Exam 2 blueprint
Mental Health and Illness NURS 3540
Exam 2 BLUEPRINT
Thursday, February 22, 2024
Chapter 6 Legal and Ethical
1. Rights of the patient admitted to a psychiatric hospital (pp. 96-99 Varcarolis 9th ed.)
Right to treatment
right to be free from excessive or unnecessary medication
right to privacy and dignity
right to the least restrictive environment
right to attorney, clergy, and private care providers
right not to be subjected to lobotomies, electroconvulsive treatment, and other treatments without fully informed consent
Right to refuse treatment
Patients can also retract consent previously given.
a person can be medicated if they meet
The person has a serious mental illness
The person’s functioning is deteriorating and if the person is suffering or exhibiting threatening behavior
The benefits of treatment outweigh the harm
The person lacks the capacity to make a reasoned decision about the treatment
Less-restrictive services have been found inadequate
Right to informed consent; must be provided to pt with basic information regarding risks and benefits with alternative treatment
prescriber is responsible for securing informed consent.
patient are informed of
• The nature of the problem or condition
• The nature and purpose of a proposed treatment
• The risks and benefits of that treatment
• The alternative treatment options
• The probability that the proposed treatment will be successful
• The risks of not consenting to treatment
Right regarding psychiatric advanced directives
Ohio declaration of mental health treatment
Designation of preferred physicians and therapists
• Appointment of someone to make mental health treatment decisions
• Preferences regarding medications to take or not take
• Consent or lack of consent for ECT
• Consent or lack of consent for admission to a psychiatric facility
• Preferred facilities and unacceptable facilities
• Individuals who should not visit.
Rights Regarding Restraint and Seclusion- The American Psychiatric Nurses Association (APNA) promotes a culture that minimizes and eventually eliminates the use of seclusion and restraint (APNA, 2018)
least restrictive means of restraint for a short duration is a general rule
nurses are to consider the following before using seclusion and restraint
Verbally intervening (e.g., asking the patient for cooperation)
• Reducing stimulation
• Actively listening
• Providing diversion
• Offering as needed (PRN) medications
Right regarding confidentiality- only patient can waive their legal privilege of confidentiality.
2. What are the hospitalization admission procedures guidelines? (p. 94 Varcarolis 9th ed.)
All admissions are based on several fundamental guidelines:
• Neither voluntary admission nor involuntary commitment determines a patient’s ability to make informed decisions about personal healthcare.
• Care providers establish that a well-defined psychiatric problem exists based on current illness classifications in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5; American Psychiatric Association [APA], 2013).
• The illness and its symptoms should result in an immediate crisis situation and other less-restrictive alternatives (i.e., outpatient care) are inadequate or unavailable.
• There is a reasonable expectation that the hospitalization and treatment will improve the presenting problems
3. What are the guidelines for voluntary, involuntary, and emergency admission or commitment?
Voluntary admissions- pt apply in writing for admission to the facility. pt need to understand the need for treating and willing to be admitted.
if pt is under 16: parent, legal guardian, custodian or next of kin may have to apply on the pt’s behalf.
adolescence 16-18 may seek admission independently or on the application by an authorized individual or agency.
Involuntary commitment: a court-ordered admission to a facility without the patient’s approval.
criteria to that allows court to decide are
Diagnosed with mental illness
Posing a danger to self or others
Gravely disabled (unable to provide for basic necessities such as food, clothing, and shelter)
In need of treatment and the mental illness itself prevents voluntary help-seeking.
Patients can file a writ of habeas corpus(formal written order to free the person.”) if they feel like they are held without a just cause
patient can also challenge hospitalization based on least retrictive alternative doctrine.- mandate that care provider take the least drastic action to achieve a specific purpose.”
Emergency commitment: also know as a temporary admission or emergency hospitalization
(1) for people who are so confused they cannot make decisions on their own or
(2) for people who are so ill they need emergency admission.
In some states, anyone can initiate these proceedings through the court system. Other states require that care providers—such as a physician, an advanced practice psychiatric nurse, a social worker, or an officer of the law—initiate a temporary admission.
The primary purpose of this type of hospitalization is the observation, diagnosis, and treatment of patients who have mental illness or pose a danger to themselves or others
temporarily admission ranges from 24-96 hr depending on the state.
A court hearing is held and a decision is made for discharge, voluntary admission, or involuntary commitment.
4. What are the 3 primary reasons an individual is admitted to the psychiatric hospital?
Three primary reason an individual is admitted to a psych hospital include
1. Diagnosed with mental illness
2. Posing a danger to self or others
3. Gravely disabled (unable to provide for basic necessities such as food, clothing, and shelter)
4. In need of treatment and the mental illness itself prevents voluntary help-seeking
5. Be familiar with discharge procedures and conditions for release (pp. 95-96 Varcarolis 9th ed.).
Discharge procedures; voluntary admitted pt have the right to request and receive release but some state provides conditional release of voluntary pt, which allows PCP to order continued treatment on an outpatient basis if pt. need futher help
Unconditional release: most common after admission is the unconditional release: termination of the legal patient-institution relationship. allowed by psych registered nurse practitioner or physician assistant or court order.
Release Against medical advice: Patients are required to sign a form indicating that they are leaving AMA. This form becomes part of the patient’s permanent record.
An AMA discharge may present an ethical dilemma for clinicians. On the one hand, patient autonomy and the right to refuse treatment support the patient’s wishes for discharge.
Conditional release: require outpatient treatment for a specific period of time. Assisted oupatient treatment is a court-ordered outpatient treatment. pt can avoid rehospitalization if they maintain their
6. What is informed consent and implied consent? (pp. 97-98 Varcarolis 9th ed.).
Informed consent: pt is provided basic information regarding risk and benefits and treatment alternatives. Physician is legally resposible in securing the informed consent. based on a pt’s right to self determination.
Element of informed consent include
• The nature of the problem or condition
• The nature and purpose of a proposed treatment
• The risks and benefits of that treatment
• The alternative treatment options
• The probability that the proposed treatment will be successful
• The risks of not consenting to treatment
Implied consent: pt willingness to participate in a care provided. eg medication administration.
Chapter 7: The Nursing Process
1. Be familiar with the Mental Status Exam (MSE) in psychiatric nursing and its uses.
purpose is to evaluate an individual’s current cognitive processes
The MSE aids in collecting and organizing objective information- all wha† nurses observe or verify through test.
VS, nonverbal cues like pt appearance, behavior, nonverbal communication, speech patterns, mood and affect, thought content, perceptions, cognitive ability,f and insight and judgment.
Chapter 12 Schizophrenia
1. What neurotransmitters are associated with schizophrenia? Are they high or low?
Dopamine plays a significant role in psychosis
Increase of Dopamine indicates
Schizophrenia and mania
serotonin
Decrease of Serotonin indicates
Depression
glutamate
Decrease of NMDA causes
Psychosis
GABA- calms
Decrease of γ-aminobutyric acid (GABA) indicates
Anxiety, schizophrenia, mania, huntingtons disease
Acetylcholine also plays a role in the psychosis
Increase of ACH indicates depression
Noephinephrine
Increase of noephinerine indicates
Mania, schizophrenia, and anxiety state
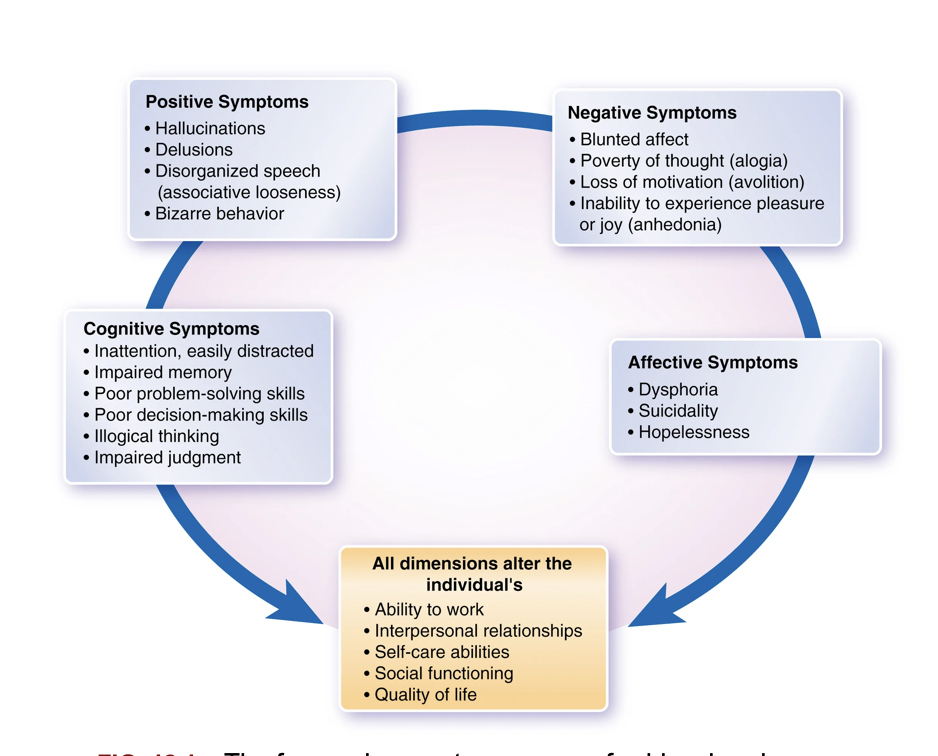
2. What are the 4 symptom types seen in schizophrenia? (pp. 194-198 Varcarolis 9th ed.).
Positive symptoms: appears early; dramatic and precipitate treatment. alters reality testing: automatic and unconscious process by which we determine what is and is not real.
Negative symptoms: negative symptoms are a serious problem for people with schizophrenia because they amount to the absence of essential human qualities. Treating negative symptoms is more difficult than treating positive symptoms.
Affective symptoms: involve an altered experience and expression of emotions. Mood may be unstable, erratic, labile (changing rapidly and easily), or incongruent (not what would be expected for the circumstances).
A serious affective change often seen in schizophrenia is comorbid major depressive disorder.
Cognitive symptoms: represent the third symptom group and are evident in most patients with schizophrenia. These impairments can lead to poor judgment and leave the person less able to cope, learn, manage health, or succeed in school or work.
Alterations of speech
associative looseness: haphazard and illogical thinking where concentration is poor and thoughts are only loosely connected. For example: “My friends talk about French fries but how can you trust the French
Word salad: jumbled up word that makes no sense to the listener e.g agents want the strength of policy on a boat reigning supreme.
Clang association: words based on their sound e.g click clack couch
Neologism: words that make sense to the pt but not to the listener e.g his mannerlogies are poor.
Echolalia: repitition of another sentence.
3. Be able to differentiate between delusions – persecutory, referential, grandiose, and control. (Table 12.1 p. 195 Varcarolis 9th ed.)
Delusion: false belief e.g persecutory, grandiose, or religious ideas
Persecutory: singled out for harm
Referential: event of no connection are somehow r/t the pt.
Grandiose: believing that they are of great important and valued
Erotomanic: believing that another desires you romantically.
Somatic: believing that the body is changing in unusual ways
Control: Believing that another person, group, or external force controls your thoughts, feelings, impulses, or behavior
4. What are the 5 types of hallucinations? (p. 196 Table 12.6 pp. 213-214)
• Auditory: Hearing voices or sounds
• Visual: Seeing people or things
• Olfactory: Smelling odors
• Gustatory: Experiencing tastes
• Tactile: Feeling bodily sensations (e.g., feeling an insect crawling on one’s skin)
5. What is considered the most dangerous type of hallucination (alteration in perception) that requires immediate attention from the nurse? (p. 196 Varcarolis 9th ed.)
Command hallucination; may be dangerous and must be evaluated carefully
For example, they may be telling a patient to “jump out the window” or to “hit that nurse.” Command hallucinations are often frightening and may be a flag warning of a psychiatric emergency.
6. Be able to differentiate between the 2 types of illusions, depersonalization and derealization. (pp. 196-197 Varcarolis 9th ed.)
Depersonalization: A feeling of being unreal or having lost an element of one’s person or identity. For example, body parts do not belong, or the body has drastically changed.
Derealization: A feeling that the environment has changed (e.g., that one is detached from the environment, that everything seems bigger or smaller, or that familiar surroundings seem somehow strange and unfamiliar).
7. What is anosognosia and what nursing cares should the nurse expect to provide? (Table 12.3 p. 201; p. 584 Varcarolis 9th ed.).
Anosognosia: is the inability to realize one is ill—an inability caused by the illness itself.
nursing care
Assesment: observe their behavior and listen to their perception of the disease
Pychoeducation: help individual and family understand the nature of their condition
Collaborate with other mental health professionals: in other to develop a comprehensive treatment such as medication, therapy or combination
Build trust: establish a therapeutic relationship with the pt is crucial for cooperation in treatment regime.
Monitor and adjust; adjust treatment plan as needed.
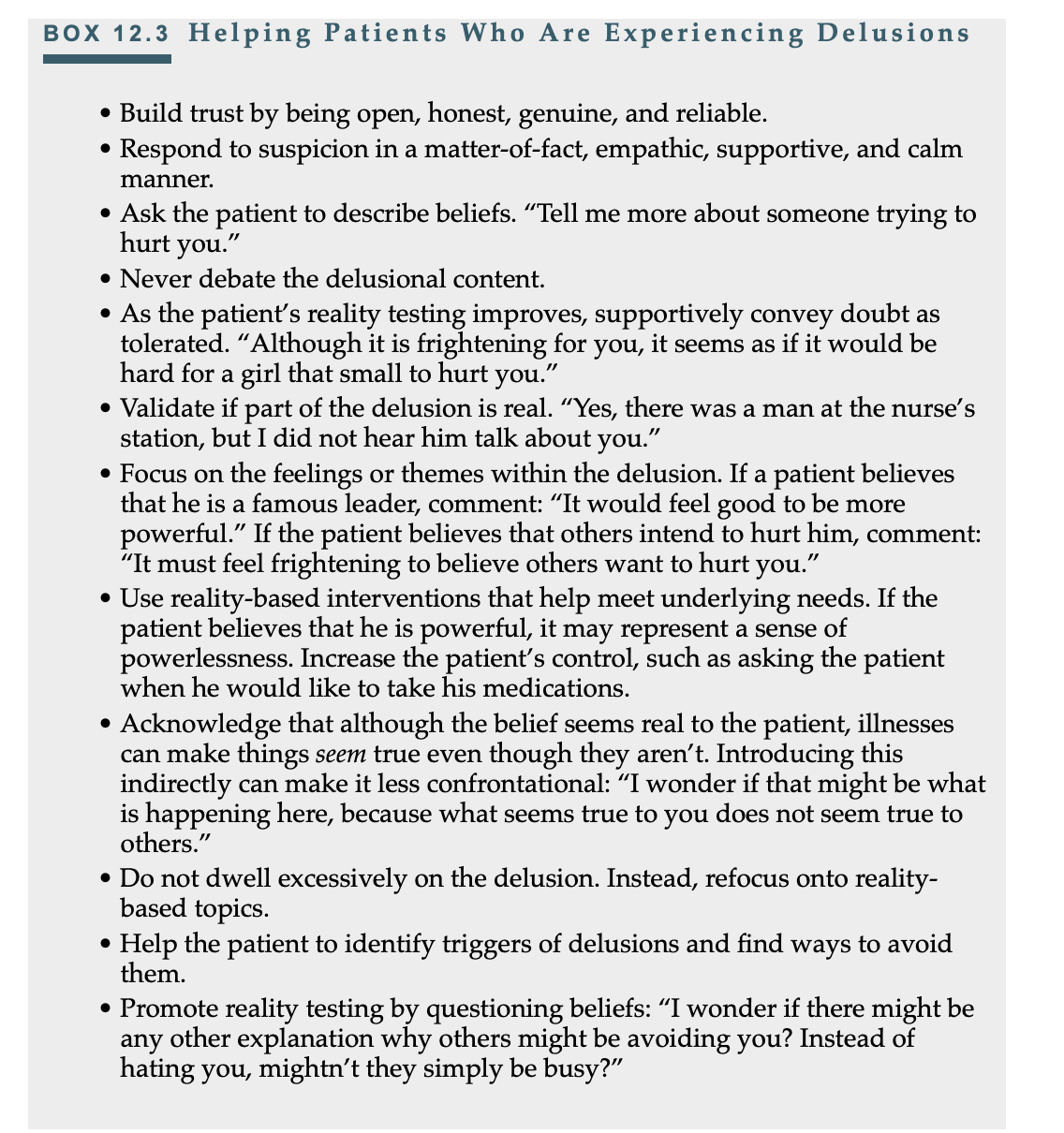
8. What should the nurse say to a patient who is experiencing delusions? (pp. 205-206 Varcarolis 9th ed.)
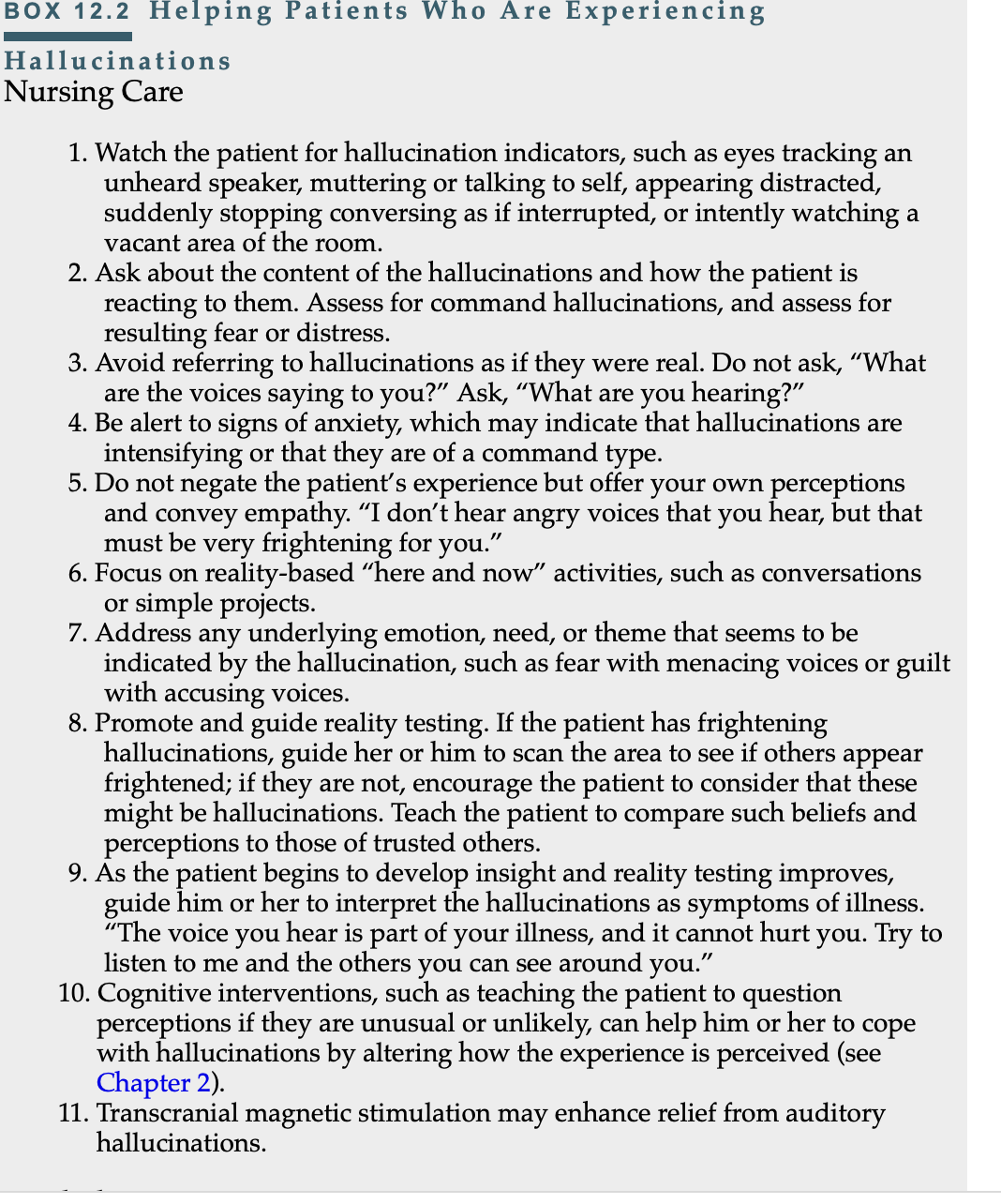
9. What should the nurse say to a patient who is experiencing hallucinations? (pp. 204-205 Varcarolis 9th ed.)
10. What are the most common side effects associated with first generation antipsychotics? (p 208; Table 12.6 pp. 213-214 Varcarolis 9th ed.). Be familiar with the side effects, symptoms of each: Neuroleptic Malignant Syndrome (NMS), Tardive dyskinesia (TD). 
11. What is the treatment for NMS, TD?
Tardive dyskinesia - screen every 3 months. in adults can be treated with two drugs (FDA recommendation)
Administer valbenazine (Ingrezza) and deutetrabenazine (Austedo).
Discontinuing the drug rarely relieves symptoms, but onset may merit reconsideration of medication.
Movements associated with tardive dyskinesia may contribute to stigmatizing response by others.
Provide support.
Teach the patient ways to conceal involuntary movements, such as holding one hand with the other.
Neuroleptic Malignant Syndrome: Prompt detection, discontinuation of the antipsychotic agent, management of fluid balance, temperature reduction, and monitoring for complications are essential.
Acute, life-threatening medical emergency
Early detection increases patient’s chance of survival.
If suspected, hold all antipsychotics and contact prescriber stat.
Transfer to a critical care unit (if in community, 911 transport to ER; notify ER of referral and reason).
Bromocriptine (Parlodel) and dantrolene (Dantrium, Ryanodex) can relieve muscle rigidity and reduce the heat (fever) generated by muscle contractions.
Cool body to reduce fever (cooling blankets; alcohol bath, cool water or ice bath as ordered).
Maintain hydration with oral or intravenous fluids; correct electrolyte imbalance.
Treat dysrhythmias.
Small doses of heparin may decrease risk of pulmonary emboli.
12. Be familiar with the four types and treatment for Extrapyramidal symptoms (EPS): Acute dystonia, Tardive Dyskinesia (TD), akathisia, pseuoparkinsonism.
Acute dystonia:A sudden, sustained contraction of one or several muscle groups, usually of the head and neck. Acute dystonias can be frightening and uncomfortable, but unless they involve muscles affecting the airway, which is rare, they are not dangerous. However, they cause significant anxiety and should be treated promptly.
limited muscle groups (e.g., tongue, face, neck, and back; usually tongue and jaw first)
Spasm of the muscles causing backward arching of the head, neck (torticollis), and spine
Eyes roll back (oculogyric crisis)
Laryngeal dystonia: could threaten airway (rare)
monitor airway
reassure pt
administer antiparkinsonian agent IM
also Benadryl IM or IV
stay with pt for support
Administer ppx oral antiparkinsonian agent
help pt understand the situation
Akathisia—A motor restlessness that causes pacing and/or an inability to stay still or remain in one place. It can be severe and distressing to patients and can be mistaken for anxiety or agitation. These symptoms may lead to mistakenly administering more of the drug that originally caused the akathisia, making it worse. A tardive form can persist despite treatment.
Consult prescriber regarding possible medication change.
Give antiparkinsonian agent as ordered.
Propranolol (Inderal), lorazepam (Ativan), or diazepam (Valium) may be used.
Relaxation exercises may be helpful.
In severe cases, may cause great distress and contribute to suicidality.
Usually subsides when antipsychotic is discontinued
Pseudoparkinsonism—A temporary group of symptoms that resemble Parkinson disease: tremor, reduced accessory movements (e.g., arms swinging when walking), gait impairment, reduced facial expressiveness (mask facies), and slowing of motor behavior (bradykinesia).
administer antiparkinsonian agents such as trihexyphenidyl (Artane) or benztropine (Cogentin).
if intolerance consults provider on reduction of dosage
provide handkerchief or towel to wipe saliva and tech on ways to prevent falls.
Tardive Dyskinesia: persistent EPS involving involuntary rhythmic movements. It develops in about 25% of patients on antipsychotics. Tardive dyskinesia is more common with first-generation antipsychotics, usually after prolonged treatment, and usually persists even after the medication has been discontinued. Smoking, alcohol, and stimulant use may increase the risk of this form of EPS. It usually begins in oral and facial muscles and progresses to include the fingers, toes, neck, trunk, or pelvis. More common in women
Administer valbenazine (Ingrezza) or deutetrabenazine (Austedo) as ordered.
Discontinuing the drug rarely relieves symptoms, but onset may merit reconsideration of medication.
Movements associated with tardive dyskinesia may contribute to stigmatizing response by others. Provide support. Teach the patient ways to conceal involuntary movements, such as holding one hand with the other.
13. What are the most common side effects associated with second generation antipsychotics? (pp. 211-214 Varcarolis 9th ed.)
second-generation antipsychotics can cause sedation, sexual dysfunction, seizures, and increased mortality in older adults with dementia.
All second-generation antipsychotics carry a risk of metabolic syndrome, which includes weight gain (especially in the abdominal area), dyslipidemia, increased blood glucose, and insulin resistance. Metabolic syndrome is a significant concern and increases the risk of diabetes, certain cancers, hypertension, and cardiovascular disease
14. Antipsychotics likely to be on the exam: clozapine (Clozaril), haloperidol (Haldol), risperidone (Risperdal), fluphenazine (Prolixin)
Clozaril help improve negative symptoms. Clozaril can also cause myocarditis and in rare cases can contribute to life-threatening bowel emergencies and new-onset diabetes as well as, rarely, ketoacidosis.
it is one of the few drugs that have FDA approval for the treatment of suicidality in schizophrenia and is the drug of choice for individuals who are unresponsive to other antipsychotics.
can cause severe neutropenia
associated with minor or no EPS
Haloperidol (Haldol): given every 4 weeks; long term treatment of psychosis. it is contraindicated for hypersensitivity and Parkinson's. it has a high potency neuroleptic drug that has a favourable. cardiovascular, anticholinergic, and sedative adverse effects can cause EPS and tardive dyskinesia
Risperidone (Risperidal): given every 2 weeks: can cause weight gain. indicative of schizophrenia and negative symptoms. causes minimal EPS.
Fluphenazine(Prolix): given every 2-3 weeks. treat schizophrenia and psychotic symptoms such as hallucination, delusions and hostility.
CHAPTER 13: BIPOLAR AND RELATED DISORDERS (ATI Chapters 14 and 23) – 10 MC, 5 select all that apply.
1. Be able to distinguish between mania and hypomania. Which is present in bipolar I and bipolar II? (pp. 219-220 Varcarolis 9th ed.)
Individual with bipolar I experience mania
Mania: a period of intense mood disturbance with persistent elevation, expansiveness, irritability, and extreme goal-directed activity or energy. These periods last at least 1 week for most of the day, every day
Individuals experiencing manic episode are energetic and euphoric.
as symptoms intensifies they become psychotic: hallucination, delusions and dramatically disturbed thought.
Individuals with bipolar II experience at lease one hypomanic episode or one major depressive episode.
Hypomania: low level and less dramatic mania. tend to be euphoric and often increase functioning.
hypomania is accompanied by excessive activity and energy for at least 4 days and involves at least three of the behavior
psychosis is never present with hypomania, but it accompanied with depressive side of the disorder.
2. How is bipolar disorder different from major depressive disorder? (pp. 219-220, 242-243 Varcarolis 9th ed.)
-Bipolar disorder alternates between states of euphoria and states of depression and/or mixed state of anxiety and depression.
Individuals with bipolar disorder tend to spend more time in a depressed state than in a manic state.
-MDD only has one phase, that being depression. length of depression episode may last 5 to 6 month.
3. Safety concerns for patients experiencing mania? (pp. 220, 223-226, Table 13.2 p. 227 Varcarolis 9th ed.)
Bc they feel so important and powerful, they engage in horrific chances and hazardous activities- do not recognize as problematic and resists treatment
- Hallucinations and delusions -- distractibility and decreased concentration
- State of depression & agitation -- lead to extreme behaviors such as
violence or attempted suicide
4. Therapeutic communication for the patient experiencing mania? (pp. 228-229 Table 13.3 Varcarolis 9th ed.)
Communication
Use a firm and calm approach- need structure and control
short and precise explanation with statement
be consistent with approach and explanation
use clear expectation
hear and act on legitimate complaint- to help reduce unneccessay acting out behaviors.
redirect energy with distraction.
Structure in the safe Millie
maintain low level stimuli in pt’s environment
provide high-calorie fluids
encourage rest period
redirect aggressive behavior
in acute media medication, restraint and seclusion can be use to minimize harm
observe for lithuim toxicity
store valuable in safe until rational judgement returns
Nutrition
monitor I&O and VS
offer high colorie meal; finger meal, sandwich, fruit, milkshakes
remind pt to eat
Sleep
encourage frequent rest period
keep pt area with low stimulation
provide hot baths at night
Hygiene
encourage appropriate clothing
provide step by step reminder of hygiene eg. here is your razor… shave from left…. now to the right
Elimination
offer food and fluid high with fiber and evaluate need for laxative. fecal compaction results from dehydration and. decrease peristalsis.
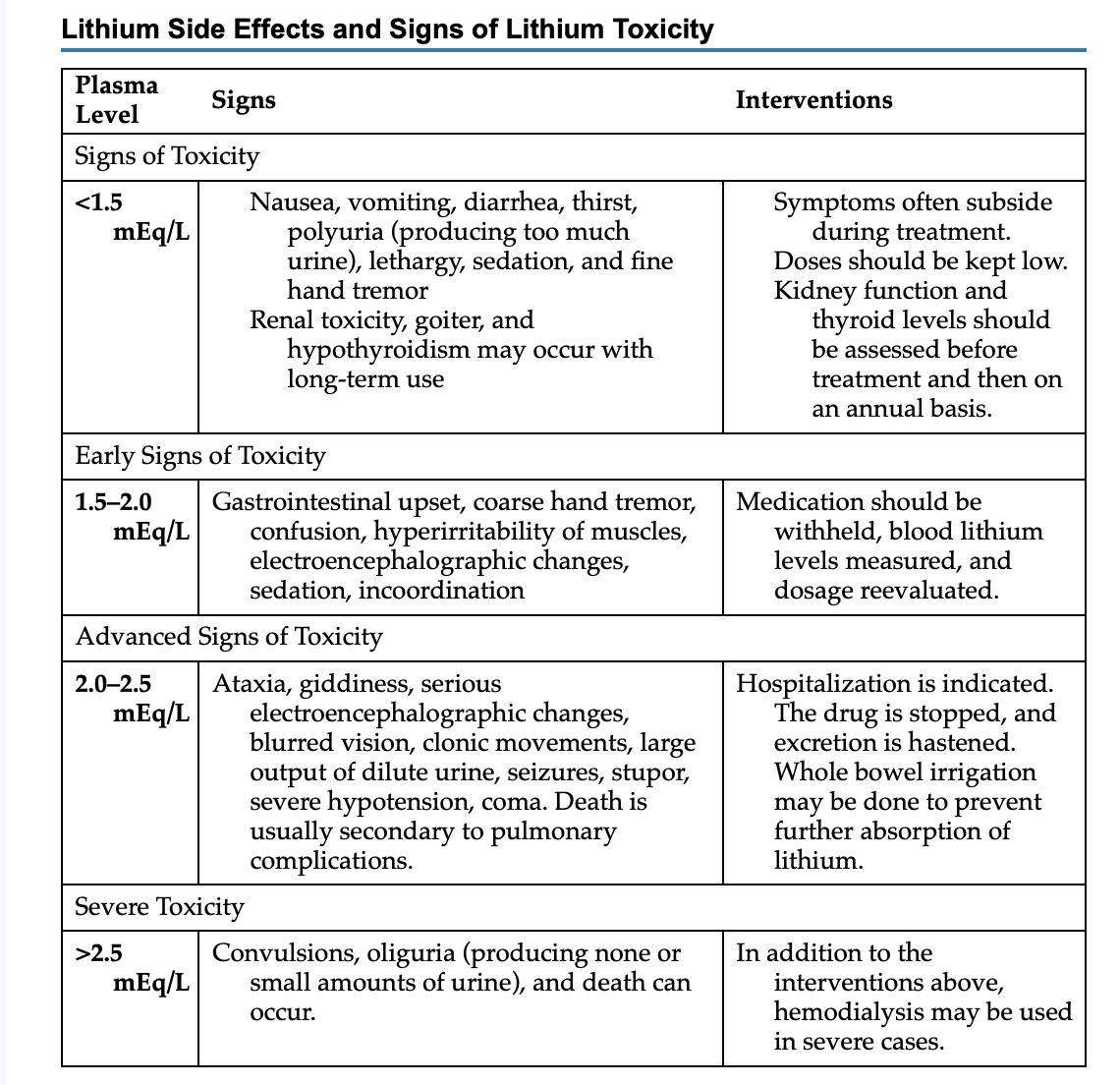
5. Therapeutic window for Lithium. (pp. 232-233 Table 13.4 Varcarolis 9th ed.; Bipolar Disorder PP)
Lithium must reach therapeutic blood levels to be effective. This usually takes 7 to 14 days, or longer for some patients. In the acute manic phase, lithium is usually started at 600 to 1200 mg a day in two or three divided doses. It is then increased every few days by 300 mg a day with a maximum dose of 1800 mg a day. A target range for a 12-hour serum trough level is 0.8–1.2 mEq/L. A greater clinical benefit for acute mania may be found in a level of 1.0–1.2 mEq/L
6. There will be one dosage calculation for daily lithium dosing. (p. 232 Varcarolis 9th ed.)
Max dose= 1800mg a day
7. Symptoms of lithium toxicity. (pp. 232-233 Table 13.4 Varcarolis 9th ed.; Bipolar Disorder PP)
Nausea, vomiting, diarrhea, thirst, polyuria, lethargy, sedation, fine hand tremor Renal toxicity, goiter, and hypothyroidism with long-term use
8. What medications used to stabilize mood for bipolar disorders increase the risk for Steven Johnson’s syndrome for those of Asian descent? (pp. 232-233 Varcarolis 9th ed.).
Carbamazepine carries a black box warning for serious dermatologic reactions. These include toxic epidermal necrolysis and Stevens-Johnson syndrome.
Patients of Asian ancestry have a 10 times greater risk for toxic epidermal necrolysis and should be genetically tested prior to using this drug.
9. What symptoms does electroconvulsive therapy (ECT) treat in bipolar disorder? (p. 234 Varcarolis 9th ed.)
ECT is most commonly used with patients who have bipolar disorder with severe levels of depression. ECT has been shown to be effective in about 80% of patients, particularly in older adults. ECT has been used effectively in mania, mixed, and depressed states of bipolar disorder as well as maintenance phases of treatment.
10. What patient and family teaching are indicated for lithium therapy? (pp. 232, 234 Box 13.2 Varcarolis 9th ed.)
Do not stop medication even if the mania episode subsides.
Lithium is not addictive.
It is important to monitor lithium blood levels closely until a therapeutic level is reached. After this level is reached, continued monitoring will be required to prevent toxicity. You will need more frequent blood level monitoring at first, then once every several months after that.
It is important to maintain a consistent fluid intake (1500–3000 mL/day or six 12-oz glasses of fluid).
Sodium intake can affect lithium levels. High sodium intake leads to lower levels of lithium and less therapeutic effect. Low sodium intake leads to higher lithium levels, which could produce toxicity. Aim for consistency in sodium intake.
You should stop taking lithium if you have excessive diarrhea, vomiting, or sweating. All of these symptoms can lead to dehydration and increase blood lithium to toxic levels. Inform your care provider if you have any of these problems.
Let your prescriber know if you take diuretics (water pills).
Talk to your prescriber about having your thyroid, parathyroid, and renal function checked periodically due to risk for hypothyroidism, hyperthyroidism, hyperparathyroidism, and decreased kidney function.
Don’t take over-the-counter medicines without checking with your prescriber. Even non-steroidal anti-inflammatory drugs (e.g., ibuprofen, naproxen) may influence lithium levels.
Take lithium with meals to avoid stomach irritation.
In the first week, you may gain up to 5 pounds of water weight. Additional weight gain may occur, particularly with females. Discuss how much weight gain is acceptable with your prescriber.
Groups are available to provide support for people with bipolar disorder and their families. A local self-help group is [provide a name and telephone number].
You can find out more information by calling [provide a name and telephone number].
Keep a list of side effects and toxic effects handy, along with the name and number of a contact person
If lithium is to be discontinued, the dosage will be tapered gradually to minimize the risk of relapse.
11. What are the classifications of and the common and adverse side effects for: Lithobid (Lithium); Carbamazepine (Tegretol); Lamotrigine (Lamictal); Lurasidone (Latuda); and Cariprazine (Vraylar). (pp. 232-235 Varcarolis 9th ed.)
Lithobid (Lithium); Lithium is particularly effective in reducing the following:
Elation, grandiosity, and expansiveness
Flight of ideas
Irritability and manipulation
Anxiety
Self-injurious behavior
To a lesser extent, lithium controls the following:
• Insomnia
• Psychomotor agitation
• Threatening or assaultive behavior
• Distractibility
• Hypersexuality
• Paranoia
Common side effect: N & V, diarrhea, thirst, polyuria, lethargy, sedation, and fine hand tremor
Carbamazepine (Tegretol); indicated for acute mania and mixed states. considered a second-line treatment.
Common side effects include dizziness, somnolence, nausea, vomiting, ataxia, constipation, pruritis, dry mouth, weakness, blurred vision, and speech problems. Liver enzymes should be monitored at least weekly for the first 8 weeks of treatment because the drug can increase levels of liver enzymes that can speed its own metabolism.
Lamotrigine (Lamictal); maintenance therapy medication approved for people 18 years and older
Common adverse reactions include dizziness, headache, diplopia (double vision), ataxia, blurred vision, nausea, somnolence, rhinitis, and pharyngitis.
Lurasidone (Latuda): second generation antipsychotic. that can cause metabolic syndrome; a cluster of problems such as high blood pressure, high blood glucose, excess body fat around the waist, and abnormal cholesterol level
Cariprazine (Vraylar): can cause metabolic syndrome such as weight gain; a cluster of problems such as high blood pressure, high blood glucose, excess body fat around the waist, and abnormal cholesterol level
12. Substance abuse, anxiety, and sleep disorders are co-morbid with bipolar disorders. Know which bipolar disorders (bipolar I, II, and cyclothymia) they are highest in and why. (p. 222 Varcarolis 9th ed.)
Anxiety – Bipolar I & II
Substance abuse – cyclothymic disorder, arise with Bipolar II Sleep disorders – cyclothymic disorder
Chapter 14 Depression
1. What is persistent depressive disorder (dysthymia) and how does it differ from major depressive disorder (MDD)? (p. 241 Varcarolis 9th ed.)
Persistent depressive disorder, formerly known as dysthymia (dys – bad + thymia – mood), is diagnosed when low-level depression occurs most of the day, for the majority of days. These depressive feelings last at least 2 years in adults and 1 year in children and adolescents. In addition to depressed mood, individuals with this disorder have at least two of the following: decreased appetite or overeating, insomnia or hypersomnia, low energy, poor self-esteem, difficulty thinking, and hopelessness.
Major depressive disorder: Major depressive disorder, or major depression, is characterized by a persistently depressed mood lasting for a minimum of 2 weeks.
The length of a depressive episode may be 5 to 6 months About 20% of cases become chronic (i.e., lasting more than 2 years). While depression begins with a single occurrence, most people experience recurrent episodes. People experience a recurrence within the first year about 50% of the time and within a lifetime up to 85% of the time.
-NO history of manic or hypomanic episodes
-Subtypes: Depression and the seasons, depression of grieving, psychotic features, atypical features, catatonic features, and postpartum onset
2. What is the DSM 5 criteria for MDD? (pp. 242-243 Varcarolis 9th ed)
DSM-5 criteria: % or more of the following symptoms nearly every day for most waking hrs. Over same 2-week period:
-Affect (depressed mood)
-anhedonia= loss of pleasure in living
-Anergia-lack of energy
-weight loss/gain
-sleep disturbances
-lack of motivation
-Feeling worthless or excessive guilt
- difficult thought process, concentration or making decisions - suicidal thoughts
3. Be familiar with the vegetative signs of depression and nursing interventions. (p. 250 & 256 Varcarolis 9th ed.)
-NO history of manic or hypomanic episodes
-Subtypes: Depression and the seasons, depression of grieving, psychotic features, atypical features, catatonic features, and postpartum onset
2. What is the DSM 5 criteria for MDD? (pp. 242-243 Varcarolis 9th ed)
DSM-5 criteria: % or more of the following symptoms nearly every day for most waking hrs. Over same 2-week period:
-Affect (depressed mood)
-anhedonia= loss of pleasure in living
-Anergia
-weight loss/gain
-sleep disturbances
-lack of motivation
-Feeling worthless or excessive guilt
- difficult thought process, concentration or making decisions - suicidal thoughts
3. Be familiar with the vegetative signs of depression and nursing interventions. (p. 250 & 256 Varcarolis 9th ed.)
Vegetative symptoms: refer to alterations in those activities necessary to support physical life and growth (e.g., eating, elimination, sleeping, and sex).
- Sleep disturbances (insomnia, wake frequently, and have a total reduction in sleep)
- Appetite disturbances
- Changes in bowel habits (constipation)
- Sexual interest declines (loss of libido)
Nursing interventions: Nutrition (Anorexia):
Offer small, high-calorie, and high-protein snacks frequently throughout the day and evening.
Offer high-protein and high-calorie fluids frequently throughout the day and evening.
When possible, encourage family or friends to join the patient during meals.
Include the patient in choosing foods and drinks. Involve a dietitian if necessary.
Weigh the patient weekly and observe the patient’s eating patterns.
Sleep (insomnia)
Provide periods of rest after activities.
Encourage the patient to get up and dress and to stay out of bed during the day.
Encourage the use of relaxation measures in the evening (e.g., a warm bath, warm milk, soothing music or sounds).
Provide decaffeinated coffee and soda.
Elimination (constipation):
- Monitor intake and output, especially bowel movements. - Offer foods high in fiber and provide periods of exercise. - encourage fluid intake
- evaluate need for laxatives, enemas
4. Which antidepressants are first line for treatment for depression? SSRI’s, SNRI’s, tricyclics, monoamine oxidase inhibitors (MAOI’s)? (p. 256-261 Varcarolis 9th ed.)
- Provide periods of rest after activities.
- Encourage the patient to get up and dress and to stay out of bed during the day.
- Encourage the use of relaxation measures in the evening (e.g., a warm bath, warm milk, soothing music or sounds).
- Provide decaffeinated coffee and soda. Elimination (constipation):
- Monitor intake and output, especially bowel movements. - Offer foods high in fiber and provide periods of exercise. - encourage fluid intake
- evaluate need for laxatives, enemas
4. Which antidepressants are first line for treatment for depression? SSRI’s, SNRI’s, tricyclics, monoamine oxidase inhibitors (MAOI’s)? (p. 256-261 Varcarolis 9th ed.)
SSRIs: Block reuptake of serotonin
- 1ST LINE THERAPY for depression & anxiety (OCD, Panic disorders)
- Citalopram (celexa)
- Escitalopram (lexapro)
- Fluoxetine (prozac)
- Paroxetine (paxil)
- Sertraline (zoloft)
**STOP DRUG IF SEROTONIN SYNDROME OCCURS
SNRIs: Block reuptake of seroronin & NE
- SNRIs may increase BP
- Venlafaxine (effexor)= used 1st if SSRIs fail
- Duloxetine (cymbalta)
- Desvenlafaxine (pristiq, khedezla)
- Levo milnacipran (Fet-zima)
MAOIs: Prevents breakdown of NTs = norepinephrine, serotonin, dopamine, & tyramine
Inhibits the enzyme monoamine oxidase (breaks down excess tyramine)
Increases amount of available:
o Norepinephrine
o Serotonin
o Dopamine
o Tyramine
- Prescribed when other antidepressants fail (last line) - highly treatment resistant depression
- FDA Approved:
o Phenelzine (Nardil)o Selegiline (Emsam) (transdermal patch)
- no dietary restrictions when used at the lowest dose
o Tranylcypromine (Parnate)
o Isocarboxazid (Marplan)
- Toxic effects
Restrictions to tyramine foods (regulated BP)
o Very high BP when taken w/ foods containing tyramine or certain meds (serotonin): Increased risk for hypertensive crisis
Hypertensive crisis: Occurs 15-90 min of ingestion of offending substance (tyramine + MAOI):
o Headache – **initial symptom
o Very high BP
o Increased body temperature (pyrexia)
o Stiff or sore neck
o Palpitations
o Sweating
o Increased or decreased HR (possibly with chest pain)o N&V
5. Which of the antidepressants have the potential to be lethal? (p. 256-261 Varcarolis 9th ed.)
TCAs should be used cautiously in suicidal patients since they are lethal in overdoses.
6. What are the signs and symptoms of serotonin syndrome? (p. 257 and Box 14.3 p. 259 Varcarolis 9th ed.)
abdominal pain
diarrhea
sweating
fever
tachycardia
elevated blood pressure
altered mental state (delirium)
myoclonus (muscle spasms)
increased motor activity
irritability
hostility
mood change
Severe manifestations can induce hyperpyrexia
7. What nursing interventions are indicated for the patient with serotonin syndrome?

Stop the drug!!
Initiate Symptomatic tx:
Serotonin receptor blockage= Propranolol (inderal)
Cooling blankets
Diazepam (valium) for muscle rigidity
Anticonvulsants
Artificial ventilation
Chapter 25 Suicide and Non-suicidal Self-Injury
1. When evaluating lethality of a suicide plan, what 3 questions should be asked of the patient immediately? (p. 476 Varcarolis 9th ed.)
1) Is there a specific plan with details?
2) How lethal is the proposed method?
3) Is there access to the planned method?
2. What are high and low risk lethality methods? (p. 476 Varcarolis 9th ed.)
Higher-risk methods, also referred to as hard methods, include:
• Using a gun
• Jumping off a high place
• Hanging
• Poisoning with carbon monoxide
• Staging a car crash
lower-risk methods, also referred to as soft methods, include:
• Cutting wrists
• Inhaling natural gas
• Ingesting pills
3. What environmental safety methods for minimizing suicidal behavior should be in place on the psychiatric unit? (p. 479 and Box 25.4 p. 481 Varcarolis 9th ed.)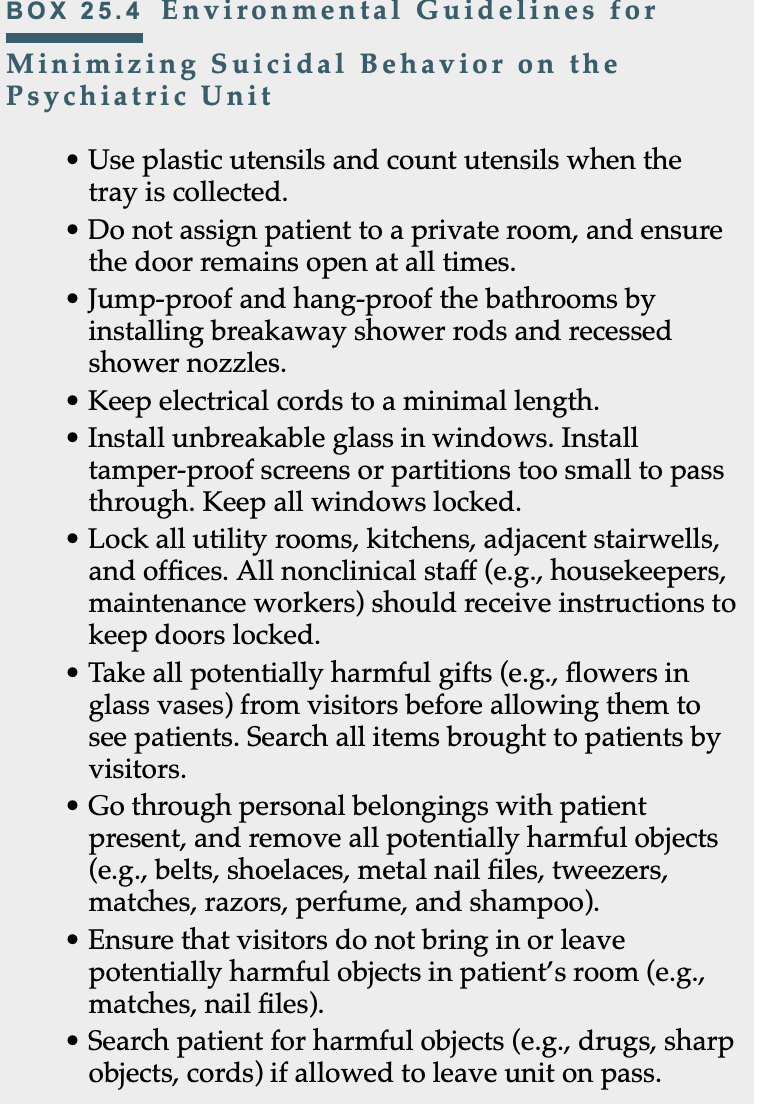
CHAPTER 27: ANGER, AGGRESSION, & VIOLENCE
Be able to distinguish between (definitions, symptoms):
1. Anger (p. 502 V9th ed.): is an emotional response to frustration of desires, a threat to one’s needs (emotional or physical), or a challenge. It is a normal emotion that can even be positive when it is expressed in a healthy way
2. Aggression (p. 502 V9th ed.): is an action or behavior that results in a verbal or physical attack. Aggression tends to be used synonymously with violence
3. Violence (p. 502 V9th ed.): violence is always an objectionable act that involves intentional use of force that results in, or has the potential to result in, injury to another person.
4. Bullying (p. 504 V9th ed.): Bullying is any negative activity, including teasing, kicking, hitting, and spitting, intended to bother or harm someone else.
5. What medications are used for acute de-escalation?
Antipsychotics and antianxiety meds
Haloperidol (haldol)- first gen antipysch
Loxapine (adasuve)- inhalation powder single use FGA, limit use due to SE fatal bronchospasm
Olanzapine (zyprexa)- 2nd gen
Ziprasidone (geodon)-2nd gen
Orally disintegrating tablets- olanzapine and risperidone (risperdal)
COMBOs- Haldol (or zyprexa) + Ativan + Benadryl (or Cogentin)
6. What can the nurse do to avoid a patient escalation?
acknowledge the distress, stress (validates feelings and indicates willingness to find solutions)
develop a relationship of trust:
numerous brief, nonthreatening, nondirective interactions
“good morning!”, “hello!”, “how is your day?”
-topic examples: weather, sports, something interesting to the patient
Chapter 32 Serious Mental Illness
1. What factors contribute to nonadherence of the treatment plan? (pp. 584-585 Varcarolis 9th ed.)
Anosognosia
Medication side effects
Medication costs
Lack of trust in providers
Poor access to care
Stigma of mental illness
2. What nursing interventions are likely to improve adherence to treatment? (Box 32.1 p. 585 Varcarolis 9th ed.)
Encourage careful selections of medications that are most likely to be effective, well tolerated, and acceptable to the patient
- Help manage side effects to minimize distress
- Simplify treatment regimens to make it more acceptable and
understandable to pt
- Tie treatment adherence to achieving patient’s goal to increase
motivation
- Assign consistently committed caregivers
- Educate patient and family about SMI and the role of treatment in
recovery
- Minimize obstacles to treatment by aiding with treatment costs and
access
- Involve pt and family in support groups
- Provide culturally sensitive care
- When other interventions not successful, use medication monitoring and
long-acting forms
- Never reject, blame, or shame the patient when nonadherence occurs
Simulation
What does the PHQ-9 used to access?
Major Depressive Disorder
Suicidal ideation
PHQ-9 scoring
0-4 none
5-9 mild
10-14 moderate.
15-19 moderately severe
20-27 severe