5 & 6 X-Ray Contrast, Radiation Dose, & Image Artifacts
[[Intro[[
- All photons impart energy to the object
- All photons deliver a dose of energy
- As photons interact with matter, they are absorbed, scattered, or transmitted
- Exposure: The amount if radiation in air measured by radiation monitors
- Exposure is measured in roentgen (R) and coulomb/kg
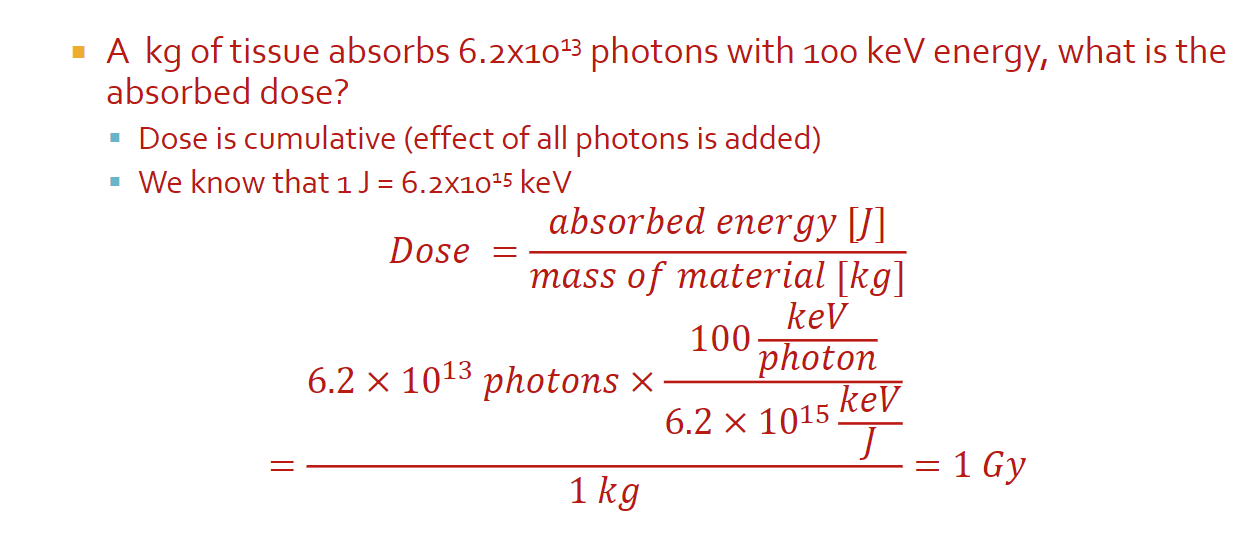
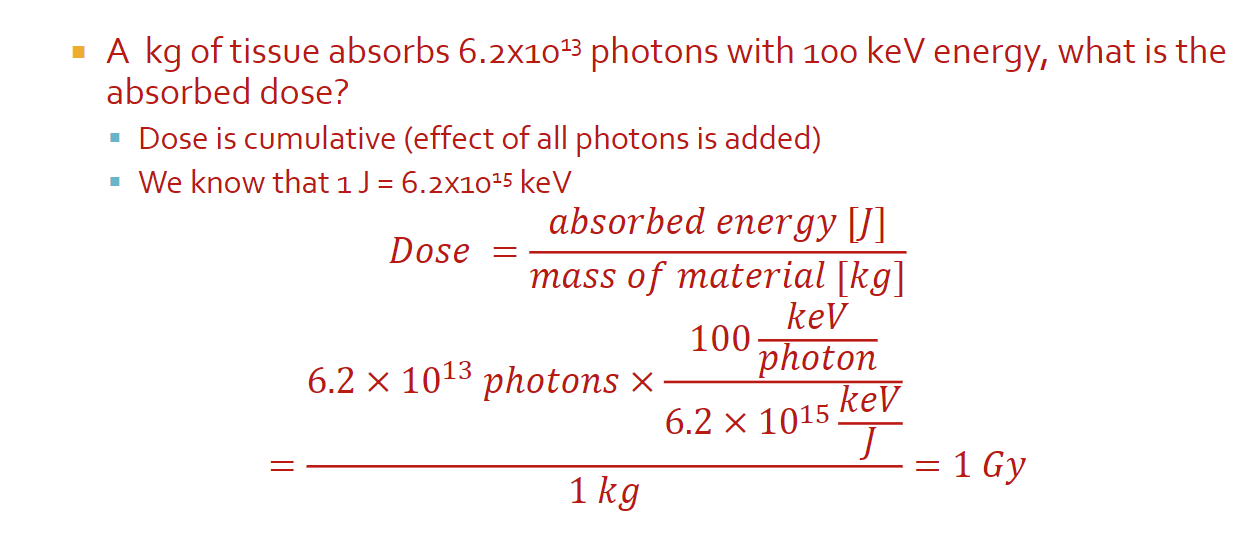
- Absorbed dose: The dose of radiation (energy) you are delivering to the tissue, measured by the energy absorbed
- The absorbed dose is measured in units of gray (Gy)
- 1 Gy = 1 J absorbed by 1kg of tissue
- Used to be rad (radiation absorbed dose) which is 0.01 Gy
- Math
- 1 J = 6.2 x 10^15 keV
- All can be done with just units
Biological Effect of Dose
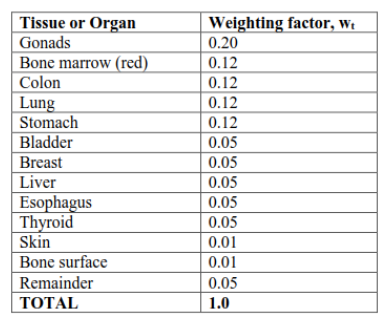
- Risk to different tissue is dependant on tissue type and the type of radiation
- Dose equivalent: A measure of the biological damage to living tissue as a result of the absorbed dose; the biological dose that delivers the same degree of risk to a tissue regardless of the radiation type
- Dose equivalent is measured in Severt (Sv) which is Gy times quality factor (f)
- Usually in mSV (small numbers)
- Effective dose: An estimate ofo the stochastic effect that a non-uniform radiation dose has on the whole body; weighted sum of dose equivalent by all organs
- Sum of each organ: weighting factor times (absorbed dose of the organ times f)
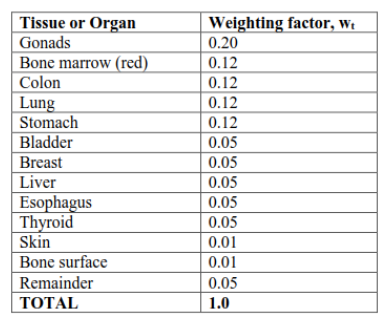
Image Contrast
- Contrast: The difference between foreground and background on an image
- In x-rays, contrast represents the difference in attenuation properties (μ) of materials along a path
- When μ increases, image brightness increases
- When the change in μ increases, image contrast increases
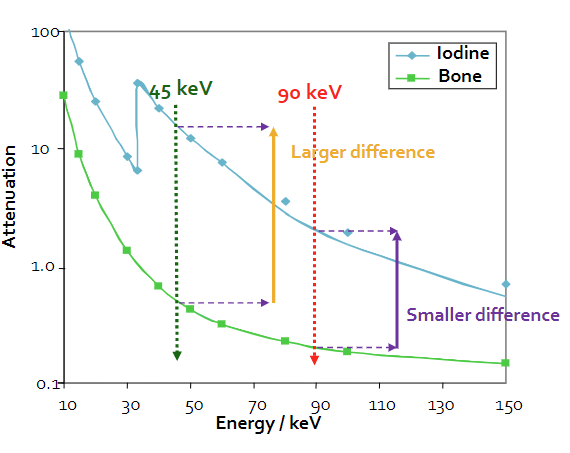
- Generally, μ decreases with energy, but it depends on the material
- Iodine injections have a higher attenuation coefficient and are used to increase contrast in imaging
- Increasing the energy decreases the change in attenuation coefficient, which can also be used to improve contrast (so that more particles hit your receptor)
Beam Intensity
- Beam intensity: The rate of change of the number of photons per unit area, represented by I
- I = (number photons/area)/change in time
- I(x) = I0 * e^-μx
- We will use “I” (intensity) interchangeably with “N” (number of photons), especially as a relative measure, however, keep in mind that they are representing different things
- Beams are polychromatic or polyenergetic (can be used interchangably)
Spectrum Effective Energy
- Effective energy is the weighted average of the spectrum energies (needed because x-rays are polychromatic)
- Because effective energy is different for different materials, we pick the μ that has the biggest difference between materials
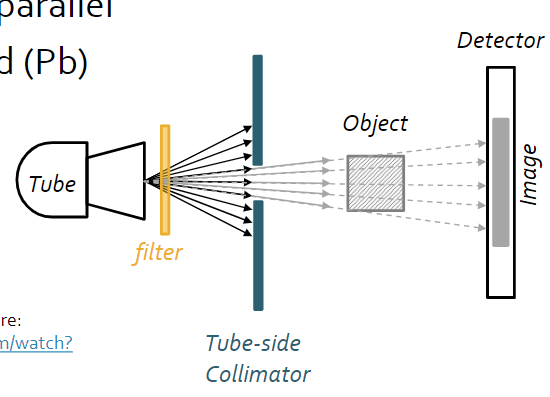
- Filters: Something used to reshape the radiation spectrum to eliminate energies that don’t contribute to the image, but do deliver dose
- Removing photons from the spectrum depends on their energy, the filter material, and the filter’s path length
- For math, remember you cannot use the same μ for different energies
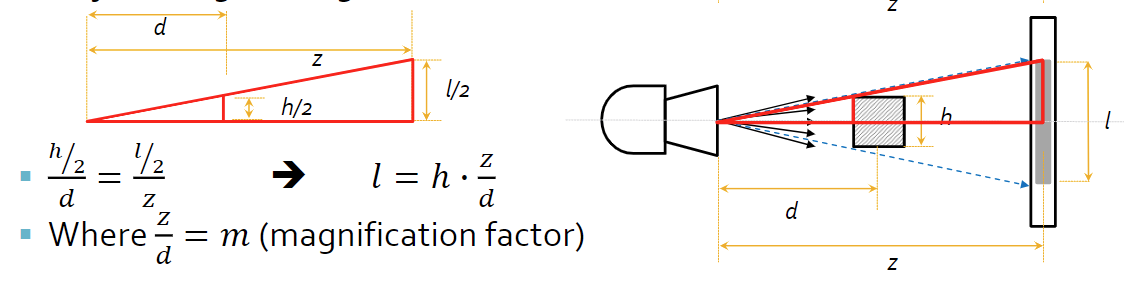
[[System & Beam Geometry[[
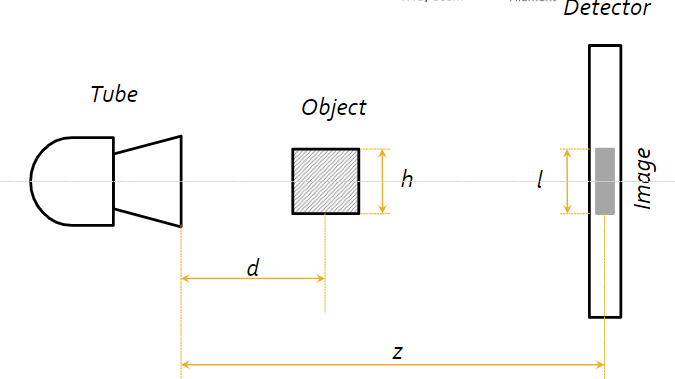
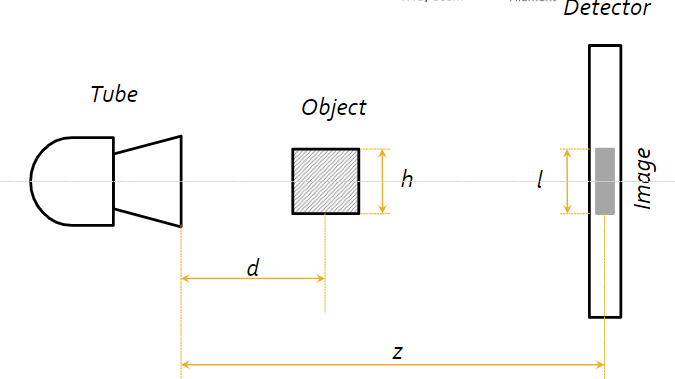
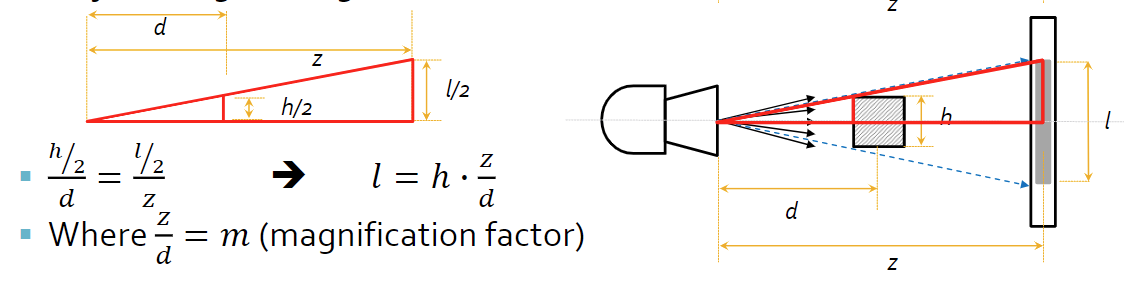
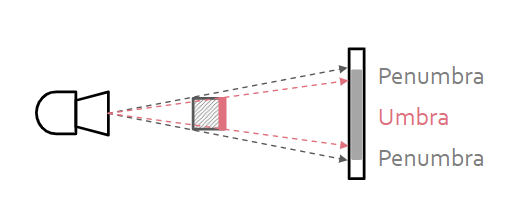
- Source-object distance (SOD): How far is the sample from the source?
- Source-image distance (SID): How far is the source from the detector image?
- Object size (h)
- Image size (l)
- Magnification factor: How much larger is the image from the actual sample?
- Parallel beam geometry is the ideal geometry, stating that all the beams move parallel to one another
- Parallel beam geometry has some limitations, because the source size must be as large as the largest object imaged, it’s inconsisent with particle physics, and complex
- Parallel beam geometry suggests simple math and no need to calculate the true size of the object from the image
- No magnification effect from a parallel beam
- Fan (divergent) beam geometry (non-ideal) suggests that the beams come out from the source in a cone-like shape
- Fan beam geometry have a more compact, practical design, and is more consistent with physics
- Fan beam geometry requires magnification factor to be taken into account, as well as depth dependent magnification (objects must be the same distance from tube)
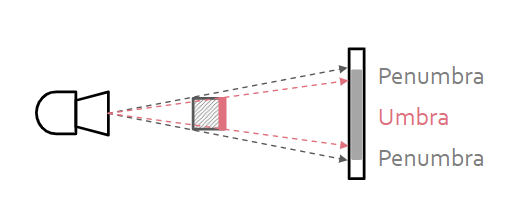
- To reduce the radiation sent to parts of the body that we don’t want to image, we use a tube-side collimator, which focuses beam on the center of the object, making the beams closer to parallel
- To reduce non-parallel beams and scattered photons, we use a detector-side collimator, or more commonly a radiographic grid, to absorb any scattered photons that are trying to reach the detector that would otherwise create noise