Module 13 Sensory
Module Overview
Focus: Assessment and care for patients with visual and auditory impairments.
Chapters: 22 and 23
Learning Outcomes
Utilize interviewing and assessment skills for clients with vision/auditory alterations.
Assess the impact of these alterations on overall human functioning.
Apply the nursing process for sensory problem care.
Identify nursing responsibilities regarding retinal detachment, orbital trauma, enucleation, and vision/auditory surgeries.
Recognize common medications for auditory and visual disturbances.
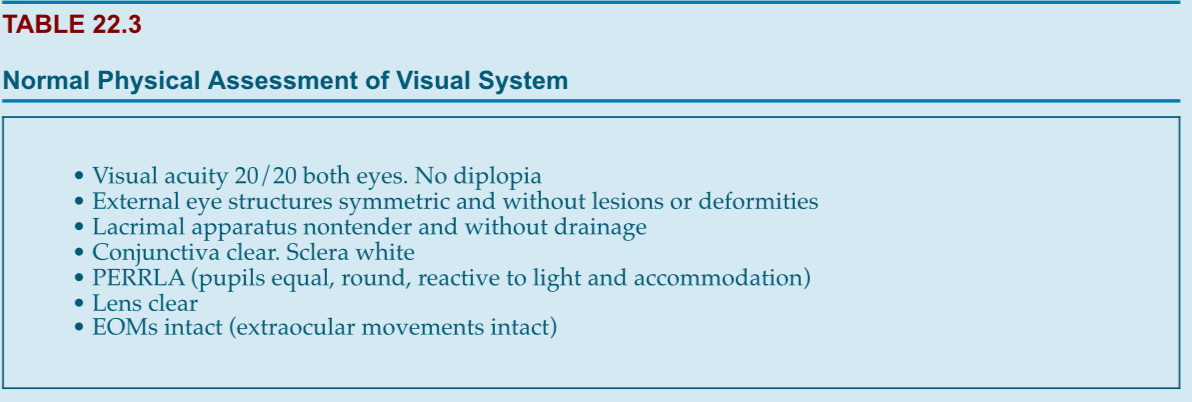
Assessment of Visual System
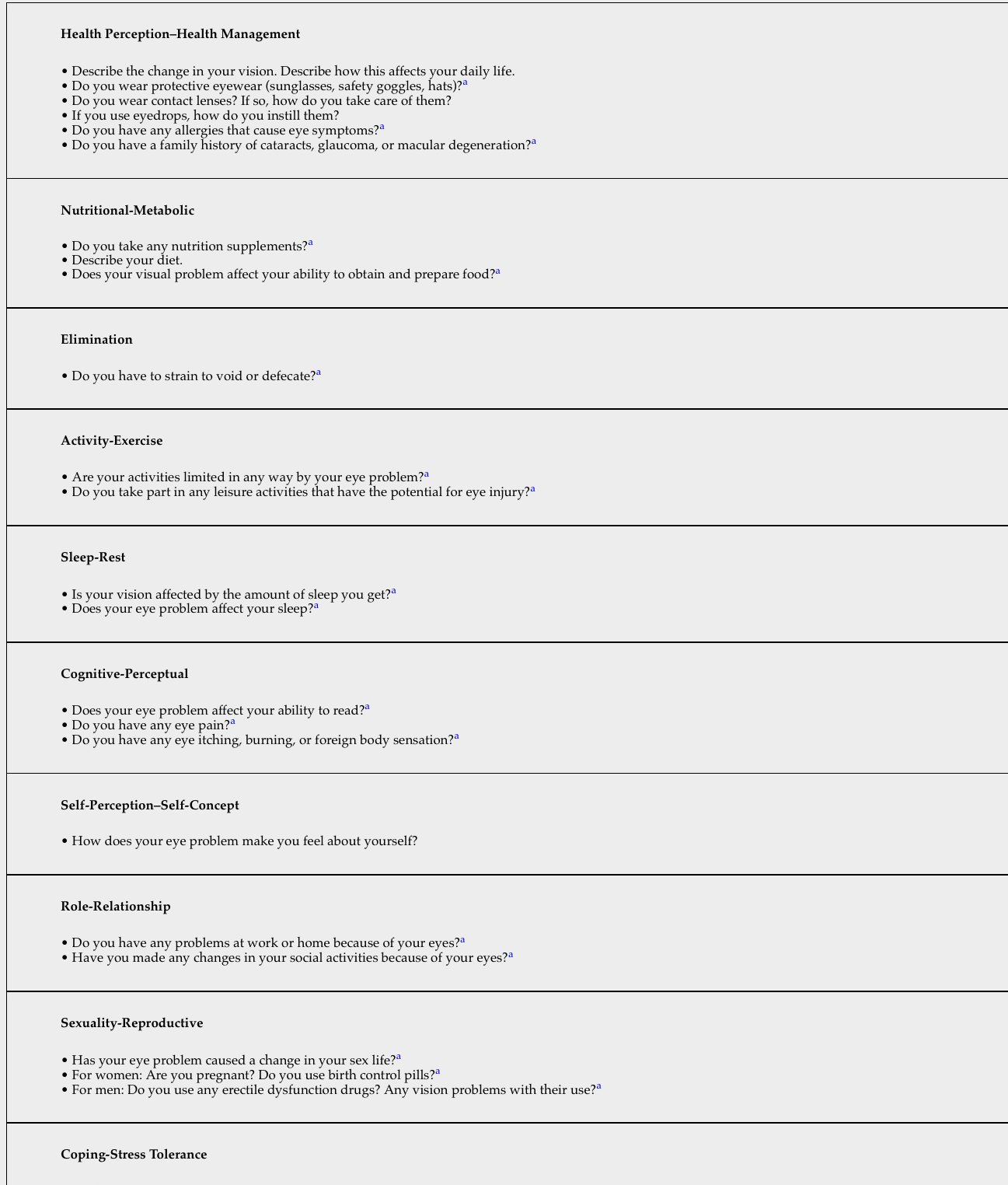
Health History Components
Last ocular exam date, use of glasses/contacts.
Medication considerations:
Eye drops and cold meds (may contain epinephrine).
Corticosteroids and thyroid medications (risks for cataracts/glaucoma).
History of ocular and non-ocular surgeries.
Nursing Assessment Techniques
Color Vision Testing: Checks ability to perceive color.
Visual Acuity Testing:
Use Snellen Chart, assess each eye separately.
Record results as a fraction (e.g., Right eye 20/30 with glasses).
Tonometry: Measures intraocular pressure.
Keratometry: Assesses curvature of the cornea.
Ophthalmoscopy: Examines interior structures of the eye.
Pupil Function Testing: Checks pupil responsiveness (PERRL).
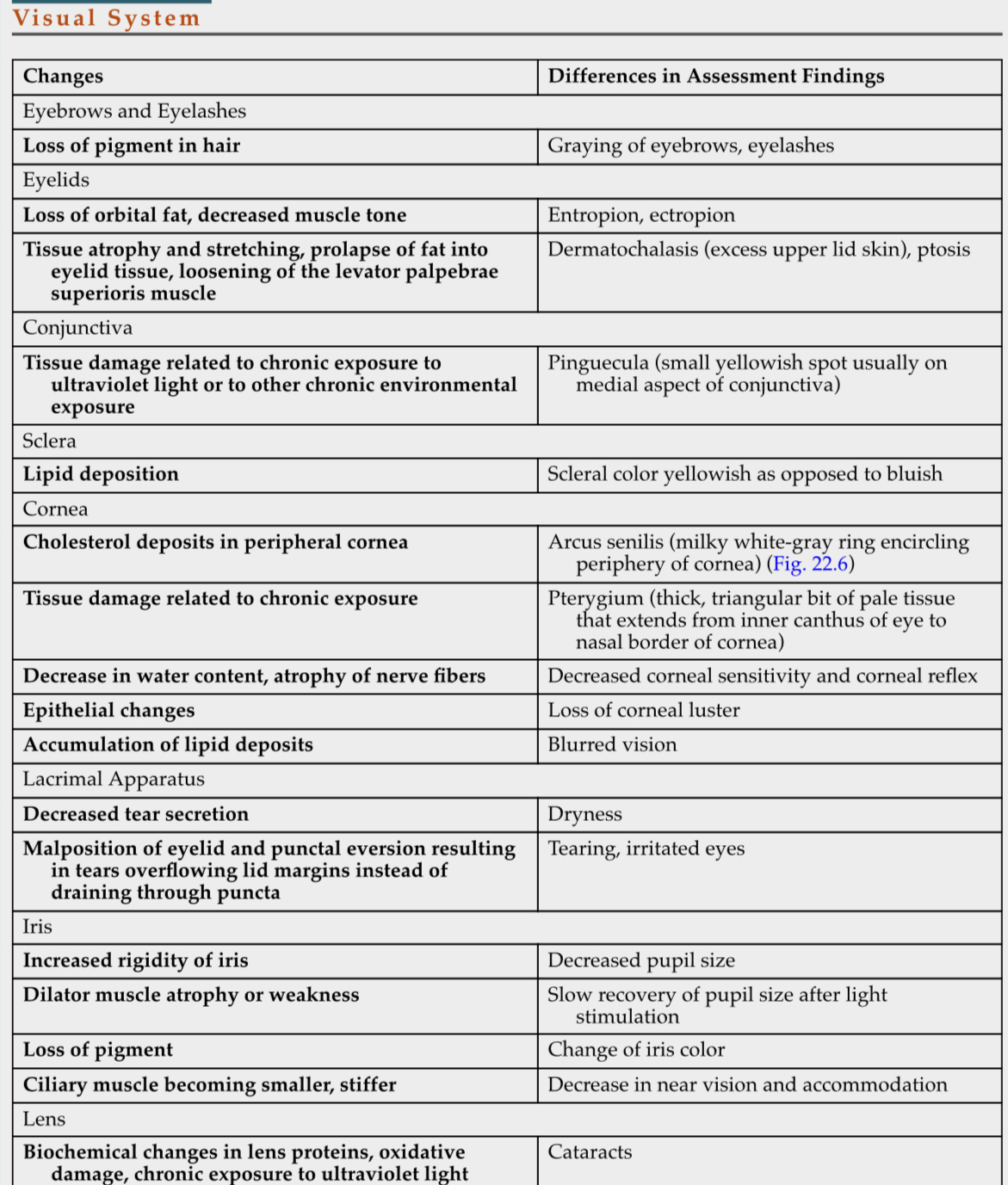
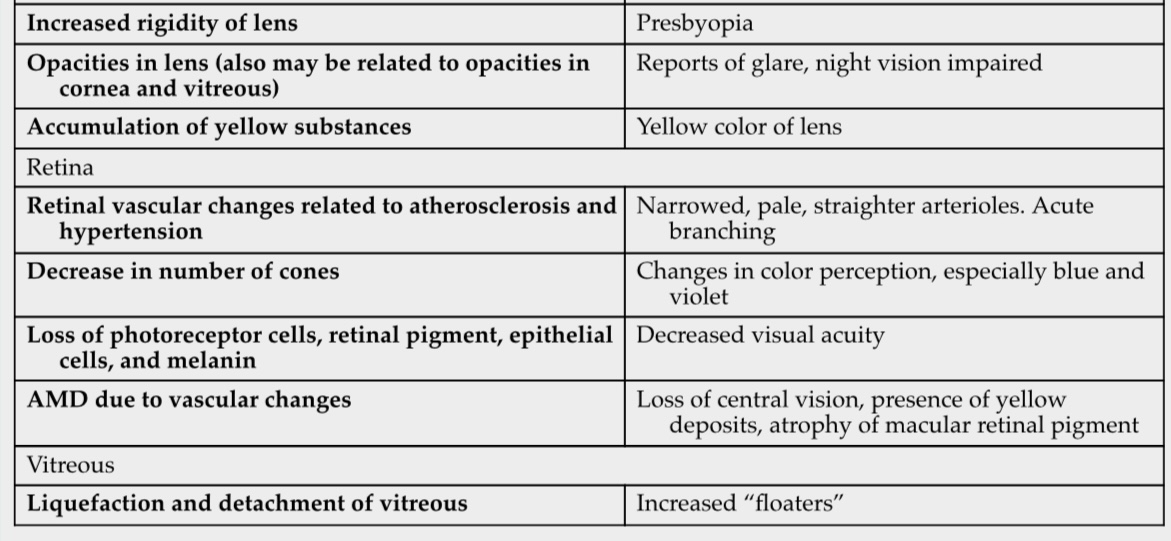
Assessment Abnormalities
Visual System Symptoms:
Blurred vision
Diplopia (double vision)
Dryness
Spots
Pain
Photophobia
Floaters
Eyelid Abnormalities:
Allergic reactions
Blepharitis - inflammation of eyelid
Ectropion - eyelid flipped out away from eye
Hordeolum - sty
Ptosis - drooping of upper eyelid
Common Diagnostic Tests
Amsler Grid Test - measure macular (waves, missing lines, abnormalities - issues)
Fluorescein Angiography (assess IV site because it is a vesicant, can cause orange/yellow)
Perimetry Testing (flashing light to test central and peripheral vision)
Refractometry (look for refraction issues)
Ultrasonography (size and structure of eye)
Refractive Errors
Myopia: Nearsightedness; light focuses in front of the retina. most common
Hyperopia: Farsightedness; light focuses behind the retina.
Astigmatism: Light focuses on multiple points. Irregular curvature
Presbyopia: Age-related loss of near vision. Lenses become larger, firmer, less elastic
Aphakia: Absence of the lens.
Common Corrections
Corrective glasses, contact lenses, surgical options (LASIK, PEK (cornea not thick enough for LASIK), IOL- replacement of lenses).
Visual Impairment
Defined as uncorrectable vision issues, ranging to blindness.
Vision is classified by the best eye
Legal blindness: best-corrected vision ≤ 20/200 or restricted visual field.
Major causes include cataracts, glaucoma, AMD, diabetic retinopathy.
Responsible Eye Care
Regular hand hygiene and protective measures.
Utilization of sunglasses and protective eye wear and nutrition for eye health.
Sight Guide Technique
Assist visually impaired individuals properly:
Offer elbow, indicate environment changes, and allow independent seating orientation.
Gerontological Considerations
Visual impairment in elderly may lead to isolation and financial issues.
Medication handling can be impacted due to decreased dexterity.
Eye Injury/Trauma
Common causes include falls, fights, and home accidents.
Emergency management should prioritize airway, breathing, circulation.
Immediate eye irrigation for chemical burns; stabilize foreign bodies.
Traumas are usually avoidable
Many times injury is caused by improper contact use and failure to wear protective eye wear
Morgan Lens
Provides continuous irrigation for chemical or thermal burns.
Common Eye Conditions
Hordeolum (Sty)
Infection of meibomian glands; treat with warm moist compresses x4 an day and, if recurrent, lid scrubs.
Bacterial Conjunctivitis (Pink Eye)
Caused by Staphylococcus aureus; involves redness and discharge. Treat with antibiotic eye drops.
Itches and discomfort
Highly contagious
Moist wet compresses
Good hygiene
Cannot use contacts
Dispose of contacts, solution, and any cosmetics and cosmetic tools that come in contact with the eye
Epidemic Keratoconjunctivitis (EKC)
Serious viral infection; requires good hygiene practices to prevent spread.
Ice packs, artificial tears, and dark glasses
Trachoma
Major cause of blindness
Spread by poor hand hygiene and rubbing eyes
Another type of conjunctivitis
Allergic conjunctivitis
Exposure to allergen
Can be severe enough to cause significant swelling
Burning, redness, tearing
Try to avoid allergen
Keratitis
Inflammation or infection of the cornea
Bacterial or viral
UV exposure
Immunosuppressed, contact wearers, nutritional deficiencies- higher risk
Treatment- antibiotic, antiviral (herpes simplex), analgesic, topical corticosteroids, mydriatic agents dilate pupil and relieve pain
Corneal Ulcers
Tissue loss due to corneal infection
Bacterial
Viral
Fungus
Cataracts
Visual opacity; gradual vision decline. Most are age-related. Treatment primarily surgical.
Retinal Detachment
Emergency condition; symptoms include flashes of light, floaters, and curtain-like vision loss.
Treatment can include surgical interventions like cryopexy or scleral buckling.
Age-Related Macular Degeneration (AMD)
Major cause of irreversible vision loss; characterized by distorted vision and blind spots.
Treatments involve injected medications to slow progression.
Glaucoma
Disorder characterized by increased intraocular pressure leading to optic nerve damage.
Two primary types: primary open-angle (most common) and angle-closure.
Management may include medications, surgery, and regular eye exams to monitor IOP.
Auditory System Overview
Hearing impairments can majorly affect social interaction and cognitive function.
Common causes include external, middle, and inner ear conditions.
signs of Possible Hearing Loss
Insufficient response to communication, need for loud volumes, inappropriate answers.
Common Conditions in Auditory System
Otitis Media
Acute form often seen in children; treatment may involve antibiotics or surgical interventions.
Chronic Otitis Media
Recurrent infections leading to potential hearing loss; surgical options may be required.
Otosclerosis
Hereditary condition causing conductive hearing loss; treated surgically by replacing the stapes.
Ménière Disease
Progressive disorder causing episodic vertigo and hearing impairment; management focuses on symptom relief.
Ménière's Disease is a progressive inner ear disorder characterized by episodes of vertigo, hearing loss, tinnitus (ringing in the ears), and a sensation of fullness in the ear. The disease typically affects one ear, but in some cases, it can affect both. Symptoms can vary in duration and intensity, with episodes lasting from 20 minutes to several hours.
Common Causes:
Abnormal inner ear fluid pressure
Allergies, infections, and genetic predispositions may contribute to the condition.
Management and Treatment:
There is no cure, but treatments focus on symptom relief.
Medications to manage vertigo and nausea
Dietary changes, such as reducing salt intake, to help manage fluid balance
Diuretics to assist in reducing inner ear fluid buildup
In severe cases, surgical options may be considered to relieve inner ear pressure or to destroy the balance function of the affected ear.
Lifestyle Adjustments:
Patients are advised to avoid triggers like stress and certain foods or beverages that may aggravate symptoms.
Balance therapy and hearing aids may also be recommended as part of comprehensive management.
Patient Teaching for Hearing Aids
Introduce aids in quiet environments, progressively increase exposure.
Care tips: keep aids dry, clean ear molds weekly, manage battery life.
 Slide 27 - 43
Slide 27 - 43
cataracts
Retinal detachment
Macular degeneration
Glaucoma
Enclunation
Vertigo and dizziness are often confused but are distinct experiences.
Vertigo:
A specific type of dizziness characterized by the false sensation of spinning or movement.
Individuals may feel as if they or their surroundings are moving when in fact they are not.
Typically related to inner ear disorders, such as Ménière's disease or vestibular neuritis.
Can be accompanied by nausea, balance problems, and visual disturbances.
Dizziness:
A broader term encompassing various sensations including lightheadedness, faintness, or unsteady feelings.
It does not imply the hallmark sensation of movement associated with vertigo.
May be caused by a variety of factors including dehydration, low blood pressure, anxiety, or medication side effects.
In summary, while vertigo is a type of dizziness, not all dizziness is vertigo. Understanding the difference is crucial for diagnosing and treating the underlying causes of these symptoms effectively.