GZOO111-Urinary-System
![]() Feel free to leave criticism and/or suggestions about this reviewer.
Feel free to leave criticism and/or suggestions about this reviewer.
Urinary System (Expiratory System)
Functions of the Urinary System
Kidneys Dispose of Waste Products in Urine
- Nitrogenous wastes
- Toxins
- Drugs
- Excess ions
Kidneys’ Regulatory Functions
- Production of renin to maintain blood pressure.
- Production of erythropoietin to stimulate red blood cell production.
 Conversion of vitamin D to its active form.
Conversion of vitamin D to its active form.
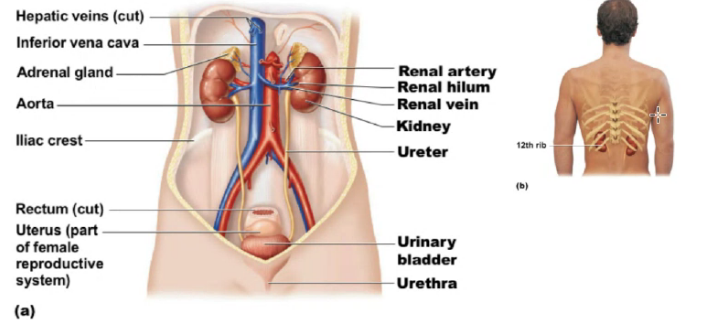
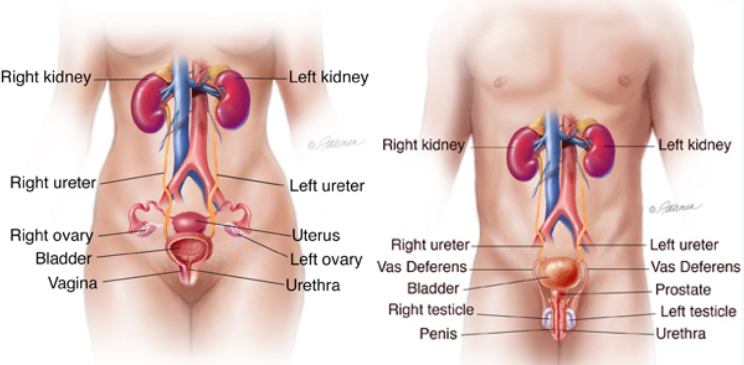
Location of the Kidney
- The kidneys are situated against the dorsal body wall in a retroperitoneal position (behind the parietal peritoneum)
- The kidneys are situated at the level of the T12 to L3 vertebrae.
 The right kidney is slightly lower than the left (because of the position of the liver).
The right kidney is slightly lower than the left (because of the position of the liver).
Structure of the Kidney
- An adult kidney is about 12 cm (5 in) long and 6 cm (2.5 in) wide.
- Renal hilum
- A medial indentation where several structures enter or exit the kidney (ureters, renal blood vessels, and nerves).
- An adrenal gland sits atop each kidney.
Three Protective Layers Enclosing the Kidney
Fibrous Capsule
Encloses each kidney.
Perirenal Fat Capsule
Surrounds the kidney and cushions against blows.
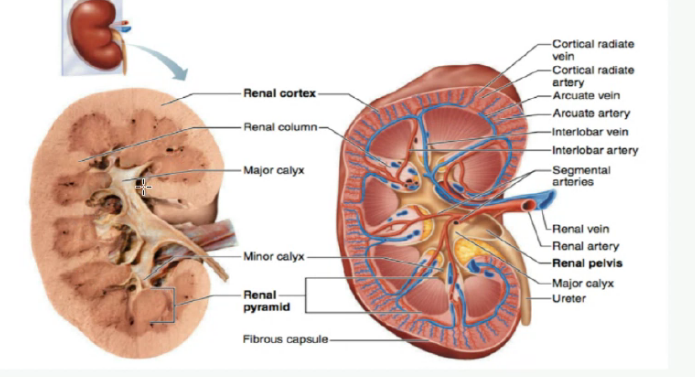
Three Regions of the Kidneys
Renal Cortex
Outer region.
Renal Medulla
Deeper region.
- Renal (medullary) pyramids – triangular regions of tissue in the medulla.
- Renal columns – extensions of cortex-like material that separate the pyramids.
Renal Pelvis
Medial region that is a flat, funnel-shaped tube.
- Calyces form cup-shaped “drains” that enclose the renal pyramids.
- Calyces collect urine and send it to the renal pelvis, on to the ureter, and to the urinary bladder for storage.
![]() Nephrons
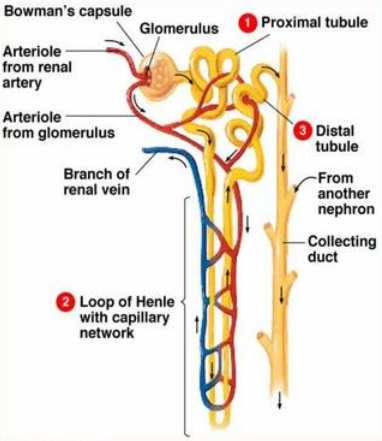
Nephrons
Structural and functional units of the kidneys.
- Each kidney contains over a million nephrons.
- Each nephron consists of two main structures.
- Renal Corpuscle
 Renal Tubule
Renal Tubule
Renal Corpuscle
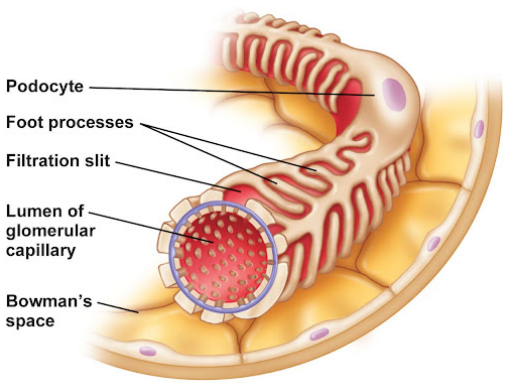
Glomerulus
A knot of capillaries made of podocytes.
Podocytes
Make up the inner (visceral) layer of the glomerular capsule.
- Foot processes cling to the glomerulus.
 Filtration slits create a porous membrane – ideal for filtration.
Filtration slits create a porous membrane – ideal for filtration.
Glomerular (Bowman’s) Capsule
A cup-shaped structure that surrounds the
glomerulus.
- First part of the renal tubule.
Renal Tubule
Extends from glomerular capsule and
ends when it empties into the collecting
duct.
Subdivisions of the Renal Tubule
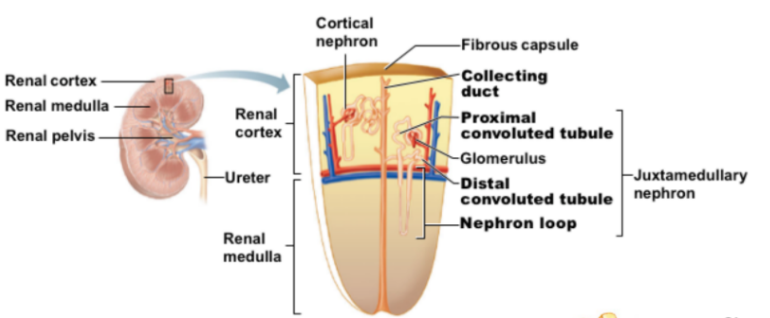 Proximal Convoluted Tubule (PCT)
Proximal Convoluted Tubule (PCT)- Nephron Loop (Loop of Henle)
- Distal Convoluted Tubule (DCT)
- Cortical Nephrons
- Located entirely in the cortex.
- Include most nephrons.
- Juxtamedullary Nephrons
- Found at the cortex-medulla junction.
- Nephron loop dips deep into the medulla.
- Collecting ducts collect urine from both types of nephrons, through the renal pyramids, to the calyces, and then to the renal pelvis.
Glomerulus
- Fed and drained by arterioles.
- Afferent Arteriole – arises from a cortical radiate artery and feeds the glomerulus.
- Efferent Arteriole – receives blood that has passed through the glomerulus.
- Specialized for filtration.
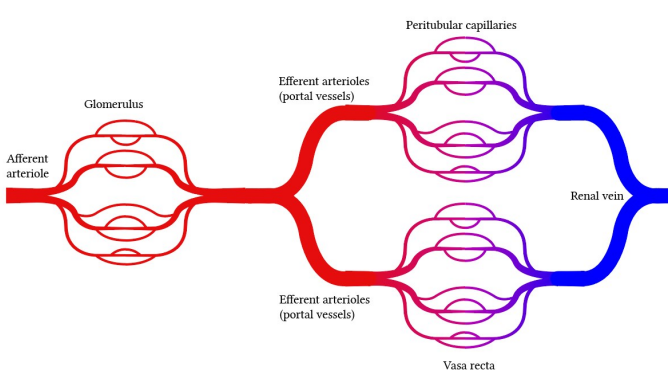 High pressure forces fluid and solutes out of blood and into the glomerular capsule.
High pressure forces fluid and solutes out of blood and into the glomerular capsule.
Peritubular Capillary Beds
- Arise from the efferent arteriole of the glomerulus.
- Low-pressure, porous capillaries.
- Adapted for absorption instead of filtration.
- Cling close to the renal tubule to receive solutes and water from tubule cells.
- Drain into the interlobar veins.
![]() Blood Supply
Blood Supply
One-quarter of the total blood supply of the body passes through the kidneys each minute.
- Renal artery provides each kidney with arterial blood supply.
- Renal artery divides into segmental arteries 🡪 interlobar 🡪 arcuate arteries 🡪 cortical radiate arteries.
- Venous blood flow, Cortical radiate veins 🡪 arcuate veins 🡪 interlobar veins 🡪 renal vein.
- There are no segmental veins.
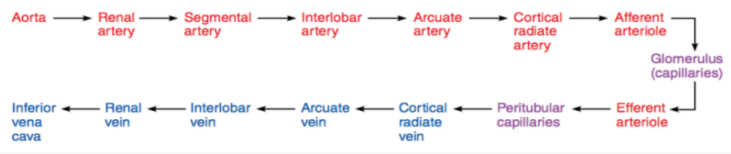 Renal vein returns blood to the inferior vena cava.
Renal vein returns blood to the inferior vena cava.
Urine Formation and Characteristics
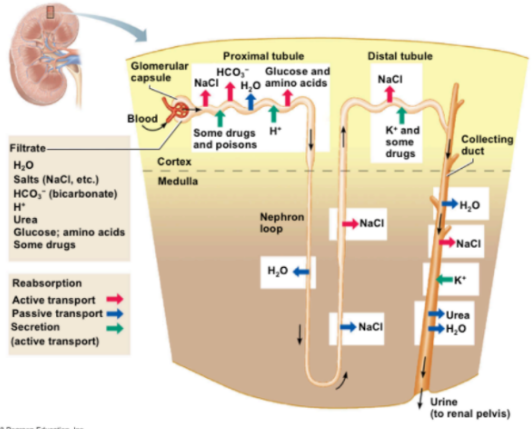
![]() Glomerular Filtration
Glomerular Filtration
The glomerulus is a filter.
- Filtration is a non-selective passive process.
- Water and solutes smaller than proteins are forced through glomerular capillary walls.
- Proteins and blood cells are normally too large to pass through the filtration membrane.
- Once in the capsule, fluid is called filtrate.
- Filtrate leaves via the renal tubule.
- Filtrate will be formed as long as systemic blood pressure is normal.
- If arterial blood pressure is too low, filtrate formation stops because glomerular pressure will be too low to form filtrate.
![]() Tubular Reabsorption
Tubular Reabsorption
The peritubular capillaries reabsorb useful substances from the renal tubule cells, such as:
- Water
- Glucose
- Amino Acids
- Ions
- Some reabsorption is passive; most is active (ATP).
- Most reabsorption occurs in the proximal convoluted tubule.
Tubular Secretion
- Reabsorption in reverse.
- Some materials move from the blood of the peritubular capillaries into the renal tubule to be eliminated in filtrate.
- Hydrogen and potassium ions
- Creatinine
- Some materials move from the blood of the peritubular capillaries into the renal tubule to be eliminated in filtrate.
- Materials left in the renal tubule move toward the ureter.
- Nitrogenous wastes.
- Nitrogenous waste products are poorly reabsorbed.
- Tend to remain in the filtrate and are excreted from the body in the urine.
 In 24 hours, about 1.0 to 1.8 liters of urine are produced.
In 24 hours, about 1.0 to 1.8 liters of urine are produced.
Urea – end product of protein breakdown.
Uric Acid – results from nucleic acid metabolism.
![]() Creatinine – associated with creatine metabolism in muscles.
Creatinine – associated with creatine metabolism in muscles.
Urine vs. Filtrate
- Filtrate contains everything that blood plasma does (except proteins).
- Urine is what remains after the filtrate has lost most of its water, nutrients, and necessary ions through reabsorption.
- Urine contains nitrogenous wastes and substances that are not needed.
Urine Characteristics
- Clear and pale to deep yellow in color.
- Yellow color is normal and due to the pigment urochrome (from the destruction of hemoglobin) and solutes.
- Dilute urine is a pale, straw color.
- Sterile at the time of formation.
- Slightly aromatic, but smells like ammonia with time.
- Slightly acidic (pH of 6)
- Specific gravity of 1.001 to 1.035.
![]() Solutes Normally Found in Urine
Solutes Normally Found in Urine
- Sodium and potassium ions
- Urea, uric acid, creatinine
- Ammonia
- Bicarbonate ions
Solutes NOT Normally Found in Urine
- Glucose
- Blood proteins
- Red blood cells
- Hemoglobin
- WBCs (pus)
- Bile
Ureters
Slender tubes 25 – 30 cm (10 – 12 inches) attaching the kidney to the urinary bladder.
- Continuous with the renal pelvis.
- Enter the posterior aspect of the urinary bladder.
- Run behind the peritoneum.
Urinary Bladder
Smooth, collapsible, muscular sac situated posterior to the pubic symphysis.
- Stores urine temporarily.
- Trigone – triangular region of the urinary bladder base based on three openings.
- Two openings from the ureters (ureteral orifices).
- One opening to the urethra (internal urethral orifice).
- In males, the prostate surrounds the neck of the urinary bladder.
Wall of the Urinary Bladder
- Three layers of smooth muscle collectively called the detrusor muscle.
- Mucosa made of transitional epithelium.
- Walls are thick and folded in an empty urinary bladder.
- Urinary bladder can expand significantly without increasing internal pressure.
Urethra
- Thin-walled tube that carries urine from the urinary bladder to the outside of the body by peristalsis.
 Release of urine is controlled by two sphincters.
Release of urine is controlled by two sphincters.- Internal Urethral Sphincter
- Involuntary and made of smooth muscle.
- External Urethral Sphincter
- Voluntary and made of skeletal muscle.
- Internal Urethral Sphincter
Location:
- Females – carries only urine
- Males – carries urine and sperm.
Length
- Females – 3 to 4 cm (1.5 inches long)
- Males – 20 cm (8 inches long.
Location
- Females – anterior to the vaginal opening.
- Males – travels through the prostate and penis.
Prostatic urethra, Membranous urethra, Spongy urethra
Micturition
Voiding, or emptying of the urinary bladder.
- Two sphincters control the release of urine, the internal urethral sphincter and external urethral sphincter
- Bladder collects urine to 200 ml
- Stretch receptors transmit impulses to the sacral region of the spinal cord.
- Impulses travel back to the bladder via the pelvic splanchnic nerves to cause bladder contractions.
- When contractions become stronger, urine is forces past the involuntary.
- Internal sphincter into the upper urethra.
- The external sphincter is voluntarily controlled, so micturition can usually be delayed.
- Fluid, electrolyte, and acid-base balance.
 Blood composition depends on three factors:
Blood composition depends on three factors:- Diet
- Cellular Metabolism
- Urine output
End of Reviewer