DP2 Biology - 6.6 & D5 (SL): Hormones, Homeostasis and Reproduction & 11.4 Sexual Reproduction (HL)
IB SKILLS
6.6 & D5 (SL): Hormones, Homeostasis and Reproduction
Homeostasis: the regulation of the internal environment between limits. Including regulation of pH in blood, metabolism, circadian rhythms, CO2 concentration, blood glucose concentration, body temperature, and osmoregulation
it is achieved through the use of brain, nerves and hormones.
Hormone - chemical signal produced in one part of the one organism that travels through the circulatory system to reach its target.
Hormones are released when a stimulus is received, and when reaching their target they cause a response.
The Endocrine system is a collection of specific organs called glands that produce/secrete hormones directly into the blood that regulate the body.
Organisms have a way in ensuring that the response can be turned OFF once desired homeostatic levels have been reached through the use of negative feedback mechanisms.
Example of Negative Feedback with ADH
The release of antidiuretic hormone (ADH) is triggered by a increase in concentration of solute in blood and lower blood pressure as a result of dehydration (when a person doesn’t drink enough water). This will trigger the release of ADH form the pituitary gland.
this hormone will stimulate osmoregulation allowing the reabsorption of water in the collective ducts to dilute the solutes in the blood and increase blood pressure (AKA homeostasis)
As homeostasis is brought onto the blood, the trigger signal will decrease and thus, subsequently, inhibit the release of ADH
this is an example of negative feedback
The pituitary gland
Anterior pituitary system:
secretes & synthesizes hormones that control growth, reproduction, and homeostasis
Posterior pituitary system:
stores & releases hormones that where once made in the hypothalamus above it.
Hypothalamus - part located in the brain that links the nervous system and endocrine system by stimulating the pituitary gland under certain conditions.
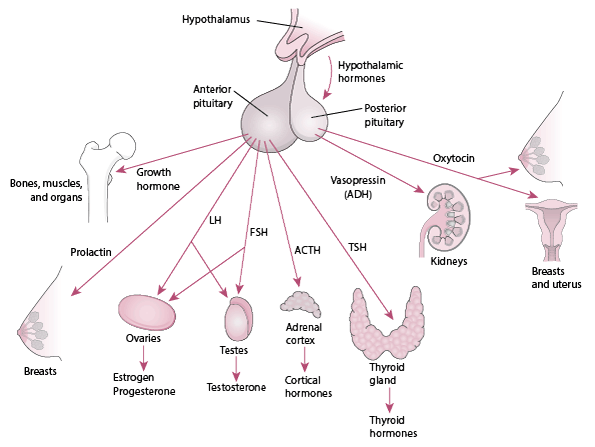 Examples of pituitary hormones in relation to one area of life:
Examples of pituitary hormones in relation to one area of life:
Growth: growth hormone
Developmental changes: follicle-stimulating hormone (FSH)
Reproduction: LH
Homeostasis: TSH (signals the thyroid gland to release of thyroxin which helps control body temperature)
Why might some athletes inject themselves growth hormones to improve performance?
Growth hormone stimulates the release of insulin-like growth factor (IGF) in the body, which in turn stimulates bone and cartilage growth. One of the side effects of IGF is muscle growth, so this hormone has been used as a performance-enhancing drug. While it does result in an increase in muscle mass, there is no conclusive evidence that it results in increased strength. In fact, research shows that the benefits are negligible compared to the risks of injecting growth hormone
Types of hormones released into bloodstream:
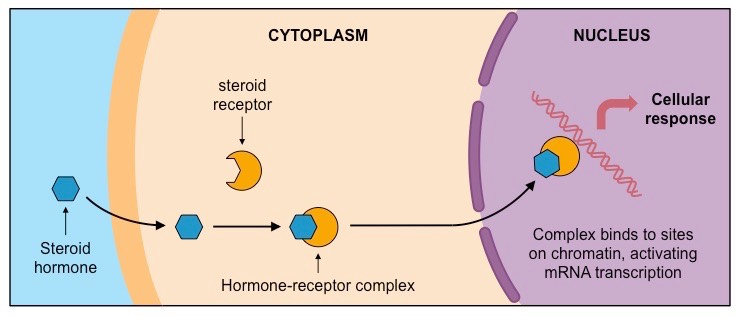
Steroid Hormone:
lipid soluble meaning they can directly pass through the cell membrane without the aid of any transport protein.
bind to a receptor in the cytoplasm forming a receptor-hormone complex that acts directly on the DNA to activate TRANSCRIPTION
examples: estrogen, testosterone and progesterone
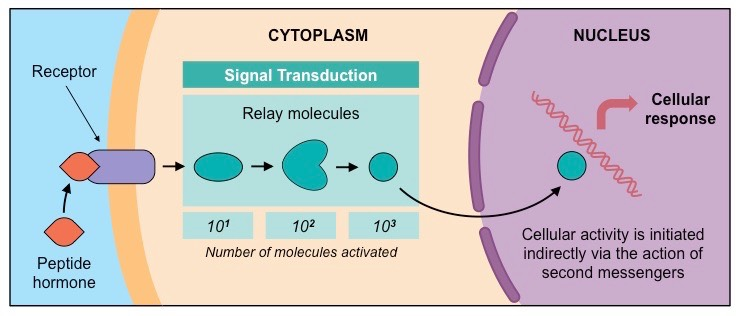
Peptide Hormones:
Hydrophylic and lipophobic (fat-hating) meaning they cannot freely cross the plasma membrane
bind to a receptor on the SURFACE of the dell activating a second messenger molecule in the cell which then can activate enzymes.
examples: Glucagon, Insulin, Thyrocine, Leptin & Melatonin
Topic 6.6:
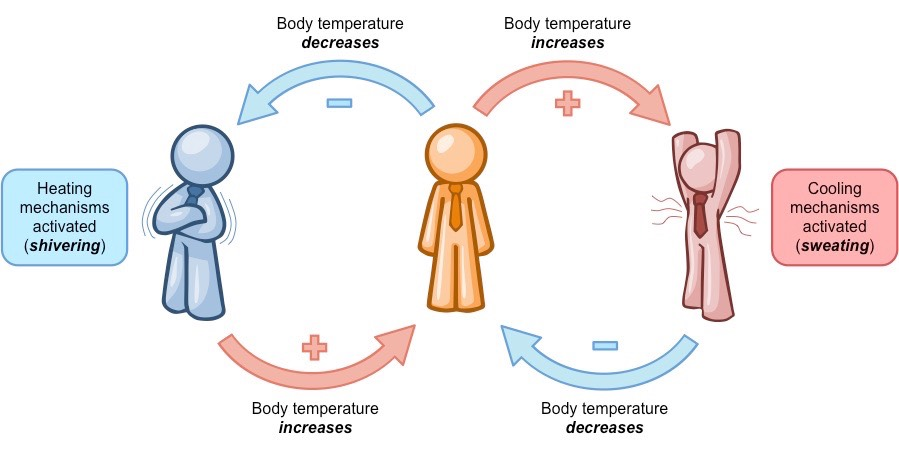
What is Negative feedback?
it’s when the result of a process influences the operation of the process itself in such a way as to reduce changes OR the SLOWING of a particular process when its product begins to accumulate.
Negative feedback involves a response that is the reverse of the change detected (it functions to reduce the change)
when change is detected by a receptor, an effector is activated to induce an opposite effect – this promotes equilibrium
Examples of processes that utilise negative feedback loops include homeostatic systems, such as:
Thermoregulation (if body temperature changes, mechanisms are induced to restore normal levels)
Blood sugar regulation (insulin lowers blood glucose when levels are high ; glucagon raises blood glucose when levels are low)
Osmoregulation (ADH is secreted to retain water when dehydrated and its release is inhibited when the body is hydrated)
What is Positive feedback?
The enhancement or amplification of an effect by its own influence on the process that gives rise to it.
A change is detected by a receptor and an effector is activated to induce the same effect – this promotes further change
Positive feedback loops will continue to amplify the initial change until the stimulus is removed
Examples of processes that utilize positive feedback loops include:
Childbirth – stretching of uterine walls cause contractions that further stretch the walls (this continues until birthing occurs)
Ovulation – the dominant follicle releases estrogen which stimulates LH and FSH release to promote further follicular growth
Hormones:
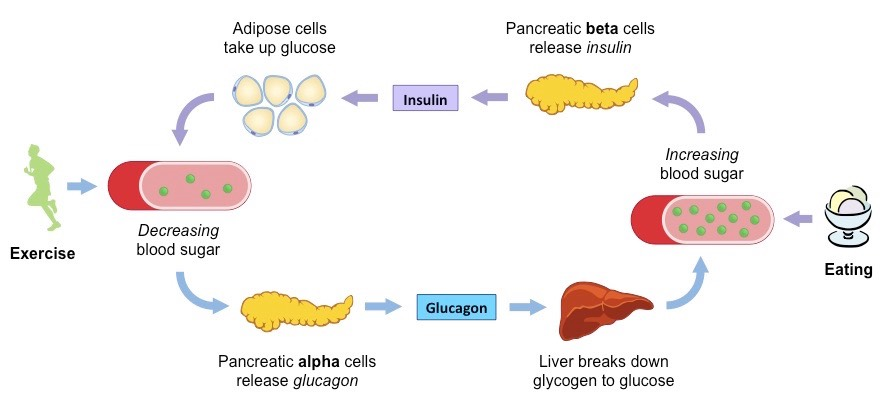
Insuline:
Location of secretion: Beta (β) cells in pancreas
Trigger: High glucose levels (e.g. after eating)
Location of target cells: liver
Function: decrease blood glucose concentration
How?
stimulating glycogen synthesis in the liver, promoting glucose uptake by the liver and adipose tissue
increasing the rate of glucose breakdown (by increasing cell respiration rates)
Glucagon:
Location of secretion: Alpha (α) cells of the pancreas
Trigger: low glucose levels (e.g. after exercise)
Location of target cells: liver
Function: increase blood glucose concentration
How?
stimulating glycogen breakdown in the liver (glycogenolysis), promoting glucose release by the liver and adipose tissue
decreasing the rate of glucose breakdown (by reducing cell respiration rates)
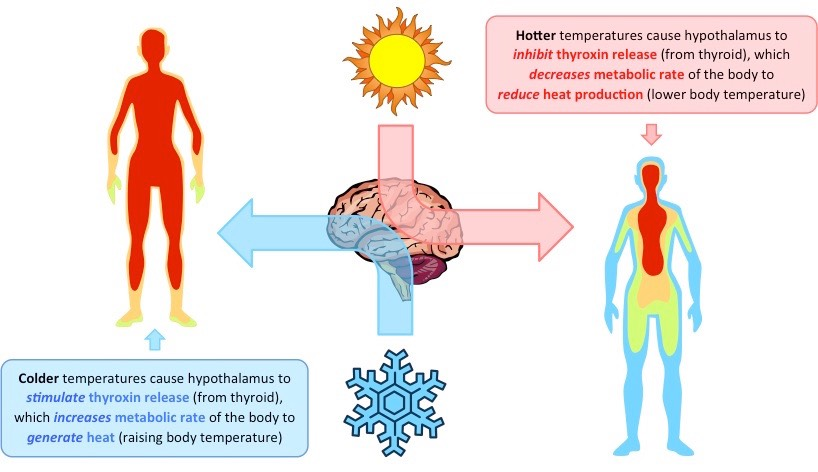
Thyroxin:
Location of secretion: thyroid gland
Trigger: decrease in body temperature
Location of target cells: nearly every tissue in the body
Function: increase the basal metabolic rate (amount of energy the body uses at rest)
A consequence of increasing metabolic activity is the production of heat – hence thyroxin helps to control body temperature
Thyroxin is released in response to a decrease in body temperature in order to stimulate heat production
What are the effects of thyroxin deficiency (hypothyroidism)?
cells grow listless
metabolism slows
changes how your body processes fat
can lead to high cholesterol & atherosclerosis
lead to heart problems line angina & heart attack
symptoms experienced might be sluggishness, sensitivity to cold, swollen joints and feeling low
Leptin:
Location of secretion: adipose cells
Trigger: Fat cells tell the brain that the body has enough energy stored to engage in normal, metabolic processes.
Location of target cells: hypothalamus receptors
Function: regulates fat stores within the body by suppressing appetite
When leptin levels are at or above a certain threshold (genetically set) your brain senses that you have energy sufficiency, which means you can burn energy at a normal rate, eat food at a normal amount, engage in exercise at a normal rate.
Because leptin suppresses appetite, it was considered as a form of treatment for individuals with clinical obesity
Theoretically, leptin injections would reduce hunger and limit food intake in obese individuals, leading to weight loss
Mice Experiment
Mice with and without the Leptin gene. When the gene is not present, no transcription can happen, therefore no hormone is translated. There is no signal to regulate the system.
Testing for this can potentially aid in treating clinical obesity.
Leptin trials were initially conducted by surgically fusing the blood circulation of obese and healthy mice (parabiosis)
This experiment was conducted using mice that were either obese due to a leptin gene mutation or a defective leptin receptor
When the obese mouse with no leptin was parabiotically fused to a healthy mouse:
Leptin in the blood of the healthy mouse was transferred to the obese mouse
The obese mouse responded to the leptin and began to lose weight, demonstrating the potential viability of leptin treatment
However, when the obese mouse with a defective leptin receptor was parabiotically fused to a healthy mouse:
Leptin was transferred to the healthy mouse (the obese mouse overproduced leptin to compensate for low receptor sensitivity)
The obese mouse remained obese as its body could not respond to leptin
The healthy mouse became emaciated due to the abnormally high levels of leptin transferred into its bloodstream
Human Experience:
Most humans have naturally high levels of leptin in the bloodstream
When linked to leptin activity, most cases of obesity are caused by an unresponsiveness to leptin and not a leptin deficiency
Hence, in clinical trials, very few participants experienced significant weight loss in response to leptin injections
However, many patients did experience adverse side effects from leptin injections, including skin irritations
For these reasons, leptin treatments are not considered to be an effective way of controlling obesity
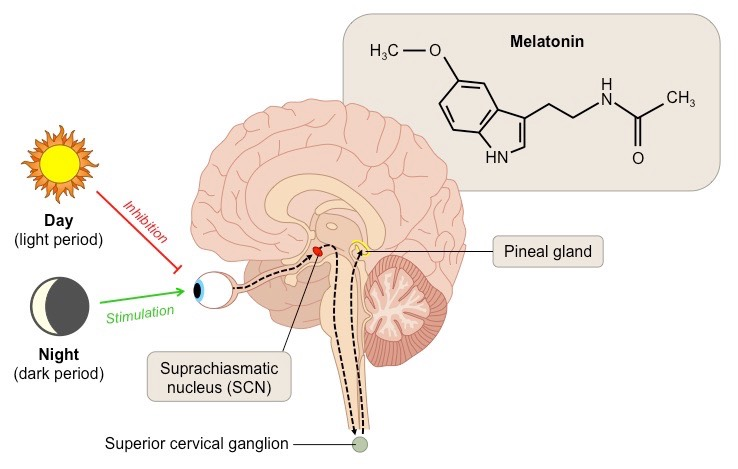
Melatonin:
Location of secretion: pineal gland
Trigger: periods of darkness
Light exposure to the retina is relayed via the suprachiasmatic nucleus (in the hypothalamus) and inhibits melatonin secretion
Melatonin is therefore secreted in response to periods of darkness, resulting in higher concentrations at night
Location of target cells: central and peripheral sections of the brain
Function: synchronizing circadian rhythms and regulates the body's sleep schedule
How can melatonin aid in jet lag?
Jet lag is a physiological condition resulting from a change to the body’s normal circadian rhythm
This alteration is caused by the body’s inability to rapidly adjust to a new time zone following extended air travel ('jet' lag)
The pineal gland continues to secrete melatonin according to the old time zone so that the sleep schedule is not synchronised to the new timezone
As a result of these sleep disturbances, individuals suffering from jet lag will often experience symptoms associated with fatigueSymptoms of jet lag include headaches, lethargy, increased irritability and reduced cognitive function
Jet lag should only last a few days and symptoms should resolve as the body resynchronises its circadian rhythm
Some health professionals recommend taking melatonin near the sleep time of the new time zone to help recalibrate the bodyBy artificially increasing melatonin levels at the new night time, the body can respond quicker to the new day-night schedule
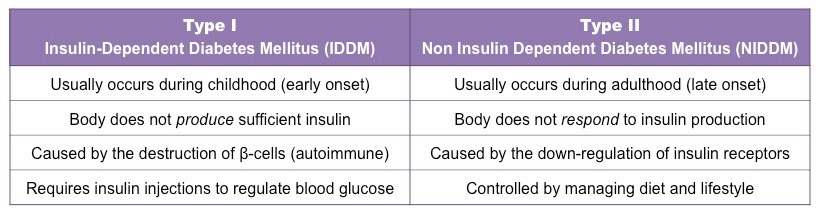
Diabetes:
Diabetes is a metabolic disorder that results from a high blood glucose concentration over a prolonged period
It is caused by the body either not producing insulin (Type I) or failing to respond to insulin production (Type II)
It is treated with either insulin injections (Type I only) or by carefully monitoring and controlling dietary intake (Type II)
Reproduction:
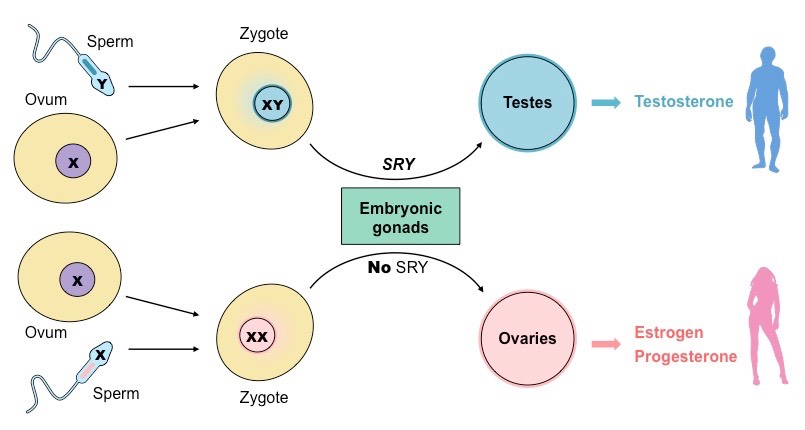
What is the SRY gene in sex determination of embryos?
SRY - Sex Determining Region Y
meaning this gene is only expressed when Y chromosome is present (aka XY)
when expressed, the zygote with experience the testicular development of the undifferentiated embryonic glands
the absence of the gene (aka those with XX chromosomes) the embryonic gonads will develop into ovaries
this absence of it allows the default (female state) to develop
Role of 3 hormones in de fetal and secondary sex characteristics development:
Testosterone:
testosterone is secreted by the testes
Fetal development - development of male genitalia (the penis and the scrotum)
Secondary sex characteristics development (during puberty) - body hair, muscle mass, deepening of voice, etc…
testosterone also aids in sperm production following the onset of puberty
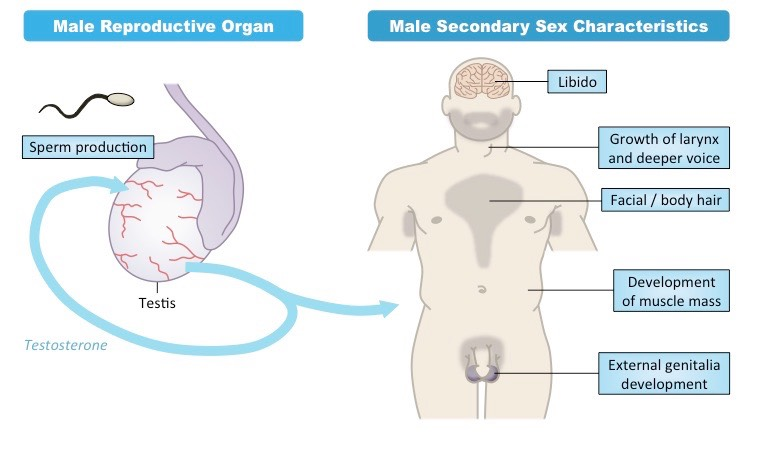
Estrogen & Progesterone:
estrogen and progesterone are secreted by the mother’s ovaries and then the placenta, it is not until full development of female reproductive organs that the hormones are secreted by the individual’s ovaries
Fetal development - reproductive organs (vagina, uterus, fallopian tubes, clitoris, cervix) & ability to produce life
Secondary sex characteristics development (during puberty) - body hair and breast development
following puberty both hormones play a role in the menstrual cycle (more on this later)
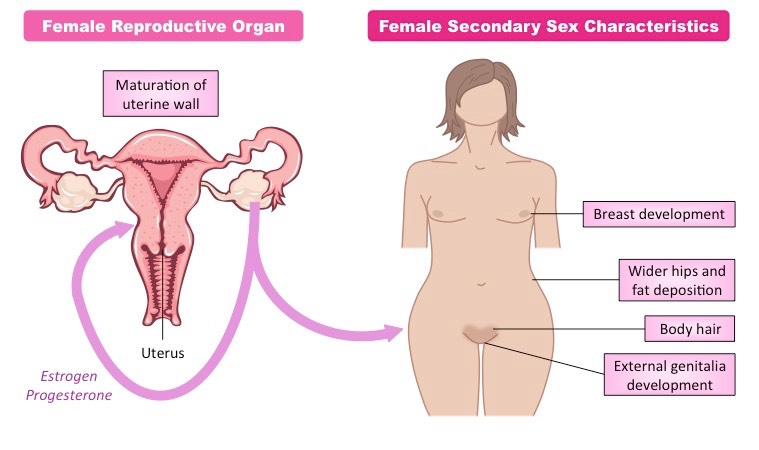
Male reproductive system:
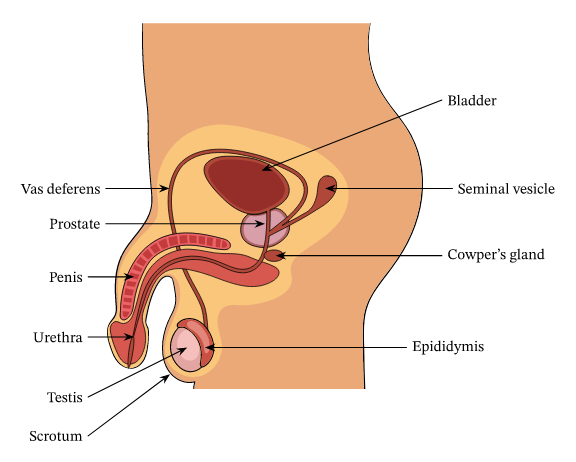
Functions of the organs:
Testis - responsible for sperm production and secretion of testosterone
Epididymis - location where sperm matures and develops (until fully developed & concentrated)
Vas Deferens - long tube which conducts sperm form testes to the prostrated glans (conects to the urethra) during ejaculation
Seminal Vesicle - produces fluid that provides nutrients and mucous that protects sperm
Prostate Gland - Secretes alkaline fluid (base solution) that neutralise vaginal acids (in other words protects sperm form the acid conditions of the vagina or the sperm would “die” form the acid conditions this maintaining their viability)
Urethra - conducts sperm form prostrate gland to outside the body via the penis (also used to convey urine)
From school slide show:
Structure | Function |
|---|---|
Testicle | Location of sperm production (meiosis!) |
Epididymis | Storage of sperm outside the testicle (until fully developed and concentrated) |
Seminal vesicle | produce a fluid that provides nutrients and protects the sperm. |
Prostate gland | Produces fluid which contains mineral ions and is basic to help protect sperm. |
Journey of sperm from production to ejaculation
Good acronym to remember: SEVENUP (Sperm, Epididymis, Vas Deferens, EN, Urethra, Penis) 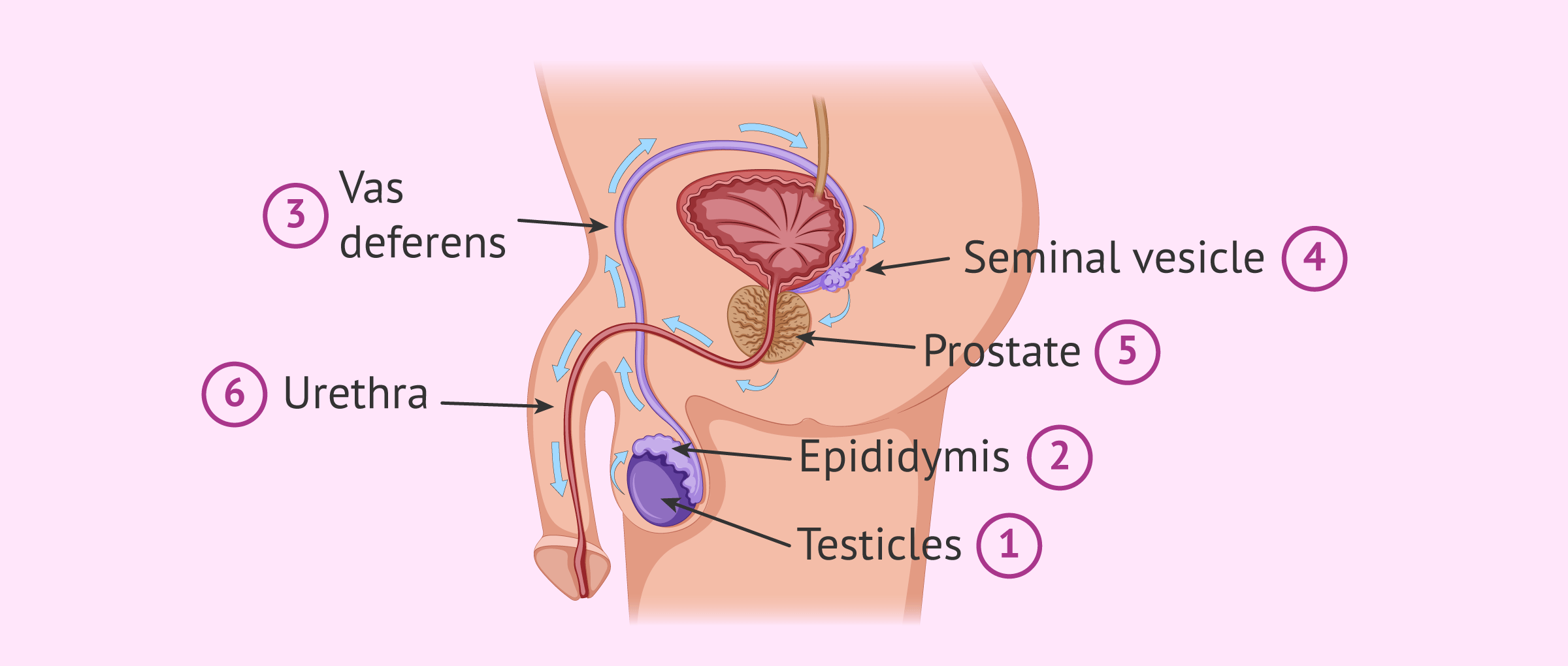
Female reproductive system:
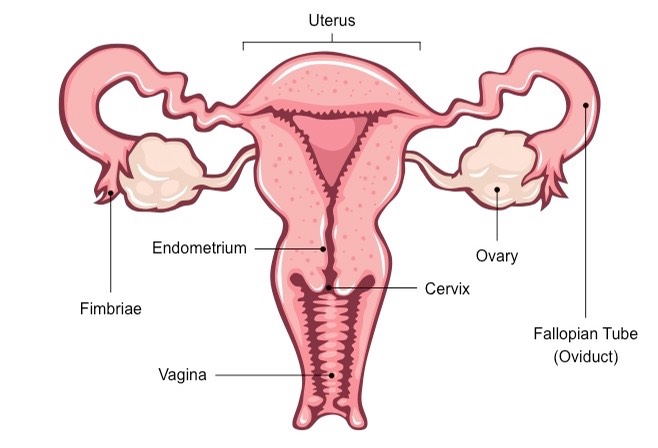
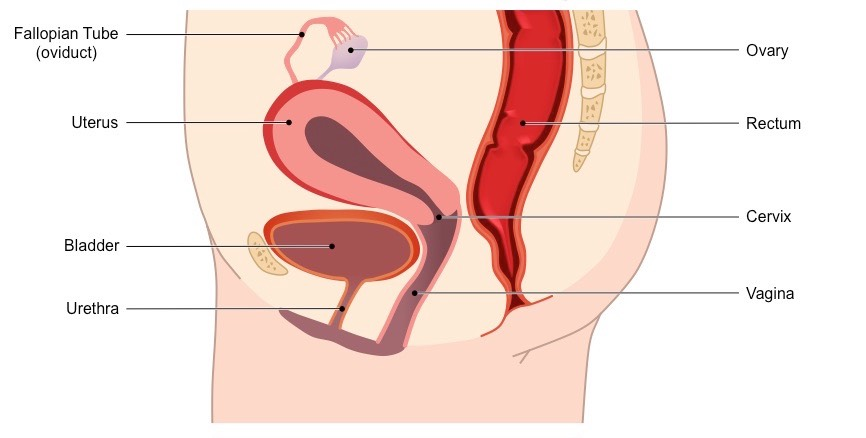
Functions of the organs: (organized according to the path taken by egg)
Ovary - location where oocytes (eggs) mature prior to release (ovulation)
also responsible for estrogen & progesterone secretion
Fallopian tube - transports the oocyte to the uterus
also location where fertilization commonly occurs
Uterus - muscle that supports a fertilized egg during pregnancy and helps push the baby out during birth.
if no implantation of eggs inner lining will shed during menstruation (aka what causes cramps)
Endometrium - mucous membrane lining of the uterus, thickened in preparation of implantation or is otherwise lost (via menstruation)
Neck of the womb (cervix) - muscular opening at the end of the vagina that protects the uterus
Vagina - Passage leading to the uterus by which the penis can enter, stores sperm for fertilization and is also the birth canal.
From school slide show:
Structure | Function |
|---|---|
Ovaries | Creation/storage of eggs until released during ovulation. |
Fallopian Tubes | Passageway from ovaries to the uterus |
Uterus | Muscle that supports a fertilized egg during pregnancy and helps to push the baby out during birth. If no implantation of egg, inner lining will be shed during menstruation. |
What’s an ectopic pregnancy?
its when the embryo attached to the fallopian tube, the problem is that as the pregnancy grows, it can cause the tube to burst and lead to major internal bleeding.
An ectopic embryo will not survive and the pregnancy will miscarry
Menstrual Cycle
Role & origin of menstrual cycle hormones:
Hormone | Source | Role |
|---|---|---|
FSH | Pituitary gland | Stimulates development of follicles and primary oocyte |
LH | Pituitary gland | Triggers egg release (ovulation) |
Estrogen | Ovary (specifically form ruptured follicle) | stimulates growth of lining of uterus and increases FSH receptors |
Progesterone | Ovary (corpus luteum) | Stimulates thickening and maintenance of endometrium and inhibits FSH and LH secretions |
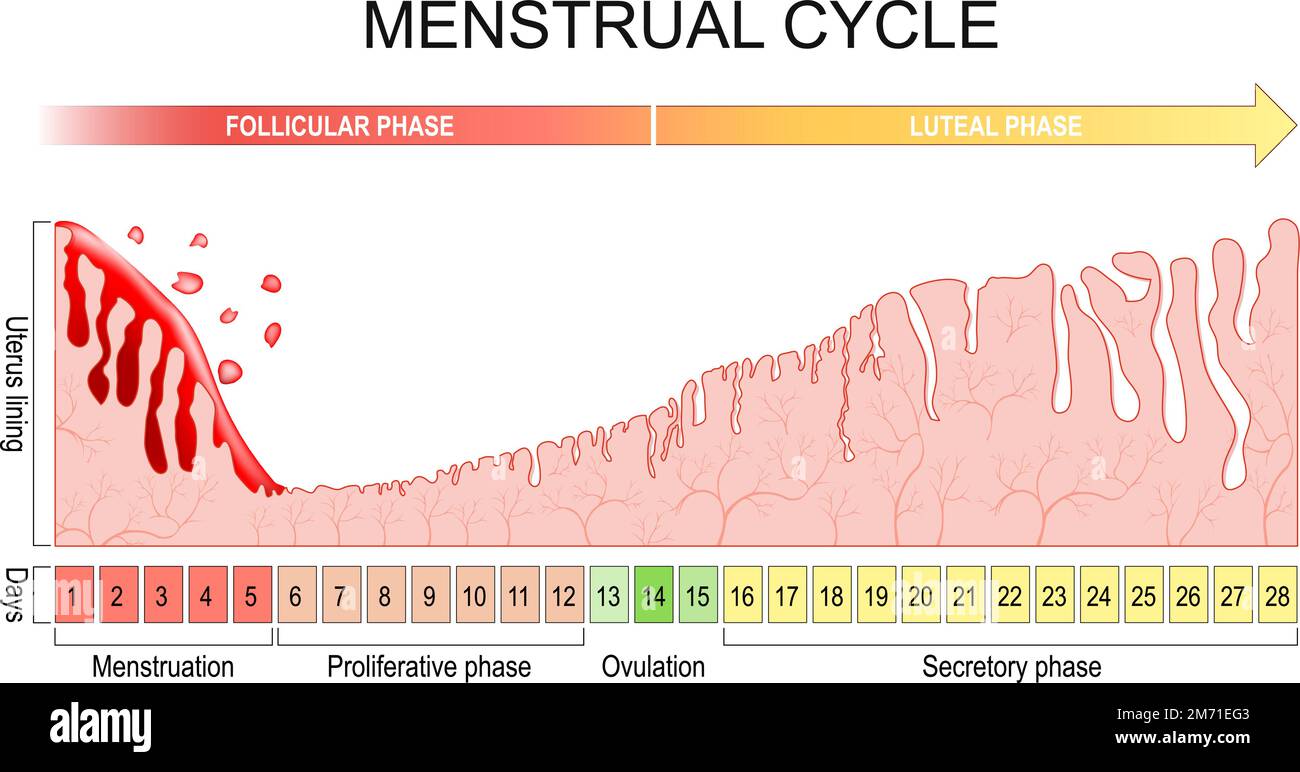
Chart of Menstrual Cycle:
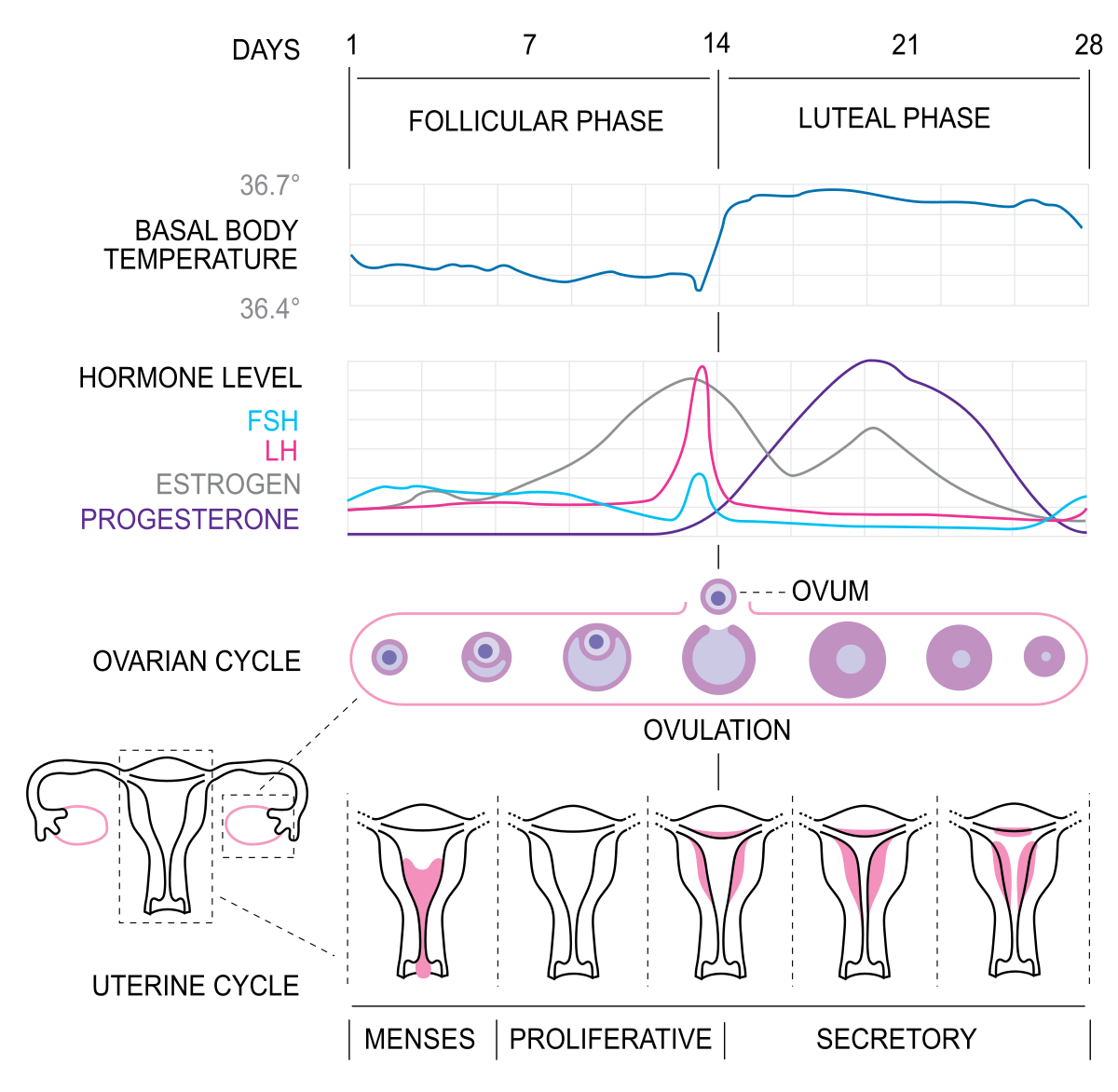
The Human menstrual cycle last ≈ one month (≈ 28 days)
begins at puberty (8-13 years old) and ends with menopause (45-55 years old)
it’s the recurring changes that occur within the female reproductive system to make pregnancy possible
Faces of the Menstrual Cycle:
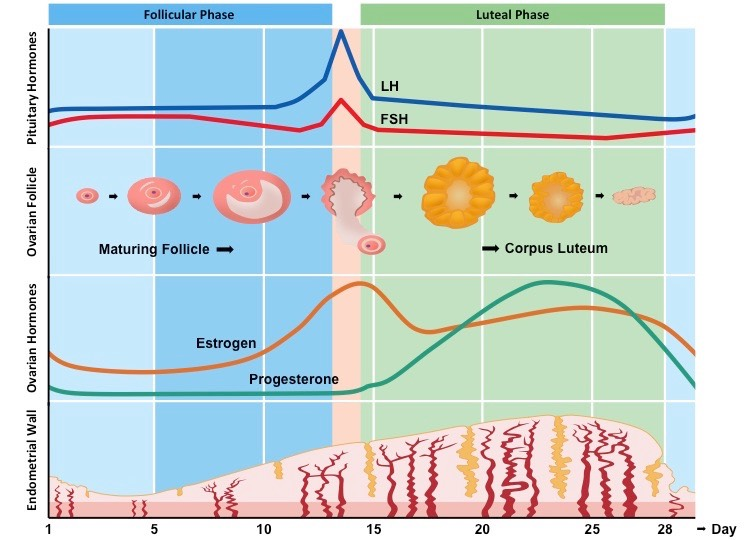
Follicular Phase: (days 1-14):
FSH (follicle stimulating hormone)
increases: is secreted from the anterior pituitary and stimulates development (growth) of follicle
Stimulates secretion of estrogen from follicle wall
Estrogen
secreted form follicle wall (increases) stimulating the repair and thickening of the endometrium
when estrogen is at high levels it inhibits FSH (negative feedback) and stimulates LH (positive feedback)
LH
sharp and sudden peak at end of Follicular Phase (≈ day 14)
stimulates ovulation (rupture of follicular wall to release oocyte)
Ovulation occurs around day 12, estrogen stimulated the anterior pituitary to secrete hormones (positive feedback) resulting in a in a large surge of LH and a lesser surge of FSH, the LH causes the dominant follicle to rupture and release an egg (secondary oocyte) – this is called ovulation
Luteal Phase (days 15-28):
LH
promotes corpus luteum development (follicle wall after ovulation)
corpus luteum secretes estrogen & progesterone (positive feedback)
Estrogen
it is still secreted but at a lower amount from the corpus luteum
works alongside progesterone to thicken the endometrial lining (in preparation for pregnancy)
Progesterone
Increases during early luteal phase
it is secreted from the corpus luteum alongside estrogen
promotes thickening of endometrium
high progesterone inhibits LH and FSH secretions (negative feedback), preventing any follicles from developing
once the levels of progesterone lower it will stimulate LH and FSH secretion again
Endometrium thickness through the menstruation cycle:
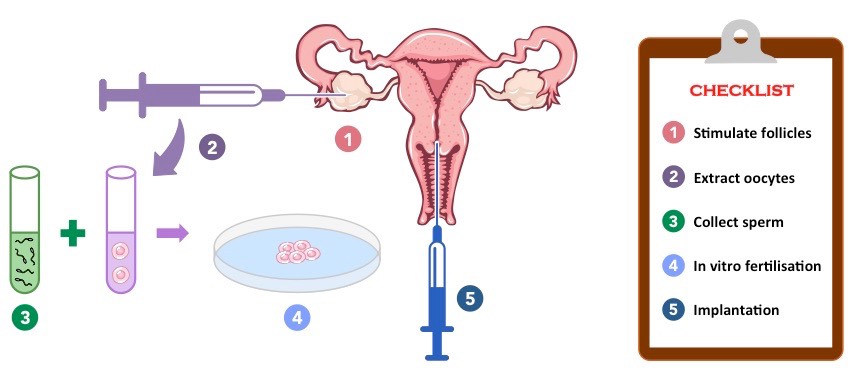
Vitro Fertilization (IVF):
IVF - complex series of procedures used to treat infertility or genetic problems and assist with the conception of the egg (aka as the name suggests In-Vitro Fertilization)
during IVF, mature eggs are retrieved from the ovaries and fertilized by sperm in a lab
Outline of procedure:
Down Regulation - drugs are used to stop the secretion of FSH and LH which in turn also stops the secretion of estrogen and progesterone (aka stop of menstrual cycle)
through stoping the cycle, doctors can take control of timing and quantity of egg production by the ovaries
treatment takes about 2 weeks and is usually done through nasal spray
Artificial doses of hormones (super-ovulation) - injections of FSH & LH to promote follicle development (A LOT OF IT) = supper-ovulation
done to develop and collect multiple eggs form the woman
first injected with large amounts of FSH to stimulate the development of many follicles
these follicles are then treated with human chorionic gonadotrophin (hCG) - a hormone produced by a developing embryo
this hormone stimulates the follicle to mature (into an egg)
Egg retrieval and fertilization - a micropipette on ultrasound scanner is passed through the uterus to collect the eggs which are then mixed with a 100,000 sperm on a petri dish. Sperm will also often be directly injected into the egg
the eggs are incubated in the presence of a sperm sample from the male donor
the eggs are then analyzed under a microscope for successful fertilization
Establishing a pregnancy (Implantation) - successful embryos are then implanted in the uterus, extra doses of progesterone are given
extra doses of progesterone are given to develop the endometrium, this is done ≈ two weeks prior to implantation
multiple embryos are transferred to improve chances of successful implantation
at about 2 weeks after implantation, a pregnancy test is taken to determine if the process has been successful.
Mnemonic to remember the stages of IVF: SHE’S FIT
Stop normal menstrual cycle (with drugs)
Hormone treatments to promote super ovulation
Extract multiple eggs from the ovaries
Sperm collected, then prepared (via capacitation) and injected into egg
Fertilization occurs externally under controlled conditions (in vitro)
Implantation of multiple embryos into uterus (either patient or surrogate)
Test for pregnancy after ~ two weeks
Diagram of IVF procedure:
11.4 Sexual Reproduction (HL)
Recall: Mitosis & Meiosis
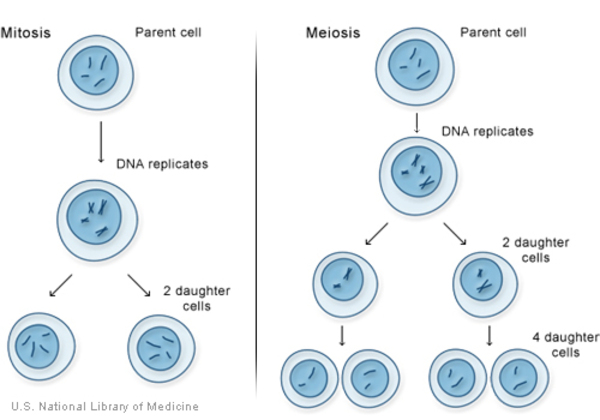
Gametogenesis is the process by which diploid precursor cells undergo meiotic division to become haploid gametes (sex cells)
In males, this process is called spermatogenesis and produce spermatozoa (sperm)
In females, this process is called oogenesis and produce ova (eggs)
The process of gametogenesis occurs in the gonads and involves the following steps:
Multiple mitotic divisions and cell growth of precursor germ cells
Two meiotic divisions (meiosis I and II) to produce haploid daughter cells
Differentiation of the haploid daughter cells to produce functional gametes
Spermatogenesis
What is it?
process of production of spermatozoa (sperm) in the seminiferous tubes of the Testes
germline cells go through mitosis (first), growth, 2 divisions of meiosis and then cell differentiation
From BioNinja:
“Spermatogenesis describes the producton of spermatozoa (sperm) in the seminiferous tubules of the testes
The process begins at puberty when the germline epithelium of the seminiferous tubules divides by mitosis
These cells (spermatogonia) then undergo a period of cell growth, becoming spermatocytes
The spermatocytes undergo two meiotic divisions to form four haploid daughter cells (spermatids)
The spermatids then undertake a process of differentiation in order to become functional sperm cells (spermatozoa)”
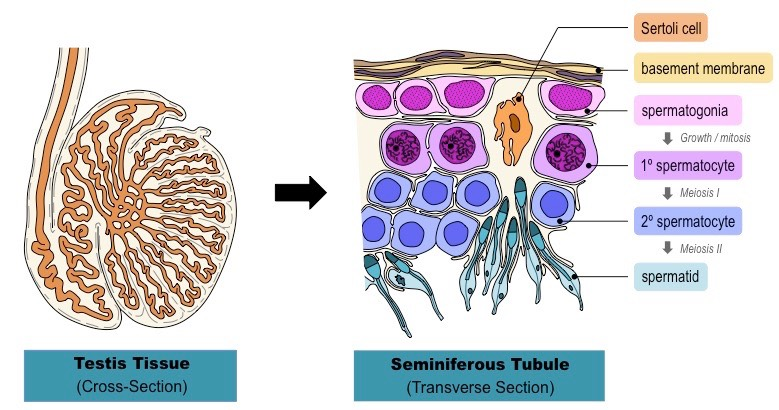
Vocabulary:
Germinal epithelium - the epithelial layer of the seminiferous tubules of the testicles
seminiferous tubules - mass narrow tubes, location of sperm production
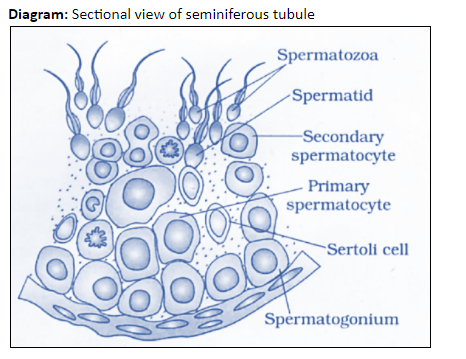
parts inside the seminiferous tubules:
Interstitial cells (Leydig cells) - cells adjacent to tubules to produce testosterone
sertoli cells - large nurse sells locaded in tubule walls
Process of Spermatogenesis
Germinal epithelium cells divide endlessly by mitosis to produce more diploids
The diploid cells undergo a period of cell growth becoming primary spermatocytes
Each primary spermatocyte will then undergo meiosis I and produce 2 haploids (secondary spermatocyte)
Each secondary spermatocyte will carry meiosis II producing 2 spermatids (in total form the after Meiosis I & II from a single cell, 4 spermatids will be produced)
Spermatids will then become associated with sertoli cells (nurse cells) that will help them develop into spermatozoa (this is a form of differentiation)
The spermatozoa detach form the sertoli cell then eventually will be carried out of the testies by fluid in the center of the tubule
Diagram of Sperm production with cells:
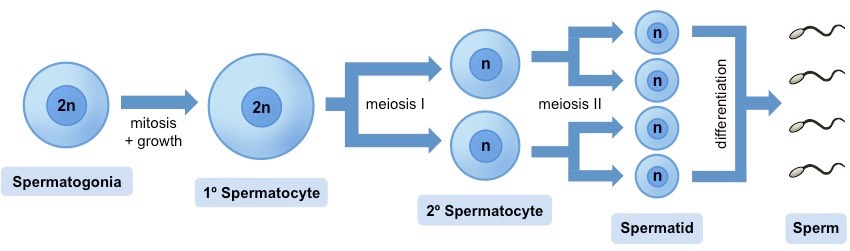
Diagram of seminiferous tubule with each stage of Spermatogenesis:
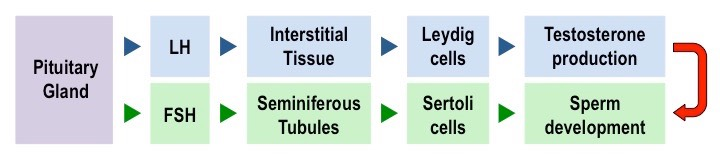
 Hormonal control of Spermatogenesis (Male Sex Hormones)
Hormonal control of Spermatogenesis (Male Sex Hormones)
spermatogenesis is controlled by three key hormones - FSH, LH & testosterone
FSH & LH are secreted by the anterior pituitary
testosterone is secreted by Leydig Cells
FSH
Starts spermatogenesis by triggering meiosis I of spermatocytes
also activate Sertoli cells, which provide nourishment for sells undergoing spermatogenesis
LH
triggers testosterone secretion by Leydig cells in the interstitial tissue
Testosterone
completes spermatogenesis by triggering meiosis II of spermatocytes
stimulates differentiation of spermatids to form mature spermatozoa
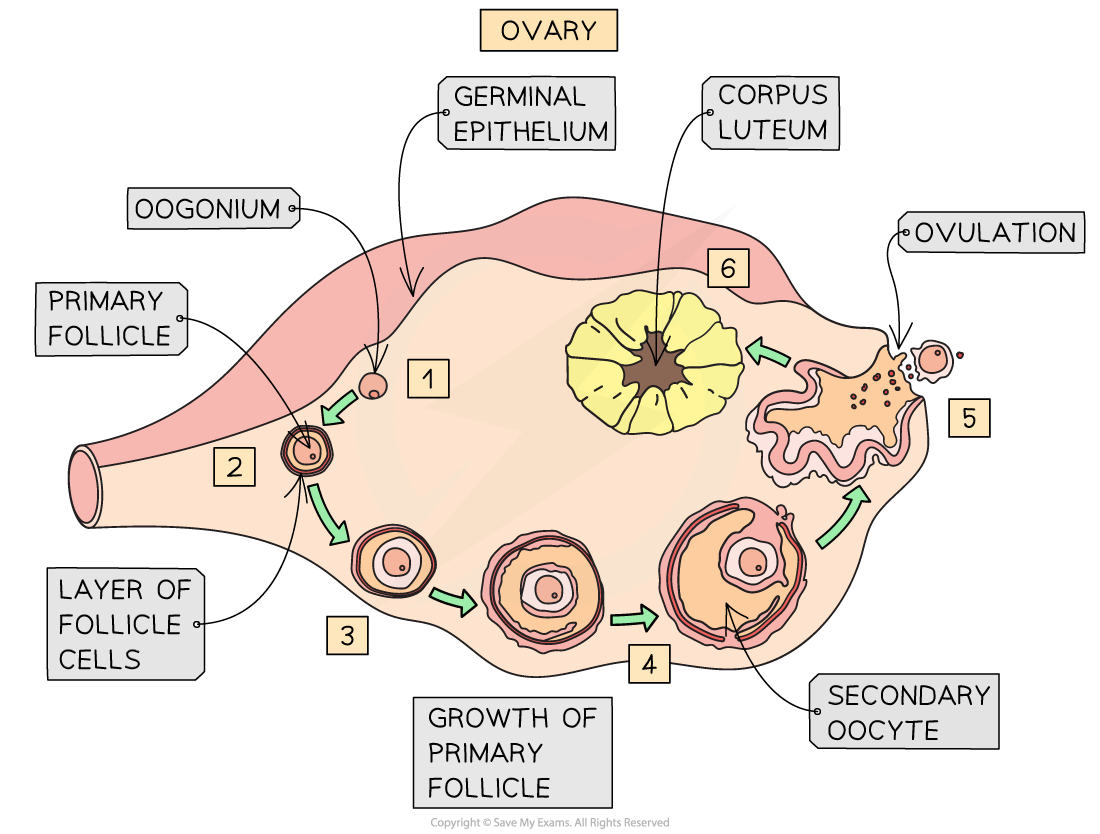
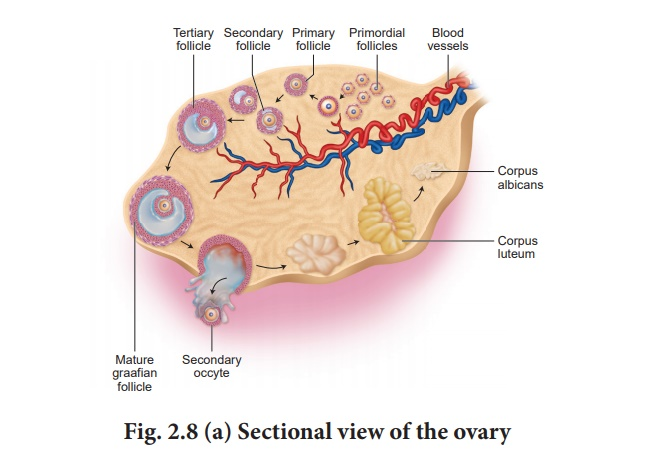
Oogenesis:
What is it?
process of creation of a human egg
involves mitosis, growth, 2 divisions of meiosis and then cell differentiation.
Vocabulary:
Primary Follicle/Primary Oocyte - cell formed before birth form germinal epithelium
Mature Follicle - mature primary follicle (this is caused by FSH stimulating their growth
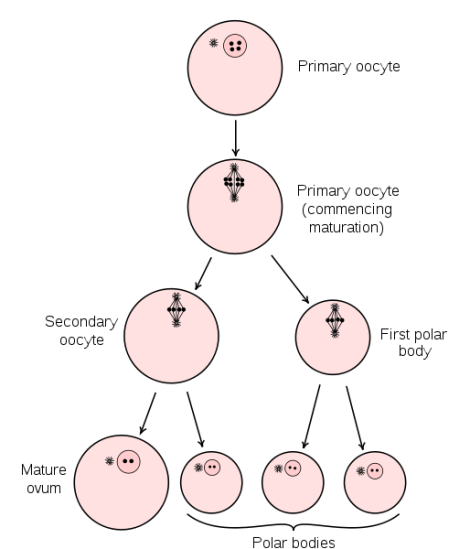
Process of Oogenesis:
process starts during fetal development, when a large number of primordial cells are formed through mitosis
these cells undergo cell growth until they are ready to go through mitosis (they are now called primary oocytes)
the primary oocytes then begin meiosis I but are arrested at prophase I when granulosa cells surround them to form follicles
they remain arrested in prophase I until puberty, when menstrual cycle begins
each month FSH will trigger the continued division of some of the primary oocytes
these will complete meiosis I producing 2 diploid cells of unequal size
one cells retains the entirety of the cytoplasm to form a secondary oocyte, while the other cell forms a polar body
Polar body - small haploid cells created during oogenesis, generally don’t have the ability to be fertilized, have berry small cytoplasm
the polar body remains trapped in the follicle until it eventually degenerates
secondary oocyte begins meiosis II but is arrested in metaphase II
here ovulation (as a consequence of LH secretion) occurs where it the sec. oocyte is released form the ovary and into the fallopian tube
the follicular cells surrounding the oocyte dorm a corona radiate and function to nourish the secondary oocyte
the the oocyte is fertilized by a sperm, chemical changes will trigger the completion of meiosis II & the formation of another polar body (the 1st one may also undergo meiosis II to form a third polar body)
once meiosis II is complete the mature egg forms a ovum, before fusing its nucleus w/ the sperm’s nucleus to form a zygote
Diagram of Oogenesis in cells:
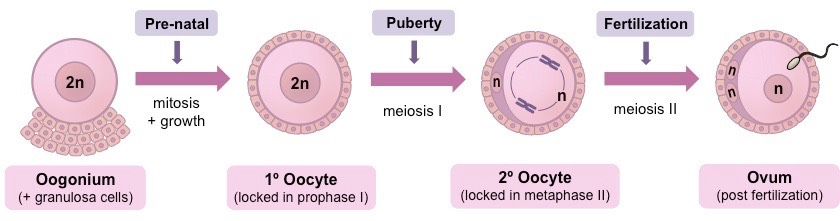
Oogenesis in the ovary diagram:
Anatomy & function of a Spermatozoa & Egg:
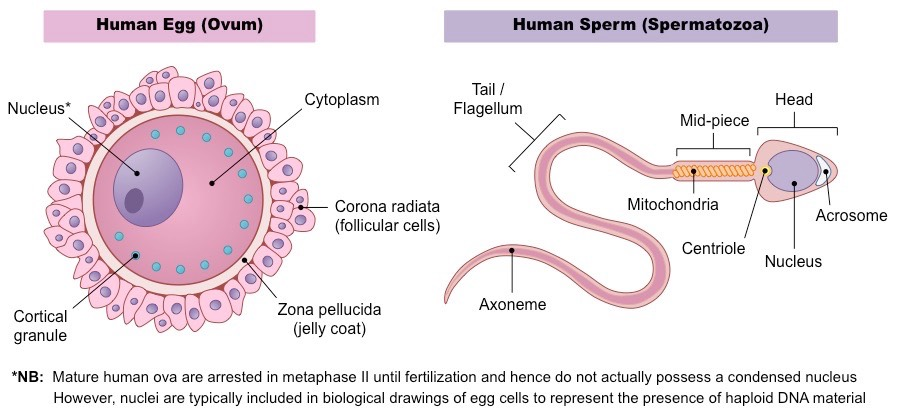
Human sperm:
Acrosome - contains hydrolytic enzymes that will hep it penetrate the egg for fertilization
Nucleus - contains the haploid nucleus w/ the male genome
Mitochondria and tail - provides ATP for locomotion. Sperm must swim form the vagina to the egg in the fallopian tubes.
Human egg:
Nucleus - contains the haploid nucleus with all of the female genome
Zona pellucida - glycoprotein layer with receptors that allow the sperm to bind
Cortical granules - vesicles near the egg membrane, once activation takes place it will release its contents vie exocytosis.
this prevents any further sperm from being able to bind to the egg
corona radiata - layer of cells that nourish the egg
Compare and contrast: Spermatogenesis and Oogenesis
Spermatogenesis | Oogenesis | |
|---|---|---|
Cells undergoing meiotic division | Germ cells | Germ cells |
Number of gametes produced | Millions produced daily. | One every 28 days. |
When do gametes start to form? | puberty | fetal development (till primary oocyte arrested at prophase I) |
Release of gametes. | ejaculation | ovulation (about day 14) of the menstrual cycle |
Duration of production | All adult life | till it becomes irregular at around 40 years old and then stops at menopause. |
Number of cells produced in each round of meiosis | 4 sperm produced per meiosis. All have reduced cytoplasm | One egg, with all the cytoplasm, produced per meiosis (others are polar bodies which disintegrate) |
Fertilization
Animal fertilization:
External
involves the fusion of gametes (egg and sperm) outside of the body of a parent
most common in aquatic animals, where water acts as a medium in which gametes can travel
this method is susceptible to environmental influences such as predators, pH change, temperature and pollution
as a consequence of such species that use this form tend to release large quantities of gametes to compensate the losses
process of releasing gametes into the water is called spawning
Internal
involves the fusion of gametes (egg and sperm) inside of the body of a parent
terrestrial animal tend to use this form of fertilization so as to prevent exposure and desiccation of gametes or embryos
It is also a form that prevents gametes from drying out and protects developing embryo.
some aquatic animals do this too (e.g. dolphins)
requires a method by which the gamete of one parent can be introduced inside the body of another (e.g. copulation)
this method offers more protection to the gametes and embryos but at a potential survival cost to the parent.
Human fertilization:
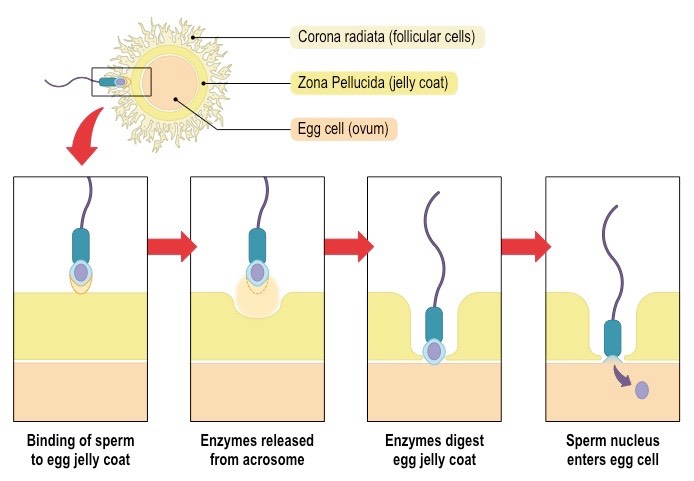
3 stages of fertilization
Acrosome reaction - the sperm contains a large lysosome-like structure (acrosome) which releases proteolytic enzymes (allows the sperm to break through the surrounding zona pellucida)
Penetration of membrane - proteins on sperm membrane bind with those on the egg membrane. When membranes fuse, the sperm’s nucleus enters the egg.
the sperm pushes through the follicular cells of the corona radiata and binds to the zona pellucida
the acrosome vesicle fuses with the zona pellucida and releases digestive enzymes with softer the glycoprotein matrix
sperm pushes its way through the softened zona pellucida and binds to the exposed receptor proteins on the egg’s membrane
the membrane of the egg and sperm fuse and the sperm’s nucleus (and centriole) enter the egg
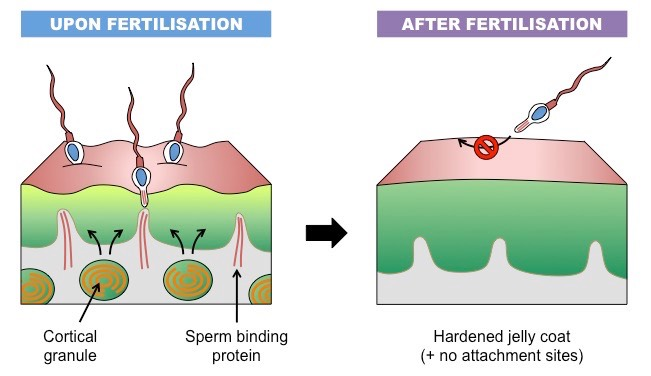
Cortical reaction - fusion of sperm and egg membrane activates cortical granules, whose enzymes digest binding proteins on the eggs so no more sperm can bind.
it occurs in order to prevent polyspermy
cortical granules within the egg’s cytoplasm release enzymes (via exocytosis) into the zona pellucida
these enzymes destroy the sperm binding sites was well as thicken & harden the glycoprotein matrix of the zona pellucida
this prevents other sperm from being able to penetrate the egg (polyspermy), ensuring the zygote formed is diploid
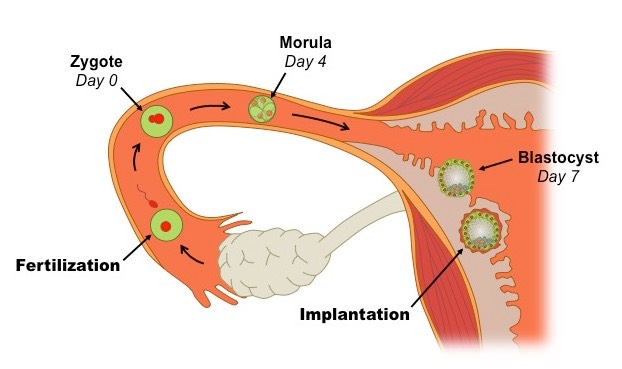
After fertilization, mitosis and cell differentiation can take place….
Implantation of Blastocyst
blastocyst - hollow ball of cells create at around 5-7 days after fertilization
The egg has used up its energy reserves and needs to connect to the endometrium (uterine lining) to be continually supplied.
final stage of embryo development
The blastocyst breaches the jelly coat that was surrounding it and preventing its attachment to the endometrium
Digestive enzymes are released which degrade the endometrial lining, while autocrine hormones released from the blastocyst trigger its implantation into the uterine wall
blastocyst is comprised of three distinct sections:
An inner cell mass (that will develop into the embryo)
A surrounding outer layer called the trophoblast (this will develop into the placenta)
A fluid filled cavity called the blastocoele
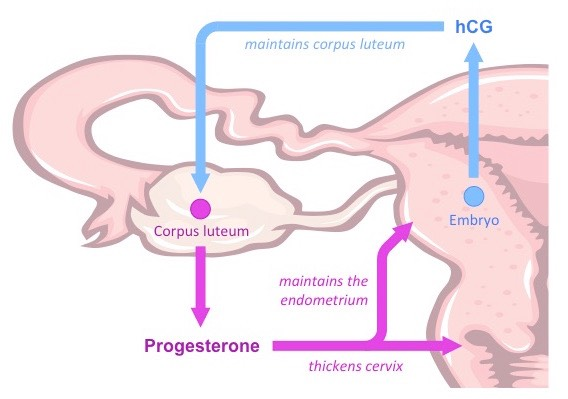
Human Chorionic Gonadotropin (hCG)
when blastasis become implanted in the endometrial lining it begins to secrete hCG
hCG promotes the maintenance of the corpus luteum within the ovary and prevents its degeneration
as a result the corpus luteum survibes and continues to secrete both oestrogen and progesterone
estrogen inhibits FSH & LH secretion, preventing the release of any more eggs form the ovaries (aka stops the menstrual cycle)
progesterone also functions to maintain the endometrium (which is nourishing the embryo) and thicken the cervix
the levels of hCG are maintained for roughly 8-10 weeks while placenta develops
after this the placenta takes the role of the hCG and starts producing progesterone and nourishing the embryo
at this point the corpus luteum is no longer needed and begins to degenerate as hCG levels drop
Fun fact - this is the horone that pregnancy test measure as it is found in the blood and urine. Testing for hCG can be done as soon as 10 days after conception to help determine if you are pregnant.
Measuring hCG can also help identify complications during pregnancy.
Also fun fact - pregnancy blood tests are about 99 per cent accurate and can detect lower amounts of hCG than urine pregnancy tests!
Why must the endometrial lining thicken? What signals this to happen & where does it come from?
It must thicken as during pregnancy the embryo will implant itself into the endometrium. The thickening of the endometrium allows the embryo to successfully implant itself on it and receive the nutrition if needs.
the endometrium gets thicker as pregnancy progresses
The endometrium will remain thick and develop a rich blood supply and form connections with the placenta to supply the baby with everything it needs.
Progesterone is in charge of stimulating this and it is first released form the corpus luteum in the ovaries and later secreted by the placenta during pregnancy
More into hormones & the placenta:
Estrogen stimulates the growth of uterine muscles (myometrium) and the development of the mammary glands
Progesterone maintains the endometrium, as well as reducing uterine contractions and potential maternal immune responses
Both estrogen and progesterone levels drop near the time of birth
Placenta
functions as the life support system for the fetus, serving two key functions:
It facilitates the exchange of materials between the mother and fetus
It secretes hormones to maintain the pregnancy after the corpus luteum has degenerated
The placenta is a disk-shaped structure formed from maternal and fetal membrane tissues. During pregnancy the placenta acts as an endocrine gland producing hCG and a site of exchange of materials between mother and fetus.
Around 9 weeks it starts producing estrogen and progesterone to maintain the endometrium.
Does the maternal and fetal blood ever mix?
Maternal and fetal blood meet at the placenta, but do not mix. The placenta and the fetus are connected through the arteries and veins in the umbilical cord.
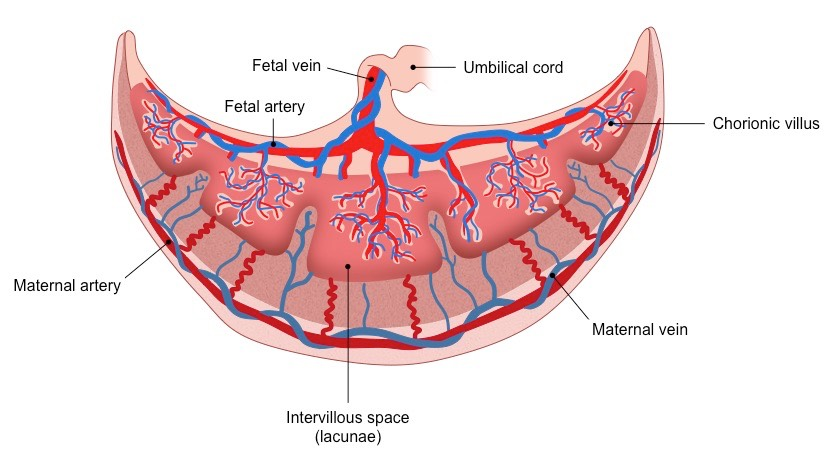
How does the structure of the placenta facilitates exchange between mother and fetus
Placental villus - fingerlike projections of placenta to increase SA
inter-villus spaces- location where Maternal blood flows it is the groves between the villus
aid in increase SA
Chorionic villi extend into these pools of blood and mediate the exchange of materials between the fetus and the mother
Fetal capillaries- its blood is close to surface of each villus = 5 um of space between fetal and maternal blood!
project up into the chorionic villus
Placental barrier - cells that separate maternal and fetal blood
Umbilical cord - connective tube between the baby and the placenta via which the exchanged material is transported from the villi to the fetus
 Material Exchange
Material Exchange
chorionic villi extend into the intervillous space and exchange materials between the mother and foetus
Chorionic villi are lined by microvilli to increase the available surface area for material exchange (increase SA)
Foetal capillaries within the chorionic villi lie close to the surface to minimise diffusion distance from blood in the intervillous space
Materials such as oxygen (, nutrients, vitamins, antibodies and water will diffuse from the intervillous space into foetal capillaries
Birth
Progesterone: increases throughout pregnancy. Falls at the end which signals the secretion of oxytocin.
Oxytocin: causes uterine contractions. These contractions stimulate stretch receptors in uterus signaling pituitary to secrete more oxytocin = contractions become stronger and more frequent!
Estrogen:
Stimulates junctions between muscles cells in the uterus so coordinated contractions can occur
Induces formation of oxytocin receptors on uterus