Chapters 27 & 28: The Reproductive System
Introduction to the Human Reproductive System
The human reproductive system functions to produce, store, nourish, and transport gametes (reproductive cells).
Fertilization is the process where a sperm from the male and an immature oocyte from the female fuse to create a zygote (fertilized egg).
Organization of the Reproductive System
The reproductive system consists of:
Gonads— Reproductive organs that produce gametes & hormones
Males— Testes & Testosterone
Females— Ovaries & Estrogen
Ducts— Recieve, store, & Transport the gametes
Accessory glands and organs— Secrete fluids into the ducts of the reproductive system or into other excretory ducts
External genitalia— Perineal structures
Male:
Testes (gonads) generate sperm, and testosterone
Female
Vagina connects the uterus to the exterior; the ovaries release an egg transported through uterine tubes.
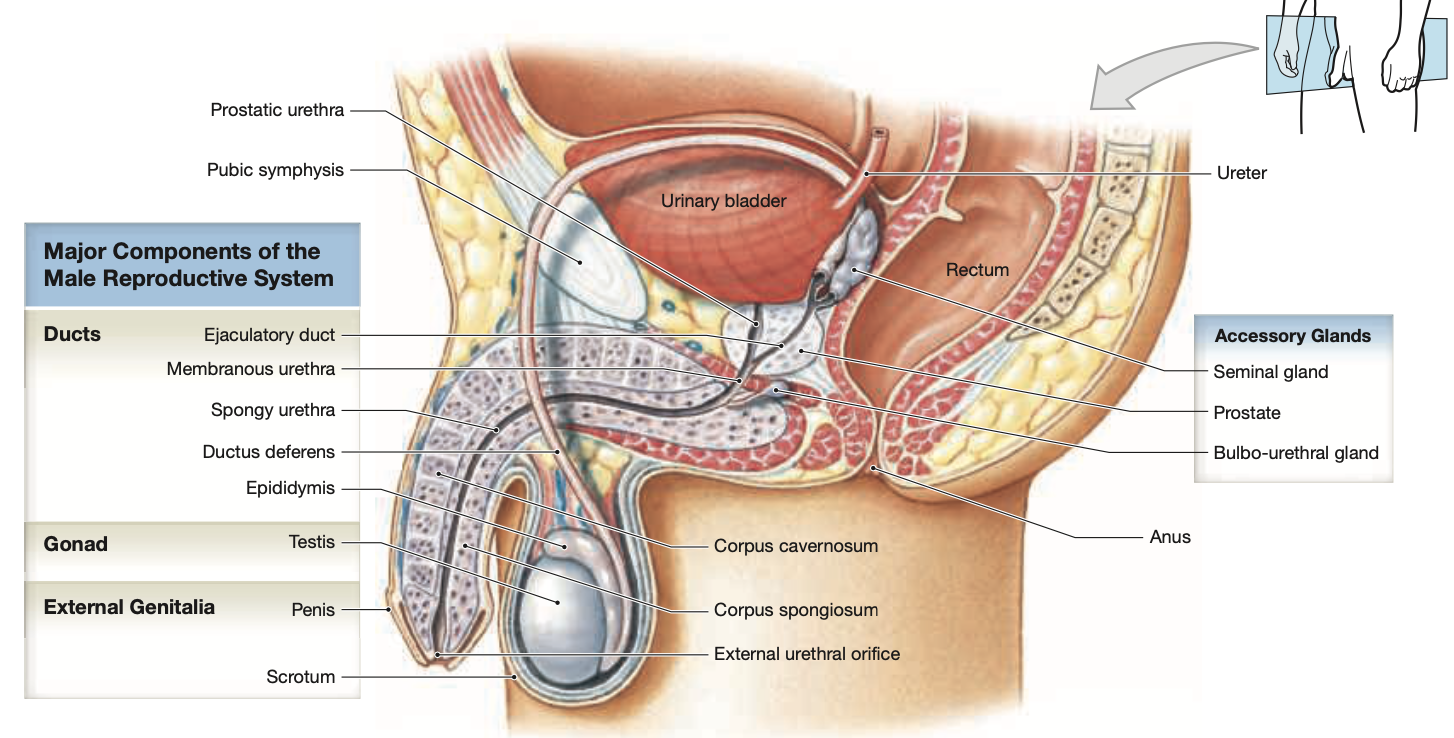
Anatomy of the Male Reproductive System
Sperm Transport Pathway:
Epididymis— a coiled tube where sperm mature and are stored after being produced in the testis.
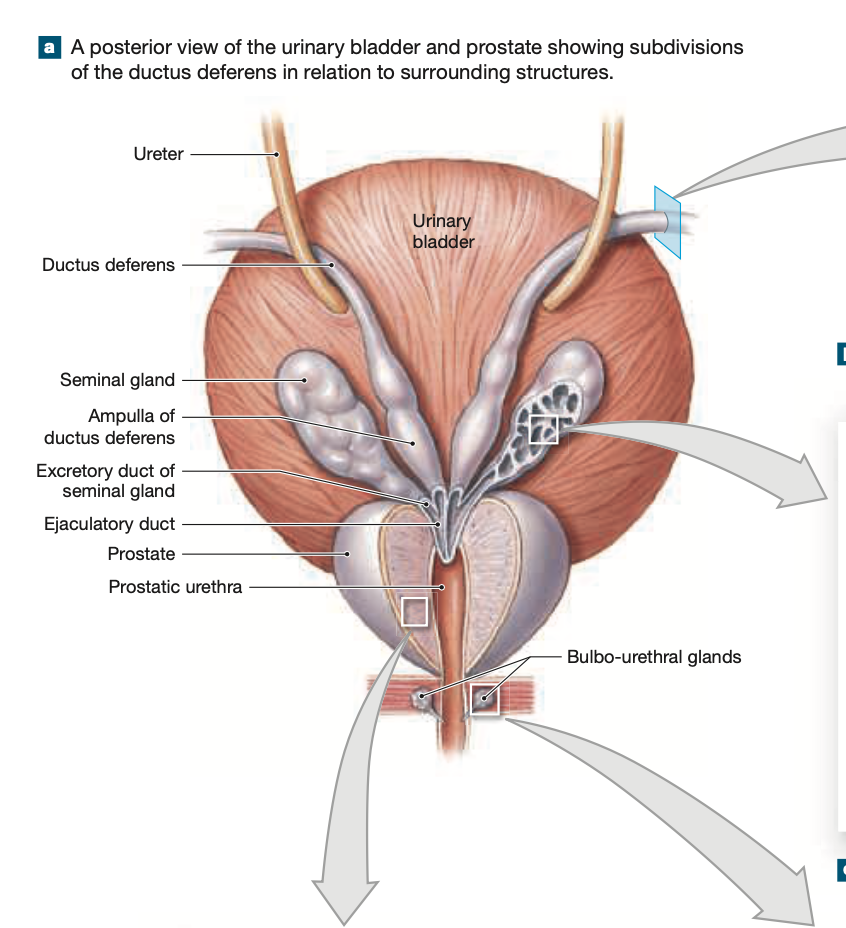
Ductus Deferens— Begins at the tail of the epididymis,travels into the abdominpelvic cavity via the inguinal canal, passes behind the bladder, and connects to the ejaculatory duct, where sperm is mixed with seminal fluid to form semen.
Serves as a transport tube that carries sperm from the epididymis to the ejaculatory duct
Ejaculatory Duct— a tube that conveys sperm mixed with seminal fluid into the urethra during ejaculation.
Urethra— the duct that carries sperm from the reproductive tract, serving as the final passage for both bodily excretions.
Prostatic
Membranous
Spongey
Accessory Organs:
(2) Seminal glands— Embedded in CT on either side of the midline, sandwiched between the posterior wall of the urinary bladder and the anterior wall of the rectum
Responsible for producing a significant portion of the fluid that composes semen (60%)
(1) Prostate— Small rounded organ that encircles the prostatic urethra as it leaves the urinary bladder
Produces a weakly acidic fluid (prostatic fluid) that nourishes and protects sperm, contributing to about 20-30% of the seminal fluid.
(2) Bulbourethral Glands— Located at the base of the penis, these glands produce a clear, slippery fluid that helps to lubricate the urethra and neutralize any acidity, contributing approximately 5% of the total seminal fluid.
External Genitalia: The scrotum & penis
The Penis— A tubular organ for sexual intercourse and conducting urine to the exterior—
Root— Attaches to the rami & ischia
Body (shaft)— Movable portion
Glans Penis— The bulbous tip of the penis that is highly sensitive and plays a crucial role in sexual arousal.
Secrete smegma
Prpuce— Foreskin
The Testes
Size: approximately 2 in. long, 1 in. in diameter.
Descent occurs via the gubernaculum testis during fetal development, usually at around 7 months.
Spermatic cord: A bundle of fibers and tissues that includes the vas deferens, blood vessels, nerves, and lymphatic vessels connecting the testes to the abdominal cavity.
Ductus deferens
Testicular artery and vein
Pampiniform plexus
Nerves (ilio-inguinal and genitofemoral).
Cremaster Muscle: This muscle regulates the temperature of the testes by contracting or relaxing to elevate or lower them in response to temperature changes.
Spermatogenesis must occur at 96 degrees
Cremasteric Reflex: Dartos (superficial) & Cremaster (deep)muscles contract due to sexual arousal or change in temperature
The Scrotum— a pouch of skin that holds the testes, helps to protect them and keeps them at the optimal temperature for spermatogenesis by adjusting its position in relation to the body.
Testicular Structure and Function
Tunica albuginea— Dense layer of CT surrounding each testis, surrounded by
Tunica Vaginalis— serous membrane that surrounds the tunica albuginea and reduces friction
Seminiferous tubules— U shaped tubule responsible for sperm production.
Testosterone is produced in the interstitial cells surrounding the seminiferous tubules
Within tubules, spermatogonia (stem cells) undergo spermatogenesis leading to the creation of spermatids, which mature into sperm through spermiogenesis.
Anatomy of a Sperm
Composed of:
Head with an acrosome
Neck
Middle piece
Tail (flagellum).
Lacks intracellular structures, depends on external environment for nutrients.
Haploid
Male Reproductive Tract
After production, sperm travel to the epididymis for maturation (capacitation).
The ductus deferens transports and stores sperm and connects to the ejaculatory duct leading to the urethra.
Accessory Glands
Activate and nourish sperm, neutralizing acidity in the urethra and vagina.
Seminal Gland: 60% of semen volume, rich in fructose for energy.
Prostate: contributes 20-30% with antimicrobial properties.
Bulbourethral Glands: provide lubrication with alkaline mucus.
Semen
Typical ejaculation: 2-5 ml, containing 20-100 million sperm/ml.
Mixture of secretions from accessory glands with enzymes for sperm function.
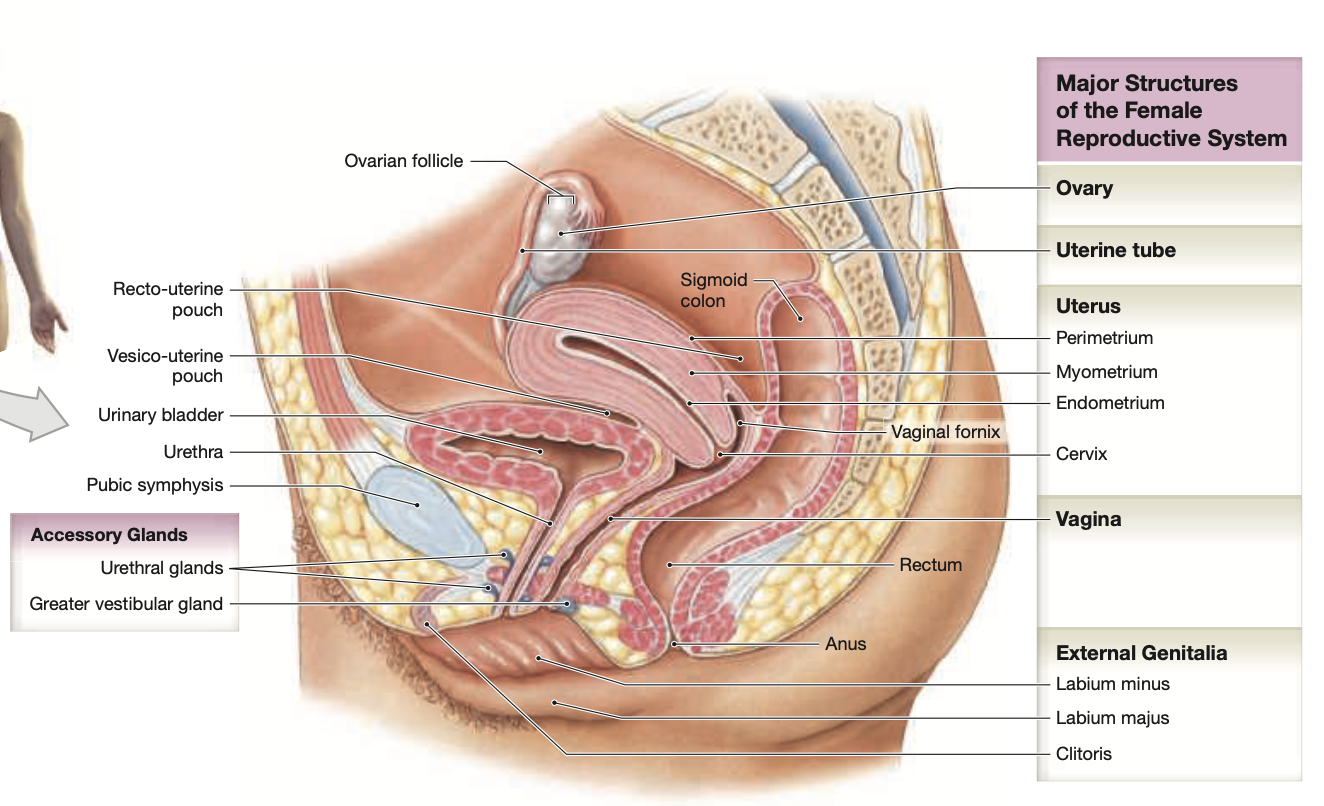
Anatomy of the Female Reproductive System
Main structures:
Ovaries— the female gonads responsible for producing ova (eggs) and secreting hormones such as estrogen and progesterone.
Uterine tubes (Fallopian Tubes)— the channels through which ova travel from the ovaries to the uterus, also serving as the site of fertilization when a sperm cell successfully meets an egg.
Uterus— The hollow, muscular organ in which a fertilized egg implants and develops into a fetus during pregnancy.
Vagina— Connects urterus to the external environment
External genitalia— The labia
Ovaries supported by ovarian and suspensory ligaments.
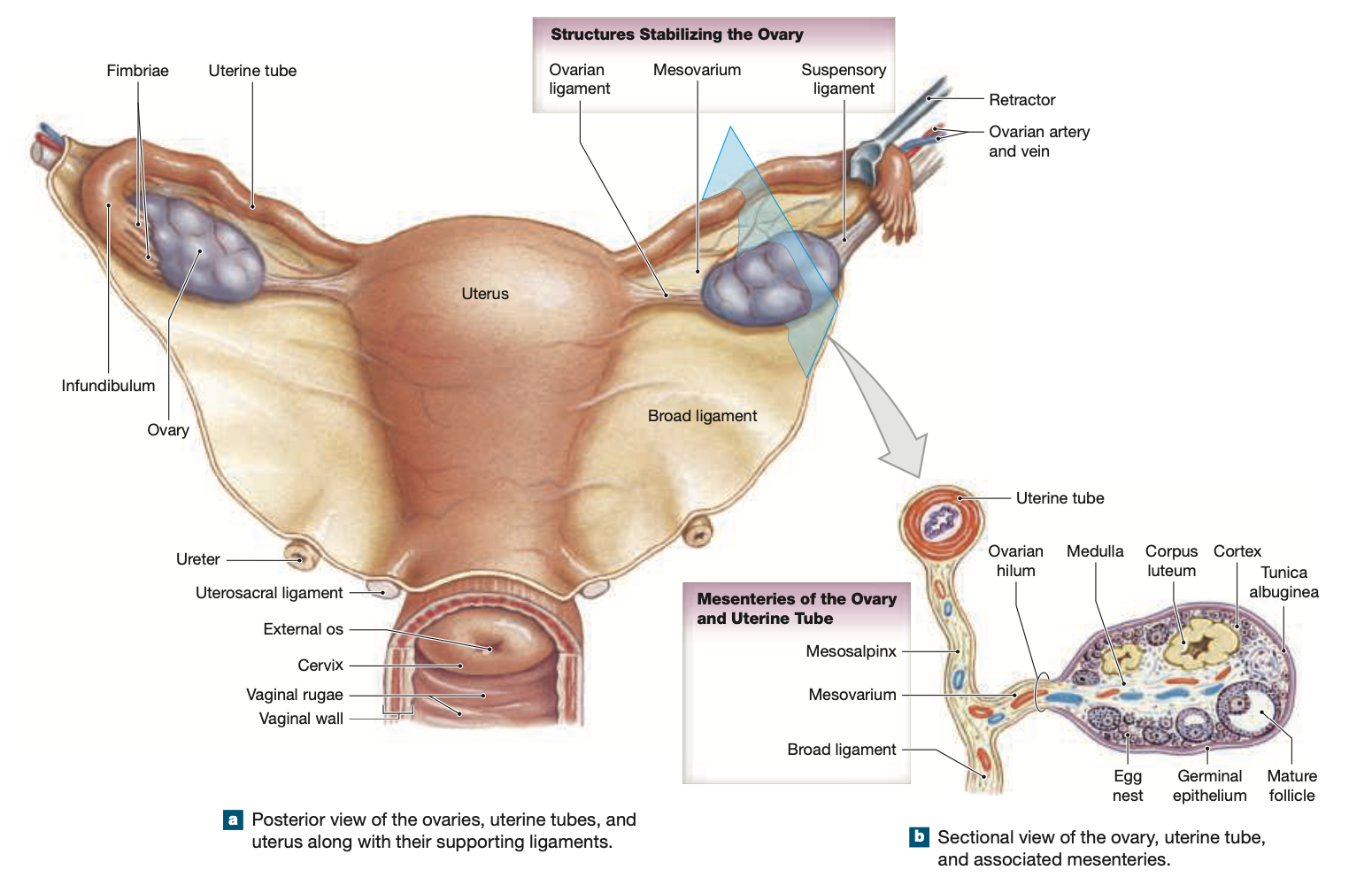
The Ovaries and Oogenesis
Lateral to the Uterus, the ovaries are anchored in the pelvic cavity
The primary function of the ovaries is to produce Oocytes & secrete Estrogen & Progesterone
Ovarian follicles undergo changes throughout the ovarian cycle.
Follicular Development: Primordial → Primary → Secondary → Tertiary (vesicular) follicle.
Ovulation: the secondary oocyte released and surrounded by corona radiata.
Corpus Luteum forms post-ovulation, secreting progestins until it degenerates into corpus albicans if no fertilization occurs.
The Uterine Tubes
The Uterine tubes transport the oocyte from the ovaries to the uterus:
Infundibulum— Funnel-shaped end containing Fimbriae — Finger-like projections that help capture the oocyte during ovulation and guide it into the uterine tube.
Ampulla— The widest and largest segment of the fallopian tubes, where fertilization typically occurs
Isthmus— The narrow, medial third of the fallopian tube that connects to the uterus
Interstitial Part— The short segment of the uterine tube that passes through the uterine wall, playing a vital role in anchoring the tube to the uterus.
Ciliated epithelium aids in transporting the oocyte to the uterus.
The Uterus
A thick-walled muscular organ that is responsible for supporting a developing fetus
Provides support and nourishment to the embryo, stabilized by various ligaments.
Located between the Urinary Bladder (anteriorly) and Rectum (Posteriorly), there are there regions of the uterus:
Fundus— The rounded, superior portion of the uterus that is positioned above the openings of the fallopian tubes
Body— The main portion of the uterus, where implantation of the fertilized egg occurs and the developing fetus grows during pregnancy.
Cervix— The narrow, lower part of the uterus that connects to the vagina, serving as a passageway for menstrual fluid to exit the body and for sperm to enter during conception.
Internal os— Opening from uterus to cervix
External os— Opening from cervix to vagina
There are 3 layers of the uterus:
Endometrium (inner)— sheds during menestration
Myometrium (muscular)— thick middle layer
Perimetrium (outer)—perimetrium serves as a protective layer for the uterus
The uterus is supported by several Ligaments that help maintain its position within the pelvic cavity—
Suspensory Ligament— Contains ovarian artery & vein
Uterine Cycle reflects changes in response to hormonal fluctuations involving endometrial formation and shedding.
The Vagina
A muscular tube serving as the passage for menstrual flow, sexual intercourse, and childbirth
Elastic muscular tube from the uterus to external genitalia, lined with stratified squamous epithelium and rugae.
Extends from cervix to the external vaginal orifice
Located posterior to the urethra and bladder, anterior to the rectum
External Genitalia (Vulva)
Structures include:
Vestibule
Labia minora and majora
Clitoris
Mons pubis.
Glands keep the area around the vestibule moistened.
The Breasts
Lactation occurs in mammary glands regulated by hormones (prolactin, human placental lactogen).
Ducts lead to the nipple, where milk is transferred.
Aging and the Reproductive System
Menopause
Occurs around age 50, signifying the end of ovulation and menstruation. Hormonal production shifts.
Male Climacteric
Occurs between ages 50-60, marked by declining testosterone levels alongside increases in FSH and LH.
Development Overview
Begins with fertilization, categorized into prenatal and postnatal stages.
Fertilization Process
Usually occurs within the uterine tube; sperm must undergo capacitation.
Around 200 million sperm reach the vicinity, with few fertilizing the oocyte.
Prenatal Development
Ensues through trimesters with critical developments occurring within the first trimester, including blastocyst formation and implantation.
Critical structures include the placenta, yolk sac, amnion, and umbilical cord.
Labor and Delivery
Stages of labor:
Dilation stage
Expulsion stage
Placental stage.
Premature labor can pose risks based on fetal development.
Neonatal Period
Post-birth phase characterized by significant physiological transitions as systems become functional independently.