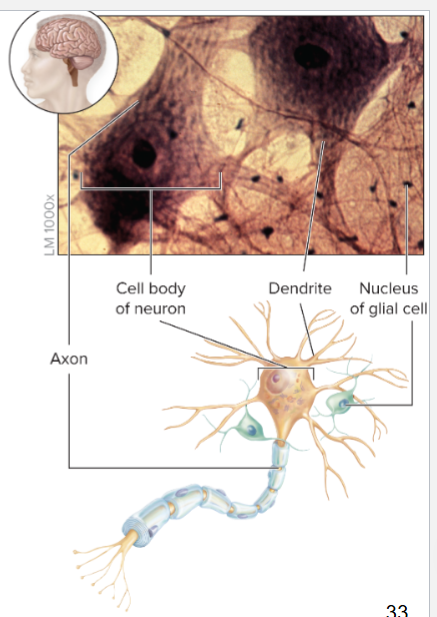
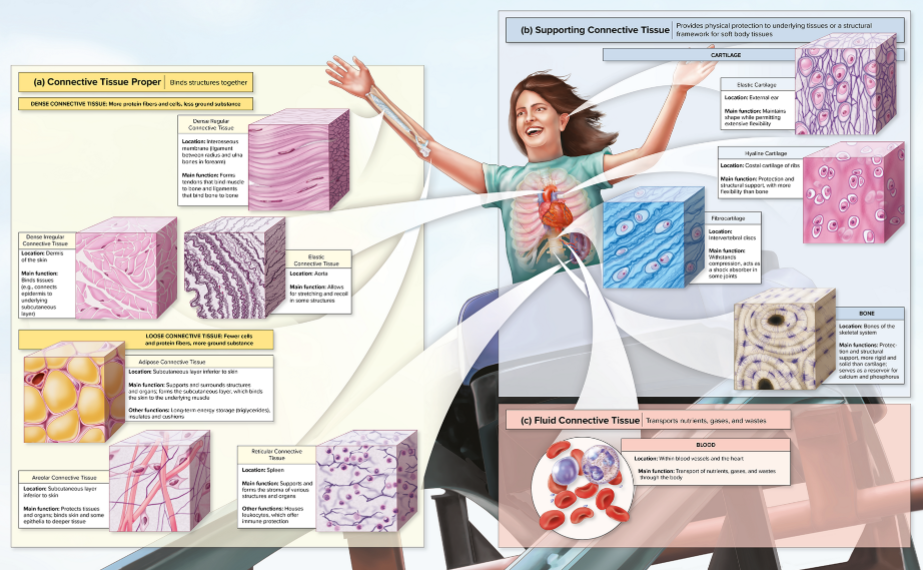
Classification of Connective Tissue
Types
Connective Tissue Proper: Includes two categories - loose (with fewer fibers) and dense (with more tightly packed fibers) connective tissues.
Supporting Connective Tissue: Encompasses cartilage (various types) and bone, providing structural integrity and support.
Fluid Connective Tissue: Consists of blood and lymph, facilitating transportation and immunity.
Connective Tissue Proper - Loose Connective Tissue
Characteristics
Characterized by fewer cells and protein fibers, with abundant ground substance serving as a flexible matrix and packing material for body structures.
Types
Areolar CT: Loose arrangement with high vascularization, providing support and a reservoir for water and salts.
protect tissues and organs
present in the dermises
irregular arrangement of collagen and elastin fibers allows for flexibility and strength, making it essential for connecting skin to underlying structures.

Adipose CT: Composed primarily of adipocytes, serving energy storage, insulation, and cushioning.
two types:
white: stores energy
brown: found in newborns, generates heat

Reticular CT: Made of reticular fibers, forming supportive frameworks, especially in lymphatic organs.
Leukocytes: White blood cells that play a crucial role in the immune response, helping to defend the body against infections and foreign invaders.
lymph notes: Small, bean-shaped structures that filter lymph and house immune cells, playing a vital role in the body's defense system.
reticular fibers: are thin, branching fibers that create a delicate network, providing structural support to various organs, including the spleen and bone marrow.

Areolar CT
Description
Features a loosely organized structure of collagen and elastic fibers, abundant blood vessels allowing nutrient and gas exchange.
Location
Found in the dermis, surrounding organs, nerves, muscles, and blood vessels, serving multiple functions in flexibility and support.

Adipose CT

Characteristics
Primarily composed of adipocytes featuring two types:
White Adipose: Functions in energy storage and thermal insulation.
Brown Adipose: Specializes in heat production, predominantly found in newborns and hibernating mammals, aiding in thermoregulation.
Reticular CT

Characteristics
Constructed of reticular fibers providing a supportive framework for various cells.
Location
Found in many lymphatic organs (e.g., spleen, thymus), facilitating the organization and functioning of immune cells.
Dense Connective Tissue
Overview
Characterized by a higher concentration of protein fibers providing stronger resistance to tensile forces compared to loose connective tissues.
Fiber blast cells (Collagen Fibers)
Types
Dense Regular CT: Contains parallel collagen fibers; offers strength primarily in one direction, ideal for tendons and ligaments.
Dense Irregular CT: Composed of collagen fibers arranged in multiple orientations; provides strength and support against multidirectional stress, found in the dermis and organ capsules.
Elastic CT: Packed with elastic fibers allowing stretch and recoil; found in structures like the walls of large arteries and the trachea.
Dense Regular CT

Characteristics
Extremely strong tissue due to its tightly packed parallel collagen fibers, resisting stretching in one direction.
Location: Commonly found in tendons and ligaments, where strength and resistance to tensile forces are crucial.
Function: Provides strong support and stability to joints and muscles, allowing for effective movement and force transmission.
Location
Typically found in tendons (connecting muscles to bones) and ligaments (connecting bone to bone), enabling joint stability and movement.
Dense Irregular CT
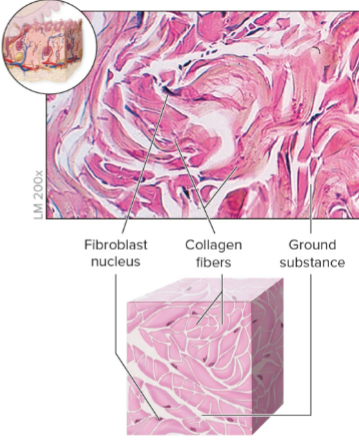
Characteristics
Composed of irregularly arranged collagen fibers that can withstand stress in multiple directions, providing robust support.
Cell type: fibroblasts, which are responsible for producing and maintaining the extracellular matrix.
Location: Found in areas such as the dermis of the skin, joint capsules, and the outer layers of bones, where flexibility and strength are essential.
knee, shoulders and cartilage, contributing to the overall stability and resilience of these structures.
Location
Located in the dermis of the skin, organ capsules, and periosteum, where flexible strength is necessary.

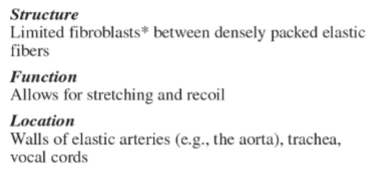
Elastic CT

Characteristics
Densely packed with elastic fibers allowing for stretch and flexibility; crucial in maintaining the integrity of certain structures.
Fiber blast cells are responsible for the production of the elastic fibers, playing a key role in the formation and maintenance of elastic connective tissue.
Location
Found in large arteries, trachea, and vocal cords, contributing to recoil and structural resilience.
Supporting Connective Tissue - Cartilage
Characteristics
A resilient and strong yet flexible tissue containing chondrocytes in lacunae, aiding in support and structure of various body parts.
Contains Collagen and Elastin proteins, which contribute to its tensile strength and elasticity, allowing it to withstand compressive forces while maintaining its shape.
Chondrocytes cells
Chondroclast
Chondroblast
Types
Hyaline Cartilage: Most common type, smooth and glassy, provides support and flexibility; found in trachea and joints.
Fibrocartilage: Contains more collagen fibers, offering significant resistance to compression; found in intervertebral discs and menisci.
Elastic Cartilage: Features a dense network of elastic fibers, allowing for great flexibility; found in the external ear and epiglottis.
Hyaline Cartilage
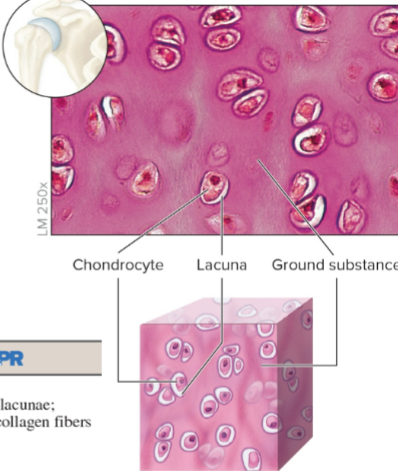
Characteristics
Clear, glassy appearance with high collagen content.
provides support with some pliability and smooth surfaces for joint movement.
no blood vessels
Chondrocytes: The cells found in cartilage that produce and maintain the cartilaginous matrix, essential for the tissue's structure and function.
Lacuna: a small cavity within the cartilage matrix that houses chondrocytes, allowing for the maintenance and nourishment of the tissue.
Ground Substance: The amorphous gel-like material found within the cartilage matrix, providing support and facilitating the exchange of nutrients and waste between chondrocytes and their surrounding environment.
Location
Present in the
nose, trachea, larynx, costal cartilage, and fetal skeleton, facilitating development and structural integrity.
Fibrocartilage
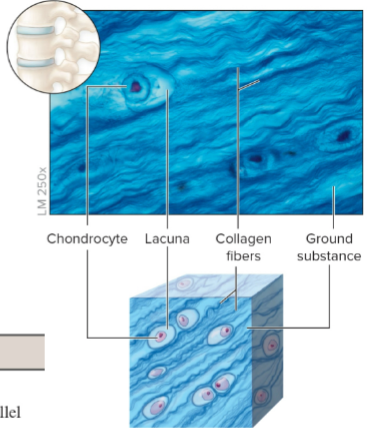
Characteristics
Resists tension and compression; contains fewer cells and more abundant fibers than hyaline cartilage.
Resists compression protein fibers
elastin fiber
Location
Found in
intervertebral discs, pubic symphysis, and menisci of joints, serving as a shock absorber and weight-bearing surface.
Knee
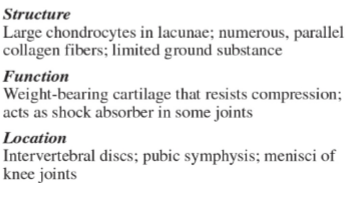
Elastic Cartilage
Characteristics
Distinguished by its flexible nature due to abundant elastic fibers; maintains shape while allowing flexibility.
chondrocyte cells
Location
Found in the
external ear, epiglottis, and some parts of the larynx, providing structural support while allowing recoil.
Bone Overview

Characteristics
A dense, hard tissue providing structural support, mineral storage, and protection to vital organs; composed of organic and inorganic components.
Components
Organic: Collagen fibers and glycoproteins contribute to flexibility and tensile strength.
Inorganic: Mainly calcium salts provide rigidity and strength.
Osteocytes: Mature bone cells residing in lacunae, critical for bone maintenance and repair.
Lacuna: Space between the cells.
Concentric Lamella: Layers of bone matrix that surround the central canal, contributing to the structure and strength of compact bone.
Types
Compact Bone: Formed of tightly packed osteons, providing strength and structural support.
Spongy Bone: Found within the interior of bones, characterized by a lattice-like structure that reduces weight while maintaining strength.

Fluid Connective Tissue - Blood
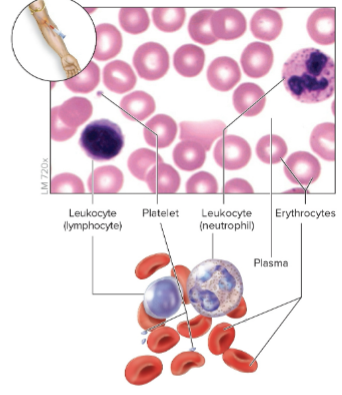
Components
Erythrocytes (RBC): Specialize in oxygen transport throughout the body. (Transport O2)
Leukocytes (WBC): Key components of the immune response, involved in defending against pathogens. (Immunity)
Plasma: The liquid matrix of blood, containing nutrients, hormones, proteins, and waste products facilitating transportation. (Clotting agent)
Lymph: A type of white blood cell that plays a crucial role in the immune system by helping to filter pathogens and produce antibodies. (Immune defense)

Clinical View on Connective Tissue
Breakdown of Locations and Functions
Dense Connective Tissue:
Dense Regular: Found in tendons and ligaments enabling connection and movement of bones; resists tensile forces.
Dense Irregular: Located in the dermis and organ capsules, providing multi-directional strength.
Loose Connective Tissue:
Adipose CT: Functions as a protective cushion and energy reservoir in various body locations.
Learning Review on Connective Tissue
Key Questions
Discuss the differences between resident and wandering cells in connective tissue.
Explain the functions of ground substance and glycosaminoglycans (GAGs).
Summarize the general functions and types of connective tissues.
Describe the composition and significance of mesenchyme in connective tissue development.
Create a flow chart for the classification of connective tissue.
Detail the description and location of fibrocartilage.
Discuss why blood is classified as connective tissue despite being a liquid.
Muscle Tissue Overview
Definition
Muscle tissue is specialized for contraction and movement, playing a vital role in facilitating locomotion and various bodily functions.
Types
Skeletal Muscle: Voluntary muscles that allow conscious movements, characterized by striated appearance.
Cardiac Muscle: Involuntary and striated tissue found exclusively in the heart, responsible for pumping blood.
Smooth Muscle: Involuntary and non-striated, located in the walls of internal organs, aiding in various autonomic functions.
Skeletal Muscle Tissue
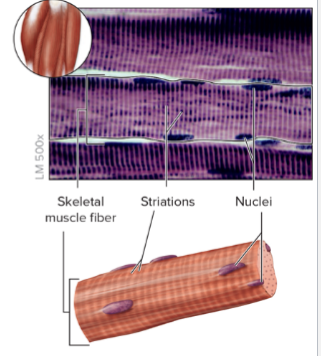
Features
Skeletal muscle features long, cylindrical, striated fibers, enabling force generation during voluntary contractions.
Function
Primary function includes movement of the skeleton and stabilization of body positions.
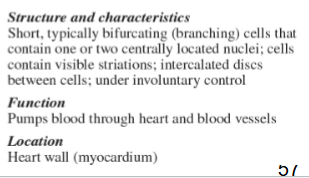
Cardiac Muscle Tissue

Features
Characterized by shorter, branched fibers connected by intercalated discs that facilitate synchronized contraction.
Involuntary Control
Controlled by pacemaker cells, allowing rhythmic contraction and relaxation necessary for efficient blood circulation.
Smooth Muscle Tissue
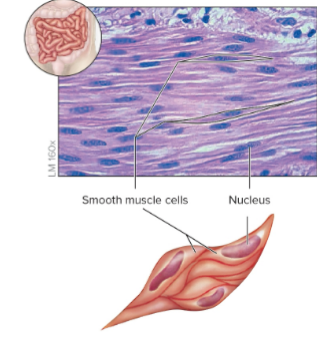
Features
Non-striated, spindle-shaped cells designed for continuous involuntary contractions, aiding in the movement of substances through pathways.
Locations
Found in organ walls such as blood vessels, intestines, and respiratory ducts, facilitating vital processes like digestion and circulation.
Learning Review on Muscle Tissue
Key Question
Compare and contrast the structures and functions of skeletal and cardiac muscle tissues, emphasizing their differences in control, appearance, and physiological roles.
Organs Overview
Definition
Organs are defined as structured aggregates of different tissue types working cohesively to perform specific physiological functions (e.g., stomach, heart).
Structure
Each organ typically consists of all four primary tissue types, facilitating complex functionality and interactions among tissues.
Body Membranes Overview
Definition
Membranes are formed from epithelial layers bound to underlying connective tissue, serving various protective and functional roles.
Types
Mucous Membrane: Lines compartments open to the external environment, providing interfaces for absorption and secretion.
outside the body
Serous Membrane: Lines body cavities not exposed to the external environment; produces serous fluid to reduce friction between organs.
Inside the body
Cutaneous Membrane: The skin, which protects internal structures and prevents water loss.
outside the body
Synovial Membrane: Lines joints, secreting synovial fluid for lubrication and nourishment of joint surfaces.
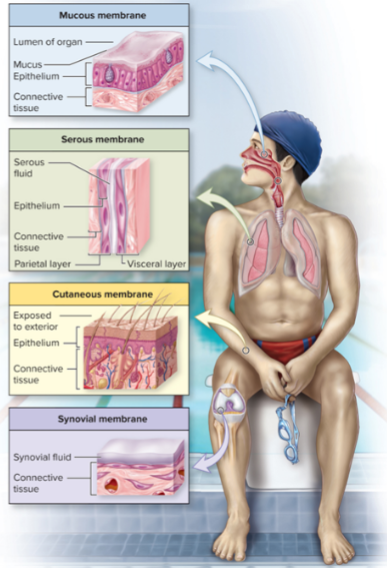
Mucous Membranes
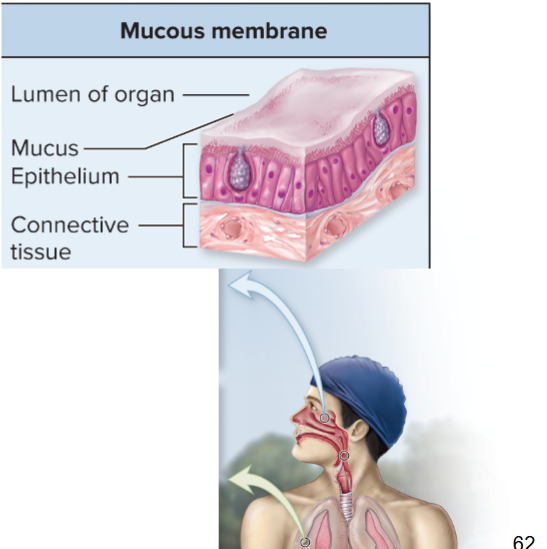
Characteristics
Epithelial lining of tracts such as the digestive, respiratory, urinary, and reproductive systems, performing protective, absorptive, and secretory functions.
Serous Membranes
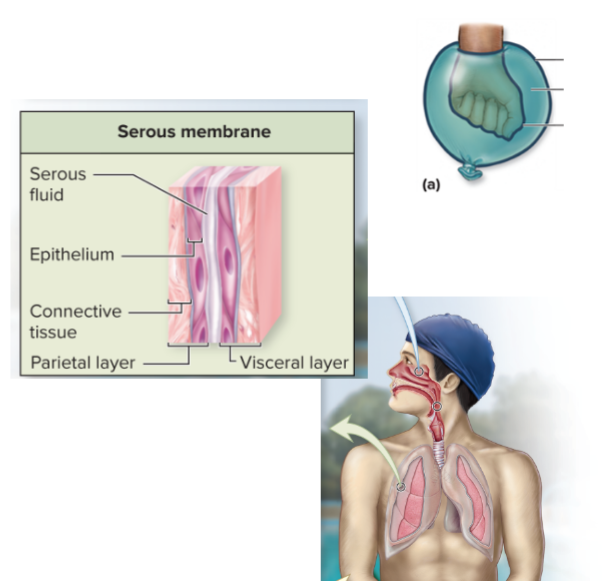
Characteristics
Line closed body cavities, producing serous fluid to minimize friction between moving organs by providing lubricating interfaces.
Cutaneous Membrane
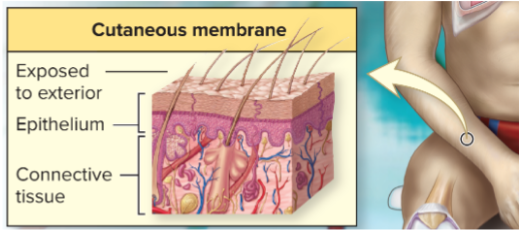
Characteristics
Composed of keratinized stratified squamous epithelium layered (dead cells) over underlying connective tissue, acting as a barrier against external threats and regulating moisture.
Skin
Synovial Membrane
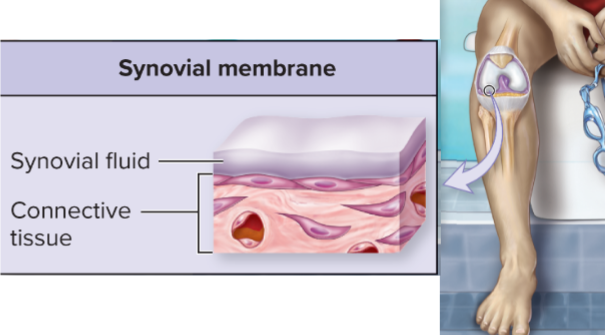
Characteristics
Composed of areolar connective tissue lined by epithelial cells, producing synovial fluid to lubricate and nourish joints, enhancing mobility and reducing wear.
Chondrocytes
present in the knee
Learning Review on Body Membranes
Key Questions
Why is the stomach classified as an organ with respect to its tissue composition?
What are the differences between the parietal and visceral layers of the serous membrane in terms of structure and function?
Tissue Development Stages
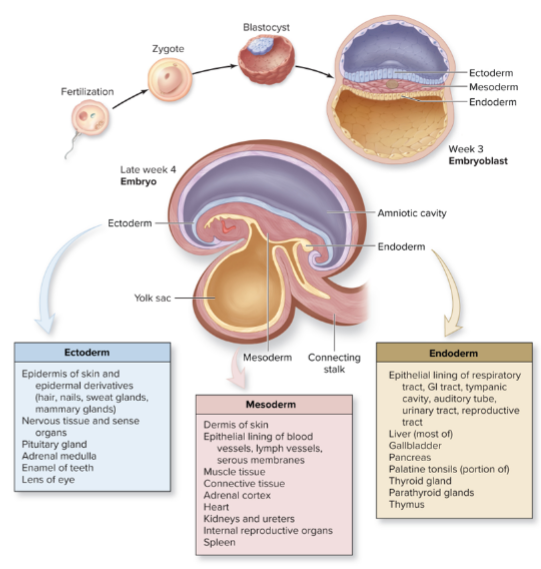
Overview
Development begins with a fertilized oocyte that undergoes division to form a blastocyst, leading to the formation of
three primary germ layers: The three primary layers of cells in the early embryo that differentiate into various tissues and organs.
ectoderm - the outermost layer, which develops into the skin, nervous system, and sensory organs.
mesoderm - the middle layer, responsible for forming muscles, bones, and the circulatory system.
endoderm - the innermost layer, which gives rise to the gastrointestinal tract, respiratory system, and various organs.
Tissue Modification Processes
Types
Hypertrophy: Increase in the size of cells, often in response to exercise or hormonal signals. (Size)
Hyperplasia: Increase in cell number, commonly seen in tissue repair and growth processes. (Tissues)
Atrophy: Decrease in tissue size due to loss of cells or shrinkage of existing cells, often due to disuse or aging.
Metaplasia: Adaptive change in tissue type as a protective mechanism, often reversible. (change of mature epithelium)
Dysplasia: Abnormal development patterns, often precancerous in nature. (Abnormal tissues)
Neoplasia: Uncontrolled tissue growth leading to tumor formation, which can be benign or malignant. (Tumor)
Benign: Non-cancerous growths that do not invade surrounding tissues or spread to distant sites, typically remaining localized and not posing a serious threat to health.
Malignment Metastasizes: The process by which cancer cells spread from the original tumor site to other parts of the body, often leading to the formation of secondary tumors.
Necrosis: Irreversible cellular injury leading to cell death, often resulting from ischemia or infection.
Gangrene: Tissue death due to inadequate blood supply, which can be caused by infection or vascular issues.
Clinical View: Gangrene
Types
Dry Gangrene: Results from extreme cold exposure, causing tissue to dry out and shrink.
Wet Gangrene: Associated with bacterial infections leading to tissue breakdown and pus formation.
Gas Gangrene: Caused by bacterial invasion that produces gas bubbles in tissues, often requiring medical intervention.
Stem Cells Overview
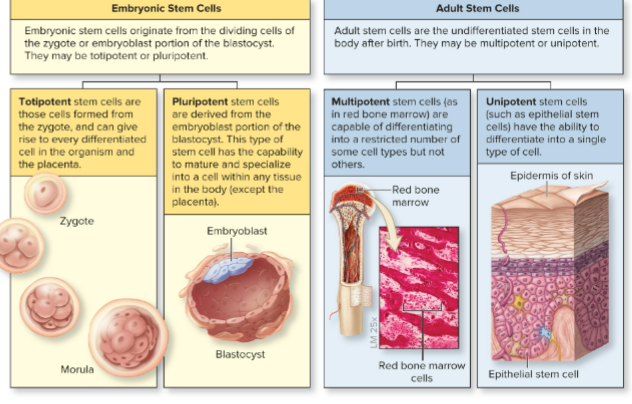
Types
Totipotent Zygotes: Capable of differentiating into all cell types, including embryonic and extra-embryonic tissues.
Pluripotent Embryoblasts: Can form nearly all tissue types but cannot form complete organisms due to lack of extra-embryonic capabilities.
Multipotent Adult Stem Cells: Limited to specific lineages (e.g., hematopoietic stem cells for blood components) critical for tissue maintenance and repair.
Unipotent Cells: Dedicated to producing a single cell type, demonstrating specific lineage.
Aging of Tissues
Effects of Aging
Aging results in decreased efficiency in maintenance and repair of tissues. Typical changes include:
Epithelial thinning, resulting in increased fragility.
Decreased collagen production leading to a loss of structural integrity and skin elasticity.
Bone brittleness due to diminished mineralization and bone density.
Learning Review on Tissue Aging
Key Questions
Identify the three primary germ layers and discuss their formation and roles in tissue development.
Explain the differences between metaplasia, dysplasia, and malignant neoplasia regarding tissue changes.
Discuss the age-related changes in epithelial and connective tissues, including impacts on health and function.
Delete all separating lines: Removing separating lines can improve clarity and allow for smoother reading, especially in documents where the natural flow of text is more important than distinguishing between sections. Consider focusing on paragraph structure, headings, and transitions to maintain organization without the use of lines.