Lectures 1-4
Lecture 1: Fundamentals of Fixed Partial Dentures
Fixed Partial Denture (FPD)
aka “bridge”
naming/describing: material+ FPD + designate pontic with “p” [ex: metal ceramic FPD #18-19p-20]
goes on teeth or implants to replace missing teeth in a partially edentulous arch; CANNOT be removed by the patient
comparing tooth replacement options:
FPD: tooth supported fixed partial denture (bridge)
Implants: either an implant supported single crown OR implant supported fixed partial denture
RPD: removable partial denture
functions of FPD
to replace missing teeth
provide proper occlusal function
maintain arch integrity/tooth position
maintain occlusal relationship
restore function, esthetics, and speech
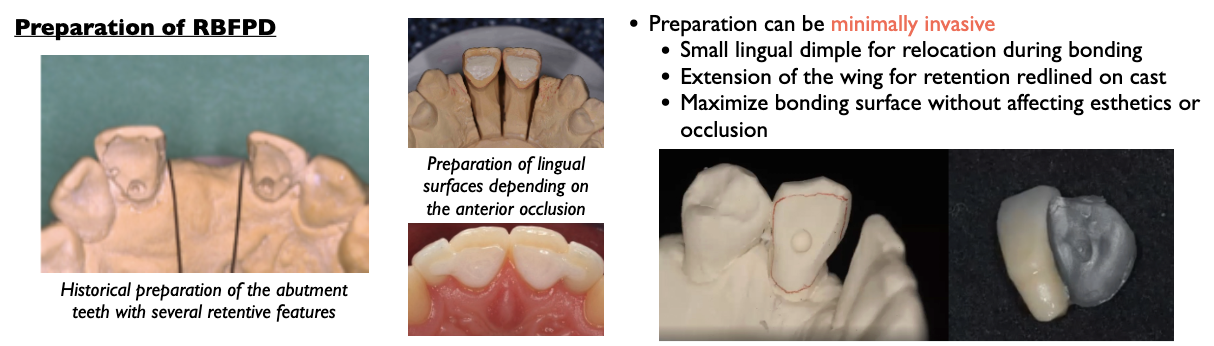
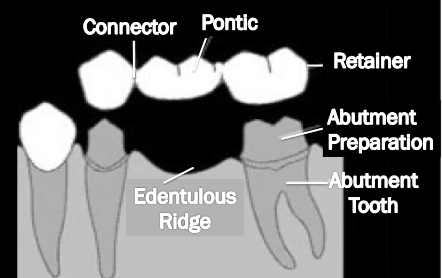
Defining terminology
abutment= a tooth/implant serving as an attachment for a fixed partial denture (Bridge)
pontic= the artificial tooth on a FPD that replaces the missing natural tooth to restore function
retainer= extra-coronal restorations that are cemented to or otherwise attached to the abutment teeth or implants in a FPD
connectors= the portion of a fixed partial denture that unites the retainers and the pontic
Types of Pontics
saddle
modified ridge lap
ovate
conical
hygienic
bounded vs cantilevered pontics
bounded=supported on both ends; both ends are retainers
cantilevered= supported on one end but not the other
Connectors
the part connecting the retainer tot he pontic
rigid vs non-rigid connector
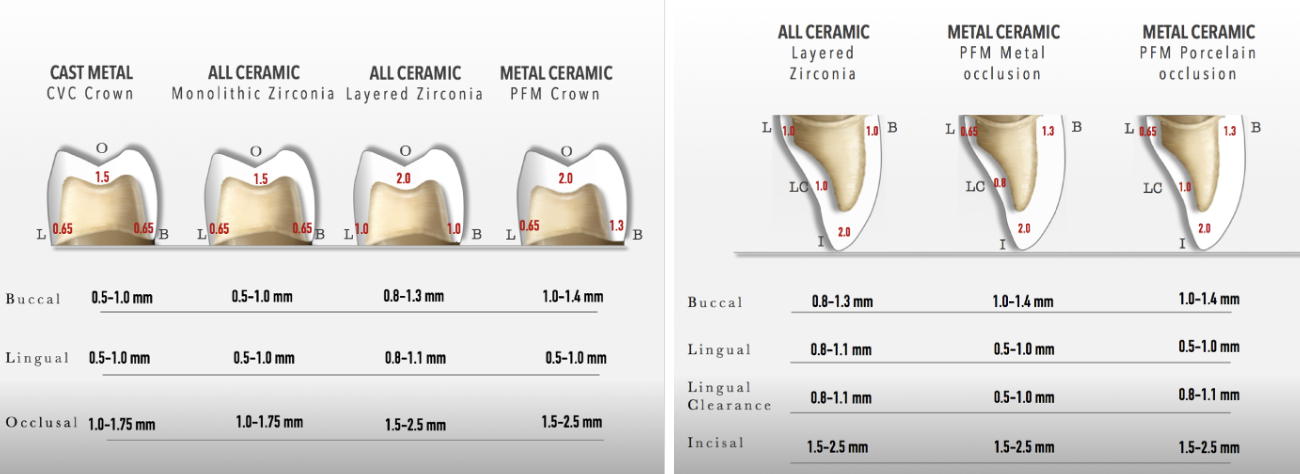
Principles of Tooth Preparation
in tooth supported FPDs the abutments (tooth) must be prepared to receive the retainers (crown)
preservation of tooth structure
aims to preserve as much sound tooth structure as possible and preserve the pulpal vitality
we must remove structure for caries and defects, to provide room for the restoration bulk, for proper POI retention and resistance, and for esthetics
outline of preparation
clinically the outline will be determined by existing restorations, caries, defects, esthetics, and retention
sim lab: 0.65mm supraginigival, 0.5mm gingival separation, and no damage to adjacent teeth or gingiva
internal reduction
avoid unnecessary removal of sound tooth structure but prep must also provide space for the necessary bulk of the restorative material
marginal integrity
margin of restoration closely adapted to finish line of the preparation= margins sealed when restoration is fully seated
finish line must terminate on sound tooth structure
appropriate margin design/configuration
well supported, clear, smooth and continuous
preservation of the periodontium
we prevent over-contouring by reduce enough gingival-axially which gives space for the material
over-contouring causes food impaction & irritation to the periodontium
supra-gingival finish lines aid in visual accessibility
sub-ginigval finish lines irritate the periodontium and cause plaque accumulation bc its harder to clean
sub-gingival finish lines acceptable- caries or defect go below the gingiva; to aid in retention for wall height
must be wary when placing sub-gingival finish lines- sealing the margins; invasion of biological width (avg 2mm)
retention and resistance
retention- prevent displacement along path of insertion
resistance- prevent displacement along planes outside of POI
factors that contribute to retention: taper, surface area, surface roughness, wall height
treat the entire FPD like one big tooth; most look at convergent/divergent walls across BOTH abutments
extra-coronal element- convergence
intra-coronal element- divergence
properly tapered walls 6-10 degrees (M/L and B/L walls)
wall height 3.0mm ideal; minimum 2.5 mm
no undercuts or parallel walls; no undercuts between abutments
secondary features properly placed
***the most important walls for FPD retention are the M wall of the mesial abutment and the D wall of the distal abutment; for longer span FPD more inclination of the distal wall may be necessary to get the draw
note: dislodging forces on a FPD tend to act in the M/D direction
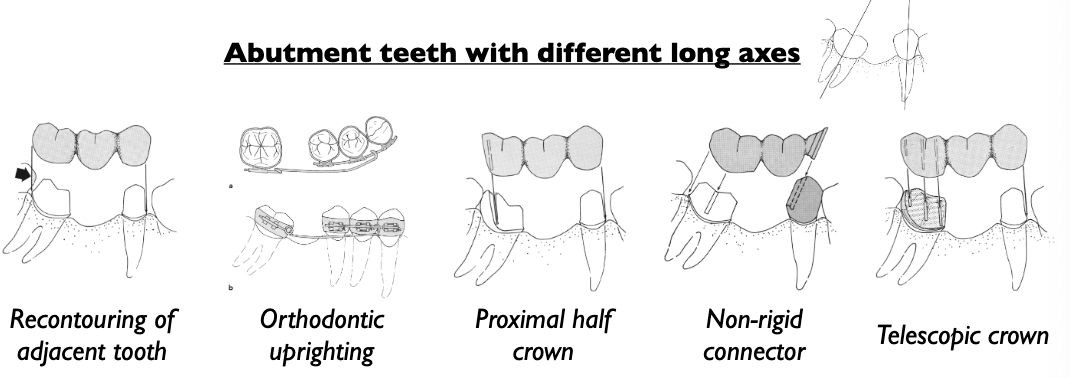
FPD path of insertion
FPD preparation is one big tooth!! we prep similar planes at the same time (lingual on one tooth and lingual on the other)
POI follows the long axis of the smaller abutment
adjacent tooth can be used as reference/guide for the POI of the smaller tooth
POI must be coincident between the abutments; so POI of larger abutment will be parallel to the POI of the smaller abutment
do NOT change angulation of the bur between abutments; therefore all gauging grooves placed should be parallel to each other
buccal and lingual walls converging on each abutment
order: buccal/lingual walls —> proximal reduction (outer walls) —> occlusal reduction —> inner walls proximal reduction —> second and third planes
Lecture 2: FPD Provisionals & Pontic Design
Pontics
definition: an artificial tooth on a fixed partial denture that replaces a missing natural tooth, restores its function, and usually restores the space previously occupied by the clinical crown
ideal characteristics:
restore function of the tooth it replaces
smooth and polished pontic surface for tissue health
mostly convex to allow for proper cleaning
restore esthetic contours confluent with the adjacent teeth
positive contact with ridge
pontic design varies based on the ridge configuration
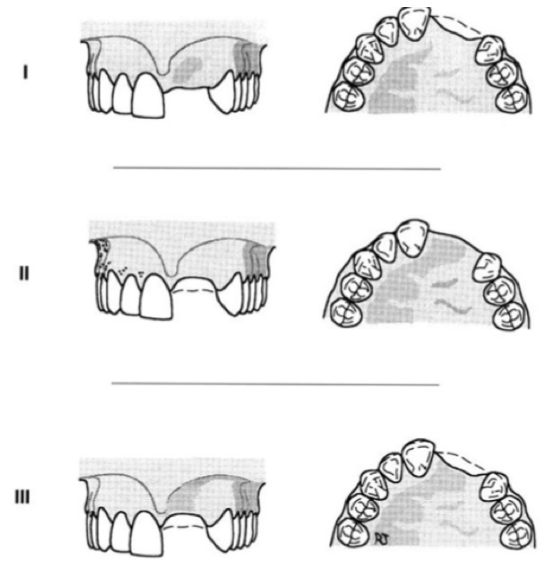
Siebert Classification of Ridge Defects
Class I: horizontal defect —> loss of facio-lingual width with normal ridge height
Class II: vertical defect —> loss of ridge height with normal width
Class III: combination defect —> loss of both height and width of the ridge
Pontic Designs
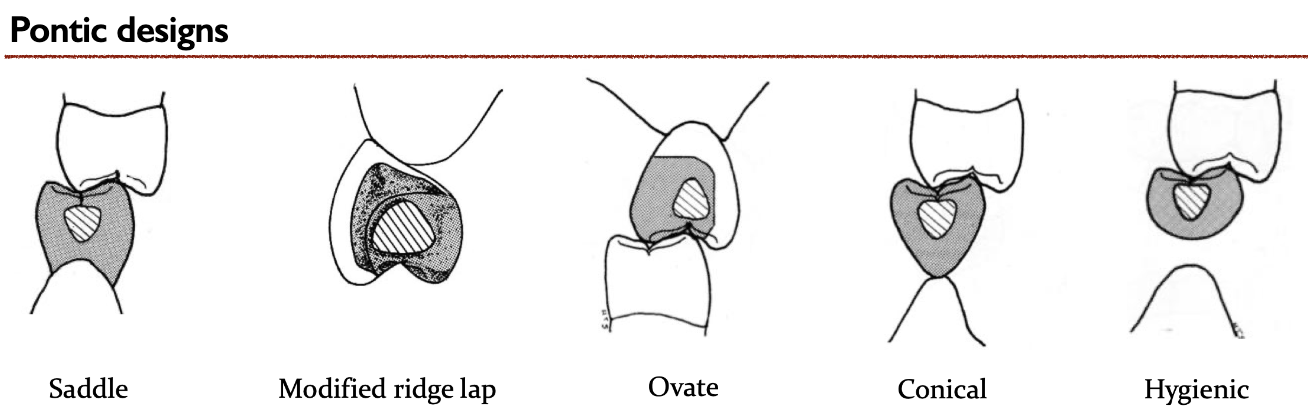
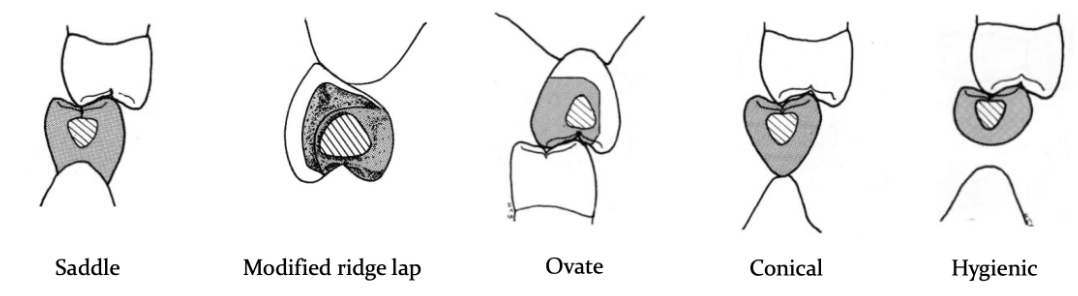
saddle pontic
aka “ridge lap”
any extension of the pontic past the crest of the ridge still constitutes a saddle
large concave contact with ridge
more difficult to clean, may cause tissue inflammation
esthetic replacing all contours of the missing tooth
modified ridge lap pontic
gives illusion of a tooth but nearly all convex surfaces for ease of cleaning
lingual has a deflective contour to prevent food impaction and minimize plaque accumulation
should not extend further lingually than the middle of the crest
slightly concave contacting the ridge to the buccal
indicated for esthetic zone maxillary and mandibular FPDs
Ovate
rounded-end design
indicated where esthetics is primary concern
for broad, flat ridge, gives appearance of emerging out of the ridge
tissue-contacting area of pontic is bluntly rounded, it seats into a concavity in the ridge
concavity can be created by placement of FPD with pontic into socket immediately after extraction of tooth, or surgically on an edentulous ridge
surgical preparation for ovate pontic
egg shaped
contour residual ridge with round/football diamond bur
buccal center 0.5-1.5mm below the buccal emergence profile
inter-proximal measurement can be as deep as 3-4mm depending upon the proximal papilla
Conical Pontic
indicated for thin mandibular ridges
rounded and easy to clean
not indicated in broad ridges since it creates areas of food trap
Hygienic Pontic
also known as “sanitary pontic”
no contact with the edentulous ride, all aspects are convex
used for non-esthetic area (mandibular first molar) gingival thickness of pontic must be at least 3mm
access for hygiene but may become a food trap
not commonly used
Lab Rx for Pontics
step 6 of the USC lab slip
can choose what style of pontic you want (modified ridge lap, ovate, saddle, conical, hygienic)
can choose how much compression you want (not applicable for hygienic style pontic
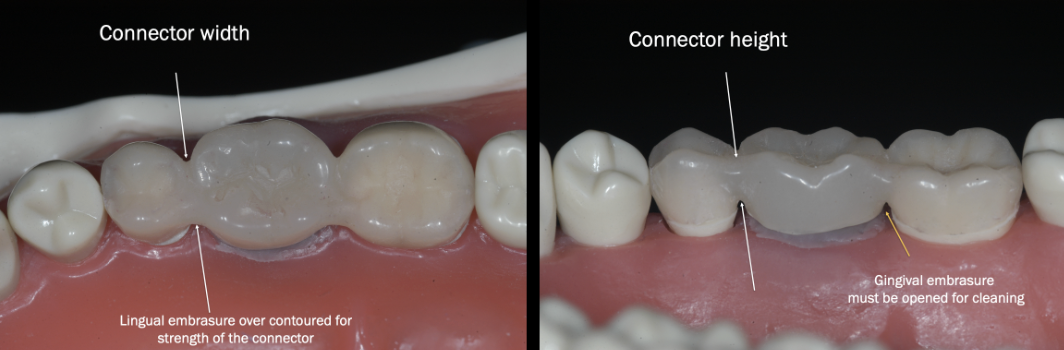
Connectors
def: the portion of a FPD that unties the retainers and pontic
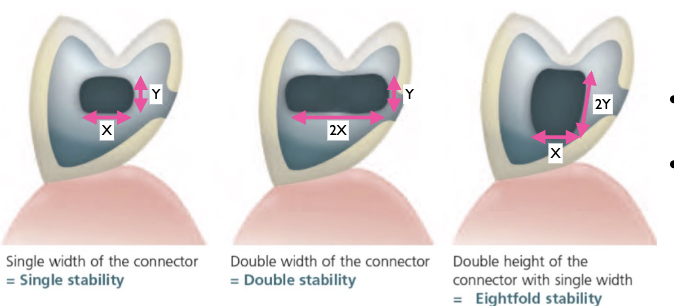
a rigid connector must be rigid enough to prevent movement and bending
Law of Beams: bending or deflection varies directly with the cube of the length and inversely with the cube of the occlusoginigval thickness of the pontic span
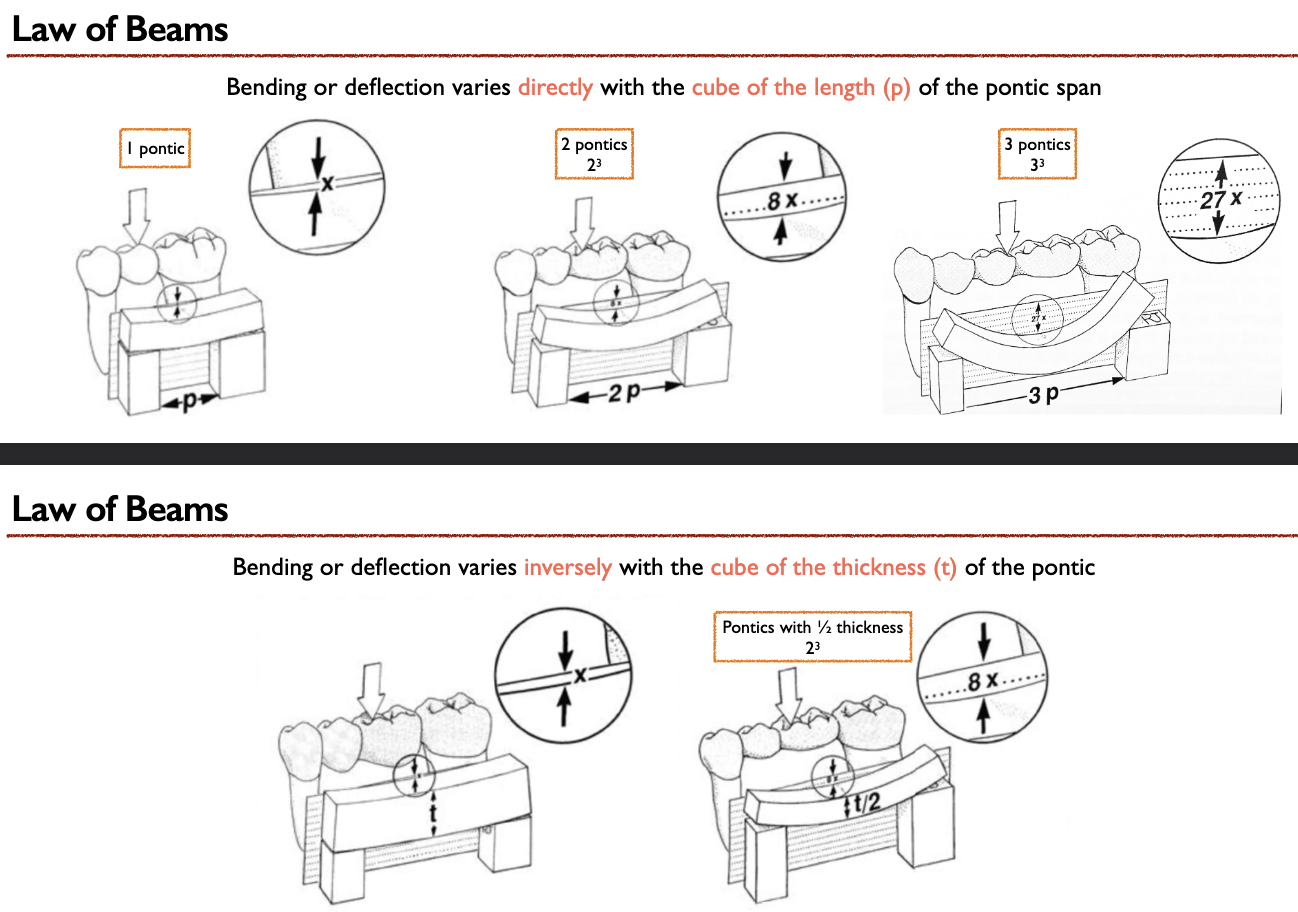
connector dimensions
as tall and wide as possible
increasing height has greater effect on reducing deflection
the longer the span, the greater the cross section of the connector is required
Preparing for FPD Provisional
goal: maximize connector cross section for fracture resistance
wax-up lingual embrasures to increase the width for the strngth of the connectors
additional wax up margins on the abutment teeth (same as single unit)
on long span FPD provisional a metal or fiber reinforced FPD may be needed
Provisional:
definition= fixed or removable prothesis designed to enhance esthetics, stabilization, and/or function for a limited period of time, after which is to be replaced by a definitive prothesis
functions:
provides the template for the final restoration
assist in the determination of the therapeutic effectiveness or the form and function of the planned definitive prothesis
allows for evaluation of parallelisms of the abutment
allows for evaluating an occlusal schemes before the definitive restoration
provides patient comfort and pulpal protection of the abutment teeth
maintains positional stability of the abutments
restores occlusal function and esthetics
favorable for periodontal health (non-impinging margins, proper gingival embrasures to facilitate cleaning)
Provisional Materials
self-cure/dual-cure composite resin
ex: bis-acrl
light-cure composite resin
ex: Fermit-N
acrylic resin
material w/ high strength and fracture resistance required
ex: polymethyl methacrylate (PMMA)
advantages: good margin adaptation, good strength, good polish-ability, easy repair, esthetic
disadvantages: exothermic rxn, volumetric polymerization shrinkage ~6-7%, soft tissue/pulpal irritation w/ excess free monomer, allergic reactions to monomer
provisional fabrication techinque = indirect-direct technique
ex: polyethyl methacrylate (PEMA)
advantages: minimal exothermic heat, good stain resistance, good polishability, low shrinkage
disadvantages: lower strength, lower fracture toughness, poor wear resistance, poor color stability
ex: CAD/CAM Acrylic Resin
advantages: high flexural strength, less porosity (pre-polymerized), color stability, good abrasion resistance
disadvantages: CAD/CAM digital workflow, time consuming, expensive, require specific thickness (occ. 1.5mm and margins 0.8mm)
Indirect-Direct PMMA Shell Provisional
1) Shell Fabrication
done prior to pt tooth prep appt
requires prep of teeth on a plaster cast
indirect technique PMMA shell fabrication
shell provides the contours for the provisional
separators: alcote or vaseline
pressure pot —> 20PSI for 5 mins
2) Shell Adjustment
intra-oral try-in shell adjustments
shell proximal contacts and internal may require additional relief so shell will seat passively and allows for relining material
no hyper-occlusion prior to relining!!
3) Shell Reline
reline is done direct intra-orally by adding mix of PMMA to adjusted shell
pt closes in MIP during initial setting of material
need to use air-water to control the heat from exothermic rxn during setting
intermittently pump up and down to avoid locking
remove the relined shell before complete setting
4) Provisional
inspect that margins and details have been captured
trim in same sequence as the single unit
additional trimming of the gingival embrasures
should be open for cleaning and gingiva health
lingual embrasures- over contoured to maintain width of connector for strength
buccal embrasures- trimmed and defined for esthetics
occlusal contacts hold mylar on the adjacent teeth and on the retainers of the FPD [for anterior FPD, drag mylar]
FPD Provisional Pontic
should have the prescribed design
must be smooth and polished
important for tissue health
must have positive contact with the ridge
should challenge the tissue and drag mylar
template for definitive restoration
esthetic changes made on provisional for patient approval
take alginate impression of approved provisional and pour up cast for lab tech to use as reference for final rest.
communicates: contour, shape and size; embrasures, line angles and texture; incisal length and position; midline and symmetry; occlusion and function
**Patient receives post op instructions for cleaning = use floss threader or super floss to clean
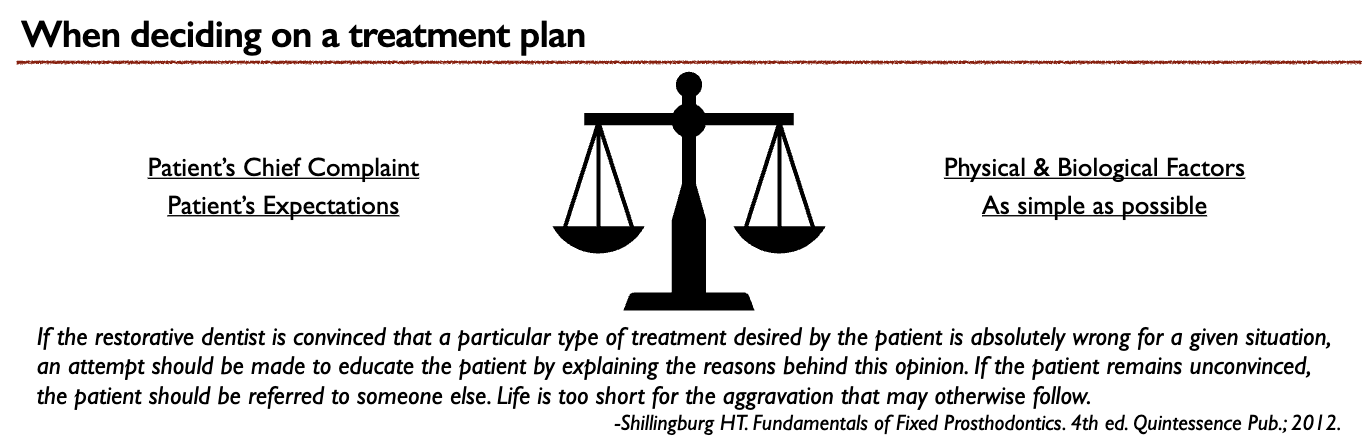
Lecture 3: Treatment Planning Considerations for Tooth Replacement
treatment plan = the sequence of procedures planned for the treatment of a patient after diagnosis
data collection & diagnosis = chief complaint, health history and dental history, intra-oral examination and periodontal charting, diagnostic casts, radiographs// diagnosis & diagnostic wax-up, treatment plan & treatment sequence, interdisciplinary approach to patient care (referrals)
developing a treatment plan: begins with looking at individual teeth, in which each tooth should be considered as a piece of the overall patient-centric treatment plan
Consider these:
why is the pt missing teeth? history of tooth loss, non-restorable tooth, caries, trauma, bruxism, drugs, extrinsic factors, periodontal disease
what is the condition of the other teeth? intact adjacent teeth, caries and existing restorations, super-erupted opposing teeth, positions of remaining teeth
what are the patients constraints? medical limitations, financial constraints, fixed vs removable, declines surgical procedures
What are my treatment options for replacing a missing tooth: fixed implant supported crown, fixed partial denture, removable partial denture, no treatment
Implant Supported Crown
advantages: most conservative to the adjacent teeth, restores function and esthetics, fixed prosthesis with high survival rate, good option for high caries risk
disadvantages: requires surgical procedure for placement, longer time to delivery of final crown, anatomical limitations for implant placement, possible peri-implantitis with bone loss
Fixed Partial Denture
advantages: restores function to some extent (Kennedy Classification), replaces missing teeth
disadvantages: higher plaque index caries prone, stresses to the abutment teeth, abutment teeth need preparation of rests and guiding planes, abutment teeth may need crowns to support the RPD, removable prosthesis, may not be esthetic metal clasps visible
No Treatment
advantages: less costly for now, no additional time spent for now
consequences of not replacing a missing tooth: alters future space for restorations, supra-eruption of opposing teeth, teeth shifting into space, tilting and rotation of adjacent teeth, ridge resorption, may alter esthetics, decreased function?
Survival Rates of FPDS
10-year success 71.1-81.1%; 10-year survival: 89.1-92%
Biological Complications: caries > loss of vitality
technical complications: loss of retention > abutment tooth fracture > fracture of framework/ceramic
FPD opposing complete dentures had longest survival rate ~16 years
Considerations when planning for a FPD
evaluate edentulous space:
span lengths —> posterior 2 or fewer; anterior 4 or fewer
span configurations —> distal abutment or short cantilever
patient factors —> finances or xerostomia
additional treatments (interdisciplinary approach to patient care):
endodontic tx, core build-up with or without a post, crown lengthening or other periodontal tx, orthodontic tx, correction of occlusal plane
evaluate abutment teeth:
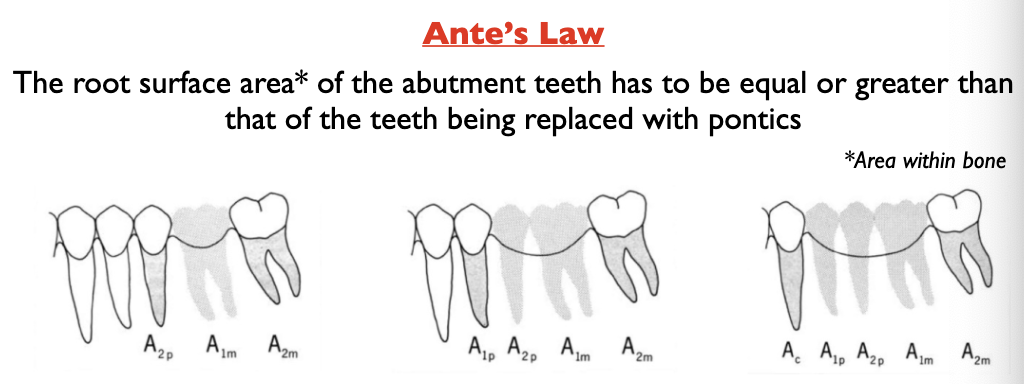
occlusal plane, crown to root ratio, root surface area, periodontal health, tooth vitality
multi-rooted teeth with separated roots are better at displacing occlusal load than teeth with fused roots
teeth w/ a winder BL dimension than MD have a greater ability to handle load than conically shaped roots
larger teeth have a greater root surface area (the area of periodontal ligament attachment of the root to bone) and are better abutments for FPD
Ante’s Law: the root surface area of the abutment teeth has to be equal or greater than that of the teeth being replaced with pontics
existing restorations and caries:
ask: direct/indirect existing restorations, intact or defective
remove defective restoration and caries clean out
evaluate remaining tooth structure for restorability check, additional endo treatment/perio surgery may be needed, additional restorative core build up with or without post may be needed
tooth vitality:
preferable vital abutment tooth, RCT teeth are not a contraindication for FPD so long as they are asymptomatic, complete obturation, good apical and coronal seal, sufficient remaining tooth structure
periodontal health:
supporting tissue surrounding the abutment must show no inflammation, periodontally involved teeth may not have enough support to withstand the occlusal forces; abutment tooth mobility=poor prognosis
optimum corwn:root ratio 2:3
minimum acceptable is 1:1
edentulous space and biomechanical considerations
deflection of the FPD; the longer the span the more the deflection
law of beams: bending or deflection varies directly with the cube of the length (p) and inversely with the cube of the occlusoginigval thickness (t) of the pontic span
MUST compensate by increasing thickness
amount of restorative space limits how thick you can make it
or we can fabricate of an alloy with a higher yield strength such as nickel-chromium
ALL FPDs regardless of span will flex to some extent
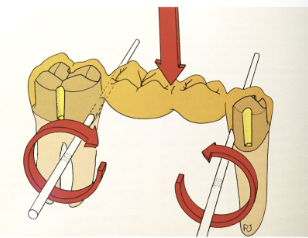
FPD dislodging forces tend to act in a M/D direction
factors that minimize dislodging forces
abutment preparation height
proper taper of the opposing walls
secondary BL retentive grooves
secondary abutment must have at least as much root surface area and must be at least as retentive as the primary abutment
the secondary retainers are placed in tensions when the pontic flexes; the primary abutments act as fulcrums (dislodging forces)
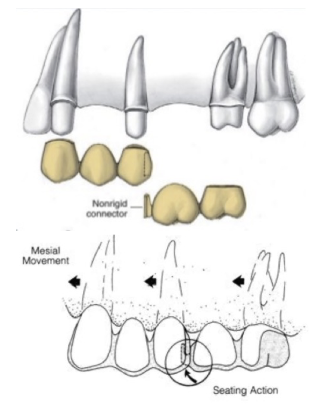
Pier Abutment
=an edentulous space lies one each side of the middle abutment
middle abutment acts as a fulcrum for displacing forces causing failure of the retainer
non-rigid connector transfers forces to the supporting bone
occlusal plane evaluation
movement of adjacent teeth after tooth loss causing a discrepancy in the occlusal plane and decreased restorative space
the malpositioned adjacent/ opposing teeth may compromise the restoration
opposing tooth may be treated via orthodontic movmnt and/or restoration
occlusal schemes
must propose an occlusal scheme for the final FPD
mutually protected occlusion, group function occlusion, balanced occlusion (complete dentures)
1) mutually protected
anterior teeth protect posterior teeth during movmnt and posterior teeth protect anterior teeth in MIP from vertical occlusal forces
canine guidance —> canine disocludes posterior teeth in excursive mvmnts of mandible
anterior guidance —> ant teeth disoclude all posterior teeth in excursive mvmnt of mandible
2) group function
aka posterior group function
multiple contact relations between the max and man teeth in lateral mvmnts on the working-side whereby simultaneous contact of several teeth acts as a group to distribute occlusal forces
**not all posterior teeth need to guide to be considered group function
indications: severe class II, III occlusion; mandible cannot be guided by anterior teeth due to missing anteriors, open bite or compromised anterior dentition; force distribution for long span FPD or compromised abutments
Other Special Problems
canine-replacement fixed partial dentures
forces on maxillary canine are more damaging because it is transmitted labially
no FPD replacing a max canine should replace more than one additional tooth
forces on mandibular canine are less damaging because the forces are directed lingually
cantilevered pontics
can only be used in specific situations:
replacing lateral incisors, replacing a premolar, double abutments required when replacing molars
pontic size reduced and occlusion on pontic minimized
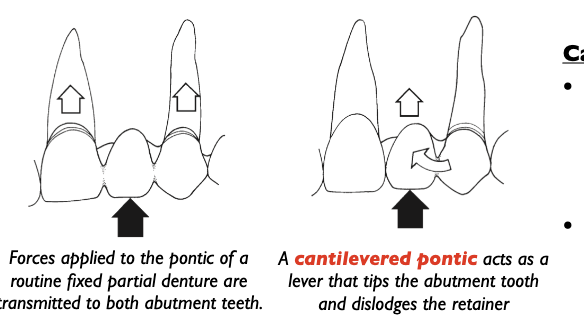
Why cantilevered pontics are not ideal:
causes greater forces on the abutment
double abutment may be indicated
a downward occlusal force on the pontic will create an upward force on the secondary abutment (the primary abutment acts as a fulcrum)
reducing the size of the pontic will reduce the dislodging forces that act on the furthest secondary abutment

Resin Bonded FPDs- Maryland Bridges
Materials
SHORT TERM fiber-reinforced composite
gold alloy framework (intorduced by Rochette 1973)
coblat or Ni-Cr framework
Oxide ceramic framework
glass infiltrated alumina ceramic
lithium disilicate based ceramic, Zirconia
Design
one wing design retainer, over-contoured lingual with strong connector
can lead to debonding or fracture at the connector
two-wing design retainers are contraindicated for definitve restoration
differential mvmnt between abutment teeth
shear forces on the wing of retainers
debonding of one wing and caries under debonded wing
preparation:
Survival
mode of failure: debonding
glass infiltrated alumina RBFPDs 10 year survival 95.4%
fracture at connector
IPS e.Max Press/CAD ceramic 5 year survival: 100%
zirconia 10 year survival 98.2-100%
18 year survival 81.8%
debonding without any fracture of framework, able to rebound
layered ceramic chipping lowered success rate
Indications for FPD
replacement of existing conventional FPD
in implant tx would require multiple surgeries for bine and tissue grafting
medically compromised patients unable to undergo implant surgery
patient expectations, cost, duration of tx
drawback in cases of compromised abutments: if one abutment fails the entire FPD will fail
Lecture 4: Restoration Delivery and Cementation