The Cardiovascular System: Blood Vessels and Circulation
Introduction to Blood Vessels and Circulation
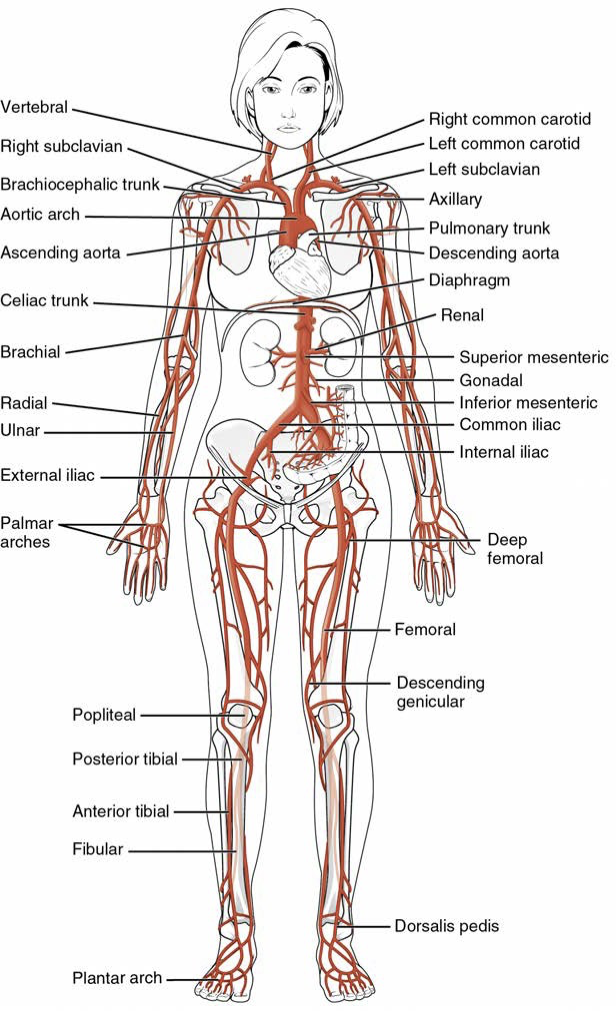
Blood vessels are crucial for transporting blood and facilitating the exchange of gases, nutrients, and waste.
Understanding the structure and function of blood vessels is essential for grasping the cardiovascular system.
Chapter Objectives
Describe the structure of blood vessels, including their walls and types.
Explain the differences between arteries, veins, and capillaries.
Discuss blood flow, blood pressure, and resistance, including major factors that affect these elements.
Explore the homeostatic mechanisms that regulate blood vessel functions.
Structure and Function of Blood Vessels
General Blood Vessel Structure
Lumen: hollow passageway of the vessel
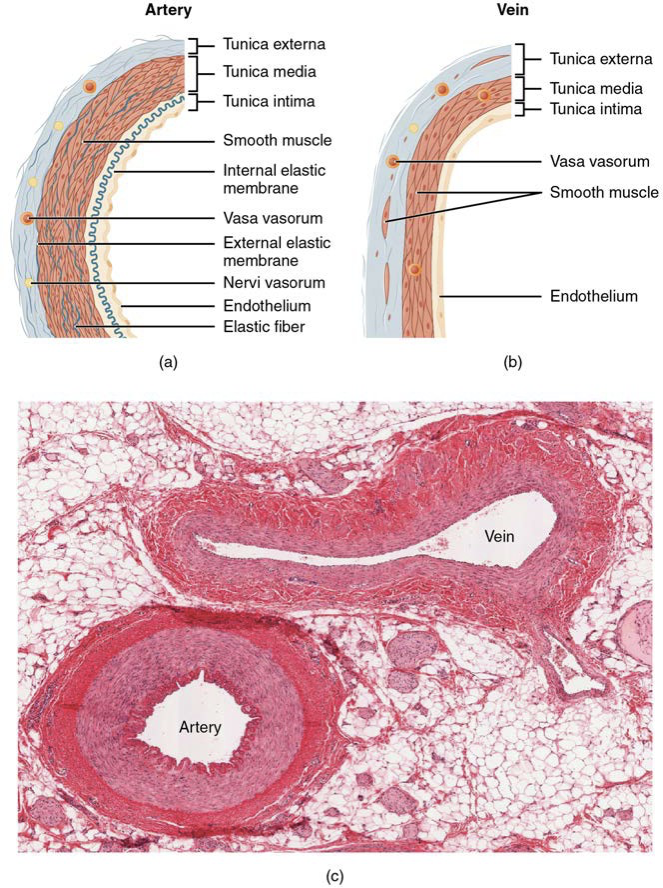
Artery
walls are thicker to withstand the high blood pressure
Veins
have larger lumens because their walls are thinner
vaso vasorum: small blood vessels that supply the walls of larger blood vessels, providing necessary nutrients and oxygen.
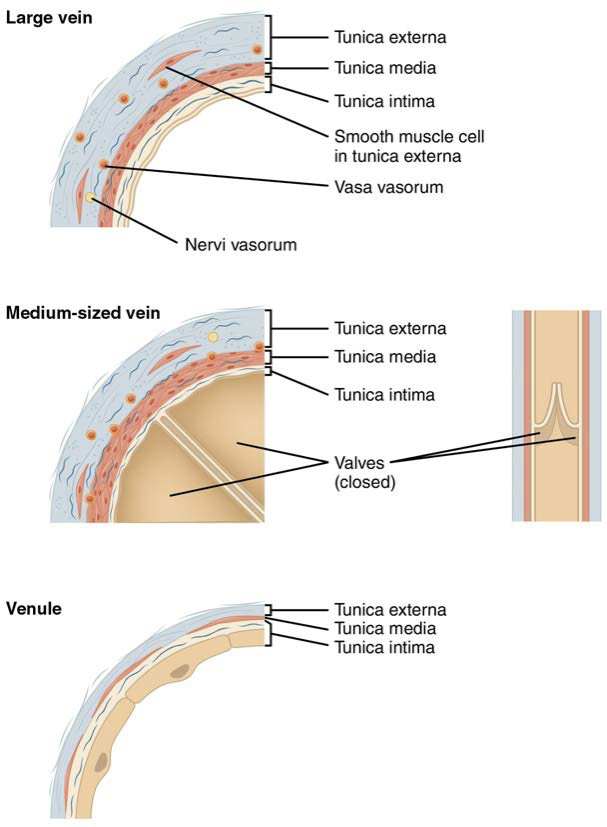
Blood vessels consist of three layers (tunics):
Tunica Intima: Innermost layer, smooth simple squamous endothelium reduces friction.
internal elastic membrane: a layer within the tunica intima that allows for flexibility and expansion of the blood vessel during fluctuations in blood pressure.
Tunica Media: Middle layer, thick in arteries with smooth muscle that controls vasoconstriction and vasodilation.
vasoconstriction: the narrowing of blood vessels due to contraction of the vascular smooth muscle, which increases blood pressure and reduces blood flow to certain areas of the body.
vasodilation: the widening of blood vessels as a result of relaxation of vascular smooth muscle, which decreases blood pressure and increases blood flow to specific regions, facilitating better tissue perfusion.
nervi vasorum: Small nerves that supply the blood vessels, providing them with the necessary stimuli to regulate their tone and maintain consistent blood flow.
external elastic membrane: the layer of elastic tissue found in larger blood vessels, specifically the arteries, which allows for expansion and recoil during the pulsatile flow of blood, thereby maintaining blood pressure.
Tunica Externa: Outermost layer, connective tissue providing structural support.
thickest layer of veins
Types of Blood Vessels
Arteries: Carry blood away from the heart. They have thicker walls and smaller lumens to withstand higher pressure.
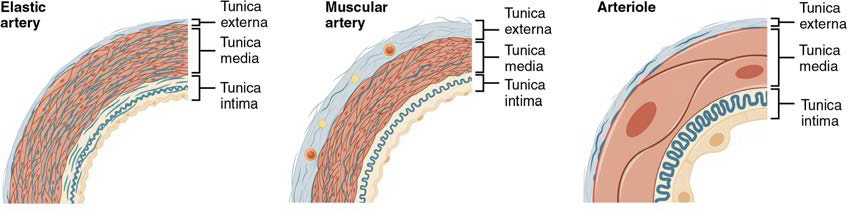
Elastic Arteries: Larger arteries like the aorta, contain elastic tissue that allows expansion during high systolic pressure and recoil during diastole.
Muscular Arteries: Medium-sized arteries that control blood flow distribution by vasoconstriction.
Arterioles: Smallest branches of arteries leading to capillaries; play a key role in regulating blood flow and pressure.
Capillaries: Microscopic vessels where exchange occurs.
perfusion: the process of delivering oxygen and nutrients to tissues through the capillary network, ensuring optimal cellular function and metabolic activity.
microcirculation: the circulation of blood in the smallest blood vessels, including capillaries and arterioles, which is crucial for the exchange of gases, nutrients, and waste products between blood and surrounding tissues.
Comprised of a single cell layer (tunica intima). Three types:
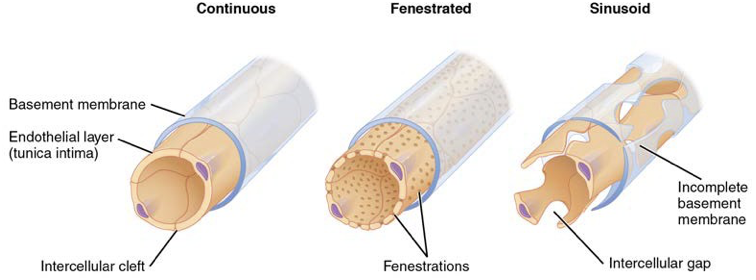
Continuous Capillaries: Most common type, with tight junctions allowing for limited transport.
endothelial lining
Fenestrated Capillaries: Contain pores for increased permeability, found in kidneys and intestines.
Sinusoidal Capillaries: Have large gaps allowing for the passage of larger molecules, found in the liver and spleen.
least common type
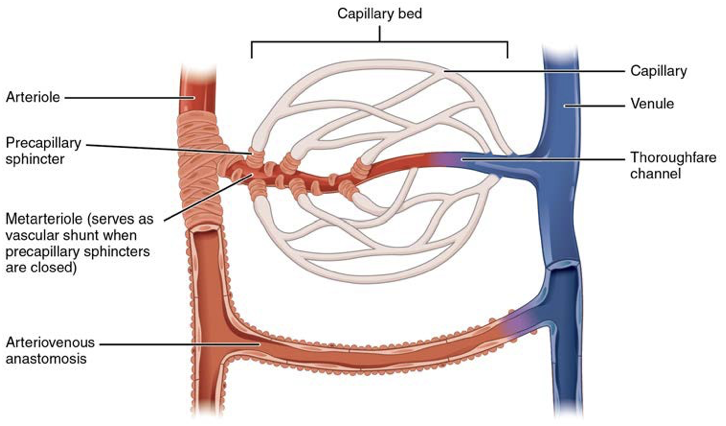
Metarterioles and Capillary Beds
Metarteriole: A short vessel that links arterioles to capillaries, playing a crucial role in regulating blood flow to tissues.
Capillary Bed: A network of capillaries that facilitates the exchange of gases, nutrients, and waste between blood and surrounding tissues.
precapillary sphincters: Small muscles located at the junctions of metarterioles and capillaries that regulate blood flow into capillary beds by constricting or relaxing, thus aiding in the control of perfusion according to tissue needs.
thoroughfare channel: A direct connection between metarterioles and venules that allows blood to bypass capillary beds during times of low metabolic demand.
vascular shunt: A vessel that connects arterioles directly to venules, providing an alternate route for blood flow and helping to regulate circulation in response to varying physiological demands.
arteriovenous anastomosis: A connection between an arteriole and a venule that allows blood to bypass capillary networks, facilitating rapid changes in blood flow and temperature regulation.
vasomotion: the process of contraction and relaxation of vascular smooth muscle that regulates blood vessel diameter, influencing blood flow and pressure within the circulatory system.
Veins: Return blood to the heart, have larger lumens and thinner walls than arteries. Many have valves to prevent backflow
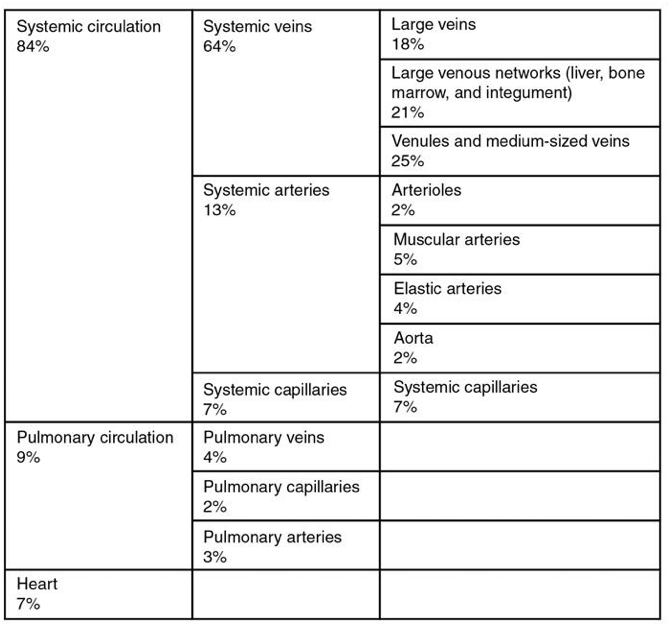
systemic veins contain around 64% of blood volume
they hold so much blood because they have high capacitance
they are capacitance vessels
venous reserve: the amount of blood stored in the venous system that can be mobilized during times of increased demand, such as exercise or hemorrhage.
Venules: Small vessels merging from capillaries, eventually leading to veins.
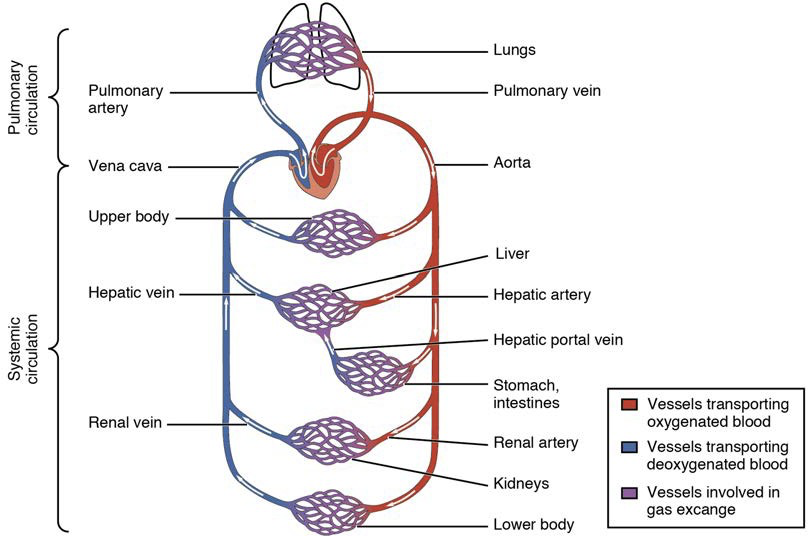
Systemic and Pulmonary Circulation
Systemic Circulation: Carries oxygen-rich blood from the left heart to tissues and returns deoxygenated blood to the right heart.
Pulmonary Circulation: Transports deoxygenated blood from the right heart to the lungs and returns oxygenated blood to the left heart.
Blood Flow, Blood Pressure, and Resistance
Blood Flow Dynamics
Blood Flow: Movement through vessels, driven by pressure gradients.
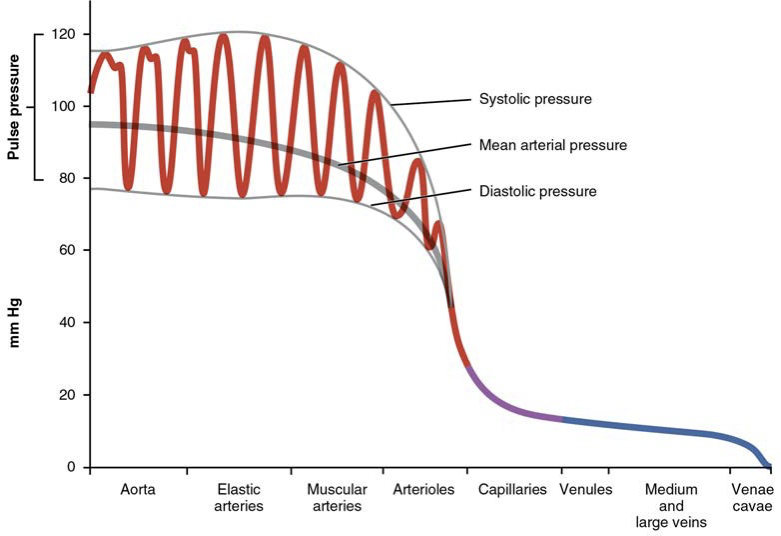
Blood Pressure: Force exerted by blood on vessel walls, measured in mm Hg (systolic over diastolic).
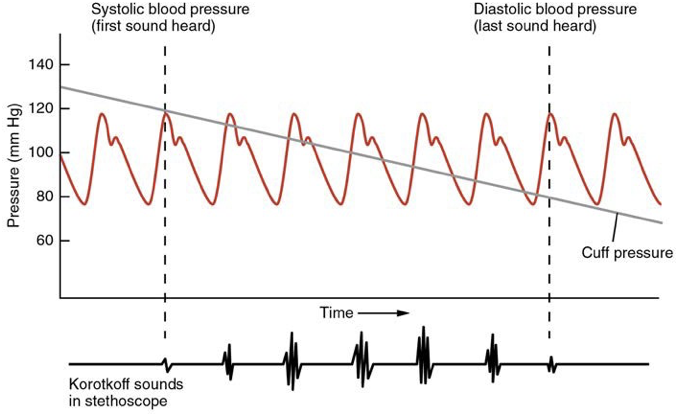
systolic pressure: the maximum pressure in the arteries during ventricular contraction, indicating the strength of heart contraction and overall cardiac output. (120mm HG)
diastolic pressure: the minimum pressure in the arteries during ventricular relaxation, reflecting the resistance of blood vessels and ensuring continuous blood flow to tissues (80 mm Hg).
pulse pressure: the difference between systolic and diastolic pressure, serving as an indicator of the health of the cardiovascular system (e.g., 40 mm Hg in a normal adult).
mean arterial pressure: the average pressure in a person's arteries during one cardiac cycle, calculated using the formula MAP = DBP + 1/3(PP), where DBP is diastolic blood pressure and PP is pulse pressure (normal range is approximately 70-100 mm Hg).
Resistance: Opposition to flow caused by friction between blood and vessel walls.
Key factors include vessel diameter (r), vessel length (l), and blood viscosity (η).
Poiseuille's Law: Q = \pi\frac{(P)(r^4)}{8l\eta} where Q = flow, P = pressure difference, r = radius, l = length, η = viscosity.
Pulse: the rhythmic expansion and contraction of the arteries as blood is pumped through them by the heart, serving as an important indicator of cardiovascular health.
Measurement of blood pressure
Koroktoff sounds: the series of sounds heard through a stethoscope during the measurement of blood pressure, which indicate the phases of blood pressure as the cuff is gradually deflated.
Sphygmomanometer: an instrument used to measure blood pressure, utilizing the oscillations in the arterial wall to determine the systolic and diastolic pressures.
Variables Affecting Blood Flow
Cardiac Output: the volume of blood the heart pumps per minute, which is a critical factor influencing blood flow and overall cardiovascular health.
Compliance: the ability of blood vessels to expand and contract as needed to accommodate varying volumes of blood, playing a significant role in maintaining stable blood pressure and facilitating efficient circulation.
Blood Volume
hypovolemia: a condition characterized by a decreased volume of blood in the body, which can lead to insufficient blood flow and potential organ dysfunction.
caused by bleeding, dehydration, vomiting, severe burns
hypervolemia: a condition marked by an increased blood volume that can lead to elevated blood pressure and increased workload on the heart, potentially resulting in heart failure.
caused by water and sodium retention, heart failure, liver diseases, steroid treatments
Blood Viscosity: the thickness and stickiness of blood, which can be influenced by factors such as dehydration, high red blood cell count, and certain medical conditions. Elevated blood viscosity can impede blood flow, increasing the risk of cardiovascular problems such as thrombosis.
Vessel Length and Diameter
longer vessels have greater resistance and lower flow
short vessels have less resistance and greater flow
diameter of vessels depends on the type of vessel it is
diameter of vessels is proportional to their resistance
vascular tone: the degree of constriction experienced by the blood vessels as a response to various stimuli, influencing blood flow and pressure throughout the circulatory system.
Venous System
Venous System: The venous system is responsible for returning deoxygenated blood back to the heart, with key components including veins, venules, and the superior and inferior vena cavae.
skeletal muscle pump: a mechanism that aids in venous return by utilizing the contraction of skeletal muscles during physical activity to compress veins and push blood upward toward the heart.
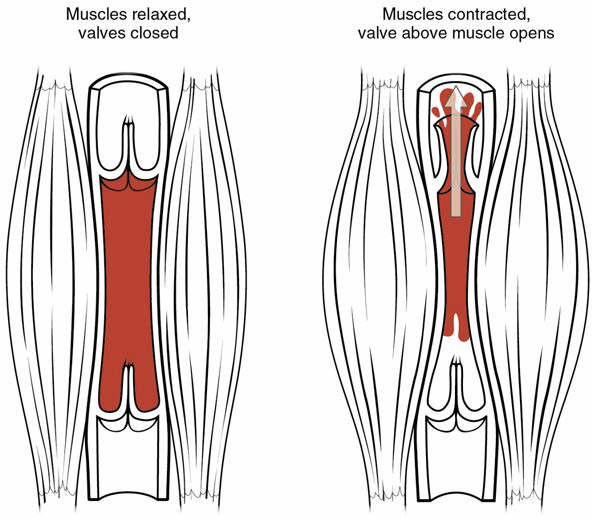
respiratory pump: a physiological mechanism that enhances venous return, particularly during breathing; as the diaphragm contracts and the thoracic cavity expands, it creates a negative pressure that draws blood into the thoracic veins and toward the heart.
blood pressure drops from venules to veins
vasoconstriction in the veins increases pressure and flow
Blood Flow Regulation
Neural Control: Autonomic nervous system influences vessel tone and thus blood flow and pressure.
Hormonal Control: Hormones like epinephrine and norepinephrine affect blood pressure and flow.
Local Control: Autoregulation by tissues responding to metabolic needs.
Significance of Blood Vessel Structure
Thicker walls in arteries allow for higher pressure capacity. Veins accommodate large blood volumes as capacitance vessels. The presence of valves in veins prevents backflow, especially in the extremities.
Vasa vasorum: Small vessels in larger vessels providing nourishment to the vessel's tissue.
Capillary Exchange
Bulk Flow
Fluid moves from high pressure in capillary bed to low pressure in tissue through filtration
Fluid moves from high pressure in tissue to low pressure in capillary bed through reabsorption
Hydrostatic Pressure: the pressure of any fluid enclosed in a space
Blood Hydrostatic Pressure: the force exerted by blood confined in blood vessels or heart chambers
Capillary Hydrostatic Pressure (CHP): pressure exerted by blood against the wall of a capillary
Interstitial Fluid Hydrostatic Pressure (IFHP): the pressure exerted by the fluid within the interstitial space that opposes the movement of fluid out of capillaries
Osmotic Pressure: the movement of fluid from the interstitial fluid back into the capillaries (reabsorption)
Blood Colloidal Osmotic Pressure (BCOP): the pressure created by the concentration of colloidal proteins in the blood
Interstitial Fluid Colloidal Osmotic Pressure (IFCOP): the osmotic pressure exerted by proteins in the interstitial fluid
Net Filtration Pressure (NFP): interaction of hydrostatic and osmotic pressure; NFP = CHP - BCOP (determines if fluid enters or exits the capillary).
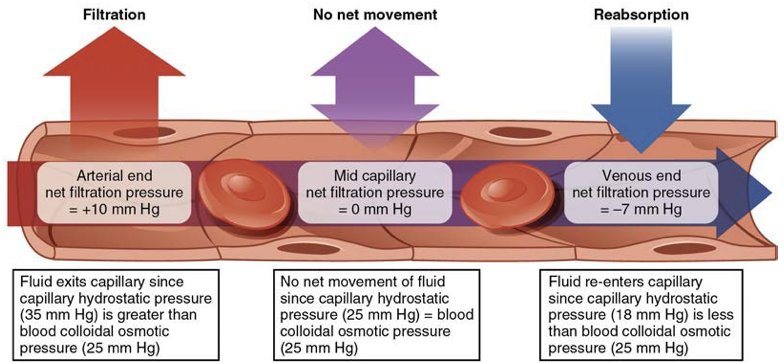
Excess fluid is picked up by capillaries in the lymphatic system
Homeostatic Regulation of the Vascular System
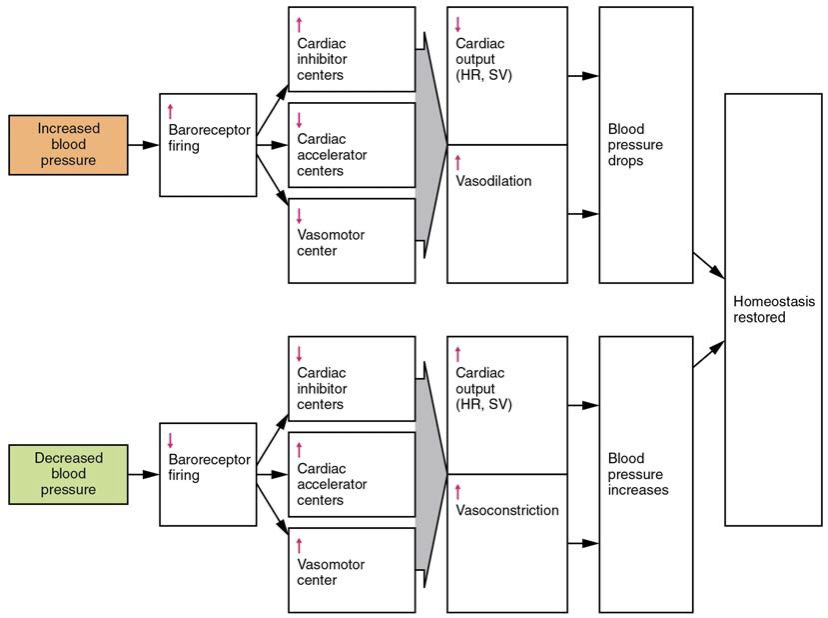
Three mechanisms maintain homeostasis: neural, endocrine, and autoregulation.
Neural Regulation: Baroreceptors and chemoreceptors provide feedback to the cardiovascular center.
Cardiovascular Center in the Brain
the cardiovascular centers located in the medulla oblongata play neurological regulation of blood pressure and flow
cardioaccelerator centers: stimulate cardiac function by regulating heart rate and stroke volume via sympathetic stimulation from accelerator nerve
cardioinhibitor centers: slow cardiac function by decreasing heart rate and stroke volume via parasympathetic stimulation from the vagus nerve
vasomotor centers: control vessel tone or contraction of the smooth muscle in the tunica media; changes in diameter affect peripheral resistance and overall blood pressure, thus influencing blood flow distribution throughout the body.
Baroreceptor Reflexes
specialized stretch receptors located within the blood vessels and heart chambers that respond to a degree of stretch caused by the presence of blood
aortic sinuses: in the walls of ascending aorta
cartoid sinuses: in the base of the internal cartoid arteries
When blood pressure rises too high, the baroreceptors fire at a higher rate and trigger parasympathetic stimulation of the heart. Sympathetic stimulation of the peripheral arterioles will also decrease, resulting in vasodilation
When blood pressure drops too low, the rate of baroreceptor firing decreases. This will trigger an increase in sympathetic stimulation of the heart, causing cardiac output to increase
atrial reflex: A mechanism that helps regulate blood pressure; it involves the stretching of atrial walls due to increased venous return, which leads to reflexive adjustments in heart rate and blood vessel diameter.
Chemoreceptor Reflexes
monitor levels of oxygen, carbon dioxide, and hydrogen ions (pH)
chemoreceptors respond to increasing carbon dioxide and hydrogen ion levels (falling pH) by stimulating the cardioaccelerator and vasomotor centers, increasing cardiac output and constricting peripheral vessels to enhance blood flow to vital organs and improve oxygen delivery throughout the body.
Endocrine Regulation: Include hormones like ADH and the renin-angiotensin-aldosterone system, affecting blood volume and pressure.
Epinephrine and Norepinephrine: released by adrenal medulla and enhance and extend the body’s fight or flight response.
increase heart rate and force on contraction
redirect blood flow to essential organs, while simultaneously constricting less critical vessels, thus optimizing oxygen delivery during stressful situations.
Antidiuretic Hormone (ADH/vasopressin): produced by the hypothalamus and released from the posterior pituitary, plays a crucial role in regulating blood pressure by promoting water reabsorption in the kidneys, which helps to maintain blood volume and, consequently, blood flow during times of dehydration or significant fluid loss.
Renin-Angiotensin-Aldosterone System (RAAS): a hormone system that regulates blood pressure and fluid balance by controlling the constriction of blood vessels and the reabsorption of sodium and water in the kidneys, contributing to the maintenance of adequate circulating blood volume.
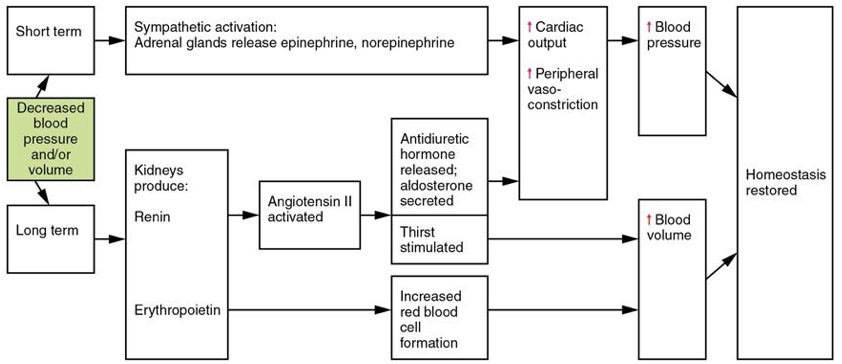
Erythropoietin (EPO): a hormone produced primarily by the kidneys, stimulates the production of red blood cells in the bone marrow in response to low oxygen levels, enhancing the blood's oxygen-carrying capacity.
Atrial Natriuretic Hormone: a peptide hormone produced by the cardiac atria that helps to lower blood pressure by promoting the excretion of sodium and water by the kidneys, thus decreasing blood volume and opposing the effects of aldosterone and angiotensin II.
Autoregulation: Local mechanisms respond to tissue metabolic needs.
Opening and contraction of precapillary sphincters are trigged by chemical signals
NO is a vasodilator released when opening
endothelins and vasoconstricitng peptides are released when contracting
Myogenic response: reaction to the stretching of the smooth muscle int he walls of arterioles as changes in the blood flow occur through the vessel
Exercise Impact
Physical activity increases heart rate, cardiac output, and redirects blood flow to muscles, heart, and lungs, improving overall cardiovascular health.
Clinical Considerations
Hypertension: A condition characterized by consistently elevated blood pressure, which can lead to increased risk of heart disease, stroke, and kidney damage if not managed effectively.
Hemorrhage: A serious medical condition involving excessive bleeding, either internally or externally, which can lead to hypovolemic shock and requires immediate medical intervention.
Circulatory Shock: A life-threatening condition resulting from inadequate blood flow to the body's tissues, leading to insufficient oxygen supply and organ dysfunction
Hypovolemic shock: A critical condition that arises when there is a significant loss of blood volume, often due to trauma or severe dehydration, resulting in decreased blood pressure and inadequate perfusion of tissues.
Cardiogenic shock: A condition that occurs when the heart is unable to pump effectively, resulting in a decreased cardiac output, which can lead to symptoms such as shortness of breath, rapid heartbeat, and confusion.
Vascular shock: A type of shock that occurs when there is widespread vasodilation, resulting in decreased peripheral resistance and leading to inadequate blood flow to vital organs.
Neurogenic shock: A form of vascular shock caused by damage to the spinal cord, leading to a disruption in the autonomic pathways and resultant loss of vascular tone, which can cause hypotension and bradycardia.
Anaphylactic shock: A severe and potentially life-threatening allergic reaction that leads to systemic vasodilation, increased vascular permeability, and difficulty breathing, usually triggered by exposure to allergens such as nuts, medications, or insect stings.
Septic shock: A serious condition that occurs as a result of a widespread infection, leading to systemic inflammation, vasodilation, and a significant drop in blood pressure, often associated with organ dysfunction.
Obstructive shock: A type of shock that occurs when blood flow is obstructed in the heart or major blood vessels, commonly resulting from conditions such as pulmonary embolism or cardiac tamponade, which can lead to decreased cardiac output and compromised tissue perfusion.
Circulatory Pathways
Blood flows from the heart via arteries to tissues, through capillaries for nutrient and gas exchange, and back to the heart through veins.
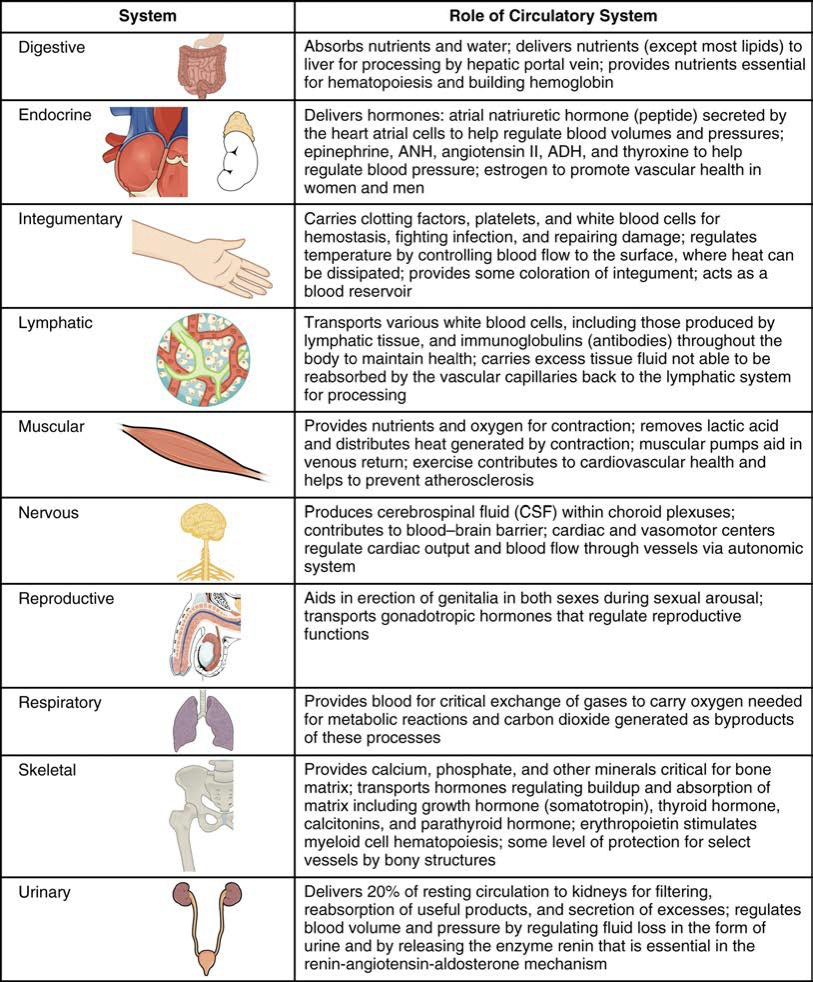
Pulmonary Circulation: The portion of the circulatory system that sends deoxygenated blood from the right side of the heart to the lungs for oxygenation and returns oxygenated blood back to the left side of the heart.
pulmonary circuit: the system of vessels in pulmonary circulation
pulmonary trunk: the large vessel that carries deoxygenated blood from the right ventricle of the heart to the lungs, where it branches into the left and right pulmonary arteries.
pulmonary arteries: the blood vessels that transport deoxygenated blood from the pulmonary trunk to the lungs for gas exchange.
pulmonary capillaries: The tiny blood vessels where the exchange of gases occurs, allowing carbon dioxide to be expelled and oxygen to enter the bloodstream.
pulmonary veins: the vessels that carry oxygenated blood from the lungs back to the left atrium of the heart, completing the pulmonary circuit.
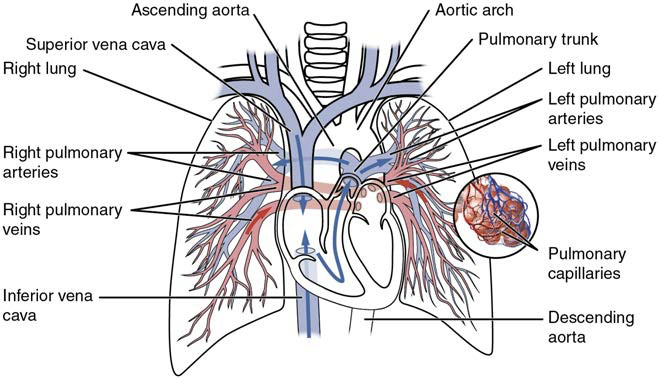
Systemic Arteries
Aorta: The largest artery in the body, responsible for carrying oxygen-rich blood from the left ventricle to distribute it to the rest of the body.
ascending aorta: the portion of the aorta that rises from the heart, directing oxygenated blood upward towards the head and arms.
aortic arch: the curve of the aorta that connects the ascending aorta to the descending aorta, giving rise to major arteries that supply blood to the head, neck, and arms.
descending aorta: the segment of the aorta that descends through the thorax and into the abdomen, delivering oxygenated blood to the lower body and vital organs.
aortic hiatus: the opening in the diaphragm through which the descending aorta passes as it transitions from the thoracic cavity into the abdominal cavity
thoracic aorta: the portion of the descending aorta that extends through the thoracic cavity, supplying blood to the thoracic organs and the upper parts of the body.
abdominal aorta: the section of the descending aorta that continues from the thoracic aorta into the abdominal cavity, providing oxygenated blood to the abdominal organs and lower limbs.
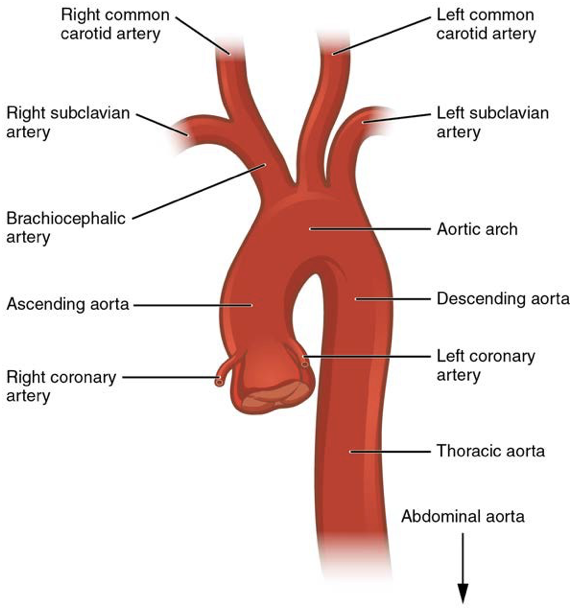
Coronary cirulcation: the flow of blood to and from the tissues of the heart, primarily through the coronary arteries and veins, ensuring that the myocardium receives the necessary oxygen and nutrients to function effectively.
Aortic Arch Branches
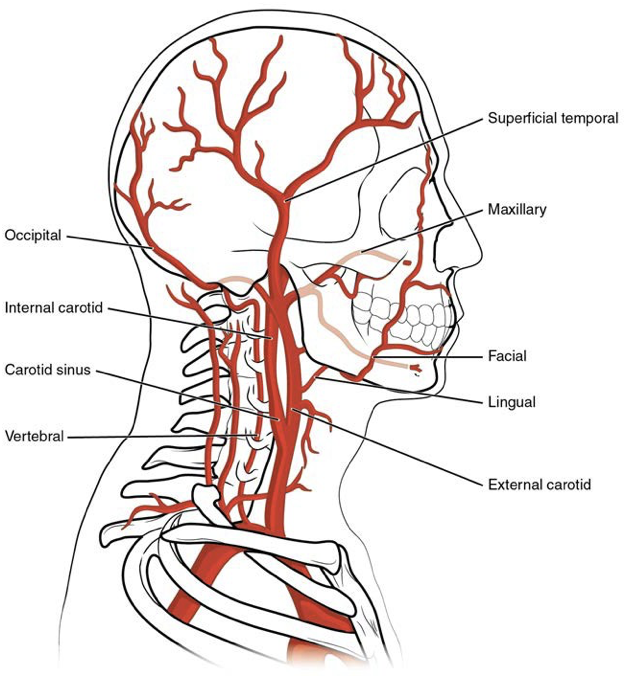
subclavian artery: the major artery that supplies blood to the arms and portions of the head and neck
internal thoracic artery: a branch of the subclavian artery that supplies blood to the anterior chest wall and breasts.
vertebral artery: a branch of the subclavian artery that supplies blood to the posterior portion of the brain and spinal cord.
thyrocervical artery: a branch of the subclavian artery that supplies blood to the thyroid gland, neck muscles, and part of the shoulder region.
common carotid artery: the artery that supplies blood to the brain, neck, and face
external carotid artery: the artery that branches from the common carotid artery, supplying blood to the face and neck regions.
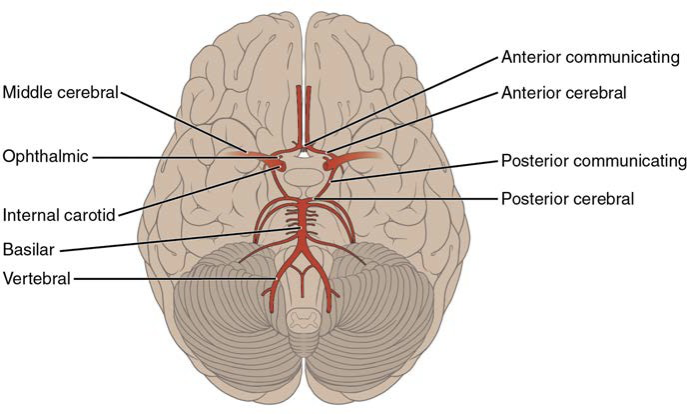
internal carotid artery: the artery that ascends the neck and supplies blood to the anterior part of the brain, with important branches extending to the eyes and forehead.
anterior cerebral artery: supplies blood to frontal lob of cerebrum
anterior communicating artery: connects the left and right anterior cerebral arteries, playing a crucial role in ensuring collateral circulation within the brain.
middle cerebral artery: supplies blood to temporal and parietal lobes
ophthalmic artery: supplies blood to eyes
basilar artery: a vital artery formed by the union of the two vertebral arteries, providing blood to the brainstem and cerebellum.
posterior cerebral artery: supplies blood to the occipital lobe and inferior part of the temporal lobe, playing a crucial role in vision.
Transient Ischemic Attack (TIA): a brief episode of neurological dysfunction caused by insufficient blood flow to the brain, often lasting only a few minutes and serving as a warning sign for a potential stroke.
Cerebrovascular Accident (CVA): a medical term for a stroke, which occurs when blood flow to a part of the brain is interrupted, leading to potential brain damage and neurological impairment.
Circle of Willis: a circulatory anastomosis that supplies blood to the brain and surrounding structures, providing a critical collateral circulation pathway in case of arterial occlusion.
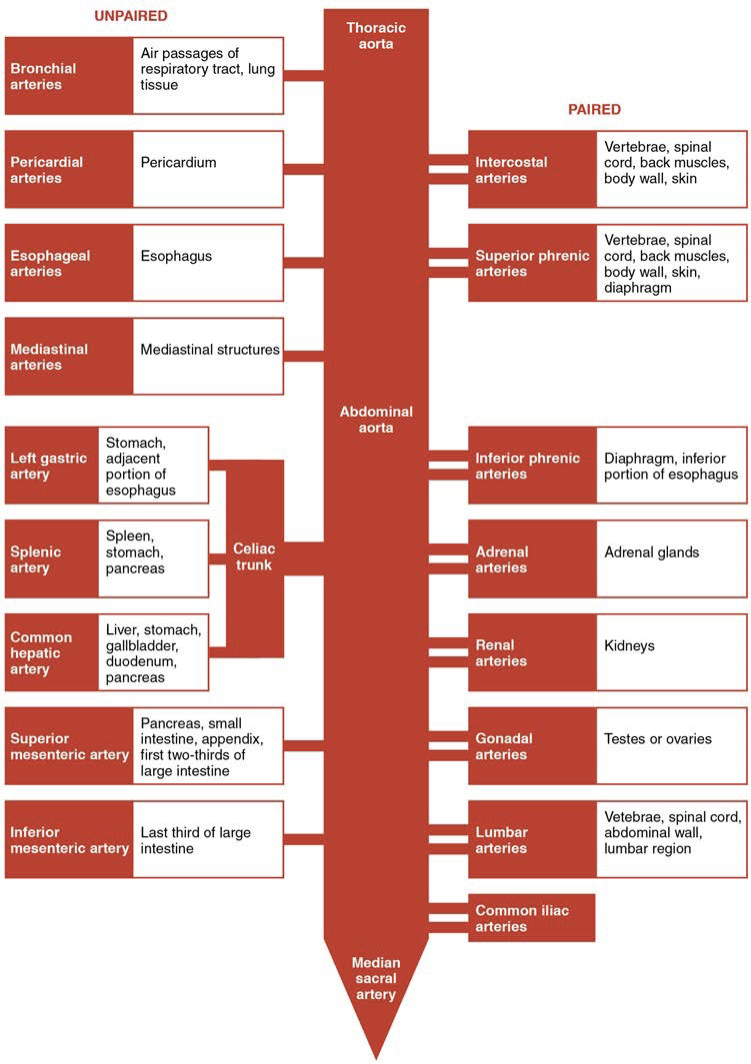
Thoracic Aorta & Major Branches
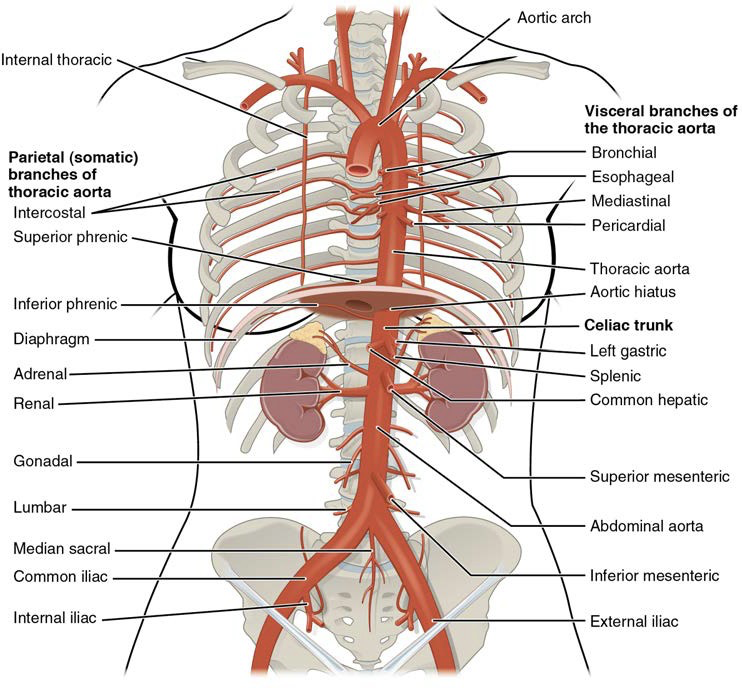
Visceral branches: A group of arterial branches of the thoracic aorta; supplies blood to the viscera (i.e., organs) of the thorax
Bronchial artery: A group of arterial branches of the thoracic aorta; supplies blood to the viscera (i.e., organs) of the thorax
Pericardial artery: Branch of the thoracic aorta; supplies blood to the pericardium
Esophageal artery: Branch of the thoracic aorta; supplies blood to the esophagus
Mediastin artery: Branch of the thoracic aorta; supplies blood to the mediastinum
Parietal branches: Also called somatic branches, a group of arterial branches of the thoracic aorta; include those that supply blood to the thoracic wall, vertebral column, and the superior surface of the diaphragm
Intercostal artery: Branch of the thoracic aorta; supplies blood to the muscles of the thoracic cavity and vertebral column
Superior phrenic artery: Branch of the thoracic aorta; supplies blood to the superior surface of the diaphragm
Abdominal Aorta & Major Branches
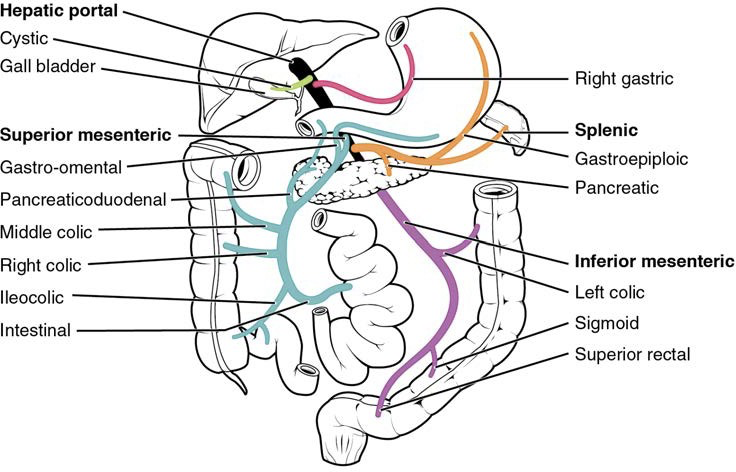
Celiac trunk: Also called the celiac artery; a major branch of the abdominal aorta; gives rise to the left gastric artery, the splenic artery, and the common hepatic artery that forms the hepatic artery to the liver, the right gastric artery to the stomach, and the cystic artery to the gall bladder
Left gastric artery: Branch of the celiac trunk; supplies blood to the stomach
Splenic artery: Branch of the celiac trunk; supplies blood to the spleen
Common hepatic artery: Branch of the celiac trunk that forms the hepatic artery, the right gastric artery, and the cystic artery
Hepatic artery proper: Branch of the common hepatic artery; supplies systemic blood to the liver
Right gastric artery: Branch of the common hepatic artery; supplies blood to the stomach
Cystic artery: Branch of the common hepatic artery; supplies blood to the gall bladder
Superior mesenteric artery: Branch of the abdominal aorta; supplies blood to the small intestine (duodenum, jejunum, and ileum), the pancreas, and a majority of the large intestine
Inferior mesenteric artery: Branch of the abdominal aorta; supplies blood to the distal segment of the large intestine and rectum
Inferior phrenic arteries: Branches of the abdominal aorta; supply blood to the inferior surface of the diaphragm
Adrenal artery: Branch of the abdominal aorta; supplies blood to the adrenal (suprarenal) glands
Renal artery: Branch of the abdominal aorta; supplies each kidney
Gonadal artery: Branch of the abdominal aorta; supplies blood to the gonads or reproductive organs; also described as ovarian arteries or testicular arteries, depending upon the sex of the individual
Ovarian artery: Branch of the abdominal aorta; supplies blood to ovary, uterine (Fallopian) tube, and uterus
Testicular artery: Branch of the abdominal aorta; ultimately travels outside the body cavity to the testes and forms one component of the spermatic cord
Lumbar arteries: Branches of the abdominal aorta; supply blood to the lumbar region, the abdominal wall, and spinal cordCommon iliac artery:
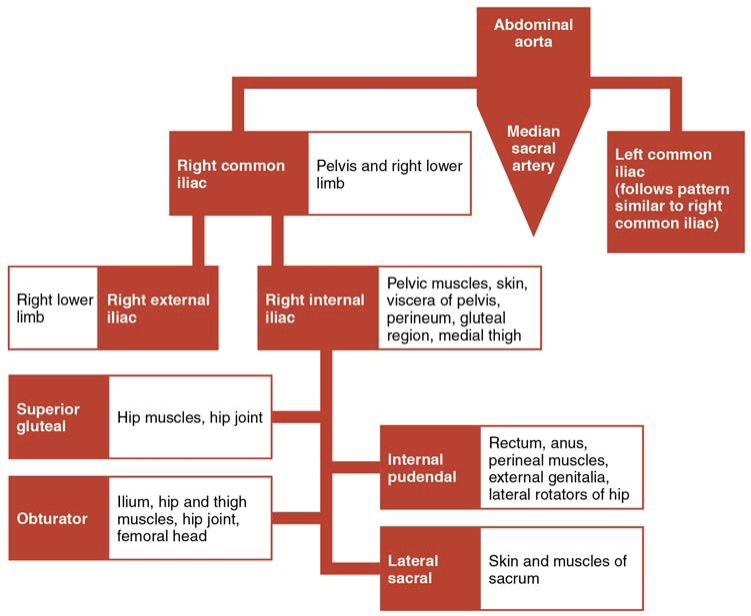
Common iliac artery: Branch of the aorta that leads to the internal and external iliac arteries
Median sacral artery: Continuation of the aorta into the sacrum
Internal iliac artery: Branch from the common iliac arteries; supplies blood to the urinary bladder, walls of the pelvis, external genitalia, and the medial portion of the femoral region; in females, also provides blood to the uterus and vagina
External iliac artery: Branch of the common iliac artery that leaves the body cavity and becomes a femoral artery; supplies blood to the lower limbs
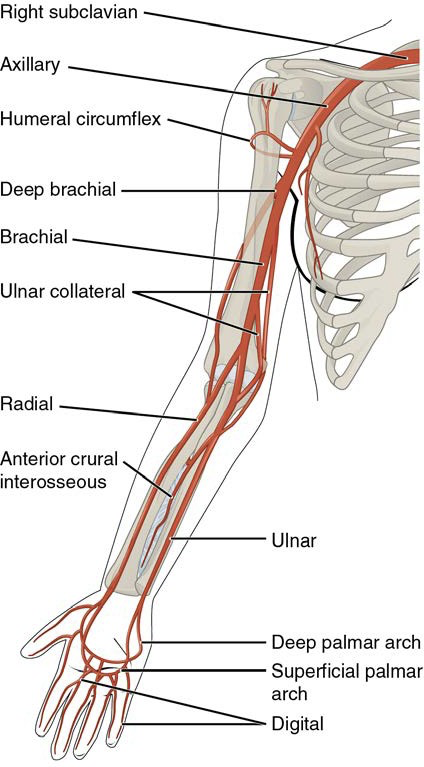
Arteries Serving Upper Limbs
Axillary artery: Continuation of the subclavian artery as it penetrates the body wall and enters the axillary region; supplies blood to the region near the head of the humerus (humeral circumflex arteries); the majority of the vessel continues into the brachium and becomes the brachial artery
Brachial artery: Continuation of the axillary artery in the brachium; supplies blood to much of the brachial region; gives off several smaller branches that provide blood to the posterior surface of the arm in the region of the elbow; bifurcates into the radial and ulnar arteries at the coronoid fossa
Radial artery: Formed at the bifurcation of the brachial artery; parallels the radius; gives off smaller branches until it reaches the carpal region where it fuses with the ulnar artery to form the superficial and deep palmar arches; supplies blood to the lower arm and carpal region
Ulnar artery: Formed at the bifurcation of the brachial artery; parallels the ulna; gives off smaller branches until it reaches the carpal region where it fuses with the radial artery to form the superficial and deep palmar arches; supplies blood to the lower arm and carpal region
Palmar arches (superficial and deep): Formed from anastomosis of the radial and ulnar arteries; supply blood to the hand and digital arteries
Digital arches: Formed from the superficial and deep palmar arches; supply blood to the digits
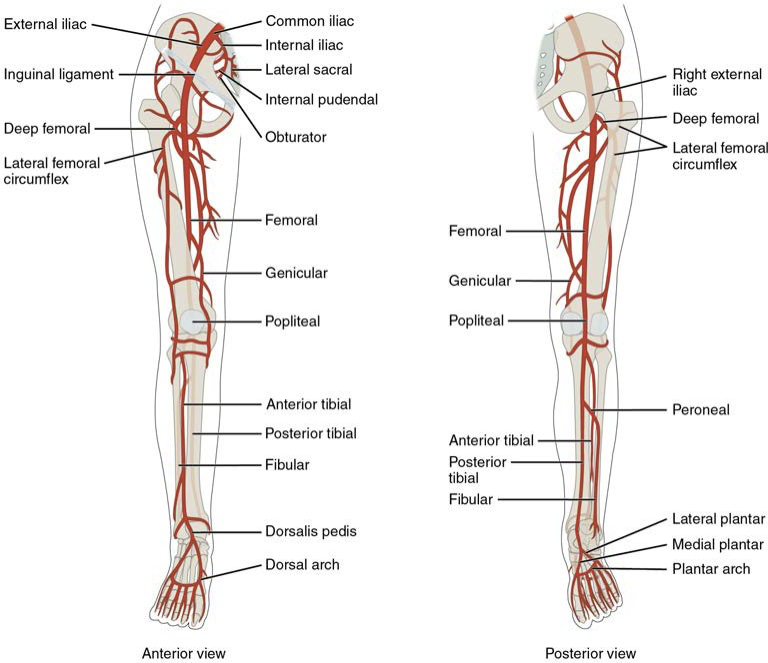
Arteries Serving Lower Limbs
Fermoral artery: Continuation of the external iliac artery after it passes through the body cavity; divides into several smaller branches, the lateral deep femoral artery, and the genicular artery; becomes the popliteal artery as it passes posterior to the knee
Deep femoral artery: Branch of the femoral artery; gives rise to the lateral circumflex arteries
Lateral circumflex artery: Branch of the deep femoral artery; supplies blood to the deep muscles of the thigh and the ventral and lateral regions of the integument
Genicular artery: Branch of the femoral artery; supplies blood to the region of the knee
Popliteal artery: Continuation of the femoral artery posterior to the knee; branches into the anterior and posterior tibial arteries
Anterior tibial artery: Branches from the popliteal artery; supplies blood to the anterior tibial region; becomes the dorsalis pedis artery
Dorsalis pedis artery: Forms from the anterior tibial artery; branches repeatedly to supply blood to the tarsal and dorsal regions of the foot
Posterior tibial artery: Forms from the anterior tibial artery; branches repeatedly to supply blood to the tarsal and dorsal regions of the foot
Medial plantar artery: Arises from the bifurcation of the posterior tibial arteries; supplies blood to the medial plantar surfaces of the foot
Lateral plantar artery: Arises from the bifurcation of the posterior tibial arteries; supplies blood to the lateral plantar surfaces of the foot
Dorsal or arcuate arch: Formed from the anastomosis of the dorsalis pedis artery and the medial and plantar arteries; branches supply the distal portions of the foot and digits
Plantar arch: Formed from the anastomosis of the dorsalis pedis artery and the medial and plantar arteries; branches supply the distal portions of the foot and digits
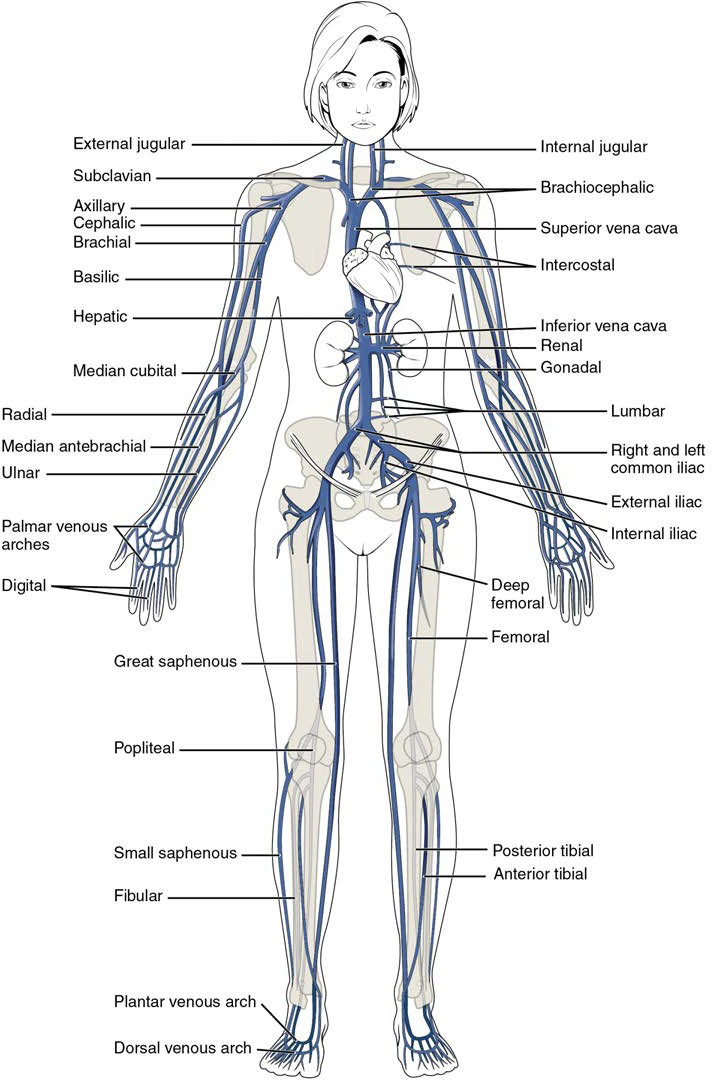
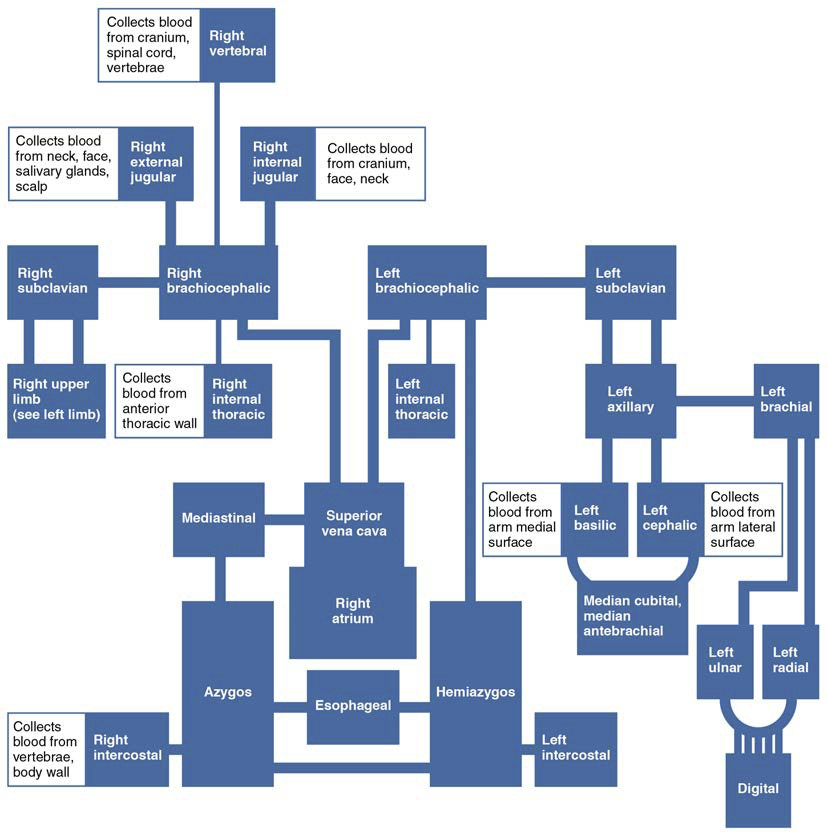
Systemic Veins
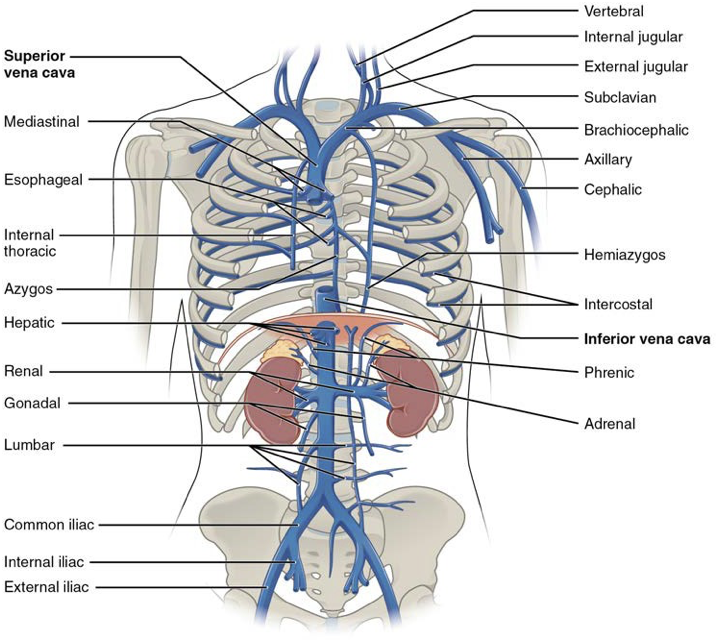
Veins of Thoracic Region
The Superior Vena Cava: Large systemic vein; drains blood from most areas superior to the diaphragm; empties into the right atrium
Subclavian vein: Located deep in the thoracic cavity; formed by the axillary vein as it enters the thoracic cavity from the axillary region; drains the axillary and smaller local veins near the scapular region and leads to the brachiocephalic vein
Brachiocephalic veins: Pair of veins that form from a fusion of the external and internal jugular veins and the subclavian vein; subclavian, external and internal jugulars, vertebral, and internal thoracic veins flow into it; drain the upper thoracic region and lead to the superior vena cava
Vertebral veins: Arises from the base of the brain and the cervical region of the spinal cord; passes through the intervertebral foramina in the cervical vertebrae; drains smaller veins from the cranium, spinal cord, and vertebrae, and leads to the brachiocephalic vein; counterpart of the vertebral artery
Internal thoracic veins: Also called internal mammary veins; drain the anterior surface of the chest wall and lead to the brachiocephalic vein
Intercostal vein: Drains the muscles of the thoracic wall and leads to the azygos vein
Esophageal vein; Drains the inferior portions of the esophagus and leads to the azygos vein
Bronchial vein: Drains the systemic circulation from the lungs and leads to the azygos vein
Azygos vein: Originates in the lumbar region and passes through the diaphragm into the thoracic cavity on the right side of the vertebral column; drains blood from the intercostal veins, esophageal veins, bronchial veins, and other veins draining the mediastinal region, and leads to the superior vena cava
Hemiazygos vein: Smaller vein complementary to the azygos vein; drains the esophageal veins from the esophagus and the left intercostal veins, and leads to the brachiocephalic vein via the superior intercostal vein
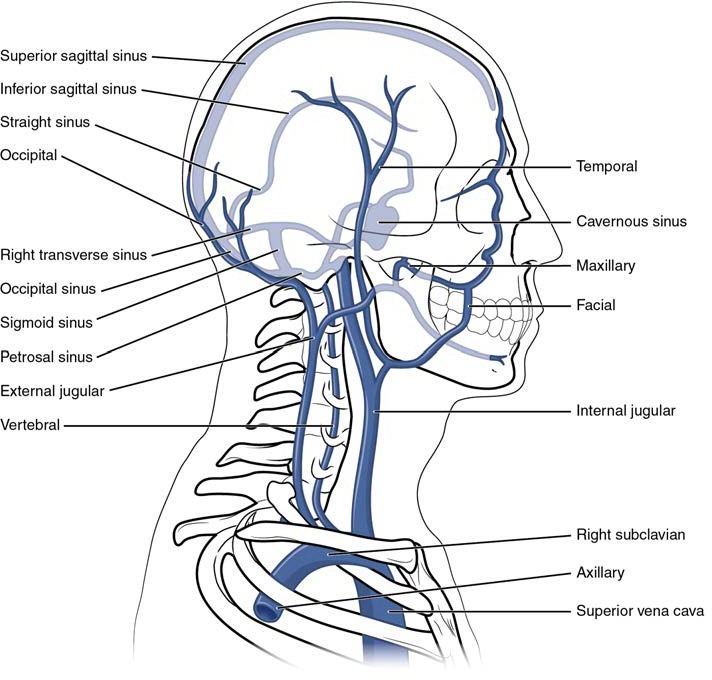
Veins of Head and Neck
Internal jugular vein: Parallel to the common carotid artery, which is more or less its counterpart, and passes through the jugular foramen and canal; primarily drains blood from the brain, receives the superficial facial vein, and empties into the subclavian vein
Temporal vein: Drains blood from the temporal region and flows into the external jugular vein
Maxillary vein: Drains blood from the maxillary region and flows into the external jugular vein
External jugular vein: Drains blood from the more superficial portions of the head, scalp, and cranial regions, and leads to the subclavian vein
Veins of the Brain
Superior sagittal sinus: Enlarged vein located midsagittally between the meningeal and periosteal layers of the dura mater within the falx cerebri; receives most of the blood drained from the superior surface of the cerebrum and leads to the inferior jugular vein and the vertebral vein
Great cerebral vein: Receives most of the smaller vessels from the inferior cerebral veins and leads to the straight sinus
Straight sinus: Enlarged vein that drains blood from the brain; receives most of the blood from the great cerebral vein and leads to the left or right transverse sinus
Cavernous sinus: Enlarged vein that receives blood from most of the other cerebral veins and the eye socket, and leads to the petrosal sinus
Petrosal sinus: Enlarged vein that receives blood from the cavernous sinus and leads into the internal jugular veins
Occipital sinus: Enlarged vein that drains the occipital region near the falx cerebelli and leads to the left and right transverse sinuses, and also the vertebral veins
Transverse sinuses: Pair of enlarged veins near the lambdoid suture that drains the occipital, sagittal, and straight sinuses, and leads to the sigmoid sinuses
Sigmoid sinuses: Enlarged vein that receives blood from the transverse sinuses and leads through the jugular foramen to the internal jugular vein
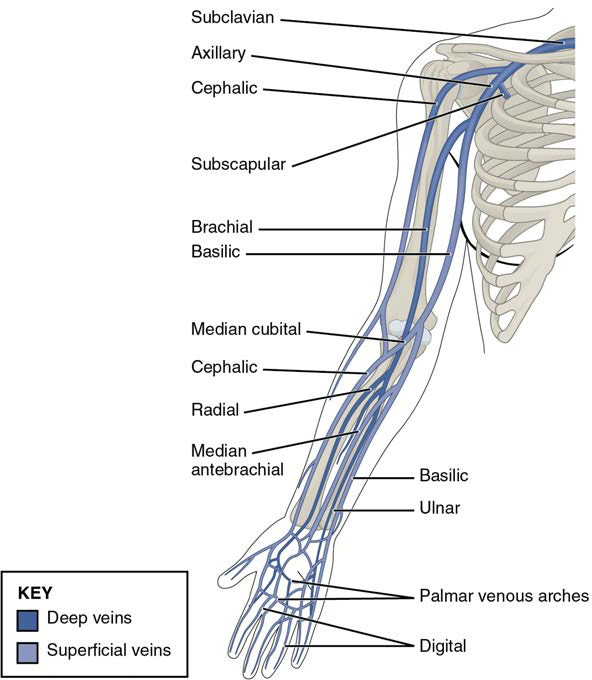
Veins of Upper Limbs
Digital veins: Drain the digits and lead to the palmar arches of the hand and dorsal venous arch of the foot
Palmar venous arches: Drain the hand and digits, and lead to the radial vein, ulnar veins, and the median antebrachial vein
Radial vein: Vein that parallels the radius and radial artery; arises from the palmar venous arches and leads to the brachial vein
Ulnar vein: Vein that parallels the ulna and ulnar artery; arises from the palmar venous arches and leads to the brachial vein
Brachial vein: Deeper vein of the arm that forms from the radial and ulnar veins in the lower arm; leads to the axillary vein
Median antebrachial vein: Vein that parallels the ulnar vein but is more medial in location; intertwines with the palmar venous arches; leads to the basilic vein
Basilic vein: Superficial vein of the arm that arises from the median antebrachial vein, intersects with the median cubital vein, parallels the ulnar vein, and continues into the upper arm; along with the brachial vein, it leads to the axillary vein
Median cubital vein: Superficial vessel located in the antecubital region that links the cephalic vein to the basilic vein in the form of a v; a frequent site from which to draw blood
Cephalic vein: Superficial vessel in the upper arm; leads to the axillary vein
Subscapular vein: Drains blood from the subscapular region and leads to the axillary vein
Axillary vein: The major vein in the axillary region; drains the upper limb and becomes the subclavian vein
Veins of Abdominal Region
Inferior Vena Cava: Large systemic vein that drains blood from areas largely inferior to the diaphragm; empties into the right atrium
Lumbar veins: Series of veins that drain the lumbar portion of the abdominal wall and spinal cord; the ascending lumbar veins drain into the azygos vein on the right or the hemiazygos vein on the left; the remaining lumbar veins drain directly into the inferior vena cava
Renal veins: Largest vein entering the inferior vena cava; drains the kidneys and flows into the inferior vena cava
Adrenal veins: Drains the adrenal or suprarenal; the right adrenal vein enters the inferior vena cava directly and the left adrenal vein enters the left renal vein
Testicular veins: Drains the testes and forms part of the spermatic cord; the right testicular vein empties directly into the inferior vena cava and the left testicular vein empties into the left renal vein
Ovarian vein: Drains the ovary; the right ovarian vein empties directly into the inferior vena cava and the left ovarian vein empties into the left renal vein
Gonadal vein: Generic term for a vein draining a reproductive organ; may be either an ovarian vein or a testicular vein, depending on the sex of the individual
Phrenic veins: Drains the diaphragm; the right phrenic vein flows into the inferior vena cava and the left phrenic vein empties into the left renal vein
Hepatic vein: Drains systemic blood from the liver and flows into the inferior vena cava
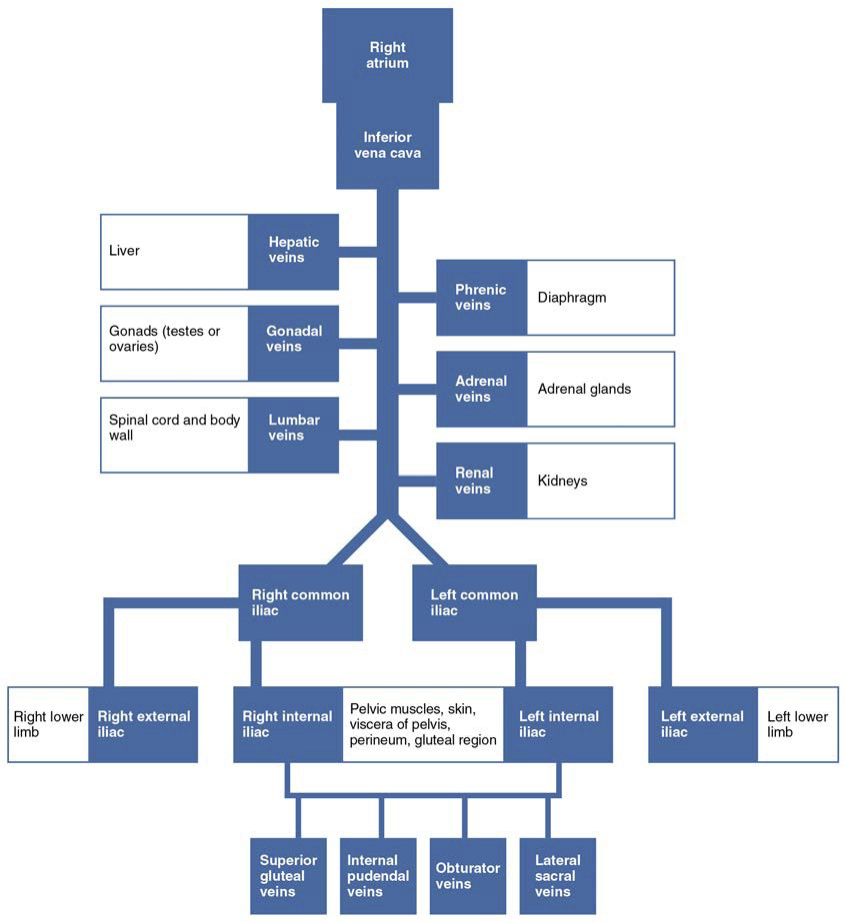
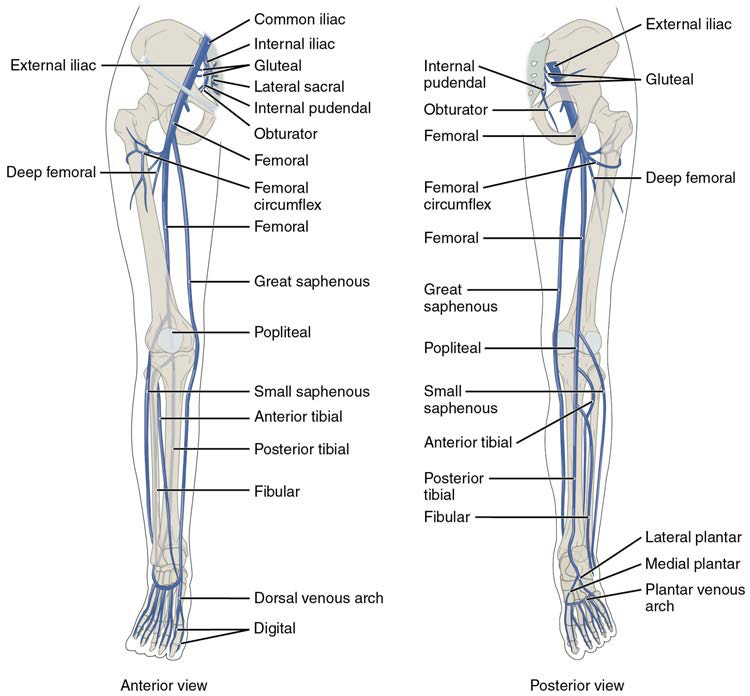
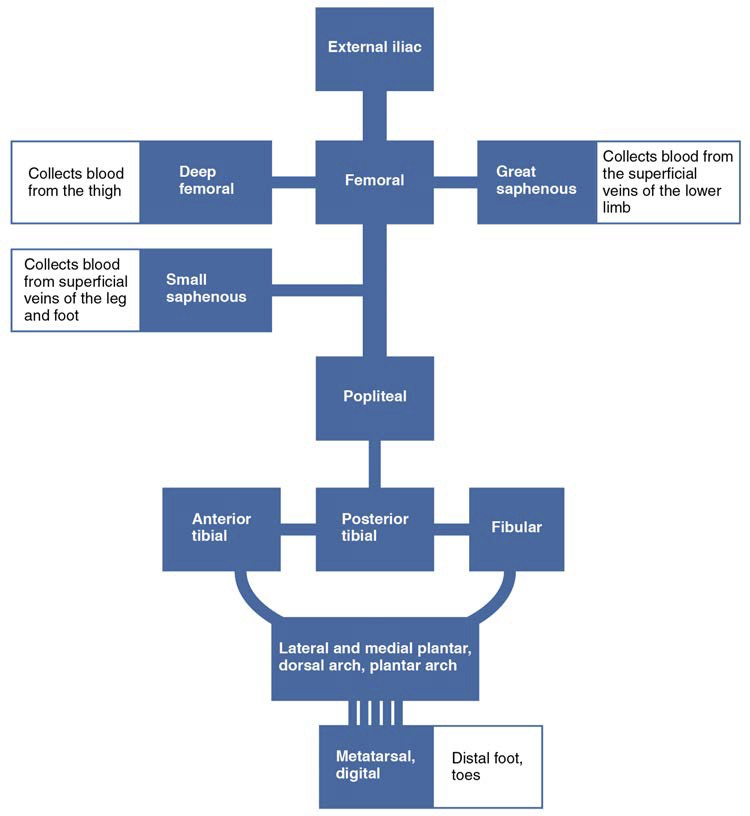
Veins of Lower Limbs
Plantar veins: Drain the foot and flow into the plantar venous arch
Dorsal venous arch: Drains blood from digital veins and vessels on the superior surface of the foot
Plantar venous arch: Formed from the plantar veins; flows into the anterior and posterior tibial veins through anastomoses
Anterior tibial vein: Formed from the dorsal venous arch; drains the area near the tibialis anterior muscle and flows into the popliteal vein
Posterior tibial vein: Formed from the dorsal venous arch; drains the area near the posterior surface of the tibia and flows into the popliteal vein
Fibular vein: Drains the muscles and integument near the fibula and flows into the popliteal vein
Small saphenous vein: Located on the lateral surface of the leg; drains blood from the superficial regions of the lower leg and foot, and flows into the popliteal vein
Popliteal vein: Drains the region behind the knee and forms from the fusion of the fibular, anterior, and posterior tibial veins; flows into the femoral vein
Great saphenous vein: Prominent surface vessel located on the medial surface of the leg and thigh; drains the superficial portions of these areas and flows into the femoral vein
Deep femoral vein: Drains blood from the deeper portions of the thigh and flows into the femoral vein
Femoral circumflex vein: Forms a loop around the femur just inferior to the trochanters; drains blood from the areas around the head and neck of the femur; flows into the femoral vein
Femoral vein: Drains the upper leg; receives blood from the great saphenous vein, the deep femoral vein, and the femoral circumflex vein; becomes the external iliac vein when it crosses the body wall
External iliac vein: Formed when the femoral vein passes into the body cavity; drains the legs and flows into the common iliac vein
Internal iliac vein: Drains the pelvic organs and integument; formed from several smaller veins in the region; flows into the common iliac vein
Middle sacral vein: Drains the sacral region and flows into the left common iliac vein
Common iliac vein: Flows into the inferior vena cava at the level of L5; the left common iliac vein drains the sacral region; formed from the union of the external and internal iliac veins near the inferior portion of the sacroiliac joint
Hepatic Portal System: Drains blood from the digestive organs and spleen to the liver; composed of the superior mesenteric vein and the splenic vein that converge to form the hepatic portal vein, allowing for the processing of nutrients before they enter the systemic circulation.
Major Systemic Circulation Vessels
Aorta branches include:
Common carotid arteries.
Subclavian arteries.
Celiac trunk.
Renal arteries.
Iliac arteries (common, internal, external).
Major veins returning blood to the heart:
Superior and inferior vena cavae.
Brachiocephalic veins.
Renal veins.
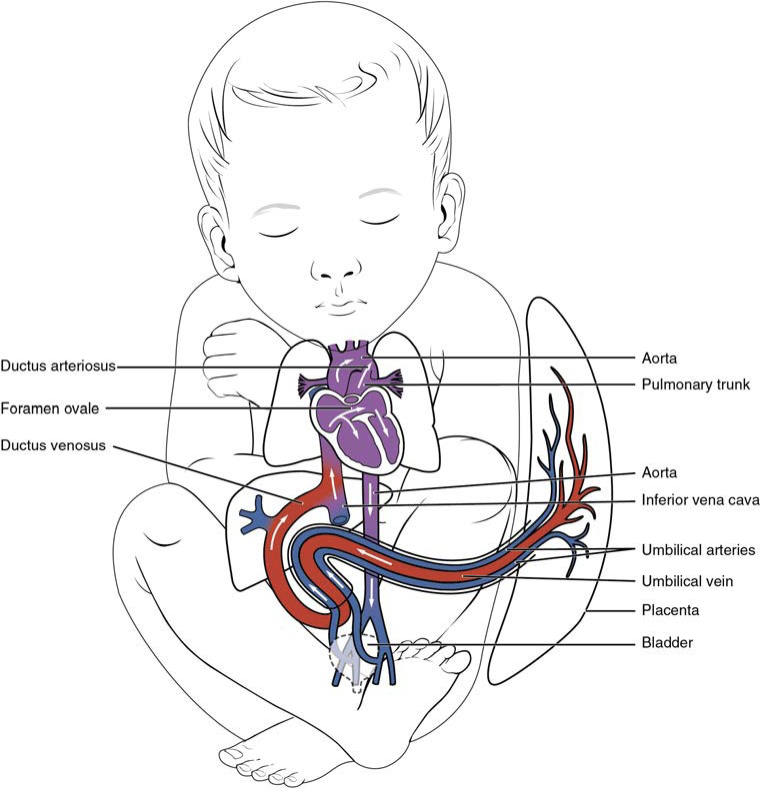
Development of Blood Vessels and Fetal Circulation
Hemangioblasts: precursor cells involved in the formation of blood vessels as well as blood cells, playing a crucial role during embryonic development.
Angioblasts: specialized cells that contribute to the formation of blood vessels by differentiating into endothelial cells, thus forming the inner lining of the vascular system.
Blood islands: clusters of hematopoietic and endothelial precursor cells that aggregate during embryonic development, leading to the formation of blood vessels and red blood cells.
Vascular tubes: structures that emerge from blood islands, which eventually fuse to establish a network of blood vessels throughout the developing organism.
Angiogenesis: the process by which new blood vessels form from existing vessels, playing a crucial role in growth, development, and wound healing.
Umbilical vein: a vital blood vessel that carries oxygenated blood from the placenta to the embryo, ensuring the delivery of essential nutrients and oxygen during gestation.
Umbilical arteries: branches that carry deoxygenated blood from the embryo back to the placenta, facilitating the exchange of waste products and carbon dioxide for oxygen and nutrients.
Foramen ovale: a fetal shunt that allows blood to bypass the non-functioning lungs by flowing directly from the right atrium to the left atrium, thus ensuring efficient circulation of oxygenated blood in the developing fetus.
Ductus arteriosus: a short connection between the pulmonary artery and the aorta that allows blood to bypass the pulmonary circulation, further optimizing the distribution of oxygenated blood throughout the body prior to birth.
Ductus venosus: a vessel that serves to divert a portion of the umbilical vein's blood away from the liver directly into the inferior vena cava, ensuring that oxygen-rich blood is delivered efficiently to the heart and brain of the fetus.
Blood vessels form from mesoderm in embryos; shunts in fetal circulation (foramen ovale, ductus arteriosus, ductus venosus) redirect blood to bypass nonfunctional lungs.
After birth, these shunts close, and normal circulation patterns are established.
Key Concepts Summary
Vascular structure importance in function; regulation of blood flow and pressure is critical in maintaining homeostasis.