Basic EKG and Dysrhythmias
Learning Objectives
Describe normal conduction pathway of electrical impulses through the heart.
Understand factors affecting the conduction systems function.
Differentiate parts of an EKG waveform.
Properly place a 5/6 lead ECG.
Calculate heart rate from an EKG strip.
Interpret ECG strips to identify principal heart rhythms and abnormalities (sinus, atrial, ectopic).
Recognize causes and clinical manifestations of cardiac rhythms.
Anticipate treatment strategies for rhythm abnormalities.
Normal Blood Flow in the Heart
Blood Flow Pathway:
Superior and Inferior Vena Cava → Right Atrium → Tricuspid Valve → Right Ventricle → Pulmonic Valve → Pulmonary Artery (deoxygenated) → Lungs (oxygenation) → Pulmonary Veins → Left Atrium → Mitral Valve → Left Ventricle → Aorta → Body and Coronary Arteries.
Pulmonary artery is only artery in body with deoxygenated blood.
Pulmonary veins only vein with oxygenated blood.
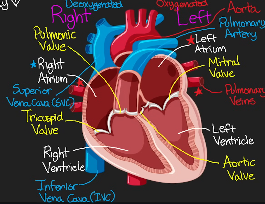
Color Coding:
Right side: Unoxygenated (blue)
Left side: Oxygenated (red)
Cardiac Cycle
Systole: Contraction phase of the heart.
Diastole: Relaxation phase of the heart.
Starling's Law of the Heart:
Involves how much blood is returning to the heart.
Strength of ventricular contraction increases with stretch (more stretch = stronger ventricle contraction because it’s filled with more blood). FRANK
Increased venous return raises filling pressure of the heart, leading to increased stroke volume. STARLING
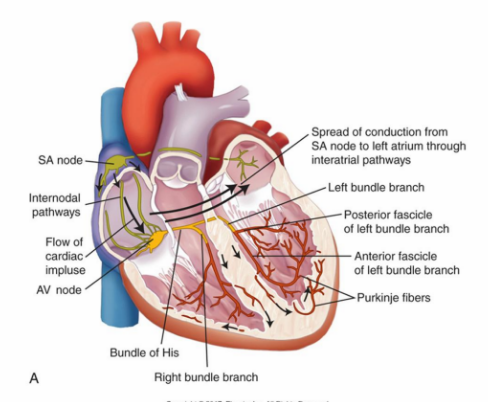
Conduction System ˚ʚ♡ɞ˚
˚ʚ♡ɞ˚ Components of the Heart Conduction System ˚ʚ♡ɞ˚:
SA Node (pacemaker): Initiates action potential with automaticity and depolarizes the atria, resulting in a contraction.
If SA node fails, other conduction cells such as the AV node will initiate an impulse.
Beats 60-100 BPM
AV Node: Relays signals from atria to ventricles for conduction.
Beats 40-60 BPM
Bundle of His: Conducts impulses through right and left ventricle branches.
Purkinje Fibers: Distribute electrical impulses throughout the ventricles, ensuring coordinated contraction and effective pumping of blood.
˚ʚ♡ɞ˚ Characteristics of Heart Cells ˚ʚ♡ɞ˚:
Automaticity: Ability to initiate an action potential (impulse) spontaneously and continuously.
All cells in the heart can generate an impulse (Impulse comes from SA)
Excitability: Respond to stimuli.
Conductivity: Transmit impulses.
A healthy heart has a predictable rhythm.
Contractility: Ability to contract and respond mechanically to impulse.
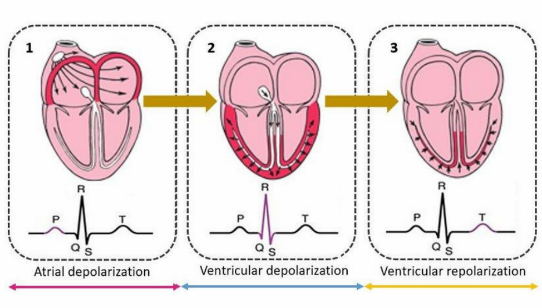
Action Potential and Repolarization
As the actional potential travels down the bundle of his and into the Purkinje fibers, it rapidly depolarizes the heart to cause contraction.
Atria depolarizes → atrial contraction while ventricles fill with blood → ventricles depolarize and contract → repolarization of heart cells.
Depolarization: Triggers contraction of the heart.
Repolarization: Cells return to resting polarized state.
Not immediate and takes a short period of time in two intervals known as refractory periods.
Refractory Periods (Repolarization):
Absolute Refractory: Unresponsive to stimulation.
Relative Refractory: Gradual regain of excitability.
If an electrical signal is received during this time → early heart beat.
Factors Affecting Conduction ˚ʚ♡ɞ˚
Autonomic Nervous System Control (automatic bodily functions): Influences heart rate via:
Sympathetic Nervous System: Increases SA node firing, increases AV conduction speed (positive dromotropic), and cardiac contractility rate and force (positive chronotropic & inotropic).
“Fight or Flight”
Drug Examples: Amphetamines (Adderall), vasopressors (epinephrine & norepinephrine).
Parasympathetic Nervous System (vagus nerve): Decreases SA node firing, slows AV conduction speed (negative dromotropic), heart rate slows down (negative chronotropic), and reduces cardiac contractility (negative inotropic).
“Rest and Digest”
Drug Examples: Beta blockers
Changes are:
Chronotropic: Rate of heart contraction. (Negative = slowed).
Inotropic: Force of heart contraction (Negative = slowed).
Dromotropic: Electrical conduction speed.
How quickly the atria and ventricle beat in comparison to each other / the interval between beats of atria and ventricle. (Positive = shorter interval)
EKG Breakdown ˚ʚ♡ɞ˚
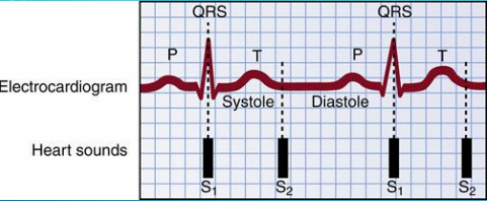
Wave Components: ˚ʚ♡ɞ˚
P-Wave: Atrial depolarization (atrial contraction).
QRS Complex: Ventricular depolarization (ventricles contract AKA systole 1).
Q: Negative downward after P.
R: First positive (upward) deflection.
S: Negative (downward) deflection after R.
Atrial repolarization happens during QRS/masked by ventricle contraction.
T-Wave: Ventricular repolarization/relaxation.
Diastole of ventricle as it relaxes.
U Wave (if present): Represents Purkinje fiber repolarization (systole 2 heard).
Sometimes seen with severe electrolyte abnormalities like hypokalemia.
Depolarization: Triggers contraction of the heart (electrical conduction).
Repolarization: Cells return to resting polarized state, awaiting next depolarization/contraction.
S1 = Tricuspid and mitral valves closing. “Lub”
S2 = Pulmonic and aortic valves closing. “Dub”
12 Lead ECG Details
12 Lead ECG: Most accurate; for acute cardiac events. Evaluates 12 angles of the heart on frontal and horizontal planes.
Only used if trying to analyze a problem in one go by getting a comprehensive view. Diagnostic measure (ex. Suspect MI, arrythmia, or if something bad is happening).
Patients need to be perfectly still otherwise artifact (unintended results from movement) can occur.
Electrode Placement Locations
V1: Right sternal edge, 4th ICS.
V2: Left sternal edge, 4th ICS.
V3: Between V2 and V4.
V4: Mid-clavicular line, 5th ICS.
V5: Between V4 and V6.
V6: Mid-axillary line, 5th ICS.
5 Lead ECG Placement ˚ʚ♡ɞ˚
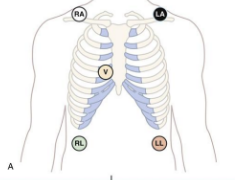
5/6 Lead ECG: For continuous monitoring (inpatient for cardiac or electrolyte abnormalities and severe illness & outpatient for event monitoring).
White on the right.
Grass under clouds (white).
Smoke (black) over fire (red).
Chocolate close to the heart (brown).
**If abnormalities are seen with the 5 lead, switch to the 12 lead. This will provide a more comprehensive view of the heart's electrical activity and help in diagnosing the specific type of dysrhythmia.
Reasons for 5/6 Lead:
Inpatient: Cardiac or electrolyte abnormalities (potassium, calcium, magnesium), or severe illnesses (DKA, PE, severe sepsis).
Outpatient: For event monitoring, measured by an external (Holter Monitor) or implantable heart monitor.
Ex. Pt keeps passing out and no idea why. An EKG is performed, not showing anything abnormal but the problem persists. Monitor will be worn while doing normal ADLs and it will record the syncopial episode.
Measuring Heart Rate from EKG ˚ʚ♡ɞ˚
Calculate heart rate using different methods:
Count QRS complexes in 6 seconds and multiply by 10 if irregular and 6-seocnd strip.
Count large squares on the R-R interval and divide into 300 if regular.
Pay attention to the lines at top to make sure it’s a 6 second strip. Lines 1-3 indicate a 6 second strip.

Normal ECG Measurements**
P-Wave: 0.06 to 0.12 seconds (atrial depolarization/contraction)
PR Interval: 0.12-0.20 seconds.
QRS Interval: <0.12 seconds (pulse/ventricle contraction).
Anything more may indicate a PVC.
ST Segment: 0.12 seconds.
T-Wave: 0.16 seconds.
QT Interval: 0.34-0.43 seconds.
**Each small box within big box is 0.04 seconds.
**The large box is equal to 0.20 seconds.
Application of Leads before ECG and During ˚ʚ♡ɞ˚
Ensure skin cleanliness (rub skin with dry gauze or clean skin with alcohol).
Ensure privacy and educate the patient.
Clip excessive hair (with permission).
Apply electrode pads carefully.
During ECG, keep the patient still to reduce motion artifacts.
Mainly for 12 leads.
Dysrhythmias
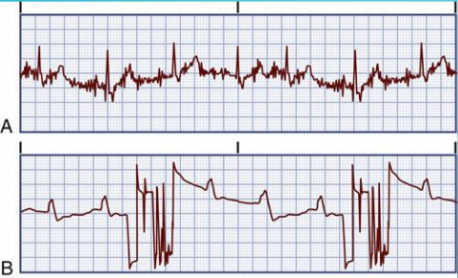
Definition: Any rhythm outside of normal sinus rhythm.
Not always concerning; may be artifacts (patient movement) triggering alarms.
Cellphones nearby or brushing teeth may cause artifact.
Sinus Rhythms ˚ʚ♡ɞ˚
Action Potential: Generated by the SA node.
Has all components (P, QRS, T)
Types Include:
Normal Sinus Rhythm (NSR)
Sinus Arrhythmia (SA)
Sinus Bradycardia (SB)
Sinus Tachycardia (ST).
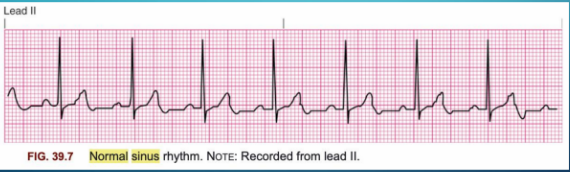
Normal Sinus Rhythm (NSR)
Indicates a normal heart function.
Characteristics: Normal-looking (Normal sinus)
P, QRS, and T waves (one normal P wave for every QRS)
P wave needs be upright and look normal for it to be NSR.
Regular rhythm (R-R intervals are consistent) and heart rate typically ranges from 60 to 100 beats per minute.
Difference between blood flow and conduction - they do not have to match
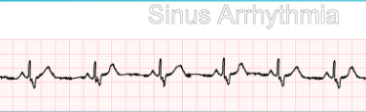
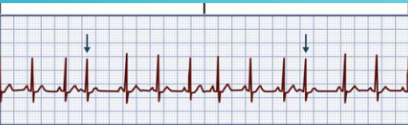
Sinus Arrhythmia
Clinical Manifestations: None; just irregular ECG (R-R interval distance varies).
Causes: Changes in thoracic (cavity) pressure during breathing.
Common in children and healthy/active adults.
Treatment: None required; sign of good health/normal.
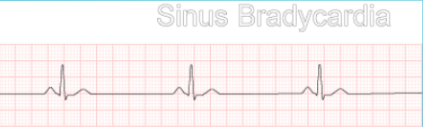
Sinus Bradycardia (slow)
Clinical Manifestations:
Hypotension (SV and CO decreased), pale/cool skin (lack of blood flow), weakness, angina, dizziness/syncope (lack of blood flow to brain), confusion, shortness of breath, tachypnea (increased respiratory rate to compensate reduced oxygen).
Characterized by slow conduction (<60 bpm) and P wave, QRS, T wave present. Increased space between complexes.
Treatment: Discontinue offending drugs, (ex. beta blockers), IV atropine to pick up rate (when symptomatic), pacemaker, dopamine and epinephrine infusions in ICU (increase contractility, HR, and CO).
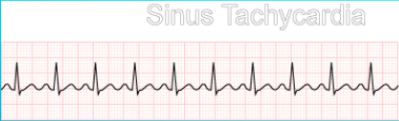
Sinus Tachycardia (fast)
Clinical Manifestations: Dizziness (lack of perfusion), dyspnea (trying to bring in more oxygen from lack of perfusion), hypotension (decreased CO), angina in patients with CAD (myocardium takes in more oxygen to compensate), palpitations.
Long-standing tachycardia causes decreased CO due to poor perfusion (heart unable to fill completely).
Characterized by rapid conduction (>100 bpm). P wave, QRS, T wave present. Closer R-R intervals.
Treatment: Guided by the cause (why the patient is experiencing tachycardia). Vagal maneuvers (stimulate the vagus nerve to slow a fast HR / have patient “bear down” or blow into an empty syringe), medications (B-blockers, calcium channel blockers) if symptomatic, synchronized cardioversion (shock delivered within normal conduction cycle of heart on R wave).
R wave is with depolarization of ventricles.
Ectopy ˚ʚ♡ɞ˚
Description: Action potential generated outside the SA or AV nodes (ectopic beats) AKA the heart beats too soon or heart “skips a beat.”
ECG Characteristics: Early contractions seen, abnormal P-wave if present; abnormal QRS may occur.
Types:
Premature Atrial Contractions (PACs) → All wave components still present from occurrence in atria.
Premature Ventricular Contractions (PVCs) → Skipping P wave (from skipping atria).
Premature Atrial Contraction (PAC)
Causes: Emotional stress, fatigue, caffeine, tobacco/alcohol (stimulates sympathetic nervous system), cardiac diseases (HF, CAD).
Clinical Manifestations: Palpitations (early heartbeats).
Characteristics: Abnormal early contractions in atria (ectopic focus) and P wave, QRS, and T wave present.
Treatment: Monitor until symptomatic, reduce stimulation, treat underlying conditions (ex. HF), B-blockers.
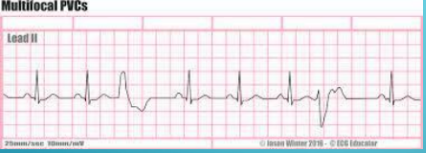
Premature Ventricular Contraction (PVC)
Causes: Emotional stress, caffeine, tobacco/alcohol (stimulates sympathetic nervous system), cardiac diseases (HF, CAD), electrolyte abnormalities (hyperkalemia).
Clinical Manifestations: Palpitations.
Treatment: Monitor, reduce sources of stimulation, treat underlying conditions, B-blockers.
Characteristics: Abnormal early contractions in ventricle (ectopic focus) with P wave, QRS, and T wave.
Unifocal (arising from or occurring in a single direction or location) or multifocal (arising in different directions like up and down).
Don’t count PVCs → watch on monitor and feel a pulse that correlates with the heart rhythm.
Atrial Rhythms ˚ʚ♡ɞ˚
Action potentials generated by atrial cells outside of the SA node; indicates abnormal heart function.
ECG Characteristics: Abnormal P-waves; may have multiple P-waves for each QRS.
Types:
PACs
Atrial Flutter
Atrial Fibrillation.
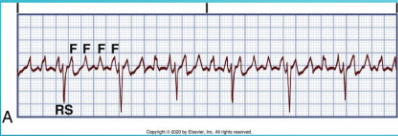
Atrial Flutter
Clinical Manifestations: Hypotension (‘atrial kick’ that pushes the rest of blood into ventricle no longer pushes enough blood into ventricle & lowers CO), palpitations, dyspnea, angina.
Characteristics: Multiple recurring P waves with a sawtooth shape (flutter waves) prior to QRS, regular rhythm → “regularly irregular”.
Single ectopic focus (atria).
Causes: HTN (uncontrolled), CAD/HF, PE (right-sided strain on heart, “cor pulmonale”), hyperthyroidism.
Treatment: CCBs, B-blockers, anticoagulants, antidysrhythmic meds.
Procedures: Synchronized cardioversion and ablation (looks for ectopic beat by entering through femoral artery to see where in atria the tissue is firing from → cauterize tissue to eliminate the source of the dysrhythmia).
Common Complication: Blood clots (atria not fully contracting → blood pools in atria).
ANTICOAGULANTS!
Atrial Fibrillation (AFib)
Clinical Manifestations: Hypotension, palpitations, dyspnea, angina.
Characteristics: Total disorganization of atrial electrical activity; fibrillary waves replace P waves.
Causes: Heart disease, thyrotoxicosis (excessive thyroid hormone), stimulants
Treatment: CCBs, B-blockers, anticoagulants (#1 treatment), cardioversion (shock at anytime), ablation.
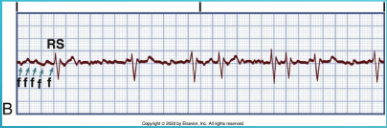
Treatment Modalities in Atrial Flutter/Atrial Fibrillation ˚ʚ♡ɞ˚
Electrical Cardioversion: Planned or emergent (electric shock to restore a normal heart rhythm, synchronized).
Make sure there is not a clot first in the atria → it can dislodge and travel through body.
Ablation: Targeting problematic areas, destroying heart tissue that causes abnormal heart rhythms.
Anticoagulation: Warfarin, NOACs to treat and prevent blood clots.
Left Atrial Appendage Ligation: A procedure that reduces the risk of stroke by closing off the left atrial appendage, where blood clots can form.
GENERAL TREATMENT NOTES: If patient is symptomatic, we go electricity. If not, we use medications.