Final exam review
Chap 5- Palliative care and End of life issues
Palliative care- focus on pain relief and other symptoms assoiciated with severe illness.
Hospice care: care of pt who has less than 6 mos to live
Palliative care is provided in the hospital, outpt and community setting.
Domain
Structure and process of care
physical aspect of care
Psychological and psychiatric aspect of care
Social aspect of care including advanced care planning
Spiritual, religious and existential aspect of care
cultural aspect of care
Care of imminently dying
Ethical and legal aspect of care
Anyone can receive hospice who has less than 6 mos to live who decides not to pursue curative treatment
Who can contact hospice: pt, family, attending physician, any member of the team.
Stages of death
Early stage- acceptance that death is approaching
pt withdrawn, low appetite, pt does not experience thirst or hunger, begins to sleep
Middle stage- Weeks before death
decline in mental status; confuse and disoriented. sleep most of the time, decrease bp and temp. pulse irregular, RR; labored and rapid, skin color change and circulation is diminished. slow or ceased speaking.
Late stage- days or hour before date
brief surge of energy, symptoms worsen, coma, extremities cool and mottled, chyne strokes, , loss of gag reflex, congestion, death follows
User reflective listening to help family process dying experience.
Postmortem care:
body should be treated with care and respect
incorporate family and cultural practice
if there is autopsy; leave tubes, catheter in place
if no autopsy , remove tubes and clean the soiled area of the body
Decisional capacity- pt deemed if they meet
understand nature and consequences of proposed treatment
rationally evaluate the burden bennefits and risk of treatment
abitlity to communicate decision.
Moral distress: inability to do morally correct thing because of situational factor. Nurses cope by talking with other nurses, receive support from chaplains and managers.
Stress reducing strategies
perform postmortem care together
pausing for a moment of silence during the monthly staff meeting
sending family a bereavement card
Chapter 9- Acid base balance
PaO2: 80-95
SaO2: >95
pH: 7.35- 7.45
PaCO2: 45-35
HCO3: 22-26
Respiratory acidosis
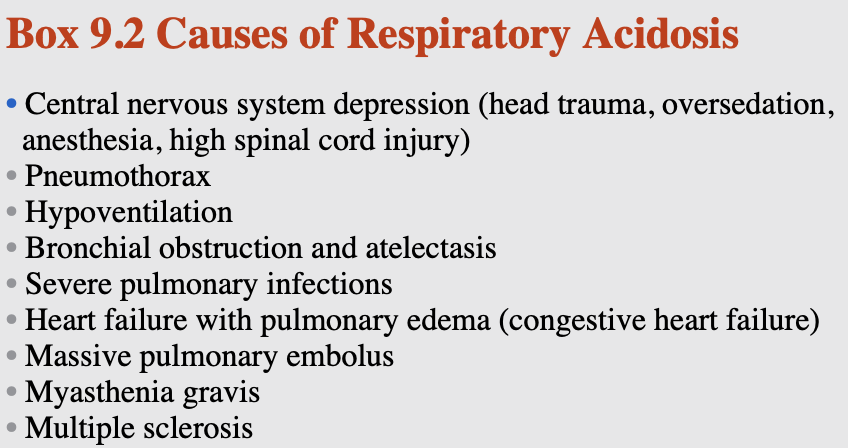
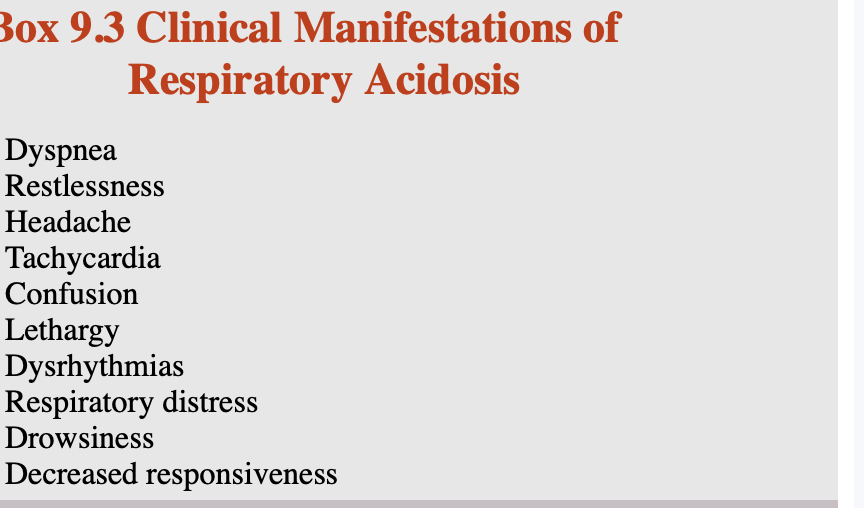 Nursing intervention for respiratory acidosis
Nursing intervention for respiratory acidosis
maintain airway
monitor ABGs
monitor VS esp; RR and depth
Administer O2
assist w/ intubation if necessary
monitor K+
administer sedatives cautiously
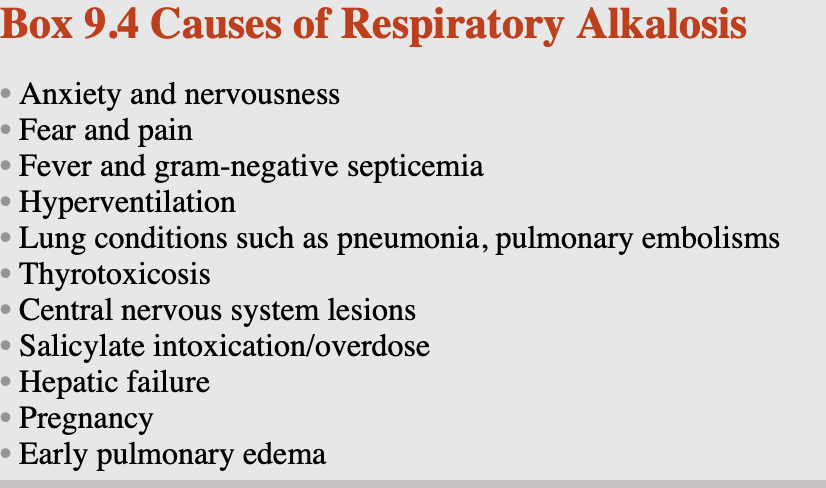
Respiratory Alkalosis
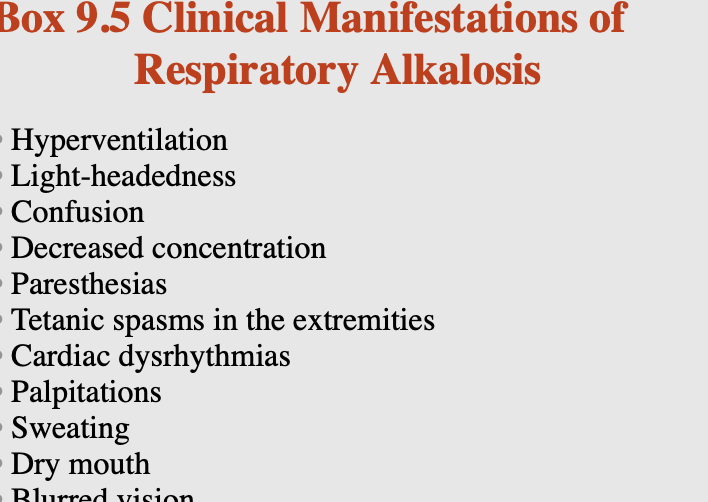 Treatment
Treatmentd/c causative agent
steps to reduce fever
eliminate source of sepsis
O2 therapy to reduce acute hypoxemia
sedative or anxiolytic to treat anxiey
diuretics to treat pulmonary edema
teach pt to breathe into paper bag or cupped hands- rebreathing and exhalation of CO2
for intubated pt;adjust mechanical vent as needed, decrease tidal volume or rate
Nursing intervention
encourage slow deep breathe
monitor VS
provide emotional support and reassure pt to reduce anxiety
Metablic Acidosis
Pt with less than pH: 7.1- bicarb is given IV
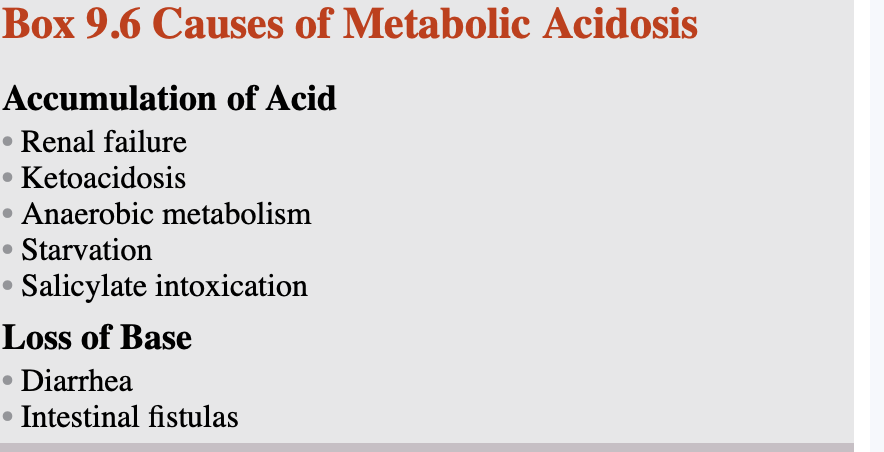
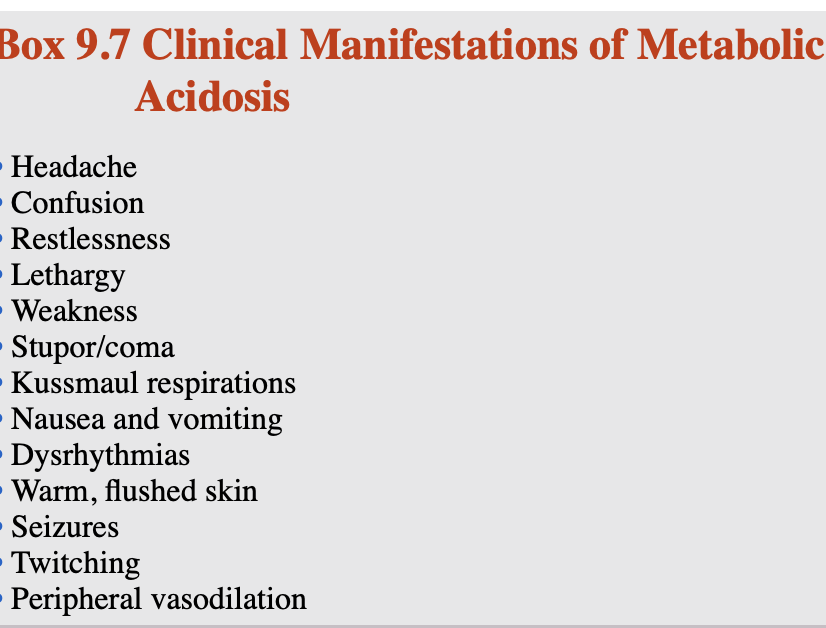 Nursing intervention
Nursing interventionfind underlying cause
monitor hemodynamic status through bp, plulse rate, respirartions and cardiac rhythms and peripheral vascular status
Metablolic Alkalosis- loss if acid; vomiting and nasogastric suctioning or renal excretion
Treatment
D/c K+ sparring diuretics and nasogastric
administer antiemtic for N/v
to increase renal excretion of bicarb; acetazolamide is administered if pt is not volume compromised or hypokalemic
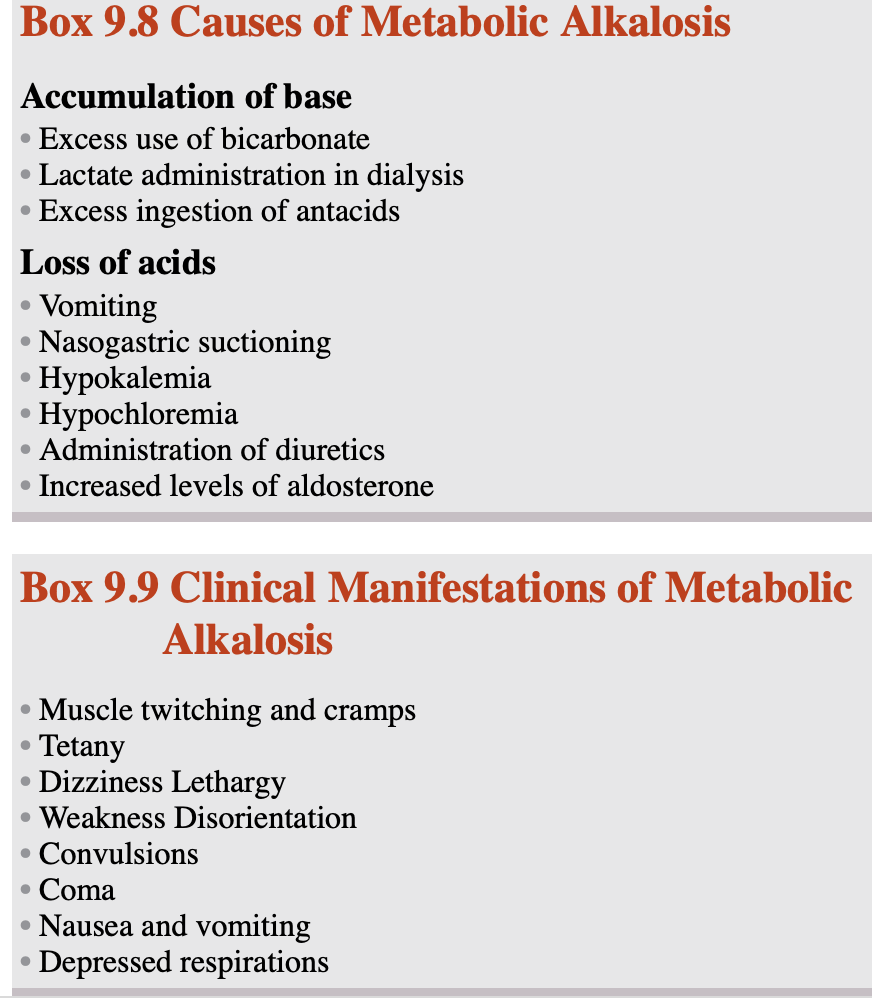
Nursing interventions
monitoring hemodynamic status through respirations, pulse rate, and cardiac rhythm
Assessing the patient’s level of consciousness.
Additional interventions include administering IV fluid
Chapter 10
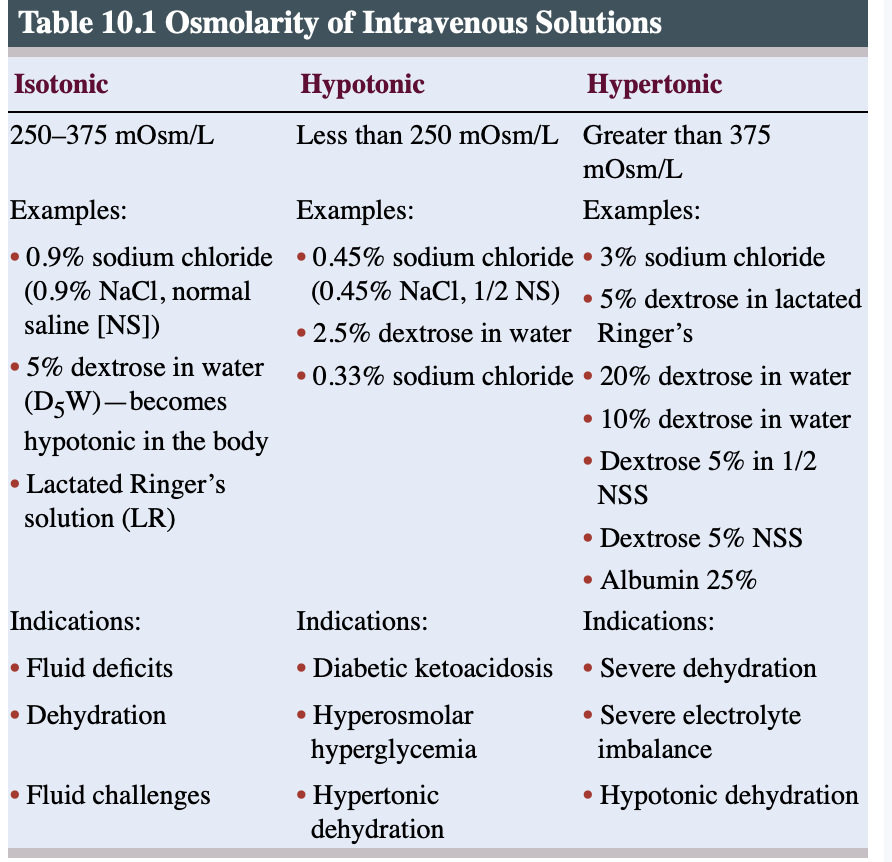
2 major IV solution: crystalloid and colloidal solutions
Crytalloid: electrolytes dissolved in water and include dextrose solution, sodium chloride solutions, balanced electrolyte solutions, and alkalizing and acidifying solutions.
Colloidial : larger molecules, usually protein or starch, suspended in fluid and are not a true solution. Colloidal solutions are frequently referred to as plasma volume expanders
used to maintain intravascular volume and prevent shock after major blood or fluid losses. Examples of colloidal solutions include albumin, dextran, and mannitol.
normal blood and body solution - 270-300 mOsm/L
Solutions can be isotonic, hypotonic, or hypertonic
Isotonic : osmolarity btw 250 and 375 mOsm/L
administered to dehydrated pt with intravascular volume deficit.
Hypotonic: used in the management of hypernatremia, hyperosmolar conditions, hypertonic dehydration, and diabetic ketoacidosis after initial sodium chloride replacement
fluid shift
Hypertonic: concentrations higher than plasma and cause fluid to move from the cells into the intravascular space.
Solutions with a concentration greater than 600 mOsm/L should be administered only via central venous access (CVA)
Nurses need to be attentive to continually assessing peripheral IV sites where antibiotics are infusing to assess for signs of warmth and tenderness that may indicate phlebitis.
aminoglycosides may be inactivated when given with penicillins or cephalosporins. Therefore, they must be given in separate sites, 1 hour apart.
Peripheral Venous Access
The most common type of peripheral IVAD is the short over-the-needle catheter
Therapies utilizing a short peripheral catheter should be expected to last less than a weeK
indications include hydration and administration of pain medications and some antibiotics
The steel-winged device (butterfly needle) is indicated only for short-term or single-dose therapy
Short-term peripheral IV access is established in the superficial veins of the upper extremity.
start therapy in the most distal available and appropriate vein and move upward with subsequent insertions
Areas of the vein containing a valve should also be avoided.
Veins in areas of flexion such as the wrist and antecubital fossa should be avoided if possible because it is more difficult to stabilize the IVAD in these areas.
Use of a vein in the arm on the side where a patient has had a mastectomy or has dialysis access is also contraindicated because venous return in the extremity may already be compromised.
Recommended veins for peripheral infusion therapy include the metacarpal, cephalic, basilic, and median veins.
Midline
Midline catheters inserted in a peripheral vein in the upper extremities with tips that terminate distal to the shoulder in either the basilic, cephalic, or brachial vein.
last between 1 and 4 weeks.
not used with vesicants, parentral nutrition or solution with pH less than 5 or osmorlarity greater than 600 mOsm/L.
Central Venous Access
IVAD terminates in the central vasculature at the level of the superior vena cava or the inferior vena cava.
comes in single or multiple lumen
the lumens are separate, incompatible solutions can be infused using the different ports attached to each of the lumens.
flushing is also used to maintain the patency of the individual lumens if fluids are not being continuously administered.
Types of IVADs used to obtain central venous access include nontunneled percutaneous central catheters, tunneled catheters, implanted ports, and peripherally inserted central catheters (PICCs).
Nontunneled percutaneous central catheters are usually inserted in either the jugular or subclavian veins using venipuncture, and the tip of the catheter is advanced into the superior vena cava.
Implanted ports (Mediports) are also used for long-term therapy
Peripherally inserted central catheters (PICCs) are CVADs that are inserted into a peripheral vein and advanced into the central vasculature.
electrocardiogram (ECG) guidance is more reliable and of lower cost compared with ultrasound guidance.
The veins used for PICC insertion are usually the larger veins in the upper extremities
Complication
Phlebitis, inflammation of the vein, is characterized by pain and erythema along the vein and is graded using a standardized scale according to signs, symptoms, and severity.
Peripheral sites that show signs of phlebitis should be removed and restarted in another location because phlebitis can progress to more serious conditions, including thrombus formation, cellulitis, and sepsis.
The antecubital fossa site has been shown to have the lowest phlebitis rates, whereas hand veins have a high risk of phlebitis.
Aloe Vera to Prevent and Treat Infusion Phlebitis
Assessed at regular intervals for phlebitis
When the solution or medication that infiltrates is a vesicant (able to cause blisters), an extravasation (leakage of IV fluid into subcutaneous tissue) has occurred.
Medications that are classified as vesicants include specific antineoplastic agents, antibiotics, and vasoactive medications.
Clinical manifestations of infiltration include blanched skin, skin cool to the touch, edema, unexpected pain or burning at the insertion site or along the path of the vein, and leaking of fluid from the insertion site
In the case of an extravasation, the infusion needs to be stopped immediately, and corrective action needs to be taken to minimize damage to the tissue.
Prevention of airbolism
proper Trendelenburg positioning during CVC insertion (10–30 degrees)
Avoiding CVC insertion during inspiration.
Correcting hypovolemia prior to CVC insertion.
Ensuring all IV connections are intact and secure
Ensuring all lumens are capped and/or clamped
Using Luer-locking connections, frequently checking the connections, and clamping catheters and injection sites when not in use
Priming
flush all air out
removal should be performed with the patient in a supine position.
Prior to removal, the patient should be instructed to perform a Valsalva’s maneuver or exhale during the removal to prevent the introduction of air into the line.
The catheter should be removed slowly, and a sterile occlusive dressing should be placed over the insertion site immediately and left in place for 24 hours.
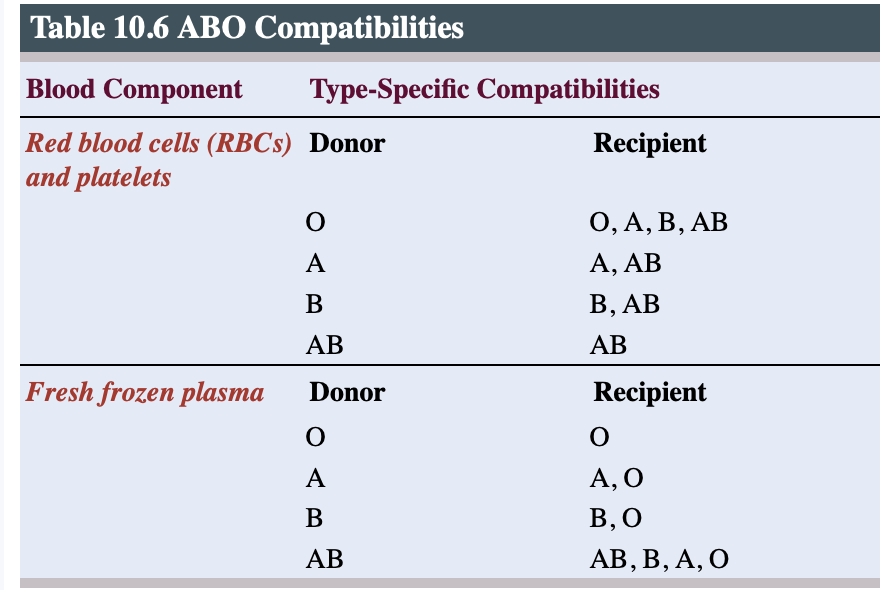
Administration of blood products
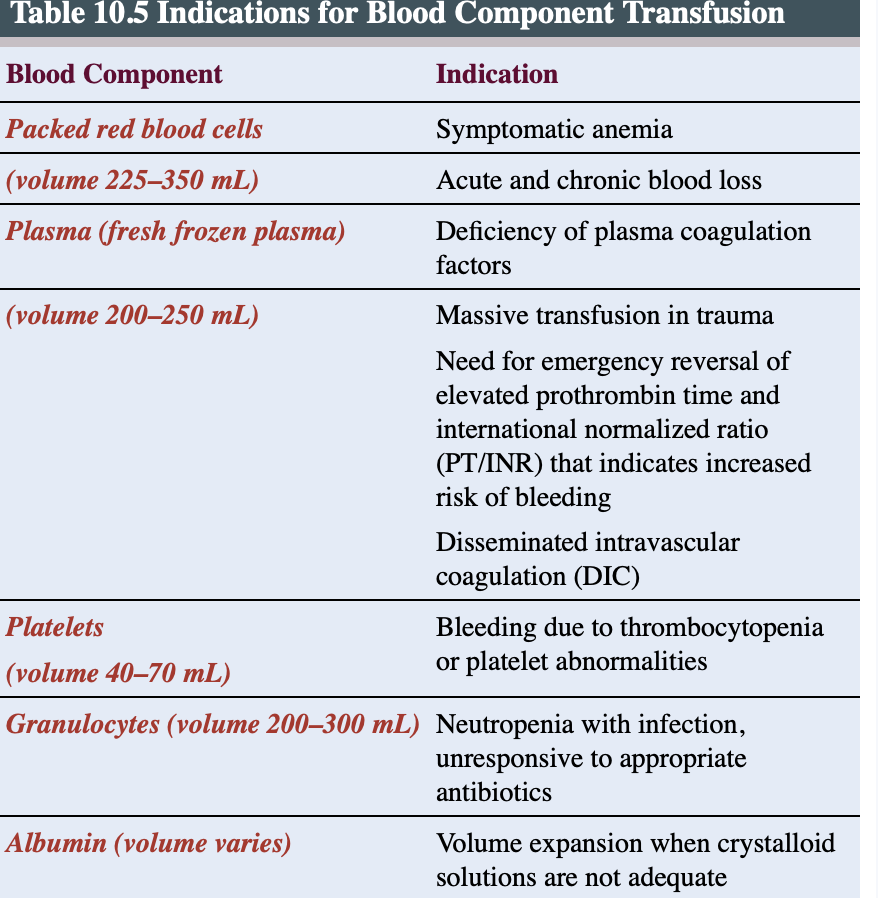
 Close observation is required to detect any reaction the patient may have to the blood product, especially during the first 15 minutes when reactions are most likely to occur.
Close observation is required to detect any reaction the patient may have to the blood product, especially during the first 15 minutes when reactions are most likely to occur.Assessments should continue at least every hour for the duration of the transfusion and should include respiratory status; vital sign status; and any complaints of discomfort, dyspnea, or itching.
0.9% sodium chloride is recommended because it does not cause fluids to move into or out of the transfused RBCs.
The gauge of the IVAD used for transfusion needs to be large enough; 18- to 20-gauge catheter is recommended for the infusion of packed RBCs in the adult population to prevent RBC lysis.
A single unit of packed RBCs has a volume between 225 and 300 mL and is usually infused over 1 1/2 to 2 hours but no longer than 4 hours.
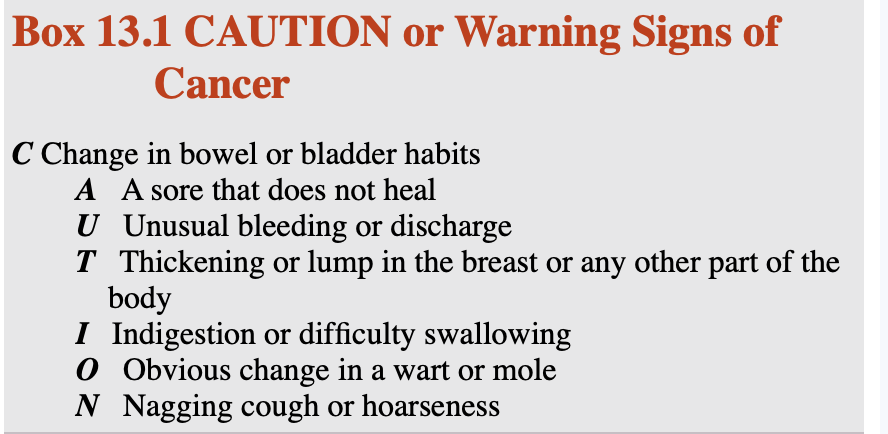
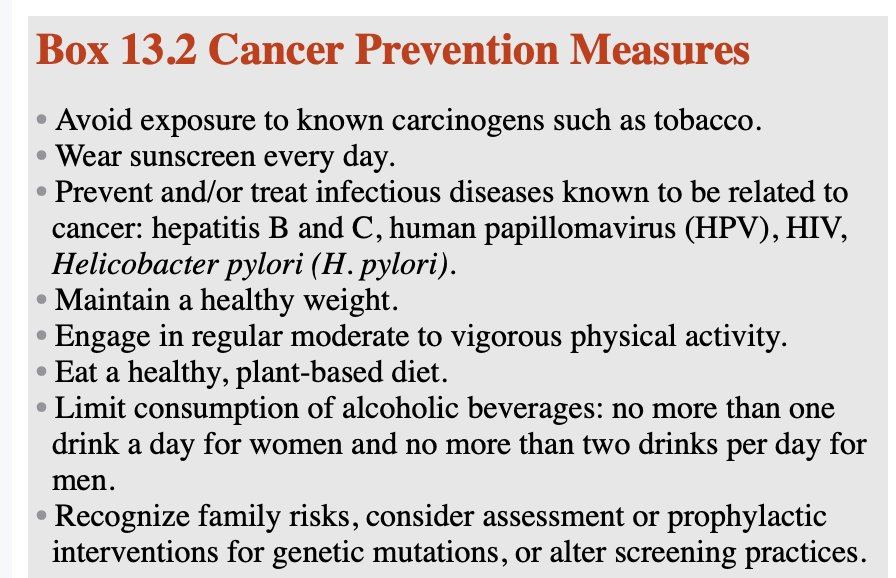
Chap 13-Overview of cancer
2nd leading cause of death
most common: lung, breast, colorectal, prostate, skin and stomach cancer.
women most likely to develop; breast, cervical, and colerectal
men most likely to develop lung, prostate, or colorectal cancer.
Etiology of cancer: Hepatitis, HPV, and carcinogen.
Risk factors: carcinogen: ionizing radiation, benzene, HPV, sun exposure, and tobacco.
Environmental, hormonal, and lifestyle factors; infectious disease; medications; immune status; and nutritional factors are all believed to influence the development of cancer.
Nonmodifiable cancer risk factors, or factors that the individual cannot alter to decrease the risk for cancer, include age and genetic predisposition.
A modifiable risk factor for cancer is lifestyle. Specifically, a sedentary lifestyle poor diet, and/or smoking
Staging
The basic components of solid malignancy staging are tumor size (T), number of lymph nodes involved (N), and presence of metastases (M).
A small tumor without obvious spread outside the organ is termed stage I
invasion of deeper tissues or involvement of local lymph nodes is stage II
large or locally invasive tumors are stage III
cancers that have metastasized are considered stage IV.
 Biopsy is the primary method of obtaining samples required to determine the presence of malignancy.
Biopsy is the primary method of obtaining samples required to determine the presence of malignancy.
Chapter 15
Type of surgical procedure
Emergency surgery: done immediately to save pt life, limb.
Urgent surgery: done in 24-48hrs to prevent death or permanent injury
Elective surgery: planed within pt and surgeon time
Ambulatory output surgery: pt can be discharged same day
Exploratory, dx surgery: done for dx
Ablative surgery: done to remove tissue.
Palliative surgery: done to decrease pain
Reconstructive surgery: done to restore function or a defect in an area of the body.
Cosmetic surgery: done to revise an area or structure of the body
Minimally invasive surge: small openings in the skin, using instruments through with the surgeon can visualize the area such as a laparoscope.
The operative experience is broken up into three phases: preoperative, intraoperative, and postoperative.
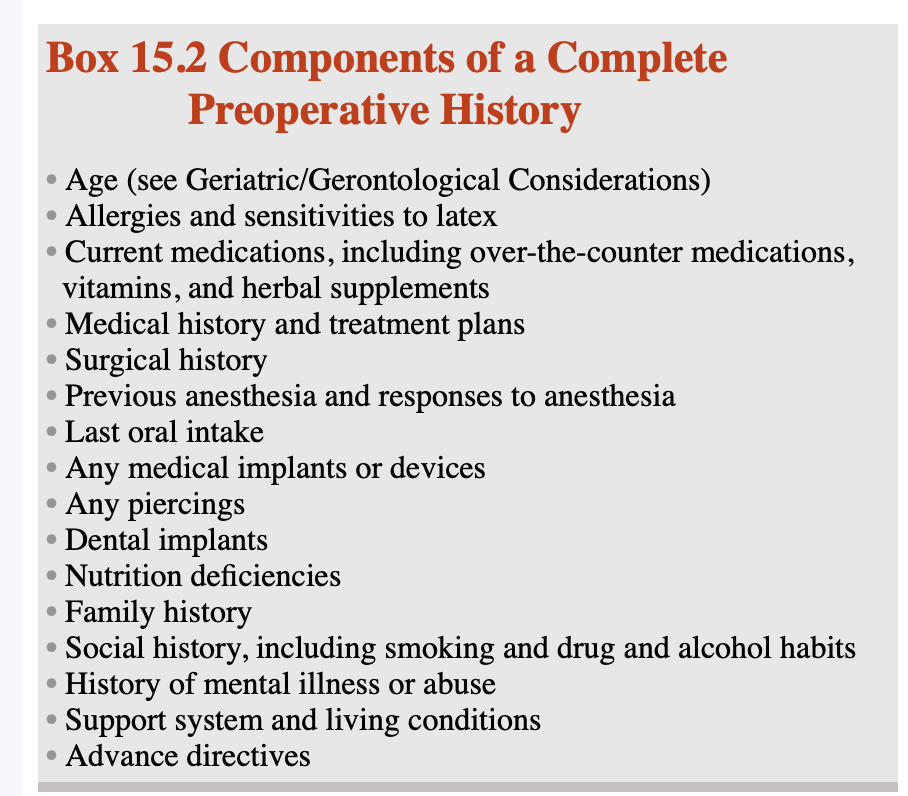
Preoperative phase:
The preoperative phase is a patient’s first impression of the surgical setting.
commences when the decision for surgery is made and ends when the patient is transferred to the surgical suite.
nurse takes in the role of an educator, advocator, admittance nurse
main priority; preoperative checklist
full med hx; prescription, OTC, herbal and other alternative therapies
assess pt health status
collect info and paperwork for intaoperative and postoperative care.
complete abx, thrombolitic deterrent.
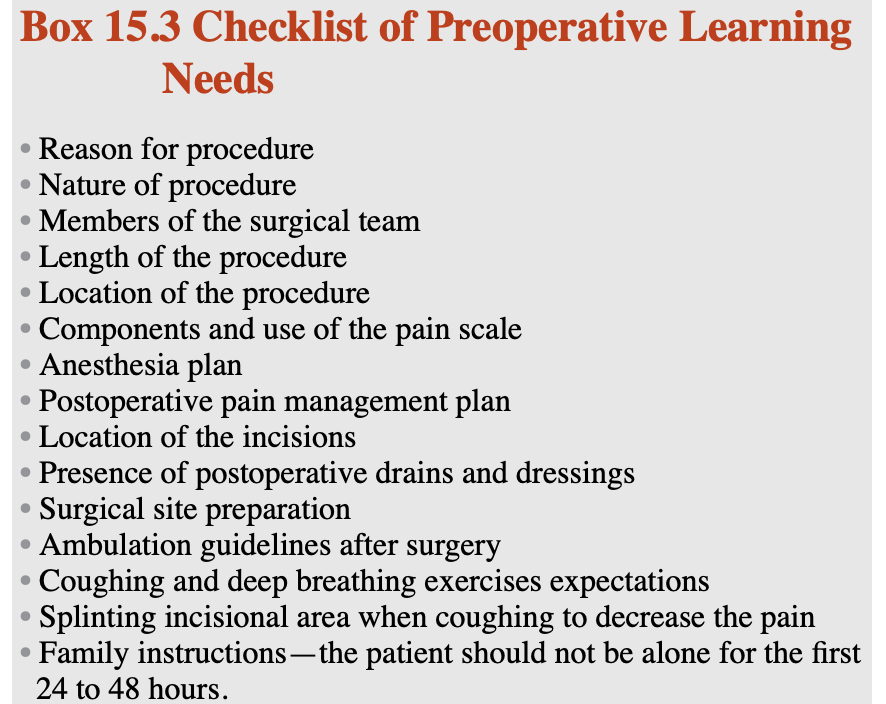
pt education about surgical process
verify pt and witness signed informed consent
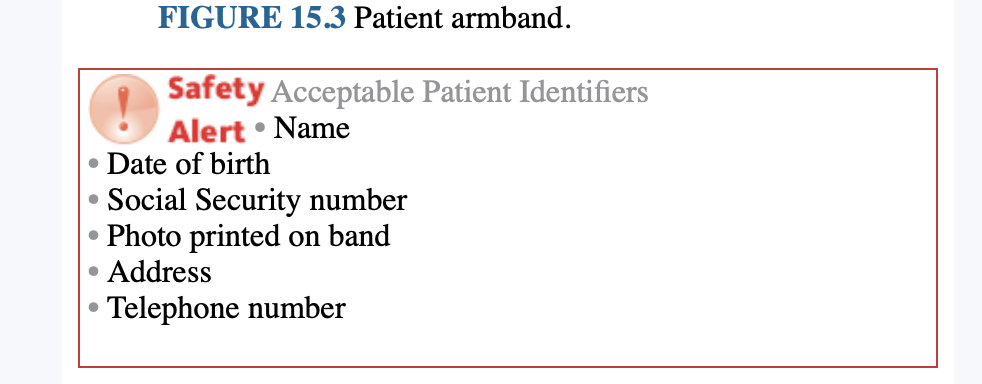
Time out- collected prior to surgery
pt verifies
all info on identification band is correct
name of surgeon
procedure that will be completed by the surgeon
correct side of the body.
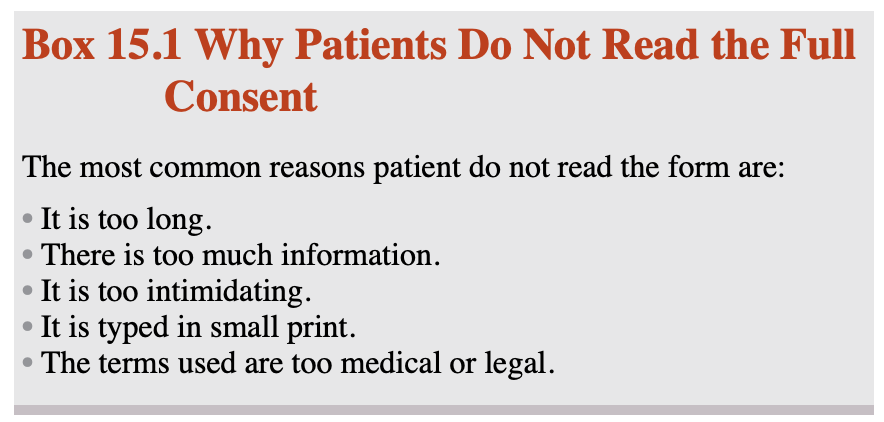
Informed consent
not job of the nurse to receive informed consent, responsibility of the nurse to ensure all information is needed to make an informed consent
Component
consent of procedure
name of surgery, type and reason for surgey
name of surgeon
reason procedure will benefit pt
alternative options
outcome if surgery is not performed
Inability to consent
In situations where the patient is impaired, a medical power of attorney may be established for consent purposes.
Patients who cannot physically sign but can make their own care decisions may sign with an “x.
needs to be witnessed by two people instead of just one as normally.
If the patient speaks another language or is deaf, a hospital interpreter may be use.
Surgical consent for minor
must be signed by legal guardian, if child is old enough, procedure is still explained
in emergency
a verbal consent is acceptable.
If the patient is incapable of giving consent, two providers document the need for surgery.
This is acceptable only if the patient’s medical power of attorney or next of kin is unreachable
or the surgery is emergent and the patient has no support presen
for sterilization- consent must be collected 6 wks prior
Advance directive: defines a patient’s wishes should he or she be deemed incompetent to express his or her wishes in a medical emergency.
the patient may name a durable medical power of attorney, usually a spouse or adult child.
a living will defines care in the case of cardiac or respiratory failure or when the likelihood of recovery to a quality level of functioning is deemed unlikely.
in the event of a cardiac arrest. The phrases “do not intubate,” DNI, or “do not resuscitate,” DNR, are recorded in the patient’s chart.
 NPO for infant and children
NPO for infant and children
No solid food is allowed for 8 hours before surgery.
Infant formula can be given up to 6 hours before surgery.
Breast milk can be given up to 4 hours before surgery.
Clear liquids can be given up to 2 hours before surgery.
Do not ask pt psychosocial questions, such as questions about abuse at home and gynecological and mental illness, with other family or support persons available.
Preoperative lab assessment
ABO and RH
CBC; liver enzymes, albumin, electrolytes, blood urea nitrogen, and creatinine
Coagulation studies
Urinalysis; glucose, blood pprotein and specific gravity and presense of ketones
Pt teaching preoperative
help decrease anxiety
pt family should be included; how long procedure, how long pt will be in the PACU, and how soon family will receive updates on pt status,and see pt.
discharge care may be covered @ this time too
nurse address family concern, and guide family to appropraite waiting area
Chapter 16-Priorities of Intraoperative pt
Minor procedures such as oral surgeries and dilations and curettage- local anesthesia; minimal post-anesthesia recovery
Regional anesthesia: keep pt head flat after spinal anesthesia to avoid headache.
Major procedures are longer, performed under general anesthesia and require overnight stays in the hospital, sometimes in the ICU setting. Cardiac procedures, neurological procedures, or thoracic procedures typically fall into this category.
The patient receiving a general anesthetic that includes the administration of a muscle relaxant requires ventilatory support in the form of an endotracheal tube (ETT).
General anesthetics can also be administered without the use of muscle relaxants. In such instances the airway is frequently supported with supraglottic airways, such as a laryngeal mask airway (LMA), oral airway, or nasal airway.
Sterile Team Members
The surgeon
Surgical assistants: NP, RN first assistant, surgical first assistant, physician assistant.
The scrub nurse or surgical technologist
Nonsterile team members
• The anesthesia provider
• The circulating RN
• Unlicensed assistive personnel
• The OR director/coordinator/manager
Role of the circulatory nurse
Initial assessment of the patient in the preoperative area. establish a therapeutic relationship with the patient, attempting to calm fears and establish trust.
Initial assessment upon admission to the OR
Assisting the anesthesia provider with positioning, monitor placement, line placement, and patient monitoring
Assisting the surgeon and scrub nurse/technologist with donning of sterile gowns, gloves, and other protective gear
Anticipating the need for equipment, instruments, and medications
Assisting the scrub nurse or technician by opening packages of sterile supplies necessary for the procedure
Ensuring samples are appropriately labeled and sent to the laboratory for analysis
Counting the number of sponges, needles, instruments, and other miscellaneous supplies used during the operation to prevent accidental retention or loss of an item in the surgical wound
Documenting information pertinent to the surgery and the surgical patient
Positioning
Supine; natural position for body @ rest. used for procedures in the anterior body surface such as abdominal, abdominalthoracic, vascular, orthopedic, head/necck and ophthalmic operations. less than 90’ arm extension
Trendelenburg; pt supine but modified head tilted down 35-45 degrees; used for lower abdomen and pelvic procedure.
Reverse Trendelenburg; bed is tilted. with the head is higher than than feet. facilitate blood flow to surgical area, and aids with breathing.
Fowler: pt is postioned with HOB 35-45 and foot lowered slightly allowing flexing of pt knees. Used for craial procedures
Prone ; ventral recumbent: pt is facedown
Jackknife position: modified prone position
Lateral: used for thoracic, renal and orthopedic hip procedure
Pt @ risk for positioning complication
getriatric pt with thin skin an d impaired circlation
peds with immature system
extremely thin pt who are malnourished, anemic or hypovolemic
obese pt
paralyzed pt
DM pt
pt with prothetic and arthritic joints
pt with edema and circulatory limitations
Pt with medical conditions such as cancer that have altered immune, cardia an d respiratory system,
pt with infections
pt with existing or previous trauma
Chapter 17- priorities for postoperative patient
The goal of care in the PACU is to safely allow the patient who has had anesthesia/sedation to awaken and resume normal bodily functions while controlling/minimizing pain and preventing complications of surgery and anesthesia.
Three levels of PACU care: phase I, phase II, and phase III.
Phase I: PACU or ICU- intensive, close monitoring of all vital signs with continuous electrocardiogram monitoring.
There is a focus on cardiac, respiratory, and neurological functions, surgical-site monitoring, and pain and temperature control.
The goals is to stabilize the patient’s vital signs, allow the patient to awaken from anesthesia, and achieve adequate pain control.
D/c criteria
An awake patient with a stable airway
Adequate oxygen saturation
Stable vital signs
Phase II: must meet criteria for phase I. The focus of nursing care is on preparing the patient to be discharged to an extended-care environment or home.
Phase II: provide care to pt on postoperative care
 Post anesthesia care unit
Post anesthesia care unitInpt PACU: for patients recovering from major or minor surgical procedures on a continuum from low to high risk of complications.
Example: radical retropubic prostatectomy, lung lobectomy, ileostomy reversal, nephrectomy, exploratory laparotomy, and open reduction and internal fixation of fracture.
Nurse 1:! or 1:2 or 1:3 length of stay is 1-2 hr.
ICU: for critically ill patients who require extensive and complex monitoring because of the high risk of complications
Example: patients undergoing transplant surgery, craniotomy, and coronary artery bypass procedures and trauma patients undergoing multiple procedures.
Outpt Post anesthesia care unit: pt going home after the procedure
example: orthopedic arthroscopic procedures, cholecystectomies, mastectomy, diagnostic procedures, dental procedures, some plastic surgery, and ophthalmological procedures.