Hematological Problems - In Depth Notes
Anatomy and Physiology Review
Review videos in the Pre-Class Lecture Checklist, which cover important aspects of the hematologic system:
Anatomy of the Hematologic System: Focus on the structures involved, including the bone marrow, spleen, and lymphatic tissues, which play critical roles in blood production and immune responses.
Blood Components: Characterize the functions of plasma, red blood cells (RBCs), leukocytes (white blood cells), and platelets in maintaining homeostasis and responding to injury.
Blood Clotting Mechanisms: Understand the physiological processes that initiate and regulate blood clot formation, including the roles of various clotting factors.
Hemostasis: Review mechanisms of control for bleeding, coagulation processes, and thrombosis to grasp how the body maintains vascular integrity during injury.
Hematologic Changes Associated with Aging
Notable changes in hematologic function include:
A decrease in overall blood volume and a reduction in plasma protein levels can impact hemostatic balance in older adults.
Reduced efficiency of bone marrow leads to fewer blood cells being produced, increasing the risk for anemia and other blood-related disorders.
A documented decrease in both RBC and WBC counts can elevate the risk for infections due to compromised immune function.
There is often a reduction in hemoglobin levels noticed after middle age, which requires monitoring in patient care, especially in the geriatric population.
Patient History Assessment Components
Essential demographics include age, gender, and other relevant personal factors.
Women have a lower RBC count than do men. This difference is greater during menstrual yrs because menstrual blood loss may occur faster than blood cell production. This difference is also related to blood dilution caused by fluid retention from female hormones. Always assess for RBC adequacy in women hospitalized for any reason.
Thorough health history assessments should inquire about:
Liver function: The liver is important in producing clotting factors. Ask about symptoms that may indicate liver problems, such as jaundice, anemia, and gallstones.
Occupation and hobbies: Identifying possible exposures to harmful substances or lifestyle factors affecting hematologic health.
Drug use and nutritional status: including dietary habits that may influence blood health and any substances that may interact with medications.
Vitamin K, can be found in leafy green veggie, may increase the rate of blood.
ask about alcohol consumption because chronic alcoholism causes nutritional deficiencies and impairs the liver, both of which reduce blood clotting
Social support and family medical history: Understanding the environment surrounding the patient and hereditary factors relevant to hematological conditions.
Identify current health problems related to hematologic status, which may provide insight into underlying conditions or complications.
Most common symptom of anemia is fatigue as a result of decreased oxygen delivery to cells
Common Drug Classes Affecting the Hematologic System
Bone Marrow Suppressants such as Ganciclovir and Zidovudine inhibit bone marrow function, often leading to decreased blood cell production.
Hemolysis Agents like amoxicillin, penicillin G, benzathine, penicillin V, vitamin K, and Glyburide can trigger destruction of red blood cells, resulting in anemia.
Platelet Action Disruptors, including Aspirin, ibuprofen, meloxicam (mobic), naproxen (aleve), and Valproic Acid affect platelet aggregation which can increase the risk for bleeding complications.
Clinical Assessment Findings
Key signs include:
Petechiae: Tiny red or purple spots indicating small bleedings – <3 mm in size.
visible only on the palms of the hands, the soles of the feet, the oral mucous membranes, and the conjunctiva.
Ecchymosis: Larger bruises, typically measuring >10 mm, indicate larger areas of bleeding under the skin.
Purpura: Intermediate in size between petechiae and ecchymosis, representing a more significant bleeding issue.
A red, beefy tongue can indicate a Vitamin B12 deficiency, emphasizing the need for dietary assessment.
Signs of oxygen deprivation should include condition indicators such as cyanosis and shortness of breath, linking these signs to potential hematologic or cardiovascular issues.
Physical assessment findings
skin: for pallor or jaundice, assess nail beds for pallor or cyanosis. Assess body hair patterns, areas with poor circulation, especially the lower legs and toes, may have sparse or absent hair, although this may be a normal finding in older adults.
head and neck: the tongue is smooth in pernicious anemia and iron deficiency anemia or smooth and beefy red in (b12 deficiency.
respiratory: Assess RR and depth while at rest and during physical activity.
cardiovascular: pulses become weaker and thready. Observe for distended neck veins, edema, or indications of phlebitis, assess BP
kidney and urinary: test urine for protein, inspect urine for blood (hematuria)
musculoskeletal:
abdominal: a palpable spleen is usually due to enlargement (don’t palpate can rupture easily,y which can lead to hemorrhage and death)
CNS:
psychosocial
Hematologic Assessment, Normal Ranges, and Key Indicators
Red Blood Cell Count normals include:
Females:
Males:
A decrease suggests anemia or hemorrhage, while an increase may indicate chronic hypoxia or conditions such as polycythemia vera.
Hemoglobin (Hgb) levels are typically:
Females: 12-16 g/dl
Males: 14-18 g/dl
Decreased Hgb levels often indicate potential anemia etiology.
Hematocrit (Hct) normals are as follows:
Females: 37%-47%
Males: 42%-52%
It can be calculated by multiplying Hgb levels by 3,
WBC: 5000-10000
reticulocyte count: 0.5 % - 2.0% of RBCs
increased levels: possible chronic blood loss or recovery from anemia
decreased levels: possible inadequate RBC production
Iron (Fe)
females: 60 - 160 mcg/dl
males: 80-180 mcg/dl
increased levels: iron excess, liver disorders, hemochromatosis, megaloblastic anemia
Decreased levels: possible iron deficiency anemia, hemorrhage.
platelet count: 150,000–400,000/mm
hemoglobin electrophoresis: lab tests to help detect sickle cell disease
Hgb A1: 95% - 98%
HbA2: 2%-3%
HbF: 0.8 % - 2%
Hgb S: 0%
Hgb C: 0%
Hgb E: 0%
lab test to determine antibodies against RBCs and circulatory antiglobulin
INR: 0.8-1.1 times the control value
increased value: longer clotting times ( desirable for Warfarin therapy)
decreased values: hypercoagulation and increased risk for VTE
PT: 11-12.5 sec
decreased time may indicate vitamin K excess
Bone Marrow Aspiration and Biopsy
evaluate the pt’s hematologic status, results provide information about bone marrow function, including the production of all blood cells and platelets.
pre-op
provide accurate information and emotional support
explain procedure
follow-up care
teach to inspect the site every 2 hrs for 24 hrs, avoid activity that could result in trauma
analgesics (aspirin-free) and ice packs.
Sickle Cell Disease: Overview
An inherited genetic disorder affecting hemoglobin structure.
autosomal recessive pattern of inheritance
It causes red blood cells to sickle, which leads to blocked blood vessels and results in hypoxia in tissues.
the clumps block blood flow; tissues become hypoxic
Characterized by severe pain during vaso-occlusive crises due to disruption in blood flow and subsequent tissue ischemia.
The prevalence is notably high in African Americans, with statistics showing 1 in 500 individuals affected. Expected life expectancy averages around 42 years for men and 48 years for women, contingent upon management and advancements in healthcare.
History
assess for previous crises, severity, and usual management
ask about changes to sleep and rest patterns, ability to climb stairs, any activity that induces SOB
physiological/psychosocial
vaso-occlusive crisis
Pain is the most common symptom of SCD crisis
pain due to poor tissue perfusion and joint destruction with low oxygen levels
fatigue
potential for infection, sepsis, multiple organ dysfunction syndrome (MODS), and death
Physical assessment/ signs and symptoms
cardiovascular
high-output HF, murmurs, S3 heart sounds, JVD, reduced perfusion (note pulses)
respiratory
pulmonary hypertension, recurrent pneumonia,
acute chest syndrome is a common reason for hospitalization and is the most common cause of death.
life-threatening condition usually associated with respiratory infection and can also be caused by fat embolism and debris from sickled cells
S/S are similar to pneumonia with cough, SOB, abnormal breath sounds, and infiltrate on chest x-ray.
Priapism
prolonged penile erection (can cause pt inability to urinate
Eyes
visual deficits
Abdominal
sleen, liver, gallbladder
skin changes
pallor or cyanosis due to poor gas exchange
Jaundice results from RBC destruction and the release of bilirubin
ulcers due to poor perfusion
usually located on the lower legs (outer sides and inner aspect of the ankle or shin. These can become necrotic or infected.
Abdominal changes
The liver and spleen may feel firm and enlarged with a nodular or “lumpy” texture in later stages of the disease.
Kidney and Urinary Changes
Chronic kidney disease (CKD) makes the kidney less effective at filtration and reabsorption
The urine contains protein, and the pt may not concentrate urine, which eventually leads to the kidneys failing
Musculoskeletal
Arms and legs are often sites of blood vessel occlusion
joints may be damaged from hypoxic episodes and have necrotic degeneration
inspect the arms and legs and record any areas of swelling, temp, or color difference. ask pt to move all joints
Dactylitis (swelling of the hands and feet)
CNS
long-term effect can lead to infarcts with repeated episodes of hypoxia, causing the pt to have seizures or symptoms of a stroke
assess for the presence of “pronator drift”, bilateral hand grasp strength, gait, and coordination
Sickle cell disease: Diagnostics
lab assessment
percentage of HbS on electrophoresis (80% to 100%)
Hematocrit is usually low during crisis (between 20% and 30%)
high reticulocyte count, indicating anemia of long duration
WBC high because of the chronic inflammation caused by tissue hypoxia and ischmia
Imaging assessment
X-rays, CT, PET, MRI
x-ray: the skull may show changes ( crew cut appearance)
ECG indicating cardiac infarcts and tissue damage
Echocardiograms may show cardiomyopathy and decreased cardiac output (low ejection fraction)
Sickle Cell Disease: Management Strategies
managing pain
acute pain episode has a sudden onset, usually involving the chest, back, abdomen, and extremities
goal: pain controlled to a level acceptable to the pt
drug therapy
morphine and hydromorphone are given IV on a routine schedule or PCA, and tapered once relief is obtained
Moderate pain may be managed with oral doses of opioids or NSAIDs.
Hydroxyurea may reduce the number of sickling and pain episodes by stimulating fetal hemoglobin (HbF) production, which is the main type present during fetal life. (This drug increases the risk for leukemia)
the drug is a teratgen (agent that can increase cause of birth defects). teach sexully active women of childbearing age to adhere to strict contraceptive measures while taking it and for 1 month after it is discontinued.
Hydration, by oral or IV route helps reduce the duration of pain episodes
pt are usually dehydrated and there blood is hypertonic, hypotonic fluids are usually infused at 250 mL/hr for 4 hrs. once pt’s blood osmolarity is reduced to a normal range of 270 to 300 mOsm, rate is reduced to 125 ml/hr
Integrative therapies
keeping the room warm, using distraction and relaxation techniques, positioning with support for painful areas, aromatherapy, therapeutic touch, warm soaks or compresses all help reduce pain perception.
prevent sepsis, MODs, and death
prevention and early detection
Frequent, handwashing is especially important. any person with an upper respiratory tract infection who enters the pt’s room must wear a mask. Strict aseptic technique is used for all invasive procedures
hydration (stop clumping of RBCs)
the pt in acute crisis needs an oral or IV fluid intake of at least 200 mL/hr
oxygen given during crises because lack of O2 is the main cause of sickling
Nebulized therapy to prevent dehydration
If saturation is low, evaluation of ABGs and chest x-ray may be needed
transfusion with RBCs can be helpful to increase HbA levels and dilute HbS levels
Care of the Pt in sickle cell crisis
administer O2
adminster prescribed pain meds
hydrate pt with normal saline IV and with beverages of choice (without caffeine)
remove any constrictive clothing
encourage pt to keep extremities extended to promote venous return
don’t raise the knee position of the bed
elevate the HOB no more than 30 degrees
keep room temp at or above 72 F(22.2 C)
avoid taking BP with a standard or automatic external arm cuff
check circulation in extremities every hour
pulse ox of fingers and toes
peripheral pulses
cap refils
Prevention of Sickle Cell Crisis
drink at least 3 to 4L of liquids every day
avoid alcoholic beverages
avoid smoking cigarettes or using tobacco or nicotine in any form
contact PHP at 1st sign of illness of infection
be sure to get a “flu shot” every year
ask your PHCP about receiving the pneumonia vaccine
avoid hot or cold temps extremes
be sure to wear socks and gloves when going outside on cold days
avoid airplanes with unpressurized passenger cabins
avoid travel to areas at high altitudes (denver, flagstaff, santa fe, lake louise)
be sure all your health care providers know that you have sickle cell disease, especially the anesthesia provider and radiologist.
consider genetic counseling before becoming sexually active
avoid strenous physical exercise
when not in crisis, perform mild, low-impact exercise 3 times a wk.
Sickle Cell Disease: Evaluation/Outcomes
report pain to be maintained at an acceptable level
maintain perfusion and gas exchange to extremities and vital organs
remain free of infection, sepsis, and multiple organ dysfunction syndrome (MODs)
pregnancy in women with SCD may be life-threatening. barrier methods of contraception ( cervial cap, diaphragm, or condoms with or without spermicides) are often recommended for women with SCD.
the use of progestin-only hormonal contraception is recommended to reduce the risk for VTEs.
Anemia: Overview
anemia is a reduction in the number of RBCs, the amount of H&H
for men Hgb less than 13.5g/dl)
for women with levels less than 12.0g/dl)
blood loss
insufficient RBC production
excess destruction of RBCs
deficiency of necessary components (iron, folic acid, vitamin B12, erythropoietin)
clinical indicator (not specific disease); occurs with many health problems
Sickle cell anemia
autosomal-recessive inheritance of 2 defective gene alleles for hemoglobin synthesis
glucose-6-phosphate dehydration (G6PD) deficiency
x-linked recessive deficiency of the enzyme G6PD
autoimmune hemolytic anemia
abnormal immune function in which a person’s immune reactive cells fail to recognize his or her own RBCs as self-cells
Vitamin B12 deficiency anemia
dietary deficiency
Failure to absorb vitamin B12 from the intestinal tract as a result of
partial gastroectomy
pernicious anemia
malabsorption syndromes
Folic Acid Deficiney anemia
dietary deficiency
malabsorbtion syndrome
drugs:
oral contraceptives
anticonvulsants
methotrexate
aplastic anemia
exposure to myelotoxic agents
radiation
benzene
chloramphenicol
alkylatine agents
antimetabolites
sulfonamides
insecticides
viral infection
Epstein-Barr virus
hep B
cytomegalovirus
Anemia: Physical Assessment/ Signs and Symptoms
Skin S/S
general pallor (more noticeable on the ears, nailbeds, palm creases, and around the mouth)
cool to the touch
pt doesn’t tolerate cooler temps
when chronic, nails become brittle and concave
Cardiovascular S/S
continuous rapid heartbeat that increases after meals and with activity
With severe anemia, abnormal heart sounds (murmurs and gallops) may be heard
orthostatic hypotension
Respiratory S/S
breathless in exertion
decreased oxygen sat levels
Neurologic S/S
fatigue
increased need for sleep
reduced energy levels
Vitamin B12 deficiency anemia specific S/S
pallor and jaundice
glossitis: a smooth, beefy-red tongue
older pt often have poor diets or chewing difficulties which puts them at risk for anemias. B12 deficiency anemia often occurs in pt 50 to 80 yrs of age
fatigue and weight loss
paresthesias (abnormal nerve sensations) in the feet and hands and poor balance,e because Vitamin B12 helps maintain nerve function
Anemia: Interventions
iron deficiency anemia
Increase oral intake of iron
ex: red meat, egg yolks, organ meats, kidney beans, leafy green vegetables, raisins
iron supplements (ferrous Sulfate)
vitamin B12 definciney anemia (pernicioud anemia)
increase intake of foods rich B12
Ex: animal proteins, fish, eggs, nuts, dairy products, dried beans, citrus fruits, and leafy green veggie
injections, oral preparations, nasal spray, sublingual cobalamin
folic acid deficiency anemia
Prevent deficiency with a diet rich in folic acid and vitamin B12
aplastic anemia
dependent upon the cause
blood transfusions
immunosuppressive therapy
G6PD Anemia
test those at high risk
hydration
osmotic diurectics
transfusions
Autoimmune hemolytic anemia
Immunotheraphy
splenectomy
immunosuppressive therapy with chemotherapy
Polycythemia Vera
PV is one of the chronic myeloproliferative neoplasms (MPNs) in which there is loss of cellular regulation with excessive expansion of specific groups of abnormal myeloid cells with decreased function
cancer of the RBCs
massive production of RBCs
excessive leukocyte production
excessive platelet production
Polycythemia Vera: Assessment Findings
facial skin and mucous membranes are dark purple or cyanotic, flushed (plethoric) appearance with distended veins
intense itching
vascular status causes thrombosis (clot formation) within the smaller vessels, occluding them, which interferes with perfusion and leads to tissue hypoxia, anoxia, later infarction and necrosis
poor gas exchange with severe hypoxia
bleeding problems are common because of platelet impairment with poor clotting
PV: interventions
fatal if untreated
Apheresis: is the withdrawal of whole blood and removal of some of the pt’s blood components, in this case RBCs. The plasma is then reinfused back into the pt
increase hydration
promote venous return help prevent clot formation
drug therapy
anticoagulants
aspirin
hydroxyurea
Self-management of PV
drink at least 3L of liquids each day
avoid tight or constrictive clothing, especially garters and girdles
wear gloves when outdoors in temp lower than 50 F (10 C)
keep all health care-related appointments
contact your PHCP at the 1st sign of infection
take anticoagulants as prescribed
wear support hose or stockings while you are awake and up
elevate your feet whenever you are seated
exercise slowly and only on the advice of provider
stop activity at 1st sign of chest pain
use electric shaver
use soft-bristle toothbrush to brush your teeth
don’t floss between your teeth
smoking cessation
Leukemia and Preleukemia
pathophysiology Overview
blood cancer that results from a loss of normal cellular regulation, leading to uncontrolled production of immature WBCs (“blast” cells) in the bone marrow
This overproduction prevents the growth of RBCs, platelets and normal WBC
Acute: acute myelogenous leukemia (AML) and acute Lymphocytic leukemia (ALL)
immature, nonfunctioning WBCs, abrupt and common in kids
Chronic: chronic myelogenous leukemia (CML) and chronic Lymphocytic leukemia (CLL)
mature cells with reduced function, slow onset of years, are common in older adults
Common Medical Terms to Know
Thrombocytopenia: reduced circulating platelet numbers
Leukopenia: reduced circulating WBC numbers
Leukemia
Etiology and Genetic Risk
genetic and environmental factors
damage to genes that control cell growth
risk factors
ionizing radiation
viral infection
exposure to chemicals and drugs
History
ask about risk and genetic factors
occupation, hobbies, medical history, exposure
history of infections, bleeding or bruising, weakness, fatigue
colds, influenza, pneumonia, bronchitis, or unexplained fevers, during the past 6 months
note S/S of excessive bleeding
Note S/S specific to weakness and fatigue from anemia
Leukemia Assessment Findings
Integumentary
ecchymoses
petechiae
open infected lesions
pallor of the conjunctivae, the nail beds, the palmar creases, and around the mouth
GI
anorexia
bleeding gums
weight loss
enlarged liver and spleen
Renal
hematuria
Musculoskeletal
bone pain
joint swelling and pain
Cardiopulmonary
tachycardia at basal activity levels
orthostatic hypotension
palpitations
Dyspnea on exertion
Neurologic
fatigue
headache
fever
psychosocial assessment
anxiety, fear, lifestyle changes, off work for treatment
Laboratory assessment
low H&H
normal Hgb: women 12-16/Men 13-18
normal Hct: women 36-48/men 39-54
Low platelets
normal: 150,000-400,000
abnormal WBC count (usually elevated)
normal: 5000-10000
bone marrow aspiration and biopsy is the definitive test
blood clotting times and factors are usually abnormal, and whole-blood clotting time is prolonged, as is aPTT
chromosome analysis
Imaging assessment
chest x-ray
skeletal x-ray
Leukemia: interventions
prevention infection
goal is to halt infection and control new infection early
drug therapy
handwashing
strict aseptic technique-cather care
hematopoietic stem cell transplantation (HSCT)
minimizing injury
conserving energy
central venous catheters and infusions
required for home infusion therapy
keep the catheter open, flush it quickly with saline once a day, and after completing the infusion
change the Luer-Lok cap on each catheter lumen weekly
clean the existing site with alcohol and povidone-iodine or with chlorhexidine
Malignant Lymphomas
Lymphomas are cancers of the lymphoid cells and tissue, with abnormal overgrowth of lymphocytes
Two major adult forms of lymphoma:
Hodgkin’s lymphoma
specific cell type: Reed-Sternberg cell
Non-Hodgkin’s lymphoma
all lymphoid cancers that don’t have the Reed-Sternberg cell
Physical assessment S/S
large, painless lymph nodes
fevers, drenching night sweats, unplanned weight loss
some have no symptoms at time of diagnosis
Interventions
external radiation of lymph node regions
for more extensive disease, radiation and combination chemotherapy is used
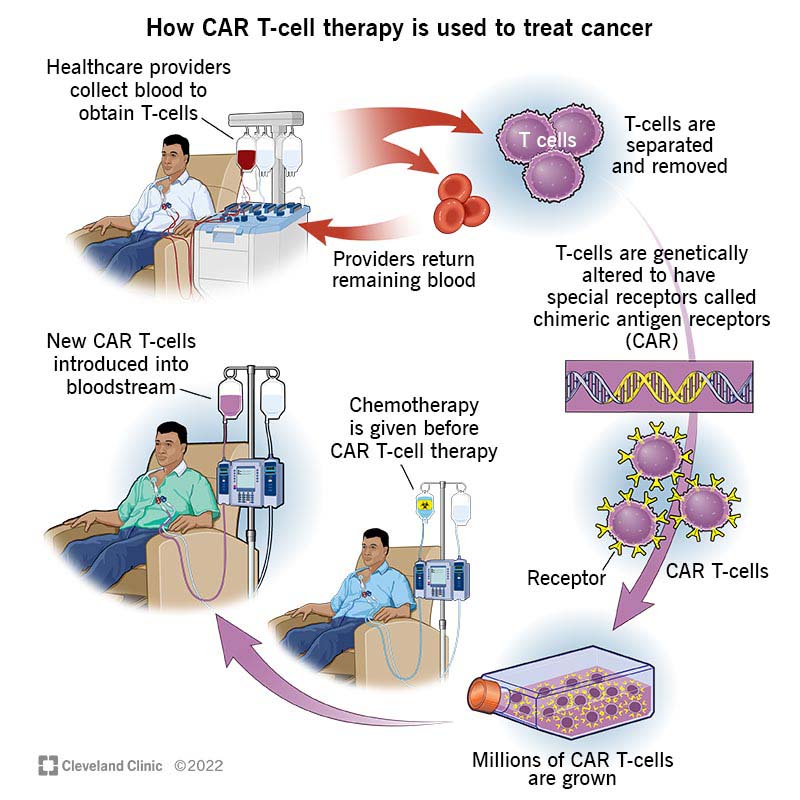
CAR-T therapy
Multiple Myeloma
WBC cancer of mature B-lymphocytes
S/S: fatigue, easy bruising, bone pain
treatment involves watchful waiting: proteasome inhibitors, immunodulating drugs, HSCT
Thrombocytopenic Purpura
destructive reduction of circulating platelets after normal platelet production; impaired clotting occurs
there are many types (ITP, TTP)
heparin-induced thrombocytopenia (HIT)- most common
Unexplained drop in platelet count after heparin treatment
ecchymosis, purpura, anemia may be present
treatment involves platelet transfusions, anticoagulants, splenectomy
Blood Transfusion Protocols
Adhere to critical procedures to ensure patient safety:
Before Infusion
assess lab values to ensure agency guidelines for blood transfusions are followed
verify the PHCP’s prescription for the type of product, dose, and duration of transfusion because the therapy legally requires a prescription
assess pt’s VS, urine output, skin color, and history of transfusion reactions to establish a baseline for identifying possible reactions during and after the procedure
establish or use venous access with a 19-gauge needle or catheter to prevent catheter occlusion or damage to RBC
transfuse blood products (after all safety checks) soon after receiving them from the blood bank to suppress bacterial growth and prevent product deterioration
with another RN, verify the pt by name and number, check blood compatibility, and note expiration time because human error is the most common cause of incompatibility reaction.
During infusion
administer the blood product using the appropriate filtered tubing to remove aggregates and possible contaminants
unless directed otherwise, infuse blood products only with IV normal saline solutions because some other IV solutions can cause hemolysis
stay with the pt for the 1st 15 to 30 minutes of the infusion because this is the time when hemolytic transfusion reactions occur
infuse the blood product at the prescribed rate for the transfusion type to avoid the possible complication of fluid overload
monitor vital signs at least as often as the agent policy and the pt’s condition indicates to identify early indications of adverse transfusion reactions
After infusion
when the transfusion is completed, discontinue the infusion and dispose of the bag and tubing according to agency and blood-bank policies to prevent the spread of bloodborne pathogens
document all aspects of the transfusion (type of product, product number, volume infused, duration of infusion, VS, and any adverse reactions) identify pt response to the transfusion as part of the permanent record
never add to or infuse other drugs with blood products because they may clot the blood during transfusion
Transfusion therapy
pretransfusion responsibilities
review ageny policy
test donor’s/recipient’s blood for compatibility
examine blood bag label, attached tag, and requisitions slip for ABO and Rh comtabilibility with the client
inspect blood for discoloration, gas bubbles, cloudiness
transfusion responsibilities
Administer the blood product using the appropriate filtered
tubing to remove aggregates and possible contaminates
Infuse blood products only with IV normal saline solutions
because some other IV solutions can cause hemolysis
Stay with the patient for the first 15 to 30 minutes of the
infusion because this is the time severe reactions occur
Infuse the blood product at the prescribed rate for the
transfusion type to avoid the possible complication of fluid
overload
Monitor vital signs at least as often as agency policy and the
patient’s condition indicates to identify early indications of
adverse transfusion reactions
transfusions
PRBC transfusions
replaces cells lost from trauma or surgery
Platelet Transfusions
given for low platelet counts, active bleeding, scheduled for invasive procedure
Plasma transfusion
replaces blood vol and clothing factors
Granulocyte (WBC) transfusions
given (rarely) to neutropenic clients
Massive transfusion protocol
given when H&H levels are low
Acute Transfusion Reactions
Febrile
hemolytic
allergic
bacterial
circulatory overload
transfusion-associated graft-versus-host disease (TA-GVHD)
occurs more often in immunosuppressed pt
Interventions for reactions
begin with stopping the transfusion and removing the blood tubing (for hemolytic and suspected bacterial reactions, return the components of bag, labels, and all tubing to the blood bank or lab
initiate RRT
if the pt has no other IV access, keep the access and flush with normal saline. Don’t flush the contents of the blood transfusion tubing, which would allow more of the reaction-causing blood to enter the pt
if shock is present, fluid resuscitation and hemodynamic monitoring are needed
blood pressure support with vasopressors may be needed
drug therapy like antipyretics for fever, antibiotics, and meperidine for rigors
autologous blood transfusions
collection and infusion of pt’s own blood
eliminates compatibility problems
reduces risk for transmitting bloodborne disease