Musculo-Skeletal System – Study Unit 1.9
Spinal Curvature Abnormalities
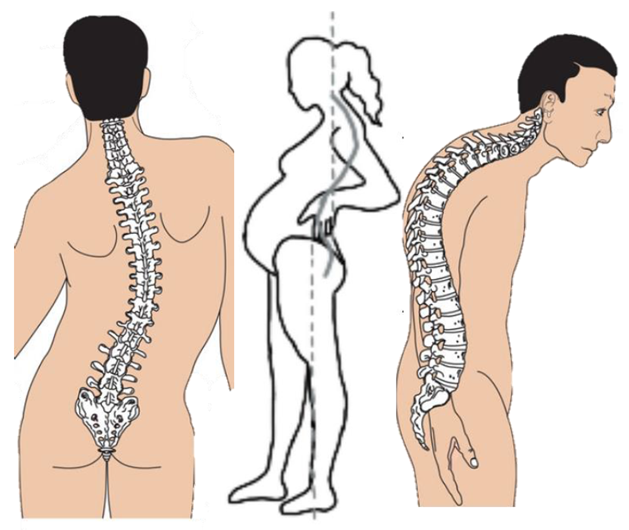
Scoliosis
Lateral curvature of the spine.
May present as an “S” or “C” curve when viewed posteriorly.
Normal spine ≠ scoliosis; visual deviation is diagnostic clue.
Lordosis
Exaggerated curve of the lumbar vertebral column.
Forms a pronounced inward arch at the lower back.
Cervical lordosis may coexist but lumbar distortion is clinically relevant.
Kyphosis
Exaggerated curve of the thoracic vertebral column.
Produces “humpback” appearance.
Fascia & Fasciotomy
Fascia: fibrous connective membrane that covers, supports & separates muscles; variable in fat, collagen, elastin & tissue fluid content.
Fasciotomy: surgical cutting/removal of fascia to relieve pressure (e.g., in compartment syndrome).
Summative Explanations of Core Medical Conditions
Osteoporosis
Metabolic bone disorder marked by significant loss of bone mass & strength ➔ fracture risk.
Pathogenesis: \text{Bone resorption rate} > \text{Bone formation rate}.
Common sites: hip, vertebrae, wrist.
Risk factors: age, menopause, corticosteroid use, low Ca/ Vit D intake, sedentary lifestyle.
Acute Infective Osteomyelitis
Pyogenic bone infection; common in children/adolescents but also in poorly-nourished or immunocompromised adults.
Sudden onset → may become chronic/debilitating if poorly managed.
Usually secondary to existing infection (haematogenous or contiguous spread).
Tuberculosis of Bone
Mycobacterium tuberculosis spreads haematogenously from lungs/lymph nodes.
Prefers vertebrae & long-bone metaphyses (rich vascular supply).
Incidence ↑ in developing countries & with AIDS.
Early painless; late presentation with severe back pain, swelling, abscesses, deformities, neurological compromise (paraplegia).
Systemic TB signs may be absent; latency common.
Treatment: 6–18 months chemotherapeutic regimen (rifampicin, isoniazid, ethambutol, pyrazinamide) ± surgery (e.g., laminectomy).
Carpal Tunnel Syndrome
Median nerve entrapment at wrist within carpal tunnel.
Etiology: repetitive hand motions, vibration, fluid retention.
Presents with numbness, tingling, night pain, thenar weakness.
Muscular Dystrophy
Group of inherited progressive myopathies → muscle fibre degeneration, weakness & replacement by connective/fatty tissue.
Pathology: fibre size variation, phagocytosis, regeneration failure.
Clinical picture (e.g., Duchenne): swayback, weak hip extensors, tip-toe gait, pseudohypertrophic calves, frequent falls.
Differences among types: pattern of inheritance, involved muscles, age of onset, progression rate.
Conditions Presented with Study Framework
Hallux Valgus
Definition
Deformity of big toe (first metatarsophalangeal joint) causing lateral deviation.
Causes/Risk Factors
Narrow-toed, high-heeled footwear.
Genetic predisposition.
Intrinsic biomechanical issues (flat foot, ligament laxity, neurologic disorders).
Pathophysiology
Failure of tendons/ligaments supporting first metatarsal → misalignment.
Progressive bunion formation & medial soft-tissue thickening.
Clinical Manifestations
Red, thickened medial skin; bony bump; pain worsened by shoes; decreased toe ROM; overlapping digits with corns/calluses; shoe-fit difficulty.
Diagnostic Tests
Inspection.
Foot X-ray.
Medical Treatment
Analgesics; corticosteroid injections; corrective surgery.
Basic Nursing Care
Post-op wound & neurovascular checks; pain control; mobilisation protocols.
Health Education
Proper shoe fit; daily foot hygiene/massage; elevation & rest.
Fractures
Definition
Break in bone due to force, trauma or disease.
Causes/Risk Factors
Direct/indirect trauma, sports, occupational hazards, degenerative disorders.
Pathophysiology
Periosteum stripping & vascular disruption ➔ bleeding, haematoma, soft-tissue damage.
Clinical Manifestations
Oedema, pain, loss of function, deformity, discoloration.
Diagnostic Tests (List Only)
X-ray, CT, MRI, bone scan.
Medical Treatment
Reduction (closed/open); immobilisation (cast, traction, ORIF); pain management.
Basic Nursing Care
Neurovascular assessment (5 P’s: pain, pallor, pulselessness, paraesthesia, paralysis).
Elevation, ice, skin integrity monitoring.
Health Education
Cast care; signs of complications (compartment syndrome, infection); nutrition for bone healing.
Types of Fractures (Learning Activity 2)
Greenstick – incomplete break in children (e.g., fall on outstretched arm).
Transverse – perpendicular to bone axis (direct blow).
Oblique – diagonal line (twisting injury).
Comminuted – bone splinters (>2 fragments) (high-energy trauma, e.g., MVC).
Compound/Open – skin breach (gunshot wound).
Compartment Syndrome
Definition
Raised pressure within closed muscle compartment leading to impaired perfusion & nerve damage.
Causes
Fracture, crush injury, severe contusion, re-perfusion, anabolic steroid-induced hypertrophy, tight casts/bandages.
Pathophysiology
Non-distensible fascia encloses muscles/nerves/vessels.
Swelling ↑ intracompartmental pressure > capillary perfusion pressure.
Ischaemia → muscle/nerve necrosis; potential limb loss.
Clinical Manifestations
Severe out-of-proportion pain esp. on passive stretch, tense swollen limb, paresthesia, pallor, pulselessness (late), paralysis (late).
Diagnostic Tests
Physical exam; X-ray to identify underlying fracture; compartment pressure monitoring (if available).
Medical Treatment
Emergent fasciotomy (two-incision four-compartment release in leg) to decompress.
Basic Nursing Care
Pre-op: loosen constrictive dressings, keep limb level with heart (no elevation above heart pre-decompression).
Post-op: sterile dressing, wound VAC, neurovascular checks.
Health Education
Early reporting of escalating pain; care of fasciotomy wounds; avoidance of tight casts or intense repetitive exercise until cleared.
Immediate Care of Acute Compartment Syndrome (Learning Activity 4)
Recognise 5 P’s promptly(Pain, Pallor, Pulselessness, Paraesthesia, and Paralysis).
Remove/loosen casts & dressings.
Keep limb at heart level.
Notify surgical team – time-critical (<6 h optimal).
Prepare for fasciotomy: consent, IV access, analgesia.