Week 10: Labor and Delivery Methods
Overview of Labor and Delivery Process
Scenario Discussion:
Case Study: A client with a previous pregnancy history of an incompetent cervix underwent a cerclage procedure at 18 weeks. Now at 37 weeks, reports irregular contractions every 5-7 minutes.
Cerclage: a surgical procedure in which stitches are used to support the cervix, helping to prevent premature labor/miscarriage in women with a history of cervical insufficiency.
Nursing Response Options:
a. Advise going to the hospital to have cerclage removed to prevent cervical injury.
b. Suggest waiting until contractions are closer.
c. Acknowledge the client's anxiety for the baby.
d. Inform that a C-section is necessary while cerclage is in place.
Critical Thinking Application
Immediate Action Required:
The client should go to the hospital for evaluation.
Discussion Points:
Reasons for cerclage placement.
Patient discharge instructions to consider.
Patient education on signs/symptoms of preterm labor (PTL).
Preterm Labor (PTL)
Definition
Preterm Labor: Defined as uterine contractions and cervical changes occurring between 20 weeks and 36 weeks + 6 days of gestation.
Classification:
Moderately Preterm: 32-34 weeks.
Late Preterm/”Early Bird”: 34-36 weeks.
Complications for Pre-Term Labor:
Asthma risk due to respiratory structure and a lack of surfactant.
Cardiac issues may arise, including an increased likelihood of congenital heart defects and other cardiovascular complications.
Neurological risk of cerebral palsy.
Preterm infants may face gastrointestinal problems, such as necrotizing enterocolitis, which can lead to serious infections and complications.
Failure to thrive/sepsis risk.
Patient Education: When to Contact Healthcare Provider (HCP)
Acronym: PROM/PPROM.
Assessment Required if Water Breaks (COAT):
Color
Should be clear.
Brown or green: sign of meconium.
The child may be at an aspiration risk.
Odor
Should smell clean or bleachy.
If odorous, it can be a sign of infection.
Amount
A liter.
Time
Within 24 hours of breakage, you want to see the baby, or else the infant and mother are at risk of infection.
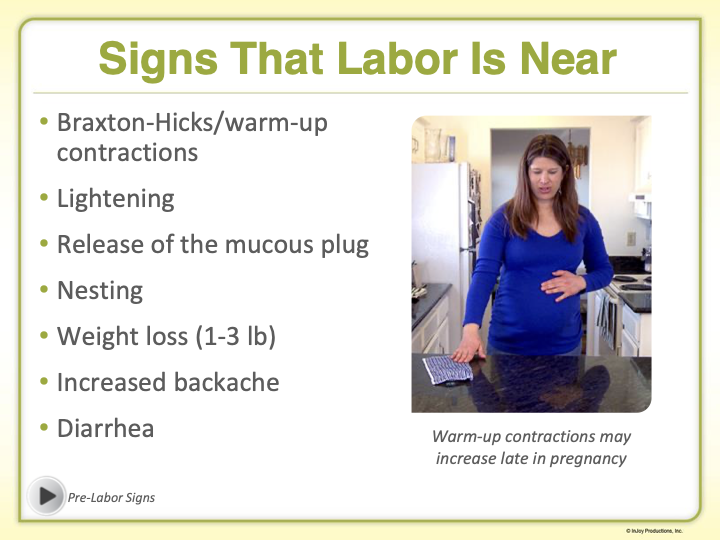
Symptoms of Concern:
Change or increase in vaginal discharge.
Pelvic or lower abdominal pressure.
Constant low-back pain.
Mild cramping.
Gush or trickling of water.
More than 4 contractions in 1 hour.
Important Note: Signs of infection must be considered!
Risk Factors for Preterm Labor
Common Risk Factors:
Infections (UTI, HIV, active HSV/herpes, chorioamnionitis).
Previous preterm births.
Multifetal pregnancies.
Substance use (smoking, drugs).
History of abuse.
More prone to domestic abuse.
Lack of prenatal care.
Uterine abnormalities.
Low pre-pregnancy weight.
Medications Used for Preterm Labor
Medication Administration Principle: The 5 Rights - Right Patient, Drug, Dose, Route, Time.
Medications Include:
Nifedipine: A Calcium channel blocker that suppresses contractions by inhibiting calcium from entering smooth muscle.
Caution: Do not administer with magnesium sulfate or beta-adrenergic agonists.
Magnesium Sulfate: A commonly used tocolytic that depresses the central nervous system (CNS) and relaxes smooth muscle to inhibit uterine activity.
Important Note: Antidote is 10% Calcium Gluconate.
Also used for preclampsia.
Terbutaline: A beta-adrenergic agonist that relaxes smooth muscle and inhibits uterine activity (“Turbulence delays arrival time”).
Dosage Information: 0.25 SQ.
Monitoring: Observe cardiac output.
Indomethacin: NSAID that suppresses preterm labor by blocking prostaglandin production, particularly effective under 32 weeks of gestation.
Enhances fetal-lung maturity.
Betamethasone: Glucocorticoid administered IM in two injections 24 hours apart; enhances fetal lung maturity.
Labor and Delivery Processes
Intrapartum Nursing Care
Key Clients:
The fetus
The birthing parent
The family unit
Understanding Labor Pain
Labor Pain Characteristics:
Purposeful: Has a reason related to childbirth.
Anticipated: Expected during the birthing process.
Intermittent: Occurs in patterns rather than continuously.
Normal: Common part of childbirth.
Pain Locations During Labor
Stages of Pain:
Early labor stage pain can vary in intensity and location.
Radiating from the back to the hips.
The delivery stage involves somatic and visceral pain.
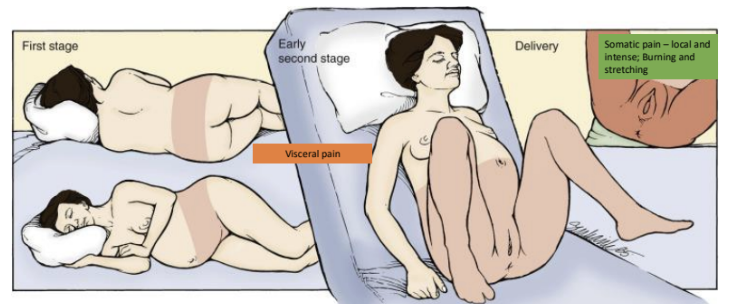
Releases endorphin when experiencing pain.
Psychological Responses: Fear-Tension-Pain Cycle
Cycle Description:
Fear results in tension.
The body won’t relax enough to deliver, thus creating more pain.
Comforting environments and support aid in labor delivery, increasing oxytocin levels, which help with uterine contractions and promote a more effective birthing process.
Tension can amplify pain perception.
Tension in areas (jaw, pelvic floor, legs) reduces oxygen to the uterus, thus affecting labor.
The Gate Control Theory of Pain
Theory Explanation:
Other sensations can block pain sensations from reaching the brain, suggesting that pleasure or various stimuli can alleviate pain during labor.
Warm compressions, rice sock, or cold wash clothes on pressure points.
The 5 P's of Labor
Overview
Essential Components:
Passageway
Passenger
Powers
Position
Psyche
5 P's Detailed
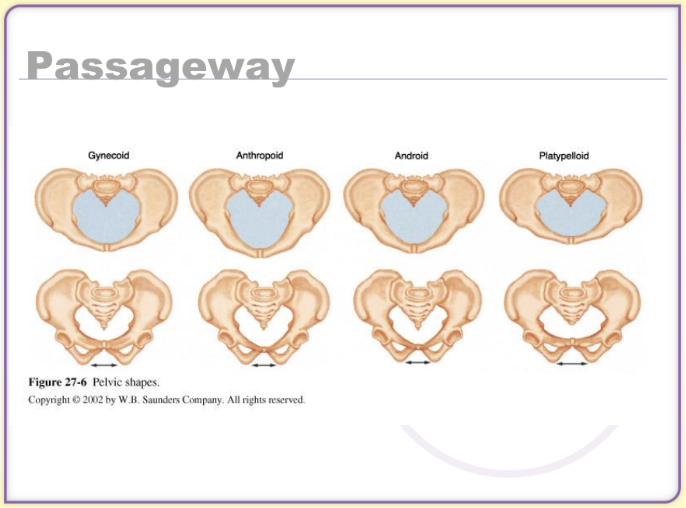
Passageway: Refers to the pelvis (the “birth canal”), the main passage for birth.
Negative movement means they're moving down the canal.
Zero at the inlit.
Positive movement when exiting mom, +4 hit the floor!
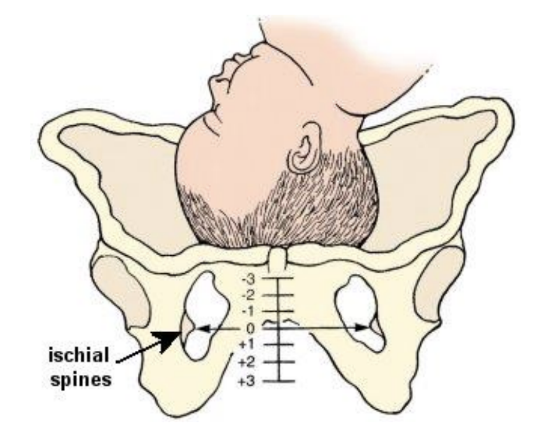
Arrest of labor/sephlow pelvis disproportion may result in the mom needing a C-section due to the inability to deliver it through the canal.
The gyneoid shape of the pelvis is PERFECT for delivery (seen in 51% of women).
Passenger: Concerns the fetus, the baby traveling through the passageway.
Presentation: The part of the fetus entering the pelvic inlet first.

Fetal Lie: Orientation of the fetus to the maternal spine (longitudinal or transverse).
Breech: When the buttocks or feet of the fetus present first at the pelvic inlet, this may complicate the delivery process and often necessitates special care or interventions (C-section delivery to lower the risk).
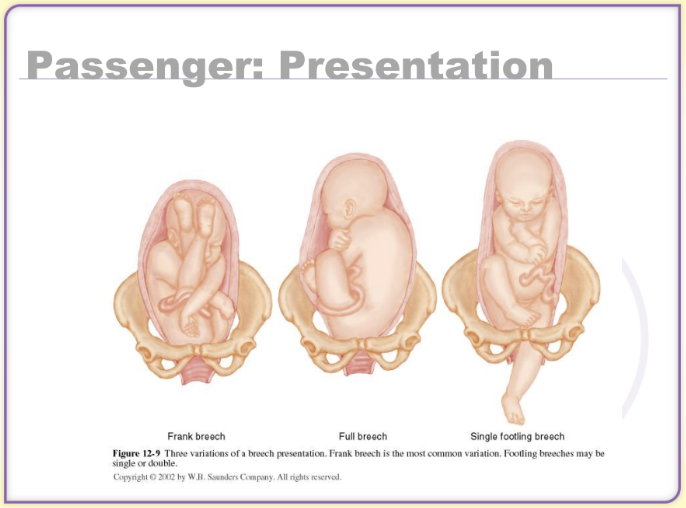
Transverse: When the fetus is positioned horizontally across the uterus, which can hinder the progress of labor and typically requires medical intervention to facilitate a safe delivery (C-section delivery to lower the risk).
Vertex: This is the most common presentation, where the fetus is positioned head down, allowing for a more straightforward delivery process.
Complete flexion: ideal, chin to the chest.
Moderate flexion
Poor flexion: head is backwards
Hyperextension: more difficult delivery.
Occipital Posterior: In this position, the fetus is facing the mother's abdomen, which can lead to a longer labor and increased discomfort for the mother; assistance may be required to help reposition the baby or facilitate delivery.
Causes back pain, have the client lean against a wall or partner during contractions to alleviate some pressure and provide support.
During delivery, give the mother a ball or have her on all 4s.
Powers: Refers to uterine contractions, the driving force of labor.
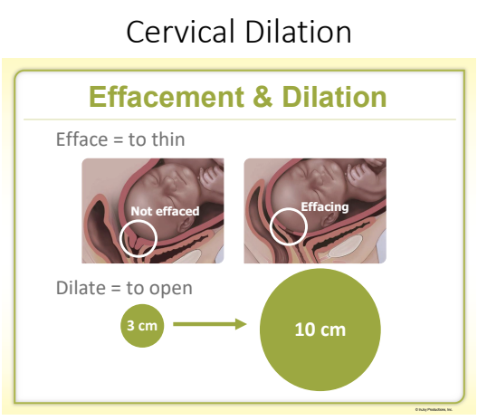
Effacement: The thinning and shortening of the cervix during labor, which allows it to open and facilitates the descent of the baby.
Dilation: The process in which the cervix opens to allow the baby to pass through the birth canal, measured in centimeters from 0 to 10.
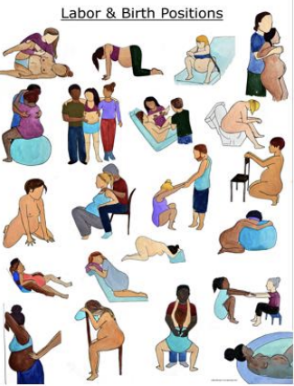
Position: Maternal positioning that enhances gravity and aids fetal descent.
Hand and knees: helps with back pain.
Movement: helps with pain, swaying, rocking, and helps to relaxes.
Contraindicated if the client has an epidural.
Psyche: Psychological readiness, including maternal stress and support factors.
Water immersion: Provides buoyancy and can ease labor discomfort, promoting relaxation and a sense of privacy.
Doula: A trained professional who provides continuous physical, emotional, and informational support to the mother before, during, and shortly after childbirth, helping to enhance the birth experience.
The body is making room and space for the baby to deliver.
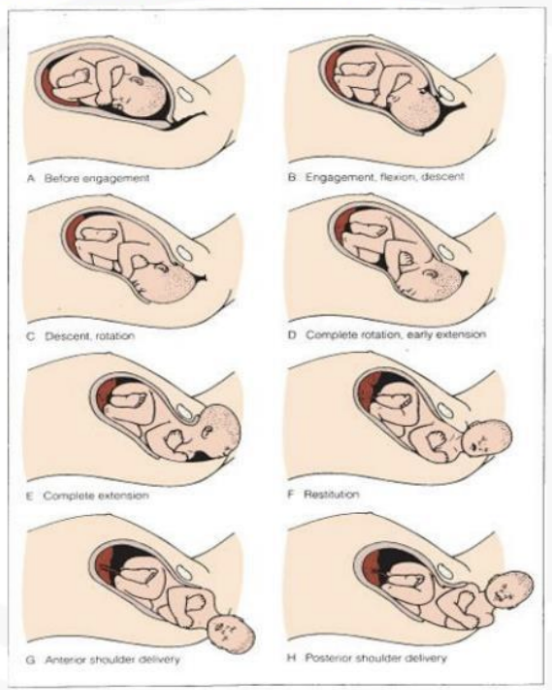
Cardinal Movements of Labor
Overview
Movements During Labor:
Engagement
Descent
Flexion
Internal Rotation
Extension
External Rotation
Expulsion
Done to adapt to the pelvis for delivery.
Descriptions of Each Movement
Engagement: Fetal head passes through the pelvic inlet.
Descent: Fetus moving down within the pelvis.
Flexion: Chin to chest to allow easier passage through the pelvis.
Internal Rotation: The presenting part rotates to align with the maternal pelvis.
Done to move against mom’s back.
Extension: The fetal head emerges from the vagina.
External Rotation: The fetal head rotates to align with the shoulders after delivery.
When the head reaches the perineum.
Expulsion: Delivery of the rest of the body post-head delivery.
Shoulder slips under the pelvic bone.
Uterine Contractions
Characteristics
Components of Contractions:
Increment, Peak (Acme), Intensity, Duration, Decrement, Interval (rest period), Frequency
5 contractions, which are 1 minute, have occurred within an hour.
Cervical Effacement and Dilation
Effacement: Thinning of the cervix expressed as a percentage (0 to 100%).
Dilation: Opening of the cervix measured in centimeters (0 to 10 cm).
Labor Stages
Stages Overview
Stage One: Cervical thinning and dilation.
Stage Two: Pushing and birth.
Stage Three: Delivery of the placenta.
Stage Four: Recovery and breastfeeding.
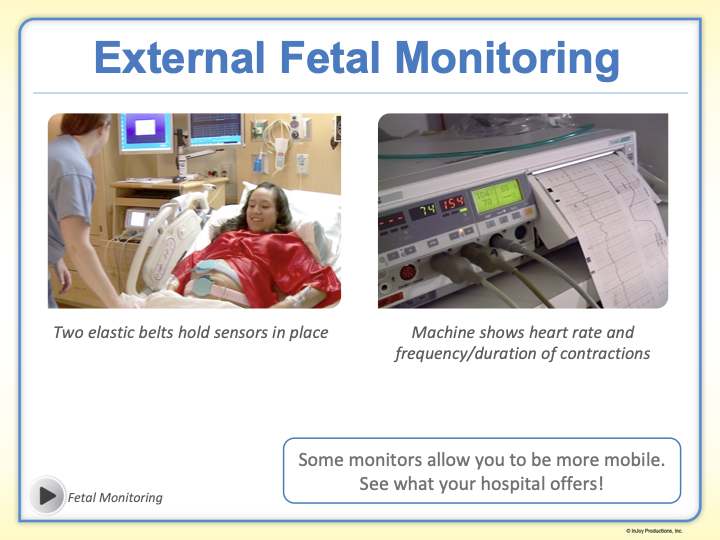
External Fetal Monitor use during labor: This device allows healthcare providers to continuously assess the fetal heart rate and the strength of contractions, ensuring the baby's well-being during the labor process.
Determines the position and presentation of the baby.
Goal: To ensure that both the mother and baby remain stable throughout labor and to identify any potential complications early on.
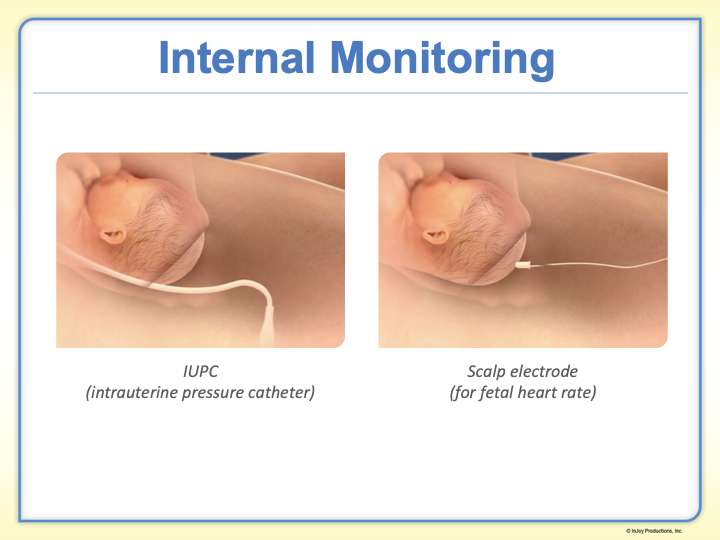
Internal Fetal Monitor use during labor: This device provides a more accurate and direct measurement of the fetal heart rate and uterine contractions by being attached to the baby's scalp, which can be helpful when external monitoring is inadequate.
It is typically indicated for high-risk pregnancies where closer monitoring is necessary to ensure the safety of both mother and child.
Mom has to be at least 2 cm dilated, and their water bag has to be broken.
Active Labor Description
Stages of Active Labor:
Latent (Early) Labor: Lasts up to 12 hours with contractions 30-60 seconds apart. Begins effacement and dilation. Expected signs include mucous discharge and potential water break.
Dilation: 0-6 cm.
Tips: Stay at home, rest, take a short walk, or do light activities.
Contractions: 30-45 seconds each, 5-30 minutes apart.
Active Labor: Lasts about 6 hours; contractions become stronger and more frequent. Dilation progresses up to 8 cm.
Dilation: 6-8 cm.
Tips: Actively try getting to the hospital, use different positions, breathing exercises, and relaxation techniques.
Contractions: 45-60 seconds each, 3-5 minutes apart.
Transition Stage: Lasts a few minutes to hours, the most intense phase, contractions are very strong. Dilation reaches 10 cm.
Dilation: 8-10 cm.
Tips: May feel nauseous or shaky, support people needed to provide focus.
Contractions: 60-90 seconds each, 3-5 minutes apart.
Pain Management During Labor
Non-Pharmacological Techniques
Techniques:
Sensory stimulation (aroma, music, lighting).
Cutaneous strategies (massage, position changes).
Continuous labor support.
Hydrotherapy (showering) and ambulation.
Focused breathing techniques.
Effleurage is a circular massage for the abdomen.
Pharmacological Pain Relief
Pain Management Options
Medications Include:
Sedatives for early labor (ex, barbiturates).
Opioids administered via IV or IM (ex, fentanyl).
Regional anesthesia options (epidural and spinal analgesia).
Types of analgesics administered must be monitored for fetal safety.
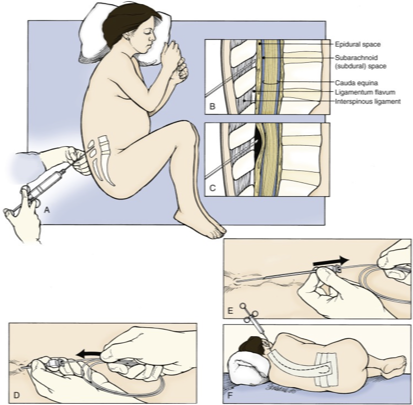
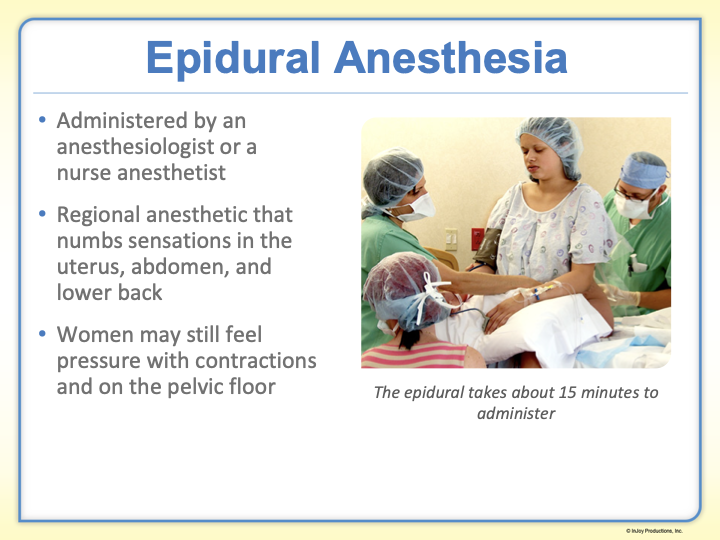
Epidural Anesthesia
Epidural Instructions:
Informed consent needed.
Education: Maternal hypotension is the biggest concern!!
Monitor for maternal vital signs and fetal heart rate frequently throughout the procedure to ensure safety and prompt intervention if necessary.
Other side effects: Loss of spinal fluid can cause headache, N/V, itching, and high block (can’t breathe).
Assess fetal heart rate before administration.
Empty the bladder.
Administration by an anesthesiologist or nurse anesthetist.
Positions must be held for effective placement.
General Anesthesia
Use Guidelines:
Reserved for emergencies due to significant risks, including respiratory depression in the neonate.
Essential preparations involve antacid administration and rapid delivery protocols to minimize fetal exposure.
Conclusion
Goal: To achieve a happy, healthy birth parent and baby!